Abstract
Sphenoid sinus anatomical variations are very common, its prior knowledge is very essential while doing skull base surgery to avoid catastrophic complications which might be due to damage of surrounding neurovascular structures. This retrospective observational study was done to examine the different anatomical variations of sphenoid sinus on CT PNS which was conducted in KMCH, Katihar from May 2019 to April 2020 involving 60 cases above 15 years of age who had undergone CT PNS. Sellar type of pneumatization was seen in 66.7%, pterygoid process pneumatization was seen in 25%. Single septation was present in 43.3%, septum attached to optic nerve was seen in 33.3%, onodi cell was seen in 36.7%, anterior clinoid process pneumatization was seen in 13.3% of cases. By this study we came to a conclusion that preoperative assessment of sphenoid sinus anatomy and its variations is mandatory to avoid surrounding neurovascular structure damage and CSF leak.
Keywords: Anterior clinoid process, FESS, Neurovascular structure, Onodi cell, Pneumatization, Pterygoid process, Sphenoid sinus
Introduction
The sphenoid sinuses are paired air filled spaces within the body of sphenoid bone, communicating with the nasopharynx via sphenoethmoidal recess through sphenoid ostium in its anterior wall. The two sinuses are separated by a septum which may or may not be in the midline. The sphenoid sinus separates cavernous sinuses, cavernous segments of carotid arteries, optic, oculomotor, trochlear and 1st and 2nd division of trigeminal nerve and pituitary gland from nasal cavity and surrounding structures. The sphenoid sinus is present only in primates. In human it develops postnatally and reaches adult size usually by the age of 12 years [1]. The sphenoid sinus varies in size, shape and degree of pneumatization. Depth of sphenoid sinus is distance from sphenoid sinus ostium to closest part of sella. In adult, average antero-posterior diameter of the cavity is 17 mm (range 12–23 mm) [2, 3]. The degree of pneumatization of sphenoid sinus is highly variable and likely to damage the surrounding structures including the optic nerve, oculomotor nerve, trochlear nerve, abducent nerve, vidian nerve, maxillary nerve, cavernous sinuses, and internal carotid arteries. So, clear conception of entire anatomy of the sphenoid sinus is necessary for successful sinus surgery [4, 5]. In relation to sella turcica three types of pneumatization patterns have been identified as sellar type (90%), presellar type (9%), conchal type (1%) [6]. For endoscopic trans-sphenoid approach, sphenoid sinus pneumatization pattern plays most important role in which the sellar type being most common and most favourable [7, 8]. Surgeon’s preference regarding skull base and parasellar space depends on particular pneumatisation pattern depending on different number and position of septa which is specific to patient [9]. For imaging of sinuses, computed tomography is a gold standard procedure [10]. Important information can be obtained from pre-operative imaging and also a plan for safe surgery can be made because sphenoid sinus acts as a corridor for reaching skull base [11]. This study was done aiming to identify incidence of various anatomical variations of sphenoid sinus in CT PNS.
Material and Methods
This retrospective observational study was carried out at Katihar Medical College, Katihar from May 2019 to April 2020. 60 patients (120 sides) above 15 years of age who had CT-PNS done were randomly included in this study. CT scan was done in the department of Radiology. Scanning was done from roof of the frontal sinus up to the hard palate. Slice thickness of 1 mm taken. Images were reconstructed in coronal, axial and sagittal view (1 mm). Coronal, sagittal and axial view of CT-PNS studied. Type of pneumatization and onodi cell were best seen in sagittal view. Number of septations, pterygoid process and anterior clinoid process pneumatization were best seen in axial and coronal view. Anatomical variations like types of pneumatization of sphenoid sinus, pterygoid process and anterior clinoid process pneumatization, presence of onodi cell, number of septations in sphenoid sinus were studied. The study was approved from the institutional ethical committee of our institute.
