Abstract
We sought to explore the frequency of stress among OPD attending Kashmiri public diagnosed as muscle tension dysphonia (MTD) and determine the subjective consequences of voice therapy in management of muscle tension dysphonia. 72 subjects that attended to ENT and HNS OPD with change of voice were prospectively evaluated and also underwent an extensive otolaryngological examination. Patients identified as MTD were provided a questionnaire which was split into 3 parts: First part dealt with the identification of the subject (age, geography, gender, profession) and also provided evaluation of perceived anxiety using Perceived Stress Scale-10. In the next part the individuals needed to assess their vocal quality based on parameters of GRBAS 4-point score scale before and also after the treatment. In the final component the subjects also needed to answer the VHI-10 (Voice Handicap Index) and also the outcome was compared with those acquired at the assessment before the beginning of the treatment. The mean age of the cohort was 30.31 ± 07.43 (age range, 12–71) and every subject was an indigenous Kashmiri. As expected, vast majority of subjects were females (43 patients). In the pooled information set, women had numerically higher PSS-10 scores than males. For women, the typical stress score was M = 18.6 and for men the average stress score was M = 16.65. In a healthy population, the typical PSS stress score is described to be 13.7 (SD = 6.6) for women and 12.1 (SD = 5.9) for men. At the Wilcoxon test for paired data, we observed a significant difference between the VHI pretreatment (mean = 19.7) and VHI post-treatment, that's at time of the research (mean = 9.73; P = 0.017). The grade (G) was assessed in terms of improvement of the vocal quality as opposed with before treatment and also the individuals demonstrated a high level of satisfaction (mean = 0.65). When looking at roughness (R) as well as breathiness (B), the individuals remember that their speech is seldom rough (mean = 0.62) and also less breathy (median = 0.44). Patients likewise noted improvement in other variables of GRBAS scale. Stress is persistent, pervasive and nearly unavoidable in contemporary life. The decades old perplexing and mind baffling pandemonium hovering around the Kashmiri population has had a tremendous impression on the psychological development of people in this region. A careful conclusion is the fact that emotional stress might play a major role in the upkeep of MTD. MTD has to be approached in a multidisciplinary environment in which closer cooperation between a laryngologist, a speech language pathologist and also a psychologist is likely.
Keywords: Muscle tension dysphonia, Stress, Speech therapy, GRBAS, VHI, PSS-10
Introduction
An individual's voice is actually a sensitive marker of thoughts, demeanors, and role assumptions. Communication skills are actually of essential significance for holding on with a fruitful existence. Regardless of the increasing value of e-mails, text messages as well as chat messengers, the capability to discuss and express thoughts by medium of speech is actually paralleled by none various other means of communication. Without having a question, in present day society people are actually likely much more subject to their voice than in the rustic community orders of old. Approximately one third of the functioning populace nowadays require the voice of theirs to procure cash [1].
Over 40% of dysphonic individuals presenting to a vocal clinic or ENT operating surgeon have no identifiable organic or mucosal disease [2]. What, decisively, establishes muscle tension dysphonia is actually vague. Certain resources have portrayed it to be a grouping of vocal indications joined up with explicit glottic as well as supraglottic compression designs [3–6].
Muscle tension dysphonia (MTD) is actually a problem normally seen in middle-aged and young females. It's recognized by an imbalance of the synergist as well as antagonist muscles impacting the vocal fold position and tensioning relative to rest of vocal tract. This substantial muscle activity has been linked to a lot of sources, including psychological and/or personality factors which are likely to cause tension [7, 8]. Of take note, stress in individuals with MTD has been anecdotally claimed to have far more to do with day to day anxieties as compared to with frank psychiatric problems [9].
No matter the origin, individuals with muscle tension voice disorders typically complain of neck as well as shoulder tightness, extra vocal work, and exhaustion, with symptoms intensifying with extensive voice use. Voice quality symptoms are able to differ in type and severity, which range from severely pressed to excessive breathiness with myriad combinations [3–7, 10].
