Abstract
Garcin’s Syndrome is a rare pathology involving multiple cranial nerves in the setting of invasive mucormycosis, usually in immunocompromised patients. Owing to its extremely high mortality rate, clinician should have a high suspicion for diagnosis. This article presents a rare case of Rhino-Orbito-Cerebral Mucormycosis with Garcin’s syndrome in a 33-years old male along with a discussion of previously reported cases. The case is discussed in light of scant contemporary literature on the cited subject. A thorough search using the keywords Garcin's Syndrome, Invasive Mucormycosis, Rhino-orbital, Rhino-cerebral mucormycosis, was conducted on Pubmed/MEDLINE, Google scholar, LILACS, medRxiv and Google. A total of six reported cases found in international literature published between 2000 and 2020 were reviewed and analyzed. Garcin’s Syndrome is associated with a high mortality rate. In our review, of the total seven patients, only three survived, bringing the collective mortality to 42.85%. Patients had multiple cranial nerve involvement leading to long term sequelae. Our case showed the unique finding of VIII nerve involvement. Early intervention helped in patient survival and better functional outcome. This literature review highlights the distinct clinical nature of the presentation of disease and the importance of prompt diagnosis and early management in the reversal of complications in an otherwise potentially fatal disease.
Keywords: Garcin's syndrome, Invasive mucormycosis, Rhino-cerebral mucormycosis, Invasive fungal rhinosinusitis, Rhino-orbital mucormycosis
Introduction
Garcin's syndrome is a rare clinical entity, described initially as a gradual involvement, leading to unilateral paralysis of at least seven and sometimes all cranial nerves, without any long tract signs or intracranial hypertension [1]. It has traditionally been observed in association with tumors involving the skull base, and the association with rhino-cerebral mucormycosis is an unusually rare occurrence [2]. Invasive mucormycosis, originating from the paranasal sinuses, can become a fatal infection once it invades the intracranial cavity. It rapidly spreads along the skull base and large vessels. The invasive nature of this pathology leads to the gradual involvement of several cranial nerves by various mechanisms. Since Garcin’s syndrome is associated with a high rate of mortality, prompt diagnosis and identification of this syndrome are critical while planning appropriate and timely treatment. To date, there are only six reported cases of this condition in association with rhino-cerebral mucormycosis. In this article, we report the 7th case along with a review of the available literature.
Case Report
We report a case of a 33-year-old male who presented to our tertiary care center with numbness and weakness of the left side of face, which started 20 days back. It was associated with drooping of left eyelid (Fig. 1a, b) and a small necrotic ulcer over the hard palate (Fig. 1c). The patient was in poor general condition and had unsteady posture. A detailed examination of cranial nerves (CN) was conducted. It revealed a loss of perception of light in the left eye (CN I); absent sense of smell (CN II), ptosis, and complete ophthalmoplegia (CN III, IV, VI). There was a gross asymmetry and weakness over the left face (CN VII) (Fig. 1b). Patient had a House-Brackmann score of V with associated severe sensory neural hearing loss (SNHL)(CN VIII), absent gag reflex (CN IX), change in voice (CN X), drooping left shoulder (CN XI) and deviation of the tongue (CN XII). He was a known case of Type 1 diabetes mellitus and was not on medication. His blood sugar levels were uncontrolled (> 300 mg/ml), and there was a presence of urinary ketone bodies. Nasal endoscopy revealed a mass in the left middle meatus and purulent discharge extruding from the sphenoid sinus. Biopsy from the necrotic edge of the ulcer in the hard palate showed aseptate hyphae with branching pattern on KOH mount (20%). Fungal invasion was further confirmed by histopathology. CT scan revealed a soft tissue density, filling anterior and posterior ethmoids and sphenoid sinuses along with the erosion of the medial orbital wall reaching the orbital apex and compressing the optic nerve (Fig. 2). There was no intracranial invasion. The patient was managed with intravenous insulin and liposomal Amphotericin B, which was administered at the dose of 5 mg/kg/day for six weeks. Signs of recovery appeared after three weeks of Amphotericin B. Upon completion of six weeks of treatment; the patient showed significant improvement in general condition. His vision improved from perception of light negative (PL-VE) to hand movement positive (HM +) and further to finger counting at 3 m at the end of 12 weeks. Ptosis, eye movements, hearing, gait, gag, and tongue movement recovered maximally by 12 weeks (Fig. 3). Also, there was slight recovery in facial weakness. The patient was discharged at the end of six weeks and was kept in a close follow-up and referred for rehabilitation for CN palsies.
