Abstract
A mucocele of a paranasal sinus is a mucus filled cystic mass lined by epithelium filling the involved sinus whose ostium is obstructed. While frontoethmoidal mucoceles are common, Onodi cell mucoceles are less frequently seen. Due to its anatomic proximity to optic nerve, it can lead to devastating visual complications. A 29 year old female presented with progressive loss of vision in right eye since 20 days leading to complete loss of vision since 12 days without any nasal complaints. Endoscopy showed fullness in right spheno-ethmoidal region. Computed Tomography scan revealed a mucocoele of the right Onodi air cell causing compression of intracanalicular part of right optic nerve. Despite urgent surgical decompression of mucocele, vision could not be restored. Poor visual acuity at presentation may be associated with bad prognosis. Hence, a high index of suspicion followed by appropriate imaging (CT scan and/or MRI nose and paranasal sinus) is crucial for early diagnosis in case of unexplained progressive diminution of vision, even in setting of no nasal complaints.
Keywords: Onodi cell, Mucocele, Visual acuity, Optic neuritis, Endoscopic decompression
Introduction
A mucocele is a dilated mucus filled sinus lined by mucus membrane. The etiology of mucocele is multifactorial which involve inflammation, allergy, trauma, anatomic abnormality, previous surgery [1]. However, in substantial number of cases, no identifiable cause is found. The vast majority of mucocele arises in frontal (65%) and ethmoidal sinuses (25%), as they are numerous with narrow ostia, in contrary to the sphenoid sinus (only 1–2%) [2–4]. The reported prevalence of Onodi cell mucocele ranges from 3 to 42% in the general population but in Asians rates can be as high as 50–60 percent [5]. An Onodi cell is the most posterior ethmoidal cell, which pneumatises laterally and superiorly, and is intimately related to the optic nerve [6]. Owing to the anatomic proximity with optic nerve, Onodi cell mucocele can result in compressive optic neuropathy and blindness. The most widely accepted treatment protocol is endoscopic marsupialisation of the mucocele [7]. We have presented a case of Onodi cell mucocele with optic neuritis and review of the current literature.
Case
A 29 year old female presented in our ENT OPD with progressive loss of vision in right eye since 20 days leading to complete loss of vision since 12 days. Patient had no prior history of any nasal obstruction or discharge or any surgical intervention for any nasal pathology. There was no history of restriction of eye movements. Patient received 2 doses of intravenous methyl prednisolone (1 mg/kg) at a peripheral centre two days prior to presenting to us. Clinical examination revealed absent perception of light in right eye. On endoscopic assessment, we found fullness in the right spheno-ethmoidal recess area as depicted in Fig. 1. Computed Tomographic (CT) scan nose and paranasal sinus revealed a mucocoele of the right Onodi air cell causing compression of intracanalicular part of right optic nerve as shown in Fig. 2 (axial section) & Fig. 3 (sagittal section).
Fig. 1.
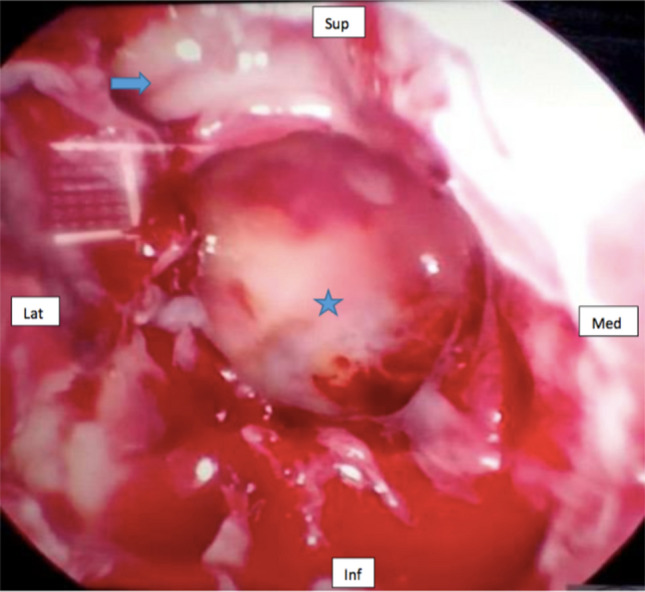
Pre operative endoscopic image. Star—mucocoele; arrow—optic nerve; Sup—superior; Med—medial; Inf—inferior; Lat—lateral
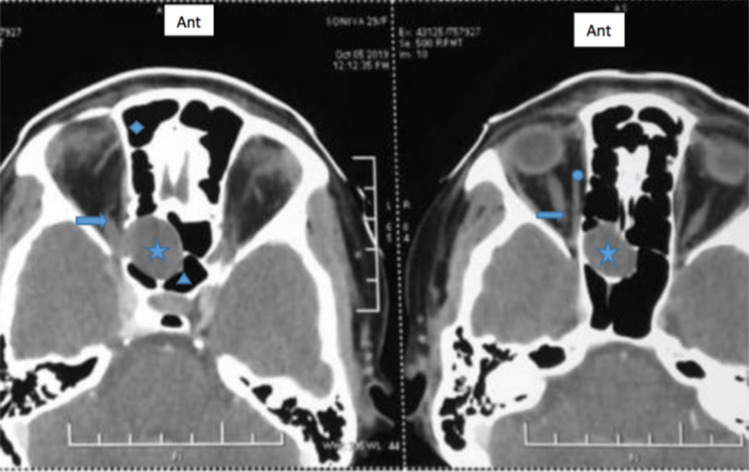
Fig. 2.