The diagnosis is not constantly obvious amid the primary connection with the patient; some percentage of the difficulty is based on the distinctive appearances of this particular voice issue. Additionally, people will generally abstain from discussing their enthusiastic clashes, notwithstanding when again and again dealt with, mirroring an underlying defense from the relationship of the physical symptoms with extreme subject matters. Another concern in affirming the realization of psychogenic dysphonia is actually the need to refuse various maladies that could show relative vocal symptoms, for example acute infectious illnesses, vocal cord paralysis, spasmodic dysphonia, and then neuromuscular diseases [11–13].
In the specific situation of functional dysphonia, Carding et al. [14] and MacKensie et al. [15] have nicely identified the role of speech therapy within the healing of vocal pathologies. Vocal therapy is actually regarded as the pioneer method of therapy in MTD [14, 15], which requires various therapeutic techniques [16, 17], like rest, yawn-sign, chewing, as well as laryngeal muscle tissue tension reduction [2, 18–20]. The working hypothesis is the fact that when muscle tension of the phonatory mechanism decreases, the vertical position of this larynx lowers which in turn enhances the voice quality.
There's consensus that if emotional and psychological factors which initiated, exacerbated, or perhaps maintained MTD aren't addressed the possibility of long-term therapy efficacy decreases even if short-term success is actually attained for the patient [5, 9, 21–25].
The present study represents an initial stage in a long-term research program which is designed to look at the mechanisms by what stress may affect voice, and the role of voice therapy as a treatment modality concentrating on these mechanisms. We made utilization of this individual’s instinctive awareness and understanding of what they thought of the treatment, altogether examining their response towards the quality of vocal impairment following the therapy and exactly how they felt on the subject of the impacts of therapy. The awareness of theirs and perception concerning the quality of breathing and roughness after the treatment was also conceived.
Aims and Objectives
To investigate the frequency of stress among individuals diagnosed with muscle tissue tension dysphonia.
To determine the subjective consequences of voice therapy in the management of muscle tension dysphonia.
Material and Methods
This prospective study included 72 individuals of the two genders, and all age groups, with a diagnosis of muscle tension dysphonia addressed inside the ENT OPD of Government Medical College, J&K, Srinagar, India from January 2016 to December 2018. Duration of symptoms ranged from six months to seven years. The subject matter incorporated vocal professionals (singers, hawkers, and teachers) and non-professionals (students, housewives, businessmen).
All participants were native Kashmiri speakers with everyday discourse as well as dialect aptitudes. None of them had hearing defects or any velopharyngeal or neurologic variants from the majority. All participants had been examined by an ENT operating surgeon ahead of the involvement of theirs in the study. Besides, an audiogram was done to refuse any severe hearing imperfections. Participants were excluded in the event that they'd acute or chronic upper respiratory infection at the time of tests and a previous history of cardiac, pulmonary, or perhaps neurologic issues. Participants had been integrated on the off possibility that they utilized Kashmiri as the essential local dialect of theirs, had not as of now taken speech therapy sessions, had normal laryngeal system with no record of laryngeal surgery, as well as had no history of swallowing problems. Written informed consent was taken from all of the participating patients.
Patients had been continually enlisted in the study, and after diagnosis, affirmation was acquired by way of a multidisciplinary analysis by an otorhinolaryngologist, psychologist, as well as speech specialist. All individuals finished the institutionalized appraisal convention for voice conditions within the clinic plus underwent a videolaryngostroboscopy, psychological evaluations and voice therapy. The videolaryngostroboscopy was performed by same otorhinolaryngologist, utilizing a rigid telescope (70◦, 8 mm; Asap Germany).
Demographic data and relevant history (age, sex, place, occupation) was collected from the subjects. The characteristics, evolution and duration of vocal symptoms, as well as videolaryngostroboscopy results were also recorded. Individuals had been identified as having MTD if they'd a history of dysphonia for ≥ 3 months and also had no proof of structural abnormality, spasmodic dysphonia, or puberphonia on fiberoptic laryngoscopy as well as videostroboscopy (i.e. carcinoma,polyp,nodules,papilloma,laryngitis,paralysis). Any suspected psychoemotional disorder associated with the picture of dysphonia was established in the psychological and speech therapy appraisals [11, 26].