Fig. 1.
a Loss of cranial nerve function is apparently noted as ptosis left eye (III), loss of nasolabial fold (VII), loss of forehead crease (VII) (at rest); b Grade V Left Sided Facial paralysis with ptosis (upon attempted smile); c Necrotic ulcer with erosion of bony hard palate is noted on the left side
Fig. 2.
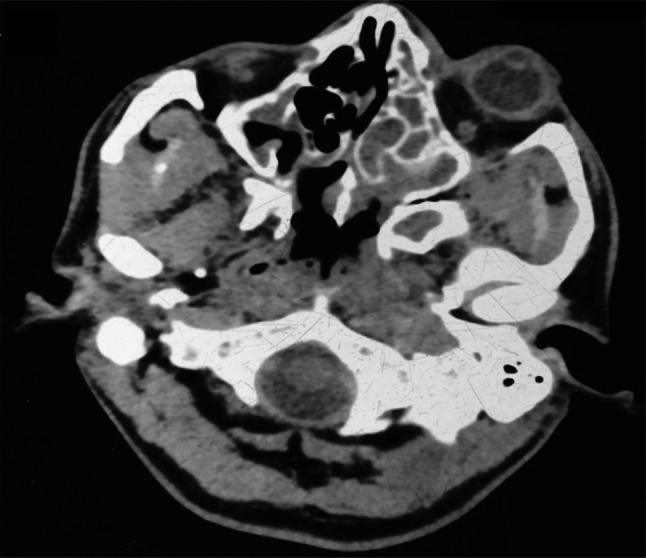
CT scan axial cut showing opacity in left ethmoidal air cells with left orbital invasion and outward displacement of left eyeball
Fig. 3.

Improvement is noted in the function of cranial nerve III after 6 weeks of amphotericin B. There is minimal recovery of VII nerve when compared with the pre-treatment score
Materials and Methods
A thorough literature search using the MeSH term—‘mucormycoses’ and keywords—‘Invasive Mucormycoses’ or ‘Rhino-orbital’ or ‘Rhino-cerebral mucormycoses’ and ‘Garcin’s syndrome’, was conducted on Pubmed/MEDLINE, Google scholar, LILACS, medRxiv and Google. A total of six reported cases were found in international literature published between 2000 and 2020. The available literature on case presentations of invasive mucormycosis presenting with Garcin's syndrome was reviewed. The data was analyzed in terms of clinical presentation, radiological features of the disease, treatment received and survival outcome.
Results
A compilation of the data is described in the Table 1.
Table 1.
