Abstract
Most simulation models in rhinology are costly and are primarily meant to enhance endoscopic surgical skills. The present study aimed to construct a 3-dimensional model of the nose which is easily constructible with commonly available low cost plaster of Paris (POP) and assess its usefulness in training residents in basic transnasal procedures. A nose model was created using plaster of Paris and assessed for face and content validity by experts in rhinology while a construct validation was performed on five specified tasks by residents. All experts agreed with the resemblance of 10 of the 13 anatomical landmarks in the POP model and its utility in teaching basic transnasal procedures. There was a statistically significant difference in the time taken by I and III year residents in performing a diagnostic nasal endoscopy (p = 0.007), anterior nasal packing with polyvinyl alcohol tampon (p = 0.007), posterior nasal packing with Foley’s catheter (p = 0) and nasopharyngeal swabbing (p = 0.025). This study demonstrates the construct of a low cost 3-dimensional POP model and validates its utility in training residents in routine transnasal rhinological procedures. Face and content validation showed a high degree of resemblance to human anatomy with good agreement that this model could increase resident competency. The significant difference in time taken by residents at various levels of experience in performing rhinological procedures also confirmed a reliable construct validity. The described model could be an affordable and easily constructible alternative tool to other simulation models in otorhinolaryngology residency programs especially in developing countries.
Introduction
Teaching anatomy of human body has undergone dramatic changes over time with supervised learning and training methods for residents evolving from standard textbook 2D drawings and cadaver dissection to teaching in conjunction with animal models, physical 3D models and virtual reality (VR) simulation models on a computer. Physical models have been employed for training in various specialties of medicine like otolaryngology, gastroenterology, cardiology, urology etc. A thorough knowledge of the three-dimensional anatomy of the nose will minimize unnecessary trauma during a number of outpatient procedures like diagnostic nasal endoscopy, anterior and posterior nasal packing and nasopharyngeal swabbing. Technological advancements in the field of rhinology and endoscopic sinus surgery have provided access to the skull base and adjacent corridors with minimal morbidity via a transnasal endoscopic approach. All these make it important to master the art of maneuvering the endoscope through the narrow nasal passages while at the same time respecting vital neighboring structures.
Diagnostic nasal endoscopy, a central component of standard rhinological examinations requires a high level of technical proficiency with ambidexterity relying mainly on good coordination and integration of cognitive, clinical and technical skills. Good technical skills in nasal endoscopy also form a foundation in performing more complex sinus and skull base surgeries [1]. These skills can only be developed through hours of repeated practice and clinical experience [2, 3].
Various rhinology simulation models are available which are intended to train for more complex surgical procedures [2, 4–7]. These models are made from various materials like silicone [8], styrofoam [9] and 3D printing [7, 10]. Various simulation softwares have also been devised which provide real time haptic feedback system [11–13]. However, these simulators are costly due to their level of fidelity and complexity, and training using them is limited to very few centers around the world and therefore not a practical alternative for training basic skills required for diagnostic nasal endoscopy and routine rhinology office procedures. Some available low cost physical models do not resemble human anatomy and are more focused on skill training like endoscopic instrumentation [14]. Thus, there is a need for a more practical alternative that will allow residents develop their skills before they go on to perform diagnostic nasal endoscopy and other office procedures on patients in the clinic which will help improve patient safety and comfort.
We have attempted to design and create a three dimensional nose model by hand using plaster of Paris (POP). We hypothesize that our model promises to help train residents in understanding the three- dimensional anatomy of the nose and provide them with the required coordination and dexterity needed to perform routine outpatient rhinological procedures in a very efficient manner.
Methods
This was a prospective project done in a tertiary care teaching hospital to create a cost effective three-dimensional model of the human nose. The feasibility of using this model in training residents in routine rhinology outpatient procedures was assessed based on a 5-point Likert scale (1- strongly disagree, 2- disagree, 3- neutral, 4- agree, 5- strongly agree). The study was conducted after obtaining institutional review board (Christian Medical College) approval—IRB No. 13657.