After diagnosis was established, the multidisciplinary treatment (psychotherapy as well as vocal treatment) was initiated in all individuals. All individuals underwent a vocal therapy based mostly on vocal hygiene and also exercises dealing with the resonance, respiratory, as well vibratory mechanisms. Individuals were additionally subjected to behavioral counseling sessions.
All individuals were followed up for 3 months within outpatient clinics after discharge from psychological and voice therapy and presented no symptom recurrence during this particular period.
Procedure
Subjects had been provided a questionnaire which was split into 3 parts:
First component dealt with the assessment of perceived stress using Perceived Stress Scale-10 [27].
Second part dealt with the evaluation of vocal quality of the subjects based on parameters of GRBAS 4-point rating scale (Grade, Roughness, Breathiness, Asthenia, Strain), each one graded on a rating scale of 0–3 (0-normal; 1-slight; 2-moderate; 3-severe), previously as well as after the treatment [17].
In the third portion, the subjects also had to reply to the VHI-10 (Voice Handicap Index) and also the results were compared to those recorded at the evaluation before the beginning of the therapy [28].
The individuals had a duration of therapy ranging from three weeks to three months having a median of 2.5 months. The duration of the therapy was adapted to each and every patient's capacity and need to absorb the vocal techniques taught. The time elapsed between the conclusion of the treatment and the time of the study ranges from three months to six months with a median of four months. The study wasn't carried out with the goal to check out the association between the severity of individual's voice disorders and the summative scores on stress.
Ethical clearance was obtained from institutional ethical committee.
Results
The mean age of this cohort was 30.31 ± 07.43 (age range, 12–71) and all of them were indigenous Kashmiris. As expected, vast majority of subjects were females (60%) as in comparison with males which comprised 40% of the study population. Male: Female ratio was 1:1.4.
In both sexes, majority of patients belonged to age group between 16 to 30 years (40.2%) followed by age group between 31 and 45 years of age (23.6%) (Fig. 1).
Fig. 1.

Age wise distribution of patients with MTD
Majority of patients were females (60%) as compared to males which comprised 40% of the study population (Fig. 2).
Fig. 2.
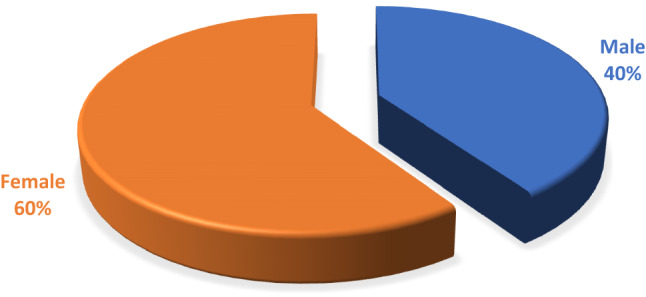
Sex wise distribution of patients with MTD
Out of total 72 patient’s more than half of patients (54%) were from rural areas while (46%) of patients were from urban areas (Fig. 3).
Fig. 3.
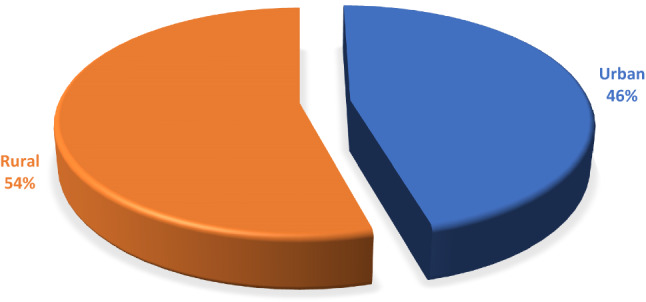
Area wise distribution of patients with MTD
Females had numerically larger PSS-10 scores than males. For females, the average stress score was M = 18.6 as well as for males the average stress score was M = 16.65. It's apparent from the pooled data set that stress scores were considerably higher for individuals with MTD as compared to for the healthy population. Also, scores were much higher in females as compared to men (Fig. 4).