Result
| Total no. studied | Result | |
|---|---|---|
| 1. Types of pneumatization (Fig. 1) | 60 |
Conchal- 2 (3.3%), presellar- 18 (30%) Sellar- 40 (66.7%) |
| 2. Pterygoid process pneumatization (Fig. 2) | 120 sides | 30 (25%) |
| 3. Septation (Fig. 3) | 60 |
Single- 26 (43.3%), multiple- 18 (30%) None- 16 (26.7%) Septa attached to carotid artery- 14 (26.7%), to opticnerve- 20 (33.3%) To both carotid artery and optic nerve- 6 (10%) |
| 4. Onodi cell (Fig. 4) | 60 | 22 (36.7%) |
| 5. Anterior clinoid process pneumatization (Fig. 5) | 120 sides |
Total- 14 (13.3%) Unilateral- 6 (5%) Bilateral- 4 (3.3%) |
Fig. 1.

Sphenoid sinus pneumatisation—post sellar type
Fig. 2.

Pterygoid process pneumatisation—left side
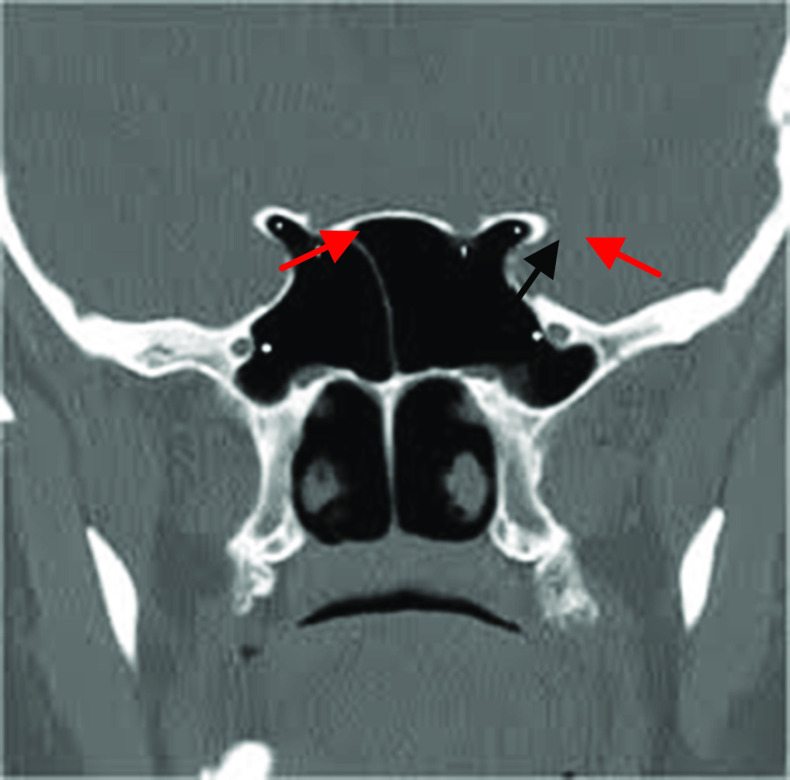
Fig. 3.

Septation—right side
Fig. 4.
White arrow—Onodi cell, red arrow—sphenoid sinus
Fig. 5.
Anterior clinoid process pneumatisation
Discussion
For removal of pituitary adenoma trans-sphenoid surgery is standard approach. Diversity of the trans-sphenoid approach is that it is least traumatic route to the Sella turcica, avoids brain retraction, and provides excellent visualization of the pituitary gland and related lesions. In comparison to transcranial procedure morbidity and mortality rate is low by this approach [12]. Sellar bulge is prominence in the roof of a well-pneumatized sphenoid sinus [13]. Intersphenoid septum usually deviates to one side and divides the sinus into two unequal cavities, resulting in asymmetrical appearance of the Sella turcica floor. Septum deviates laterally and terminates on the carotid artery in about 32–40% of cases, hence under such circumstances extreme precaution requires to be taken during removal of terminal septum to prevent accidental and serious injury to the carotid artery [14, 15]. Most common type of pneumatisation is sellar type, where the air cavity extends into the body of sphenoid below the Sella and may extends to clivus [16].