Model Creation
A thermoplastic ray cast of the head used in radiation therapy was used as a template on which 12–14 layers of 6-inch POP roll, each layer 15 cm in length soaked in water was applied. Four custom cut cardboard templates were made separately for (1) dorsum of the nose, (2) floor of nasal cavity and nasal septum, (3) lateral nasal wall with inferior turbinate, middle turbinate, middle meatus, uncinate process and bulla ethmoidalis and (4) nasopharynx, torus tubarius and eustachian tube opening. These were then assembled onto the POP head cast (Figs. 1, 2 and 3). The model was made by 2 resident doctors over 4 hours.
Fig. 1.
Nose model components—Ray cast and cardboard templates
Fig. 2.

Construction of head template
Fig. 3.
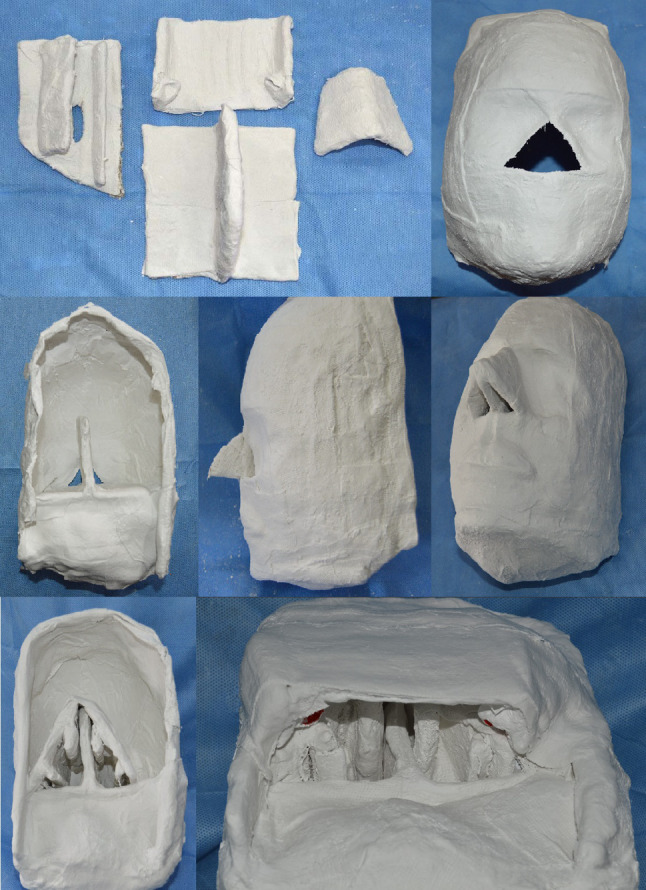
POP components and sequential assembly of nasal floor, septum, dorsum, lateral wall and nasopharynx
Validation
Five experts and 20 residents in otorhinolaryngology were recruited to assess the validity of the 3D POP nose model. The experts were professors and the residents were in their I, II and III year of training in otorhinolaryngology.
Face Validation
The face validity in this study was defined as the anatomical realism of the model based on experts’ review. The experts were asked to identify 13 anatomical landmarks (nasal septum, nasal floor, inferior meatus, inferior turbinate, middle turbinate, middle meatus, uncinate process, bulla ethmoidalis, hiatus semilunaris, nasopharynx, eustachian tube opening, torus tubarius and fossa of Rosenmuller) (Fig. 4). A 5-point Likert scale was used to evaluate the resemblance of these landmarks with actual anatomy.
Fig. 4.

Endoscopic view: a Inferior turbinate, inferior meatus, nasal floor and septum b nasopharynx, torus tubarius, eustachian tube orifice (marked red) c middle turbinate, middle meatus, uncinate process, hiatus semilunaris, bulla ethmoidalis, d) middle turbinate and sphenoethmoidal recess
Content Validation
The content validity was defined as the usefulness of the model with respect to training in basic outpatient rhinology procedures. The experts were asked to score the utility of the model in training to perform the following prespecified tasks on a 5-point Likert scale: (1) performing a systematic diagnostic nasal endoscopy including all 3 endoscopic passes and identification of individual structures, (2) anterior nasal packing with polyvinyl alcohol tampon, (3) anterior nasal packing with ribbon gauze, (4) posterior nasal packing with Foley’s catheter and (5) performing nasopharyngeal swabbing.
Construct Validation
Construct validity was defined as the ability to discriminate between users of differing experience. The performances between the operators with different levels of clinical experience were compared.