Fig. 4.
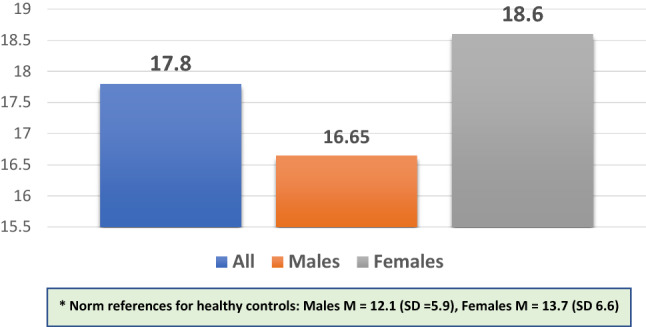
Perceived Stress Scale-10 scores
VHI values pre- and post-treatment are shown in Fig. 5. Results showed statistically significant reduction in the mean VHI scores across subject with MTD (significant at P < 0.05).
Fig. 5.
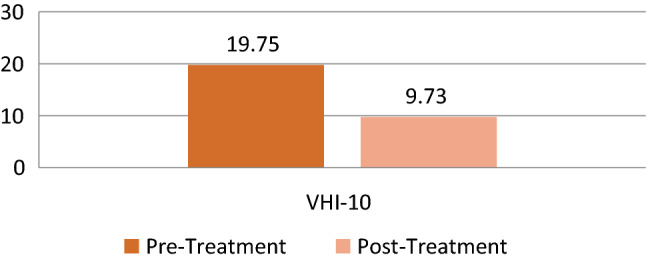
Pre- and post-treatment VHI-10 scores
GRBAS (Perceptual Rating of Voice Quality)
The outcomes for all 5 of the GRBAS (perceptual rating of vocal quality) parameter values pre and post treatment are shown in Fig. 6. The P value was estimated using the Wilcoxon signed rank test. These perceptual parameters clearly show a statistically significant improvement in subjects with MTD after voice therapy (P < 0.05).
Fig. 6.
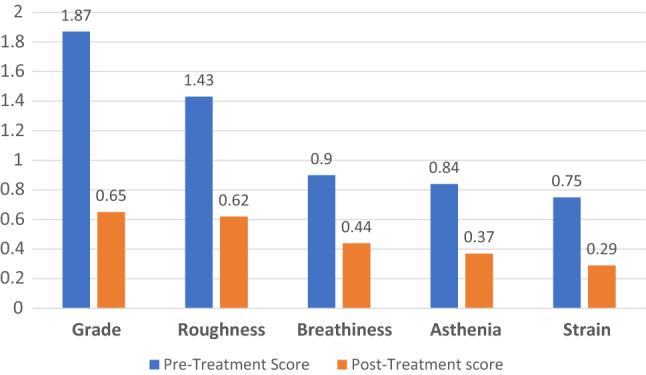
Pre- and Post-treatment GRBAS scores
Discussion
Muscle tension dysphonia is regarded as a functional speech disorder, as you can find no structural laryngeal lesions or neurological alterations specifically associated with the apparent vocal symptoms [11, 21, 26].
Muscle tension dysphonia has been mentioned to be highly predominant in women [11, 26], as we discovered in this specific study. Women are actually the unrecognized frontline fighters that, if recognized, may expose an alternative reality by presenting a unique voice along with a revisionist discourse to be heard. Female's psychosocial and physical wellness as well as survival are consequently essential to the well-being of kids, both during as well as after armed conflict.
Research indicates that females in conflict areas tend to be more susceptible compared to males to depression, post-traumatic stress disorder (PTSD), along with other psychopathologies [28].
Women’s duties in a conflict zone are actually formidable. They hold communities and families together through the key roles of theirs in food production, economic activities, caring for other family members and children and they act to sustain the social order [29, 30].
It may be argued that dysphonia is actually grounded in the origin of muscle tension, that is not really a perceived and observable mechanism but just as a result of an inappreciable as well as imperfect vocal kinesis as well as gesticulations. The associated complex mental state of affairs is the primary barrier in the patient's treatment and analysis. The patient's own perception hindering the treatment.
