Abstract
This study aims to propose a novel surgical technique to rehabilitate patients with long term complication of trachea-esophageal puncture and stomal stenosis. Ours is retrospective study. Ten patients with tracheo-esophageal puncture who developed long term complications and who failed conservative management were included in our study. Majority of our patients were males within the age group of 50–70 years of age. Most of our patients had received adjuvant radiotherapy (8/10). All patients had multiple change of prosthesis. Nine patients suffered from multiple complications of TEP. Most common complication was that of progressive thinning of trachea-esophageal wall. All the patients who underwent this procedure healed well without any major complications. Long term trachea-esophageal puncture may undergo significant modification in terms of position and size. This technique gives a satisfactory and viable method of excising the altered anatomy and establishes speech & swallowing in such patients who fail conservative management.
Keywords: Tracheo-eshophageal puncture, Laryngectomy, Voice prosthesis, Stomal stenosis, Aspiration
Introduction
Since the introduction of Tracheo-Esophageal Puncture (TEP) and subsequent development of voice prosthesis by Bloom and Singer in early 80′s, this procedure has become a standard,well accepted and easily reproducible method of speech rehabilitation following total Laryngectomy [1]. Long term survivors of this procedure tend to develop various complications, commonest being enlargement of fistula, thinning of tracheo-esophageal wall, displacement of fistula either up or down and last but not the least, stomal stenosis.
These complications predispose the patient to salivary leak, chronic aspiration leading to frequent lung infection, poor quality of voice, difficulty in valve maintenance and frequent change of prosthesis. Various methods, surgical and non-surgical, have been employed to address these complications with variable outcomes. In the eventuality of failure, closure of fistula is the only option left thereby depriving the patients of their voice. This study proposes a novel surgical technique to address the above mentioned long term complications of TEP with or without stomal stenosis and re-establish communication.
Material and Methods
Our’s is a retrospective study carried out from 2015–2020 at department of otorhinolaryngolgy and head and neck surgery, Sri Devaraj Urs Medical College. After obtaining institutional ethical committee clearance, 10 patients were included in our study.
Inclusion Criteria
Patients who developed refractory complications of TEP such as fistula widening, displacement, thinning of trachea-esophageal wall and stomal stenosis,who failed conservative management where included in our study.
Methodology
This procedure was performed under General Anaesthesia. A flexo-metallic endotracheal tube was introduced into the tracheostome and secured in the midline allowing adequate length to facilitate frequent removal and operative manoeuvres. A second 8 Fr. endotracheal tube was passed per-orally into the neopharynx for ease of identification. A 16 Fr. Ryles tube was also introduced through the nose and positioned in the stomach for subsequent feeding. The patient was placed in supine position, hands by the side and neck extended.
A generous inverted ‘D’ shaped incision was marked around the stoma (Fig. 1). The incision was taken and developed from 3 to 9 o’clock position. The lower skin flap was developed all along to expose and mobilise the tendon of Sternocleidomastoid muscle (SCM) bilaterally and the anterior wall of trachea (Fig. 2). Carefully palpating the trachea and the endotracheal tube in the neopharynx the dissection was further carried out on the lateral tracheal wall till the trachea-esophageal groove bilaterally. At this stage, the horizontal limb of the ‘D’ was incised and the superior skin flap elevated, clear of TEP and the neopharynx. Tracheal ring below the existing TEP was marked by electrocautery and the anterior wall of trachea was incised at the corresponding ring. The Incision was extended laterally on both sides and thereafter across the posterior wall of trachea (Fig. 3). The cut tracheal segment was grasped with Allis Forceps and reflected upwards. Carefully palpating the pre-positioned Foleys catheter in the TEP, endotracheal tube in the neopharynx and the Ryles Tube in the cervical oesophagus, the entire fistulous tract was dissected till its entry into the neopharynx. Extreme care was taken to avoid the tracheo-esophageal assembly below the line of fistula. The fistulous tract was cut flush with the pharyngeal wall. The tracheostome now was refashioned and a new TEP was created by passing a blunt haemostat through the pharyngeal opening and an incision was made into the posterior tracheal wall in the midline on the tip of the haemostat. A 14 Fr. Foleys catheter was inserted well into the thoracic oesophagus after taking out the per-oral endotracheal tube (Fig. 4). The pharynx was closed in two layers and finally the superior skin flap was sutured to the posterior wall of trachea to complete the tracheostome. Since the dissection was strictly in the midline, the tissues easily fell into place and therefore, no drains were used (Fig. 5). All our patients were fed through the Ryles tube for 4–5 days after which test feed was given and normal alimentation restored. After carefully sizing the TEP on 10th Post-operative day, appropriate voice prosthesis was introduced to restore normal communication.
Fig. 1.

Picture showing incision planning and positioning of endotracheal tube
Fig. 2.