Depending on the pneumatization of the sphenoid bone, the sphenoid sinus can be classified into the following types:
Conchal—a small pit-like depression.
Presellar—extending up to the anterior wall of the pituitary fossa.
Sellar—extending up to the clivus. The pituitary forms a distinct bulge in the roof of the sinus.
In the present study of 60 cases, conchal type of pneumatization was seen in 3.3%, pre sellar type was seen in 30%, and sellar type was seen in 66.7%. This was in agreement with the work done by Baldea and Sandu [17] who found conchal type 14%, presellar type 44% andsellar type 82%.
In the present study of 120 pterygoid process (i.e.; two pterygoid process of each sphenoid bone) pneumatization was found in 25% of cases. This was in accordance with the findings of Alam-Eldeen et al. [18].
In the present study of 60 sphenoid sinuses, intersphenoid sinus septum was found single in 43.3%, multiple in 30% and none in 26.7%. Inter sphenoid sinus septum was attached to carotid artery in 26.6%, to optic nerve in 33.3%, to carotid artery and optic nerve in 10% of cases. This was in agreement with the work done by Famurewa et al. who found single septum in 46.9%, multiple in 50.6%, none in 2.5% and attached to carotid artery in 31.6% cases [19].
In the present study of 60 sphenoid sinuses, Onodi cell was found in 36.7% cases. This observation was comparable with the work done by Thimmaiah et al. who found Onodi cell in 24.7% cases [20].
In the present study of 60 sphenoid sinuses with 120 Anterior clinoid processes, pneumatization wasseen in 13.3% of cases. It was seen unilateral in 5% and bilateral in 3.3%. This was in agreement with the work done by Mikami et al. who found Anterior clinoid process pneumatization in 9.2% [21].
Conclusion
Due to vast anatomical variations which are commonly seen in pneumatization of sphenoid sinus, surgeon should be very careful while performing FESS or skull base surgery to avoid neurovascular injuries because of exposed neural and vascular structures and CSF leak.
Funding
None.
Availability of data and materials
Data obtained from the available patient treatment record in record section of our Institute and images taken from the memory of the machine of the Institute.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval for study taken from institutional ethics committee.
Consent to participate/publication
As it is record based observational study and patient identity is not revealed hence consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Md. Akbar Ali, Email: ali.drakbar@yahoo.com
D. Manish Jaiswal, Email: rush.manish@gmail.com
D. B. Sameer Ahamed, Email: dbsameerahamed666@gmail.com
Vinita Kumari, Email: vinitabinay@yahoo.com.
Shamser Alam, Email: Shamsheer.jnmc@gmail.com.
References
- 1.Vidić B. The postnatal development of the sphenoidal sinus and its spread into the dorsum sellae and posterior clinoid processes. Am J Roentgenol Radium Ther Nucl Med. 1968;104(1):177–183. doi: 10.2214/ajr.104.1.177. [DOI] [PubMed] [Google Scholar]
- 2.Fujii K, Chambers SM, Rhoton AL., Jr Neurovascular relationships of the sphenoid sinus: a microsurgical study. J Neurosurg. 1979;50:31–39. doi: 10.3171/jns.1979.50.1.0031. [DOI] [PubMed] [Google Scholar]
- 3.Hardy J. Transsphenoidal hypophysectomy. J Neurosurg. 1971;34:582–594. doi: 10.3171/jns.1971.34.4.0582. [DOI] [PubMed] [Google Scholar]
- 4.DeLano MC, Fun FY, Zinreich SJ. Relationship of the optic nerve to the posterior paranasal sinuses: a CT anatomic study. AJNR Am J Neuroradiol. 1996;17(4):669–675. [PMC free article] [PubMed] [Google Scholar]