Remodeling the vocal bearing as well as response was the primary goal of the treatment. The goal of the research was to evaluate the long-term effectiveness of the individuals being treated for muscle tension dysphonia. Patients own personal sense of total satisfaction with regard to other issue that he feels bothered the voice of his in terms of effectiveness and quality, has been evaluated as ways of success in therapy.
In our study, the multidisciplinary approach is actually thought to be the key element to good results and good evolution in all cases. Treatment is actually protracted, strenuous, and difficult in individuals reluctant to psychotherapy, requiring energy, discipline, and determination by both therapist and patient.
Sudhir et al. and Baker reinforced the value of a multidisciplinary approach in psychogenic dysphonia, emphasizing it's essential to recognize the complicated association between neuropsychological, intrapsychological, and interpersonal actions that impact these patients [31, 32].
Van Lierde et al. made a study on the long-term efficacy of vocal therapy in individuals with hyper functional dysphonia and they also discovered that six years after treatment, the objective measurements (video and acoustical laryngostroboscopy) are actually sometimes stable or perhaps aggravated and that 51% of the individuals continue to have a pathological larynx. Despite this, they don't view a strong psychosocial effect of the vocal problem as expressed by the VHI [16].
Only subjective parameters were used in this specific study to evaluate the reaction to voice therapy in individuals with muscle tension dysphonia. The parameters we used to assess vocal quality are actually influenced from GRBAS scale [17]. We noted considerable improvement in all of the parameters of GRBAS scale. These perceptual parameters show a statistically significant (P < 0.05) improvement in subjects with MTD after voice therapy. Similar results have been concluded by Morsomme et al. [33].
With the consideration of being succinct, we chose to make use of the VHI-10 to evaluate the vocal impairment. Evaluating the handicap related for dysphonia has been proven to be dependable with VHI [28]. We observed a major distinction between the outcomes of pretreatment VHI-10 (19.75) as well as the post treatment VHI-10 (9.73). We realize that there's no consensus in the literature on the required reduction of the score to signify an enhancement in vocal disability. The outcome of the pretreatment VHI-10 corresponds to the importance which has been discovered earlier in the affected person group' muscle tension dysphonia [34]. The consequence of the post treatment VHI-10 may be viewed as higher when compared with the median of 1 obtained by the controls in Rosen's study [34]. What this means is that our people continue to have a vocal impairment that's inferior to the normophonic public, although they find the therapy to achieve success and believe that the overall level of their vocal quality has improved.
Speyer et al. show that the objective changes of the vocal quality just play a small role in the subjective perception of the patient. Possibly the individual doesn't perceive the improvement or maybe he thinks that his voice has improved although there are actually no measurable objective changes [17, 35, 36].
Because of the small sample we should be careful with the findings; nonetheless, we trust they provide the present state of research with results that are interesting.
Conclusion
Stress in modern life is overwhelming, constant and almost inevitable. Mental and emotional stress compounded with apprehension, have long been designated as the issues of the fairer sex, thus inviting research in this area corroborated by additional decrees and directives. Women often suffer more from this psychological burden than men due to violent politics and patriarchal demands.
The decades old perplexing and mind baffling pandemonium hovering around the Kashmiri population has had a tremendous impression on the psychological development of people in this region. In conflict-ridden Kashmir, the psychological impact of living in the politically conflict-ridden zone can be minimized by voice therapy.
A cautious conclusion is actually that stress might play a major role in the upkeep of MTD. MTD has to be approached in a multidisciplinary environment in which close cooperation between a laryngologist, a speech language pathologist as well as a psychologist is actually possible.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ihsan Ali, Email: dralisan@gmail.com.
Raj Tajamul Hussain, Email: raj.tajamul@gmail.com.