Participants, Setting and Tasks
20 residents from otorhinolaryngology attended a classroom session on the five prespecified tasks. A senior faculty member then demonstrated the procedures on the POP model after which the residents were required to perform the same independently. The number of attempts and time taken for each task was recorded. Their ability to perform the task and overall experience with the model were surveyed based on the 5-point Likert scale. For analysis scores 4 and 5 (agree and strongly agree) were considered as ‘agree’ and scores 1 and 2 (disagree and strongly disagree) as ‘disagree’.
Statistical Analysis
Statistical analysis was carried out using Stata I/C 16 software. The difference of time used in completing each task was analyzed by ANOVA test. The level of statistical significance was set at p < 0.05.
Results
All experts agreed on the resemblance of 10 of the 13 anatomical landmarks in the POP model to that of actual human anatomy while resemblance of the 3 remaining landmarks (fossa of Rosenmuller, hiatus semilunaris and uncinate process) were agreed upon by 4 of the 5 experts (Fig. 5). Majority of the experts agreed to the utility of the model in teaching basic transnasal procedures with all experts agreeing on its usefulness in teaching nasopharyngeal swabbing and accelerating the learning curve, improving the confidence, hand eye coordination and camera skills for performing nasal endoscopy (Fig. 6).
Fig. 5.
Bar diagram showing number of experts who “agree” to resemblance of various anatomical landmarks in 3D physical model to actual human anatomy
Fig. 6.
Content validation by expert questionnaire
The post graduate residents were asked to perform the various outpatient rhinological procedures and the time taken for each was noted. Systematic diagnostic nasal endoscopy with the various passes were completed by the I, II and III year residents in 59.8, 33.1 and 31.2 s respectively (Fig. 7). I year residents completed this task in an average of 1.8 attempts (range = 1–3, n = 8), while II and III year residents were able to perform this task accurately in a single attempt. There was a statistically significant difference in the time taken by I and III year residents in performing a systematic diagnostic nasal endoscopy (p = 0.007). A similar significant difference was observed between these two groups in performing other procedures like anterior nasal packing with polyvinyl alcohol tampon (p = 0.007), posterior nasal packing with Foley’s catheter (p = 0) and nasopharyngeal swabbing (p = 0.025). Even between the II and III year residents there was a statistically significant difference in the time taken in performing diagnostic nasal endoscopy (p = 0.002) and posterior nasal packing with Foley’s catheter (p = 0).
Fig. 7.
Bar diagram showing average time taken by residents for performing each task
In a post procedure questionnaire based survey, majority of the residents felt that the POP model provided them an enjoyable experience, accelerated their learning curve in developing the right techniques and enhanced their skills and confidence in performing basic rhinological outpatient procedures (Fig. 8).
Fig. 8.
Post training resident satisfaction score
Discussion
A number of simulation models have been identified in rhinology training ranging from synthetic, computer-based, 3D printing, animal cadaver, and hybrid models. Majority of these models described are used to enhance overall endoscopic sinus and skull base surgery skills. Our nose model was primarily meant to develop skills in performing basic outpatient rhinology procedures. Made with easily available POP, the model was created in only four hours by two resident doctors and costed only 10$ (INR 700). A 3D printed sinus and skull base model for endoscopic surgical training created by Tsung-yen Hsieh costed $800 and took more than 19 hours for construction [15]. Chen Zhuo et al. devised a 3D printed nasal cavity and sinus model using thermoplastic polyurethane elastomer (TPU) and polylactic acid (PLA) which took 24 hours for construction and costed around $15 [16]. A number of low cost simulation models have also been developed but were mainly meant to enhance endoscopic surgical skills [8, 9, 17]. A model with a lower cost will be more accessible to a wider number of institutions with different sized budgets, which in turn can lead to its more widespread adoption.
The described model showed good face and content validation and agreement by the experts that this model could be used to train residents and increase resident competency. Construct validity in our model also showed a significant difference in the time taken by residents at various levels of experience and training in performing the prespecified outpatient rhinological procedures except for anterior nasal packing with ribbon gauze because of the large variability in the time taken among the same year residents.