Radiological image (axial section) depicting right Onodi cell mucocele compressing intracanalicular optic nerve. star—mucocele; arrow—optic nerve; circle—extraocular muscle; triangle—sphenoid sinus; diamond—ethmoid sinus; Ant—anterior
Fig. 3.

Radiological image (sagittal section) depicting right Onodi cell mucocele compressing optic nerve. star—mucocele; arrow—optic nerve; circle—extraocular muscle; triangle- sphenoid sinus; Sup- superior
We did endoscopic surgical decompression of the mucocele under general anaesthesia in emergency on the same day when patient presented. We performed right sphenoidotomy, identified the mucocele and marsupialised it into ipsilateral nasal cavity as shown in Fig. 4. The patient recovered well, however the postoperative ophthalmological examination also showed absent perception of light in right eye. Postoperatively we continued intravenous steroids (methyl prednisolone 1 mg/kg) in an attempt to salvage the vision, along with antibiotics and regular assessment of vision. However, due to the late presentation of the patient, we could not recover her right eye vision. The patient is still on follow up.
Fig. 4.
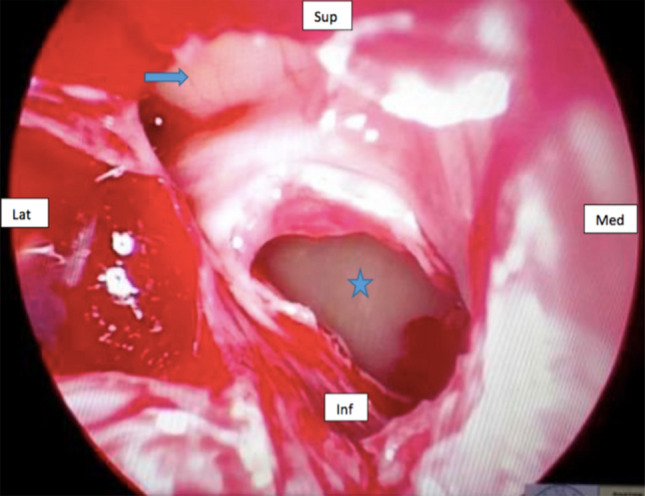
Post operative endoscopic image. star—enlarged sphenoid ostium; arrow—optic nerve; Sup—superior; Med—medial; Inf—inferior; Lat—lateral
Discussion
Mucoceles are collection of mucus lined by mucus secreting epithelial cells of paranasal sinus. Mucoceles of Onodi cell are rare. The reported prevalence of Onodi cell mucocele ranges from 3 to 42 percent in the general population but in Asians rates can be as high as 50–60 percent [5]. Lee et al. [4] suggested in their review article that 12 out of 16 cases of Onodi cell mucocele were Asians.
Onodi cell is a posterior ethmoid cell that pneumatises lateral and superior to sphenoid sinus, its pneumatisation extending around optic canal and nerve. Proposed theories for optic nerve neuropathy in Onodi cell mucocele are:
Direct compression of optic nerve due to close anatomic proximity and absent surrounding fat or soft tissue.
Ischemia due to resulting compression of vasa nervosum.
Inflammation due to infected mucocele, wherein infection spreads along nerve via cleavage in optic canal wall or bone resorption site [3].