A compilation of the data on studies involving Garcin’s Syndrome and Mucormycosis
| No | Age/sex | Comorbidity | Organism | Management | Cranial nerve involvement | Outcome | |
|---|---|---|---|---|---|---|---|
| 1 | Hanse Mc et al. [2] | 47/M | Diabetes | Mucor | Orbital exenteration, medial maxillectomy, debridement, lip + Amp B | I, II, III, IV, V, VI, VII, VIII, IX, XII | Improved |
| 2 | Mutsukura K et al. [3] | 64y/M | Diabetes | Mucor | Amp B | II, III, IV, V, VI, VII, IX, X | Died |
| 3 | Yang NH et al. [4] | 45y/F | Diabetes | Mucor | Amp B | II, III, IV, V, VIVII, IX, X | Died |
| 4 | Narayan S et al. [5] | Male | Diabetes | Mucor | Amp B | II, III, IV, V, VIVII, IX, X, XII | Died |
| 5 | Ozkul A et al. [6] | 65y/F | Immunosuppressed + diabetes | Mucor | Debridement Amp B | II, III, IV, V, VII, VIII, IX, X, XI, XII | Died |
| 6 | Safder S et al. [7] | 12y/F | Immunosuppressed | Mucor | Orbital exenteration + endoscopic middle & inferior turbinectomy + partial ethmoidectomy + Amp B | Multiple cranial neuropathies | Improved |
| 7 | Present Case | 40y/M | Diabetes | Mucor | Debridement, lip. amphotericin B | II, III, IV, V, VI, VII, VIII, IX, X, XII | Improved |
Discussion
First described in 1926, Gullian-Alajouanine-Garcin Syndrome or Garcin’s syndrome, is characterized by deterioration of the function of all ipsilateral cranial nerve palsies [8]. However, with technological advancements in radiology, it is diagnosed much earlier and therefore, the criteria now include multiple cranial nerve involvement (at least 7), in the absence of long tract signs and raised intracranial pressure [9]. Many possible causes of Garcin’s syndrome have been reported, including primary tumors of the skull base, such as nasopharyngeal carcinoma [2, 10], tonsillar carcinoma [8], giant cell tumor [11], and non-Hodgkin lymphoma [12], metastatic tumors, such as those arising from lung cancer [13], breast carcinoma [14], and renal carcinoma. [15] However, Garcin’s syndrome, in association with invasive mucormycosis, is seldom encountered and rarely documented. Our case represents the seventh patient described in the literature. The novelty of this case is the involvement of the VIII nerve which was yet unreported.
Mucormycosis is caused by the opportunist, ubiquitously present fungi which commonly belongs to the family Mucorales. Nonetheless, cases of invasive fungal rhinosinusitis caused by other rare genus have also been reported [16]. Invasive fungal sinusitis is an affection of the immunosuppressed state like uncontrolled diabetes mellitus, hematologic malignancies etc., with a high mortality rate, being reported by some authors to be as high as 40% [5]. In the setting of skull base involvement and Garcin’s syndrome, it may rise further. In our review, of the total seven patients, only three survived, bringing the collective mortality to 42.85%. Mortality rate due to this disease is likely to be higher had there been more data/studies. The main drawback in the management of such patients is the inability of the treating physicians to identify the process at an early stage.
The symptoms are similar to those of acute sinusitis and the gold standard for diagnoses in this situation is the histology of the endoscopic biopsy specimen, complemented by microbial studies to identify the pathogen [17]. Pathologically, mucormycosis infections are characterized by explosive growth due to angioinvasion, infarction, and direct spread and necrosis by fungal hyphae. However, there is a strict unilateral occurrence of the disease process in Garcin’s Syndrome. A likely explanation could be the perineural spread of the fungal hyphae and growth along the leptomeningeal vessels [18]. The radiologic evaluation based on CT and magnetic resonance image (MRI) helps to determine the extent of the skull base and intracranial involvement beyond the sinuses and orbits. The MRI provides better visualization of the CNS, perineural invasion and vascular obstruction.
The patients suspected of developing Garcin’s syndrome should always be managed at a tertiary care center involving a multidisciplinary team. Correction of acidosis and regulation of the blood glucose levels is imperative in diabetics. The patient should be rehydrated, and electrolyte imbalance normalized. Treatment with amphotericin B should be commenced at the earliest, initially at the dose of 1 mg/kg/day, which can be increased to 3 or even 5 mg/kg/day. Liposomal amphotericin B is preferred due to its reduced renal toxicity, fewer adverse effects, and better penetration in the CNS [19]. The renal function, as well as potassium and magnesium, must be rigorously monitored during the treatment. Surgical debridement has a crucial role and should be undertaken in all patients with necrotic tissue. Regular cranial nerve testing is essential to identify any change or worsening of nerve functions which may warrant a change in the treatment strategy. Posaconazole and Voriconazole [20] are being increasingly used in cases of Amphotericin resistance or intolerance with good results. It can be administered orally and is well tolerated with a high response rate.