The nasal cavity is an enclosed structure lined by highly sensitive and vascularized mucosa and having close proximity to critical structures. A high level of precision and knowledge regarding its three-dimensional anatomy is required to perform routine outpatient based rhinology procedures safely without trauma and patient discomfort. While textbooks and atlases provide two-dimensional (2D) illustrations, they are of limited value in understanding the spatial relations to adjacent structures. Endoscopic procedures being performed in the narrow confines of the nose require greater dexterity and hand eye coordination. Physical 3D models provide the residents an opportunity to develop a better understanding of the anatomy, improve their ergonomic skills and dexterity and thus form a strong foundation before embarking on complex endoscopic procedures on patients. Incorporation of these models in training programs provides a safe environment for residents to rehearse and learn from their mistakes thus enhancing patient care. A survey by the American rhinology society showed that majority of the training programs observed improved surgical skills and knowledge after simulation training [18]. However, the limited availability and increased costs were barriers to its widespread use in many countries.
Alwani et al. conducted a systematic review of various simulation models that have proven beneficial in otolaryngology training programs [19]. Of the many simulation models, 17 were identified in rhinology and were mainly used for enhancing skills in endoscopic sinus surgery. Leung et al. created a non-biologic sinus surgery task trainer using readily available components focusing on increasing hand-eye coordination and endoscope handling skills [9]. The ES3 virtual reality sinus surgery simulator validated by Fried et al. included a cognitive component that was coupled with surgical practice [20]. However, virtual reality systems have not reached mainstream use due to high cost, reduced availability and maintenance requirements.
The limitation of our model is that it can be used only for basic diagnostic endoscopy and transnasal outpatient procedures training and cannot be subjected to drilling, tissue removal exercises or targeted injections.
Our nose model is the first in world literature to be made from POP. The main advantage of this model is that it is easily constructible using commonly available low cost material, avoids the sophistication of software, expensive hardware and is maintenance free. The model serves as a trainer to teach basic endoscopy skills and enhance the technical expertise to perform routine outpatient rhinology procedures in a safe environment before carrying out these procedures on patients and embarking on more complex endonasal procedures.
Conclusion
The described POP nose model serves as a good low cost alternative to 3D printed expensive physical models with anatomical realism. In countries or institutions where 3D printed models are not easily available or acquirement is limited due to high cost, this POP model can be easily constructed with a much lower cost. Given the good face and content validation and high user satisfaction score, this model provides the potential to be incorporated in otorhinolaryngology residency programs worldwide especially in developing countries.
Acknowledgements
We would like to thank all the faculty and residents in the Department of ENT for their participation and encouraging support towards this project. We would also like to thank Dr B.Antonisamy for his kind input towards the statistical analysis.
Author Contribution
Dr. RRB: Concept and Design, Methodology, Data acquisition and analysis, Literature search, Statistical analysis, Manuscript preparation, Manuscript review &final approval, accountable for all aspects of the work. Dr LV: Concept and Design, Methodology, Data acquisition & analysis, Literature search, Manuscript preparation, Manuscript editing, Manuscript review &final approval, accountable for all aspects of the work. Dr RK: Concept and Design, Methodology, Data acquisition and analysis, Literature search, Manuscript preparation, Manuscript editing, Manuscript review and final approval, accountable for all aspects of the work.
Funding
This project received no financial support.
Data Availability
The datasets generated during and analysed during the current study are available from the corresponding author on request.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Consent to participate
All participants consented to be part of the study.