The vision loss accompanying an Onodi cell mucocele can be sudden or gradual. It is suggested that gradual visual acuity decrease is caused by direct mechanical compression of mucocele whereas, rapid loss of visual acuity is by spread of infection and inflammation [8]. Argyrios et al. [9] also proposed that microvascular and inflammatory factors were more frequently related to acute onset and rapid progression of visual disturbances rather than mechanical compression which was mainly characterised by gradual appearance of clinical symptoms. The common complications of Onodi cell mucocele are vision loss, eye pain and swelling, extra-ocular movement restriction, cranial nerve palsies, optic neuropathy and hence urgent investigation and intervention is recommended.
High index of suspicion is warranted for patients fitting in the clinico-pathological profile. On CT scan, a mucocele appears as a hypo dense, non enhancing, well defined mass that fills and expands sinus cavity. Contrast enhanced MRI reveals regular peripheral enhancement with central low signal intensity on T1 weighted imaging. Coronal cuts to be included to rule out retrobulbar neuritis. Prompt endoscopic sinus surgery should be done following the imaging, along with intravenous corticosteroids and antibiotics.
Azgyrios et al. [9], reviewed 24 patients, 15 patients out of them reported improvement in vision. However, for nine out of 24 patients, surgical intervention did not result in vision improvement. We also found no improvement in visual acuity. Initial poor visual acuity (< finger counting) upon presentation is associated with adverse recovery as compiled in Table 1. Nonaka et al. [3] reported that prognosis is poor when preoperative degree of visual impairment is high and onset is sudden, which is also in concordance with our finding. Yumoto et al. reported that decompression within 2 days of visual loss and within 24 h of loss of light sensitivity results in complete restoration of visual acuity [10]. Arnavielle et al. reported a case in which decompression three days after onset of symptoms resulted in complete resolution of symptoms. Therefore early diagnosis and intervention is imperative. However, Kitagawa et al. [11] and Yoshida et al. [12] reported complete visual recovery despite decompression surgery being delayed for one week and three weeks respectively while Lee et al. [4] concluded that early surgical intervention may improve visual outcome dramatically. Delayed treatment has been associated with poor prognosis.
Table 1.
Review of cases presenting with poor visual acuity in Onodi cell mucocele
| S. no | Author | Age/sex | Presentation | Exam findings | Medical history | Time to surg | T/t | Course | Final visual acuity |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Nonaka et al 2007 | 41 yr/male | sudden painful decrease vision | Light perception + | 12 days | FESS + steroid |
No improvement Follow up (6 months)—stable |
light perception + | |
| 2 | Loo et al., 2008 | 53 yr/ male |
first visit-intermittent blurring of vision headache Second visit-5 months later- loss of vision |
No light perception RAPD Proptosis |
ESS + steroid | No light perception, optic nerve atrophy(2 months later) | No light perception | ||
| 3 | Nickerson et al. 2010 | 51 yr/female |
Complete loss of vision Diagnosis 5 week later- optic nerve atrophy |
No light perception | orbital fracture 38 years ago | 7 week | FESS + steroids | Anatomical success, no visual acuity improvement | no light perception |
| 4 | Victories et al., 2010 | 46 yr/ Male |
Blurring of vision-3 days Sudden loss of vision |
no light perception | Chronic sinusitis, previous endoscopic surgery | FESS | 1 month- no improvement | No light perception | |
| 5 | Fleissig et al., 2014 |
53 yr/ femalesudden loss of vision Pain in ocular movements Eye edema Double vision |
RAPD Eyelid edema Diplopia Paresthesia V1and V2 Eye movement limitation |
finger counting | chronic rhinosinusitis treated with ESS | 1 day | FESS + steroids |
No light perception Normal eye movements Optic disc atrophy |
no light perception |
| 6 | Cheon et al., 2014 | 60 yr/Male |
Headache Visual loss |
no light perception | Brain infarction for 5 year | 2 year | ESS |
No headache Visual improvement (Content-fungal ball- aspergilloma) |
No light perception |
| 7 | Rueping et al., 2014 | 39 yr/male |
acute visual loss Dull orbital headache |
no light perception RAPD |
ESS 20 yr ago for chronic sinusitis | ESS | No light perception | no light perception | |
| 8 | Kwon et al., 2019 | 62 yr/ | Double vision decreased vision |
trochlear nerve palsy Pathological ocular motility test VA = 1.0 |
ESS + steroid |
Orthotropia Improvements in ocular motility(4 months later) |
No improvement in vision | ||
| 9 | Tzamalis,2019 | 34 yr/ male | sudden loss of vision |
finger counting + RAPD |
ESS + steroid |
VA = hand motion + Optic nerve paleness Follow up (3 years)-VA = light perception Stable(content = purulent fluid) |
Light perception + | ||
| 10 | Kirti et al., 2021 | 29 yr/ female | progressive loss of vision for 20 days and complete loss for 12 days | no light perception | 20 days | ESS + i.v. steroid | no improvement in vision | no light perception |
To summarise, poor visual acuity at presentation may be associated with worse prognosis. Hence, a high index of suspicion is crucial for early diagnosis since timely diagnosis is a major challenge. Appropriate investigation and prompt intervention can assist in speedy recovery.