Unfamiliarity with the symptoms of Garcin’s Syndrome and the rapidity of disease progression leads to loss of life and function. A very high index of suspicion and early treatment is critical for patient survival and reduction in long term sequelae. Just as medical therapy, rehabilitative treatment holds an important place in the management of these patients. In our patient, for CN III, IV, and VI, muscle transpositions or botox injections to weaken the antagonist muscle action were considered after treatment. Intense rehabilitation was started for facial nerve palsy due to CN VII weakness. Sequential audiograms were planned and hearing rehabilitation considered for CN VIII weakness. Speech and swallowing therapy were started for CN IX and CN X palsy [21].Our patient had survived the disease process due to the prompt diagnosis and timely intervention. Expeditious initiation of appropriate treatment resulted in partial reversal of CN III, IV, V, VI and VIII palsies thereby providing a better quality of life in the post treatment period.
Conclusion
Garcin’s syndrome is an extremely rare association in patients with rhino-orbito-cerebral mucormycosis. A prompt diagnosis, appropriate and timely antifungal management along with post-treatment monitoring and rehabilitation is crucial to improve the survival, revert the damage and reduce the sequelae in patients presenting with this disease.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interest
Authour declared that they are no conflict of interest.
Footnotes
All authors meet the ICMJE authorship criteria in writing this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Garima Yadav, Email: garimayaadav@gmail.com.
Neha Verma, Email: dr.neha.verma@gmail.com.
Sarthak Sachdeva, Email: sachdevasarthak68@gmail.com.
Arun Goyal, Email: arungoyal150@yahoo.co.in.
References
- 1.Guillain G, Alajouanine T, Garcin R. Le syndrome paralytiqueunilatéralglobale des nerfscraniens. Bull Med Hop (Paris) 1926;50:456–460. [Google Scholar]
- 2.Hanse MCJ, Nijssen PCG. Unilateral palsy of all cranial nerves (Garcin syndrome) in a patient with rhinocerebralmucormycosis. J Neurol. 2003;250(4):506–507. doi: 10.1007/s00415-003-1019-y. [DOI] [PubMed] [Google Scholar]
- 3.Mutsukura K, Tsuboi Y, Imamura A, Fujiki F, Yamada T. Garcin syndrome in a patient with rhinocerebralmucormycosis. No ToShinkei. 2004;56:231–235. [PubMed] [Google Scholar]
- 4.Yang HN, Wang CL. Looks like tuberculous meningitis, but not: a case of rhinocerebralmucormycosis with garcin syndrome. Front Neurol. 2016;7:1–3. doi: 10.3389/fneur.2016.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Narayanan S, Panarkandy G, Subramaniam G, et al. (2017) The "black evil" affecting patients with diabetes: a case of rhino orbito cerebral mucormycosis causing Garcin syndrome. Infect Drug Resist. 2017;10:103–108. doi: 10.2147/IDR.S130926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Özkul A, Başak S, Ertuǧrul MB, Odabaşi O, Özgeçen-Dinçel H, Öztürk B. Garcinsendromuylakendinigösterenrinoserebralmukormikozolgusu. KlimikDergisi. 2011;24(3):187–190. doi: 10.5152/kd.2011.46. [DOI] [Google Scholar]