Ethical Approval
Institutional review board approval was obtained prior to the commencement of the study (IRB No. 13657).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sgambatti Celis L, Gil Melcón M, Franco Calvo F, et al. Complications of endoscopic Sinus surgery in a residency training program. Acta Otorrinolaringol. 2010;61:345–350. doi: 10.1016/j.otorri.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Ooi EH, Witterick IJ. Rhinologic surgical training. Otolaryngol Clin North Am. 2010;43:673–689. doi: 10.1016/j.otc.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 3.Marks SC. Learning curve in endoscopic sinus surgery. Otolaryngol Head Neck Surg. 1999;120:215–218. doi: 10.1016/S0194-5998(99)70409-2. [DOI] [PubMed] [Google Scholar]
- 4.Wiet GJ, Stredney D, Wan D. Training and simulation in otolaryngology. Otolaryngol Clin North Am. 2011;44:1333–1350. doi: 10.1016/j.otc.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arora A, Lau LY, Awad Z, Darzi A, Singh A, Tolley N. Virtual reality simulation training in Otolaryngology. Int J Surg. 2014;12:87–94. doi: 10.1016/j.ijsu.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 6.Varshney R, Frenkiel S, Nguyen LH, et al. The McGill simulator for endoscopic sinus surgery (MSESS): a validation study. J Otolaryngol Head Neck Surg. 2014;43:40. doi: 10.1186/s40463-014-0040-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Narayanan V, Narayanan P, Rajagopalan R, et al. Endoscopic skull base training using 3d printed models with pre-existing pathology. Eur Arch Otorhinolaryngol. 2015;272:753–757. doi: 10.1007/s00405-014-3300-3. [DOI] [PubMed] [Google Scholar]
- 8.Burge SD, Bunegin L, Weitzel EK, McMains KC. The validation of an endoscopic sinus surgery skills training model: A pilot study. Am J Rhinol Allergy. 2012;26:409–413. doi: 10.2500/ajra.2012.26.3798. [DOI] [PubMed] [Google Scholar]
- 9.Leung RM, Leung J, Vescan A, Dubrowski A, Witterick I. Construct validation of a low-fidelity endoscopic sinus surgery simulator. Am J Rhinol. 2008;22:642–648. doi: 10.2500/ajr.2008.22.3245. [DOI] [PubMed] [Google Scholar]
- 10.Alrasheed AS, Nguyen LHP, Mongeau L, Funnell WRJ, Tewfik MA. Development and validation of a 3d-printed model of the ostiomeatal complex and frontal sinus for endoscopic sinus surgery training. Int Forum Allergy Rhinol. 2017;7:837–841. doi: 10.1002/alr.21960. [DOI] [PubMed] [Google Scholar]
- 11.Dharmawardana N, Ruthenbeck G, Woods C, et al. Validation of virtual-reality-based simulations for endoscopic sinus surgery. Clin Otolaryngol. 2015;40:569–579. doi: 10.1111/coa.12414. [DOI] [PubMed] [Google Scholar]
- 12.Edmond CV., Jr Impact of the endoscopic sinus surgical simulator on operating room performance. Laryngoscope. 2002;112:1148–1158. doi: 10.1097/00005537-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Tolsdorff B, Pommert A, Hohne KH, et al. Virtual reality: A new paranasal sinus surgery simulator. Laryngoscope. 2010;120:420–426. doi: 10.1002/lary.20676. [DOI] [PubMed] [Google Scholar]
- 14.Malekzadeh S, Pfisterer MJ, Wilson B, Na H, Steehler MK. A novel low-cost sinus surgery task trainer. Otolaryngol Head Neck Surg. 2011;145:530–533. doi: 10.1177/0194599811413373. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh TY, Cervenka B, Dedhia R, Strong EB, Steele T. Assessment of a patient-specific, 3-dimensionally printed endoscopic sinus and skull base surgical model. JAMA Otolaryngol Head Neck Surg. 2018;144:574–579. doi: 10.1001/jamaoto.2018.0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhuo C, Lei L, Yulin Z, et al. Creation and validation of three-dimensional printed models for basic nasal endoscopic training. Int Forum Allergy Rhinol. 2019;9:695–701. doi: 10.1002/alr.22306. [DOI] [PubMed] [Google Scholar]
- 17.Wais M, Ooi E, Leung RM, et al. The effect of low-fidelity endoscopic sinus surgery simulators on surgical skill. Int Forum Allergy Rhinol. 2012;2:20–26. doi: 10.1002/alr.20093. [DOI] [PubMed] [Google Scholar]
- 18.Chen PG, Chang DR, Weitzel EK, Peel J, Chandra RK, McMains KC. The role of simulation in teaching sinus surgery in otolaryngology residency: A survey of rhinologists. Allergy Rhinol. 2016;7:244–248. doi: 10.2500/ar.2016.7.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alwani M, Bandali E, Larsen M, Shipchandler T, Ting J. Current state of surgical simulation training in otolaryngology: systematic review of simulation training models. Arch Otorhinolaryngol Head Neck Surg. 2019;3:5. doi: 10.24983/scitemed.aohns.2019.00109. [DOI] [Google Scholar]
- 20.Fried MP, Sadoughi B, Gibber MJ, et al. From virtual reality to the operating room: the endoscopic sinus surgery simulator experiment. Otolaryngol Head Neck Surg. 2010;142:202–207. doi: 10.1016/j.otohns.2009.11.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and analysed during the current study are available from the corresponding author on request.