Conclusion
Onodi cell mucocele owing to its close proximity to optic nerve can lead to serious ophthalmologic complications. The delay in time elapsed between the onset of symptoms and adequate treatment points towards poor recovery of the vision. Therefore, such cases are an eye opener for practioners all over the country. In case of dilemma in diagnosis of unexplained diminution of vision even in setting of no nasal complaints, it is imperative to undergo appropriate imaging (CT scan or MRI nose, paranasal sinuses and orbit) so that such lesions aren't missed. Immediate surgical decompression for mucocele is to be considered to avoid complications.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures were in accordance with the ethical standards of the institution.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aggarwal SK, Bhavana K, Keshri A, Kumar R, Srivastava A. Frontal sinus mucocele with orbital complications: management by varied surgical approaches. Asian J Neurosurg. 2012;7(3):135–140. doi: 10.4103/1793-5482.103718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Devars du Mayne M, Moya-Plana A, Malinvaud D, Laccourreye O, Bonfils P. Sinus mucocele: natural history and long-term recurrence rate. Eur Ann Otorhinolaryngol Head Neck Dis. 2012;129(3):125–130. doi: 10.1016/j.anorl.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Nonaka M, Fukumoto A, Nonaka R, Ozu C, Baba S. A case of a mucocele in an Onodi cell. J Nippon Med Sch. 2007;74(4):325–328. doi: 10.1272/jnms.74.325. [DOI] [PubMed] [Google Scholar]
- 4.Lee JM, Au M. Onodi cell mucocele: case report and review of the literature. Ear Nose Throat J. 2016;95(9):E4–E8. doi: 10.1177/014556131609500905. [DOI] [PubMed] [Google Scholar]
- 5.Moeller CW, Welch KC. Prevention and management of complications in sphenoidotomy. Otolaryngol Clin North Am. 2010;43(4):839–854. doi: 10.1016/j.otc.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 6.Stammberger HR, Kennedy DW. Paranasal sinuses: anatomic terminology and nomenclature. Ann Otol Rhinol Laryngol. 1995;104(10_suppl):7–16. doi: 10.1177/000348949510410s01. [DOI] [PubMed] [Google Scholar]
- 7.Qureishi A, Lennox P, Bottrill I. Bilateral maxillary mucoceles: an unusual presentation of cystic fibrosis. J Laryngol Otol. 2012;126:319–321. doi: 10.1017/S002221511100329X. [DOI] [PubMed] [Google Scholar]
- 8.Moriyama H, Nakajima T, Honda Y. Studies on mucocoeles of the ethmoid and sphenoid sinuses: analysis of 47 cases. J Laryngol Otol. 1992;106(1):23–27. doi: 10.1017/S002221510011850X. [DOI] [PubMed] [Google Scholar]
- 9.Tzamalis A, Diafas A, Riga P, Konstantinidis I, Ziakas N. Onodi cell mucocele-associated optic neuropathy: a rare case report and review of the literature. J Curr Ophthalmol. 2020;32(1):107–113. doi: 10.1016/j.joco.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yumoto E, Hyodo M, Kawakita S, Aibara R. Effect of sinus surgery on visual disturbance caused by sphenoethmoid mucoceles. Am J Rhinol. 1997;11(5):337–344. doi: 10.2500/105065897781286025. [DOI] [PubMed] [Google Scholar]
- 11.Kitagawa K, Hayasaka S, Shimizu K, Nagaki Y. Optic neuropathy produced by a compressed mucocele in an Onodi cell. Am J Ophthalmol. 2003;135(2):253–254. doi: 10.1016/S0002-9394(02)01941-4. [DOI] [PubMed] [Google Scholar]
- 12.Yoshida K, Wataya T, Yamagata S. Mucocele in an Onodi cell responsible for acute optic neuropathy. Br J Neurosurg. 2005;19(1):55–56. doi: 10.1080/02688690500081032. [DOI] [PubMed] [Google Scholar]