- 7.Safder S, Carpenter JS, Roberts TD, Bailey N. The “black turbinate” sign: an early MR imaging finding of nasal mucormycosis. Am J Neuroradiol. 2010;31(4):771–774. doi: 10.3174/ajnr.A1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greulich W, Sackmann A, Schlichting P. Garcin syndrome. Clinical aspects and diagnosis of a rare cranial nerve syndrome with special reference to computerized tomography and nuclear magnetic resonance image findings. Nervenarzt. 1992;63:228–233. [PubMed] [Google Scholar]
- 9.Bignas B, Vinken PJ, Bruyn GW. Tumors of the base of the skull. In: Vinken PJ, Bruyn GW, editors. Handbook of clinical neurology. Amsterdam: Elsevier; 1974. pp. 180–183. [Google Scholar]
- 10.Xia NG, Chen YY, Wang XS, Xu HQ, Zheng RY. Garcin syndrome caused by parotid gland adenoid cystic carcinoma. Medicine. 2017 doi: 10.1097/MD.0000000000008508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bibas-Bonet H, Fauze RA, Lavado MG, Páez RO, Nieman J. Garcin syndrome resulting from a giant cell tumor of the skull base in a child. PediatrNeurol. 2003;28(5):392–395. doi: 10.1016/s0887-8994(03)00009-2. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura A, Toyoda K, Shozawa Y, Saito-Arai Y, Shimizu T, Matsumura K. Primary non-hodgkin lymphoma of the skull base presenting with garcin syndrome: MRI manifestations. J Neuroimaging. 2009;19:295–297. doi: 10.1111/j.1552-6569.2008.00264.x. [DOI] [PubMed] [Google Scholar]
- 13.Fujii M, Kiura K, Takigawa N, Yumoto T, Sehara Y, Tabata M, Tanimoto M. Presentation of Garcin syndrome due to lung cancer. J ThoracOncol. 2007;2(9):877–878. doi: 10.1097/JTO.0b013e31811f473d. [DOI] [PubMed] [Google Scholar]
- 14.Benedetti J. Garcin syndrome—a case report. SchweizRundsch Med Prax. 1989;78:1045–1048. [PubMed] [Google Scholar]
- 15.Kawahara Y, Deguchi K, Sato K, Hishikawa N, Kono S, Ohta Y, Yamashita T, Hayashi E, Sato Y, Abe K. Aggressive Garcin's syndrome by acquired cystic disease of kidney-related renal cell carcinoma in a long-term hemodialytic patient. J NeurolSci. 2015;355(1–2):216–218. doi: 10.1016/j.jns.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Liu YC, Zhou ML, Cheng KJ, Zhou SH, Wen X, Chang CD. Successful treatment of invasive fungal rhinosinusitis caused by Cunninghamella: a case report and review of the literature. World J Clin Cases. 2019;7(2):228–235. doi: 10.12998/wjcc.v7.i2.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gillespie MB, Malley BWO. An algorithmic approach to the diagnosis and management of invasive fungal rhinosinusitis in the immunocompromised patient. OtolaryngolClin North Am. 2000;33(2):323–334. doi: 10.1016/S0030-6665(00)80008-0. [DOI] [PubMed] [Google Scholar]
- 18.McLean FM, Ginsberg LE, Stanton CA. Perineural spread of rhinocere-bralmucormycosis. AJNR. 1996;17:114–116. [PMC free article] [PubMed] [Google Scholar]
- 19.Saedi B, Sadeghi M, Seilani P. Endoscopic management of rhinocerebralmucormycosis with topical and intravenous amphotericin B. J LaryngolOtol. 2011;125(8):807–810. doi: 10.1017/S0022215111001289. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J, Kim JD, Beaver HA, Takashima M, Lee AG. Rhino-orbital mucormycosis treated successfully with posaconazole without exenteration. Neuro-Ophthalmology. 2013;37(5):198–203. doi: 10.3109/01658107.2013.809463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Netterville JL, Civantos FJ. Rehabilitation of cranial nerve deficits after neurotologic skull base surgery. Laryngoscope. 1993;103:45–54. doi: 10.1002/lary.1993.103.s60.45. [DOI] [PubMed] [Google Scholar]