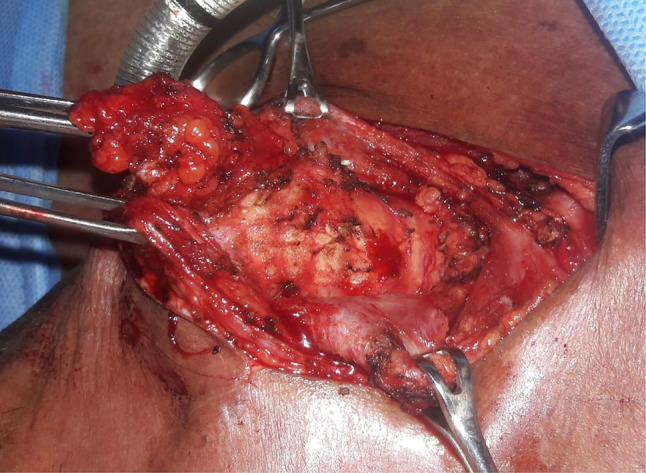
Picture showing mobilized bilateral sternocleidomastoid muscle and anterior tracheal wall
Fig. 3.
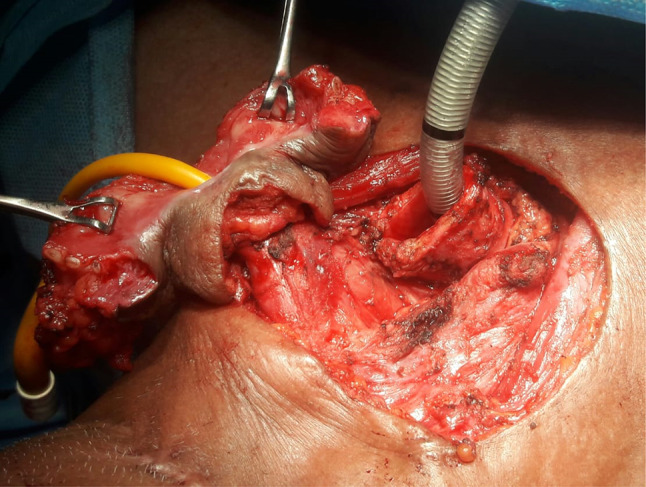
Picture showing tracheal incision and isolation of TEP-fistulous tract
Fig. 4.
Picture showing refashioned tracheostoma, new TEP and closure of neopharynx
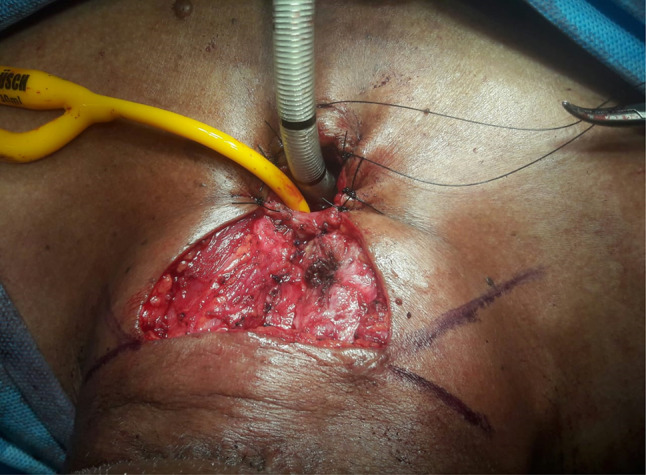
Fig. 5.

Postoperative picture showing healed stoma and revised TEP
Results
Except one, all our patients were male and were in the age group ranging between 50–70 years. Eight patients had laryngeal carcinoma while the other two were diagnosed as carcinomas of the hypopharynx.Eight patients included in our study had received adjuvant radiation therapy. Among the 10 patients, 4 patients had stomal stenosis, one patient had upward shift of TEP,one patient had downward shift of TEP, eight patients had progressive thinning of tracheo-oesophageal wall needing frequent change of prosthesis and 4 patients had frequent lung infection due to aspiration secondary to dilatation of TEP. Majority of our patients (9/10) suffered multiple complications of TEP (Table.1).
Table 1.
Clinical data of patients with TEP related complications
| Serial no. | Diagnosis and staging | Patients who received adjuvant Radiotherapy | Complication of Tracheo-eshophageal puncture | |||||
|---|---|---|---|---|---|---|---|---|
| Stomal stenosis | Upward shift of TEP | Down ward shift of TEP | Progressive thinning of part of tracheoesophageal wall | Widening of TEP with Aspiration | Frequency of voice prosthesis replacement | |||
| 1 | Carcinoma glottis (Stage IV) | + | + | – | – | + | + | 3 |
| 2 | Carcinoma glottis (stage III) | – | – | – | + | – | – | 5 |
| 3 | Carcinoma glottis (Stage IV) | + | – | – | – | + | – | 4 |
| 4 | Carcinoma glottis (Stage IV) | + | – | – | – | + | + | 4 |
| 5 | Carcinoma glottis (Stage IV) | + | + | + | – | + | + | 4 |
| 6 | Carcinoma glottis (Stage IV) | + | + | – | – | + | – | 5 |
| 7 | Carcinoma glottis (Stage III) | – | – | – | – | + | + | 4 |
| 8 | Carcinoma glottis (Stage IV) | + | – | – | – | + | – | 3 |
| 9 | Carcinoma Hyphopharynx (Stage IV) | + | – | – | – | + | – | 3 |
| 10 | Carcinoma Hyphopharynx (Stage IV) | + | + | – | – | – | – | 2 |
All ten patients who underwent this procedure healed well without any major complications. Since the dissection was kept to the minimum, the surrounding tissue could be brought together in tension-free manner obviating any need of reconstruction procedure.