References
- 1.Vilkman E. Voice problems at work: a challenge for occupational safety and health arrangement. Folia Phoniatr Logop. 2000;52:120–125. doi: 10.1159/000021519. [DOI] [PubMed] [Google Scholar]
- 2.Koufman JA, Blalock PD. Functional voice disorders. Otolaryngol Clin North Am. 1991;24:1059–1073. doi: 10.1016/S0030-6665(20)31068-9. [DOI] [PubMed] [Google Scholar]
- 3.Morrison MD, Nichol H, Rammage LA. Diagnostic criteria in functional dysphonia. Laryngoscope. 1986;94:1–8. doi: 10.1288/00005537-198601000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Morrison MD, Rammage LA, Gilles ME, Pullan CB, Hamish N. Muscular tension dysphonia. J OtolaryngoI. 1983;12:302–306. [PubMed] [Google Scholar]
- 5.Morrison MD, Rammage L. Muscle misuse voice disorders: description and classification. Acta Otolaryngol (Stockh) 1993;113:428–434. doi: 10.3109/00016489309135839. [DOI] [PubMed] [Google Scholar]
- 6.Koufman JA, Blalock PD. Classification and approach to patients with functional voice disorders. Ann Otol Rhinol Laryngol. 1982;91:372–377. doi: 10.1177/000348948209100409. [DOI] [PubMed] [Google Scholar]
- 7.Aronson AB. Clinical voice disorders: an interdisciplinary approach. 3. New York, NY: Thieme; 1990. [Google Scholar]
- 8.Rammage LA, Nichol H, Morrison MD. The psychopathology of voice disorders. Hum Commun Canada. 1987;11:21. [Google Scholar]
- 9.Seifert E, Kollbrunner J. Stress and distress in non-organic voice disorders. Swiss Med Wkly. 2005;57:584–594. doi: 10.4414/smw.2005.10346. [DOI] [PubMed] [Google Scholar]
- 10.Greene M, Mathieson L. The voice and its disorders. 5. London, England: Whurr; 1989. [Google Scholar]
- 11.Schalén L, Andersson K, Eliasson I. Diagnosis of psychogenic dysphonia. Acta Otolaryngol Suppl. 1992;492:110–112. doi: 10.3109/00016489209136824. [DOI] [PubMed] [Google Scholar]
- 12.Andersson K, Schaltn L. Etiology and treatment of psychogenic voice disorder: results of a follow-up study of thirty patients. J Voice. 1998;12:96–106. doi: 10.1016/S0892-1997(98)80081-7. [DOI] [PubMed] [Google Scholar]
- 13.Baker J. Psychogenic voice disorders—heroes or hysterics. A brief overview with questions and discussion. Logoped Phoniatr Vocol. 2002;27:84–91.6. doi: 10.1080/140154302760409310. [DOI] [PubMed] [Google Scholar]
- 14.Carding PN, Horsley IA, Doherty GJ. A study of the effectiveness of voice therapy in the treatment of 45 patients with nonorganic dysphonia. J Voice. 1999;13(1):72–104. doi: 10.1016/S0892-1997(99)80063-0. [DOI] [PubMed] [Google Scholar]
- 15.MacKensie K, Millar A, Deary IJ, Wilson JA. Does voice therapy work? A randomized controlled trial of the efficacy of voice therapy for dysphonia. Clin Otolaryngol Allied Sci. 1999;14(4):377. doi: 10.1046/j.1365-2273.1999.00254-9.x. [DOI] [Google Scholar]
- 16.Van Lierde KM, Claeys S, De Bodt M, van Cauwenberg P. Long-term outcome of hyperfunctionnal voice disorder based on a multiparameter approach. J Voice. 2007;21(2):179–188. doi: 10.1016/j.jvoice.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Speyer R, Wieneke GH, van Wijck-Warnaar I, Dejonckere PH. Effects of voice therapy on the voice range profiles of dysphonic patients. J Voice. 2003;17(4):544–566. doi: 10.1067/S0892-1997(03)00079-1. [DOI] [PubMed] [Google Scholar]
- 18.Mathieson L. Voice treatment: the wider perspective. Speech Therapy Prac. 1989;5(5):6–8. [Google Scholar]