- 5.Cho JH, Kim JK, Lee JG, Yoon JH. Sphenoid sinus pneumatization and its relation to bulging of surrounding neurovascular structures. Ann Otol Rhinol Laryngol. 2010;119(9):646–650. doi: 10.1177/000348941011900914. [DOI] [PubMed] [Google Scholar]
- 6.Hammer G, Radberg C. The sphenoidal sinus: an anatomical and roentgenologic study with reference to transsphenoid hypophysectomy. Acta Radiol. 1961;56:401–422. doi: 10.3109/00016926109172836. [DOI] [PubMed] [Google Scholar]
- 7.Sethi DS, Leong JL. Endoscopic pituitary surgery. Otolaryngol Clin N Am. 2006;39:563–583. doi: 10.1016/j.otc.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Hamid O, El Fiky L, Hassan O, Kotb A, El Fiky S. Anatomic variations of the sphenoid sinus and their impact on trans-sphenoid pituitary surgery. Skull Base. 2008;18(1):9–15. doi: 10.1055/s-2007-992764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tomovic S, Esmaeili A, Chan NJ, Shukla PA, Choudhry OJ, Liu JK, Eloy JA. High-resolution computed tomography analysis of variations of the sphenoid sinus. J Neurol Surg B Skull Base. 2013;74(2):82–902. doi: 10.1055/s-0033-1333619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohnen M. Radiological diagnosis of the paranasal sinuses. Radiologe. 2010;50(3):277–94. doi: 10.1007/s00117-009-1976-y. [DOI] [PubMed] [Google Scholar]
- 11.Unlu A, Meco C, Ugur HC, Comert A, Ozdemir M, Elhan A. Endoscopic anatomy of sphenoid sinus for pituitary surgery. Clin Anat. 2008;21(7):627–632. doi: 10.1002/ca.20707. [DOI] [PubMed] [Google Scholar]
- 12.Sandulescu M, Rusu MC, Ciobanu IC, Ilie A, Jianu AM. More actors, different play: sphenoethmoid cell intimately related to the maxillary nerve canal and cavernous sinus apex. Rom J Morphol Embryol. 2011;52(3):931–935. [PubMed] [Google Scholar]
- 13.Cavallo LM, Messina A, Cappabianca P, et al. Endoscopic endonasal surgery of the midline skull base: anatomical study and clinical considerations. Neurosurg Focus. 2005;19:E2. [PubMed] [Google Scholar]
- 14.Romano A, Z uccarello M, Van Loveren HR, Keller JT, Expanding the boundaries of the transsphenoidal approach: a micro anatomic study. Clin Anat. 2001;14:1–9. doi: 10.1002/1098-2353(200101)14:1<1::AID-CA1000>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 15.Sethi DS, StenleyRE PPK. Endoscopic anatomy of sphenoid sinus and sella turcica. J Laryngol Otol. 1995;109:951–955. doi: 10.1017/S0022215100131743. [DOI] [PubMed] [Google Scholar]
- 16.Sethi DS, Pilley PK. Endoscopic management of lesion of sella turcica. J Laryngol Otol. 1995;109(10):956–962. doi: 10.1017/S0022215100131755. [DOI] [PubMed] [Google Scholar]
- 17.Baldea V, Sandu OE. CT study of sphenoid sinus Pneumatization types. Rom J Rhinol. 2012;2(5):17–30. [Google Scholar]
- 18.Alam-Eldeen MH, et al. CT evaluation of pterygoid process pneumatization and the anatomic variations of related neural structures. Egypt J Radiol Nucl Med. 2018;49:658–662. doi: 10.1016/j.ejrnm.2018.03.011. [DOI] [Google Scholar]
- 19.Famurewa OC, et al. Sphenoid sinus pneumatization, septation, and internal carotid artery. A CT study Niger Med J. 2018;59(1):7–13. doi: 10.4103/nmj.NMJ_138_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thimmaiah VT, et al. Pneumatization patterns of onodi cell on multidetector computed tomography. J Oral Maxillofac Radiol. 2017;5(3):63–66. doi: 10.4103/jomr.jomr_3_17. [DOI] [Google Scholar]
- 21.Mikami T, et al. Anatomical variation in pneumatisation of anterior clinoid process. J Neurosurg. 2007;106:170–174. doi: 10.3171/jns.2007.106.1.170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data obtained from the available patient treatment record in record section of our Institute and images taken from the memory of the machine of the Institute.