Discussion
Tracheo-Esophageal Puncture and subsequent introduction of indwelling voice prosthesis has revolutionised the vocal rehabilitation following total laryngectomy with a success rate of 70–90% [2]. Complications of this procedure do occur, especially in long term survivors who undergo multimodality treatment. Progressive enlargement of fistula, thinning of tracheo-esophageal wall, displacement of fistula, accidental dislodgement of prosthesis and stomal stenosis are some of the complications we encounter.
Progressive dilatation of fistula are prone to occur in 42–70% of patients, [2] predisposing the individual to salivary leak, chronic aspiration, poor quality of voice and frequent change of prosthesis. The problem is addressed by various techniques such as removal of prosthesis to allow spontaneous shrinkage, cauterization of fistula to facilitate narrowing, injection of granulocyte-macrophage colony stimulating factor, purse string suture around the fistula. Spontaneous shrinkage has been found to be successful in around 50% of patients and not so useful in individual who have received adjuvant radiation [3, 4]. Purse string suturing, although a minor surgical procedure, may require multiple sittings and multiple suturing, a small stoma makes this procedure difficult and at times impossible [2].
Progressive thinning of trachea-esophageal wall is also known to allow salivary leak and chronic aspiration. Various techniques have been employed to increase trachea-esophageal wall thickness like injection of collagen, hylaform, bioplastique and colony stimulating factor. The disadvantage of these procedure is recurrence and requirement of repeated injections which may not be cost effective [2].
In the long term, displacement of fistula tends to occur either in the upward or downward direction. Upward displacement of fistula can hamper with effective stomal closure and poor voice quality, whereas downward displacement hampers voice production and further valve replacement. When all methods fail, the only option is to close the fistula and deprive the patient of his voice [5].
As highlighted in our study, patients can suffer from multiple problems and a single modality may not be effective in addressing all of them. Therefore, our technique essentially aims to excise the malfunctioning fistula and create an altogether new TEP, with refashioning of tracheostome. Our technique can address multiple factors contributing to failure of TEP and help in vocal rehabilitation of such patients.
Conclusion
Primary tracheoesophageal puncture remains the gold standard method of speech rehabilitation following total laryngectomy. However, in long term survivors due to advancing age, TEP may undergo significant modification in terms of position and size. This technique gives a satisfactory and viable method of excising the altered anatomy and establishes speech and swallowing in such patients who fail conservative management.
Authors Contributions
R.P.D: Contributed to the design of study, collected samples, did data analysis and drafted the manuscript., S.A: Contributed to the design of study, data analysis, helped frame and edited the manuscript, Corresponding author for the manuscript, B.A.K. Contributed to the design of study, data analysis, helped frame and edited the manuscript, S.M.A.M Contributed to the design of study, data analysis, helped frame and edited the manuscript.
Funding
There was no funding by any organization or source for this study.
Compliance with Ethical Standard
Conflict of interest
The authors declare no conflict of interest or commercial affiliation related to this study.
Ethics Approval
This study was approved by institutional ethical committee,No.SDUMC/KLR/IEC/1778/2020–21.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figure(s) 1,2,3,4 and 5.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Op B, de Coul F, Hilgers AB, Tan I, van den Hoogen F, van Tinteren H. A decade of postlaryngectomy vocal rehabilitation in 318 patients. Arch Otolaryngol Head Neck Surg. 2000;126:1320. doi: 10.1001/archotol.126.11.1320. [DOI] [PubMed] [Google Scholar]
- 2.Jacobs K, Delaere P, Poorten V. Submucosal purse-string suture as a treatment of leakage around the indwelling voice prosthesis. Head Neck. 2008;30:485–491. doi: 10.1002/hed.20732. [DOI] [PubMed] [Google Scholar]
- 3.Brasnu D, Pages JC, Laccourreye O, Jouffre V, Monfrais P, Fauwadel MC, Crevier Buchman L. Results of the treatment of spontaneous widening of tracheoesophageal punctures after laryngeal implant. Ann OtolaryngolChirCervicofac. 1994;111:465–560. [PubMed] [Google Scholar]
- 4.Andrews JC, Mickel RA, Hanson DG, Monahan GP, Ward PH. Major complications following tracheoesophageal puncture for voice rehabilitation. Laryngoscope. 1987;97:562–567. doi: 10.1288/00005537-198705000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Hosal S, Myers E. How I do it: closure of tracheoesophageal puncture site. Head Neck. 2001;23:214–216. doi: 10.1002/1097-0347(200103)23:3<214::AID-HED1020>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]