- 19.Ruotsalainen JH, Sellman J, Lehto L, et al. Interventions for treating functional dysphonia in adults. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD006373.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Ramig LO, Verdolini K. Treatment efficacy: voice disorders. J Speech Lang Hear Res. 1998;41:S101–S116. doi: 10.1044/jslhr.4101.s101. [DOI] [PubMed] [Google Scholar]
- 21.Roy N. Functional dysphonia. Curr Opin Otolaryngol Head Neck Surg. 2003;11:144–148. doi: 10.1097/00020840-200306000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Roy N, Bless DM, Heisey D. Personality and voice disorders: a superfactor trait analysis. J Speech Lang Hear Res. 2000;43:749–768. doi: 10.1044/jslhr.4303.749. [DOI] [PubMed] [Google Scholar]
- 23.Butcher P, Elias A, Raven R, Yeatman J, Littlejohns D. Psychogenic voice disorder unresponsive to speech therapy: psychological characteristics and cognitive behavior therapy. Br J Disord Commun. 1987;22:81–92. doi: 10.3109/13682828709088690. [DOI] [PubMed] [Google Scholar]
- 24.Günther V, Mayr-Grafl A, Miller C, Kinzl H. A comparative study of psychological aspects of recurring and non-recurring functional aphonias. Eur Arch Otorhinolaryngol. 1996;253:240–244. doi: 10.1007/BF00171135. [DOI] [PubMed] [Google Scholar]
- 25.Roy, Bless DM, Heisey D, Ford CN. Manual circumlaryngeal therapy for functional dysphonia: an evaluation of short- and long-term treatment outcomes. J Voice. 1997;11:321–331. doi: 10.1016/S0892-1997(97)80011-2. [DOI] [PubMed] [Google Scholar]
- 26.Behlau M, Azevedo R, Pontes P, Brasil O. Disfonias funcionais. In: Belhau MA, editor. voz. O livro do especialista. Revinter: Rio de Janeiro; 2001. pp. 247–294. [Google Scholar]
- 27.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- 28.Karam EG. Women and the Lebanon wars: depression and post-traumatic stress disorder. In: Shehadeh L, editor. Women and War in Lebanon. Miami: University Press of Florida; 1999. [Google Scholar]
- 29.Bennett O, Bexley J, Warnock K, editors. Arms to protect, arms to fight: women speak out about conflict. London: Panos; 1995. [Google Scholar]
- 30.UN . Platform for action. New York: Author; 1995. [Google Scholar]
- 31.Sudhir PM, Chandra PS, Shivashankar N, Yamini BK. Comprehen-sive management of psychogenic dysphonia: a case illustration. J Commun Disord. 2009;42(305–12):16. doi: 10.1016/j.jcomdis.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 32.Baker J. Persistent dysphonia in two performers affecting the singing and projected speaking voice: a report on a collaborative approach to management. Logoped Phoniatr Vocol. 2002;27:179–187. doi: 10.1080/140154302762493234. [DOI] [PubMed] [Google Scholar]
- 33.Morsomme D, de la Bardonnie MF, Verduyckt I, Jamart J, Remacle M. Subjective evaluation of the long-term efficacy of speech therapy on dysfunctional dysphonia. J Voice. 2010;24(2):178–182. doi: 10.1016/j.jvoice.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Rosen CA, Murry Th, Zinn A, Zullo Th, Sonbollian M. Voice Handicap Index change following treatment of voice disorders. J Voice. 2000;14(4):619–623. doi: 10.1016/S0892-1997(00)80017-X. [DOI] [PubMed] [Google Scholar]
- 35.Speyer R, Wieneke GH, Dejonckere PH. Self-assessment for chronic dysphonia. Clin Otolaryngol. 2003;29:66–74. doi: 10.1111/j.1365-2273.2004.00782.x. [DOI] [PubMed] [Google Scholar]
- 36.Speyer R, Wieneke GH, Dejonckere PH. Documentation of progress in voice therapy: perceptual, acoustic, and laryngostroboscopic findings pretherapy and posttherapy. J Voice. 2004;18(3):325–340. doi: 10.1016/j.jvoice.2003.12.007. [DOI] [PubMed] [Google Scholar]


