Abstract
Juvenile nasopharyngeal angiofibroma is a benign vascular lesion with propensity of bony erosion leading to skull base involvement and intracranial extension. It involves multiple compartments which are difficult to access surgically. With surgical expertise endoscopic resection of angiofibroma has become the preferred choice of surgical management. This article presents our experience with endoscopic approach for angiofibroma and establishes the modified Denker’s procedure as a effective approach for removal of tumor. A prospective case study was done on 25 cases of juvenile nasopharyngeal angiofibroma treated surgically by endonasal endoscopic modified Denker’s approach in the department of ENT at BJ Medical College, Ahmedabad over a period of 4 years from January 2015 to January 2019. This technique was used up to Fisch stage 3b with extension up to infratemporal fossa. Using this technique no major recurrence or major morbidity was observed and did not produce any late serious complications. The endoscopic technique allows the surgeon to achieve an extensive exposure of the sinuses and control of the sphenopalatine and internal maxillary arteries without the risk of palatal dysfunction, oronasal fistula, or facial scarring. In addition, the modified Denkers approach can be an effective and less mutilating technique in managing recurrences.
Keywords: Angiofibroma, Modified Denker’s, Endoscopic
Introduction
Juvenile nasopharyngeal angiofibromas (JNA) are uncommon, highly vascular neoplasms that are histologically benign but can be locally invasive and destructive [1]. They account for less than 0.05% of all the head and neck tumors and occurs exclusively in adolescents males. It is the most common benign tumor of the nasopharynx [1, 2].
JNA originate from the superior lip of the sphenopalatine foramen and has the tendency to grow along the natural foramina associated with its site of origin [3]. The tumor can grow into the nasopharynx and nasal cavity, with invasion of maxillary, ethmoid and sphenoid sinuses and spread laterally into pterygopalatine fossa. Tumor can erode the pterygoid plates leading into the infratemporal fossa. It may involve the orbit through the inferior orbital fissure. Extension into middle cranial fossa may occur via foramen rotundum, ovale and lacerum. From the middle cranial fossa, the tumor can invade the parasellar region, usually remaining extradural and lateral to the sphenoid sinus [4–6]. Intracranial extension can occur through destruction of the skull base at the attachment of the pterygoid process, lateral to the internal carotid artery or through the sphenoid sinus and into the region of the cavernous sinus [5].
Diagnosis of this tumor is done by careful clinical and radiographic evaluation. Nasal endoscopic examination and contrast enhanced computed tomography paranasal sinuses (CECT PNS) along with magnetic resonance imaging (MRI) for intracranial and intraorbital extension are done for diagnosis. Surgical resection is regarded as the mainstay of treatment [7]. Ancillary treatment modalities such as radiotherapy and chemotherapy are on rare occasions recommended, as in presence of intracranial extension and involvement of the cavernous sinus and carotid artery [8]. Several surgical approaches have been recommended in the literature, the success of which depends on a good preoperative staging and the surgeon’s expertise.
This article reviews our experience in the management of nasopharyngeal angiofibromas over a period of 4 years by endonasal endoscopic modified Denker’s approach as an effective technique for removal of JNA.
Aims and Objectives
This article presents our experience with endoscopic approach for angiofibroma and eastablishes the modified Denker’s procedure as a effective approach for removal of tumor.
Materials and Methods
A prospective case study was done on 25 cases of juvenile nasopharyngeal angiofibroma treated surgically by endonasal endoscopic modified Denker’s approach in the department of ENT at BJ Medical College, Ahmedabad over a period of 4 years from January 2015 to January 2019. All patients underwent computed tomographic scanning or magnetic resonance imaging as a means of radiologic evaluation. Nasal endoscopy was done in all patients. Angiographic studies were performed, showing the internal maxillary artery and the ascending pharyngeal artery of the external carotid system as the main source of blood supply. Tumor staging was done by review of the clinical examinations and the radiologic imaging studies and followed the criteria proposed by Fisch. Patients up to stage 3b according to fisch classification were included in our study. Patients with intracranial extension were excluded from the study. All the patients were followed up for 18–24 months (Figs. 1, 2, 3).
Fig. 1.
Intranasal incisions are made with cautery along the dotted lines and carried through the periosteum. Specifically, an inferior incision is made at the junction of the nasal floor and lateral nasal wall, followed by a superior incision along the lateral nasal wall and anteriorly overlying the pyriform aperture. IT, inferior turbinate; M, middle turbinate; NF, nasal floor; NS, nasal septum [9]
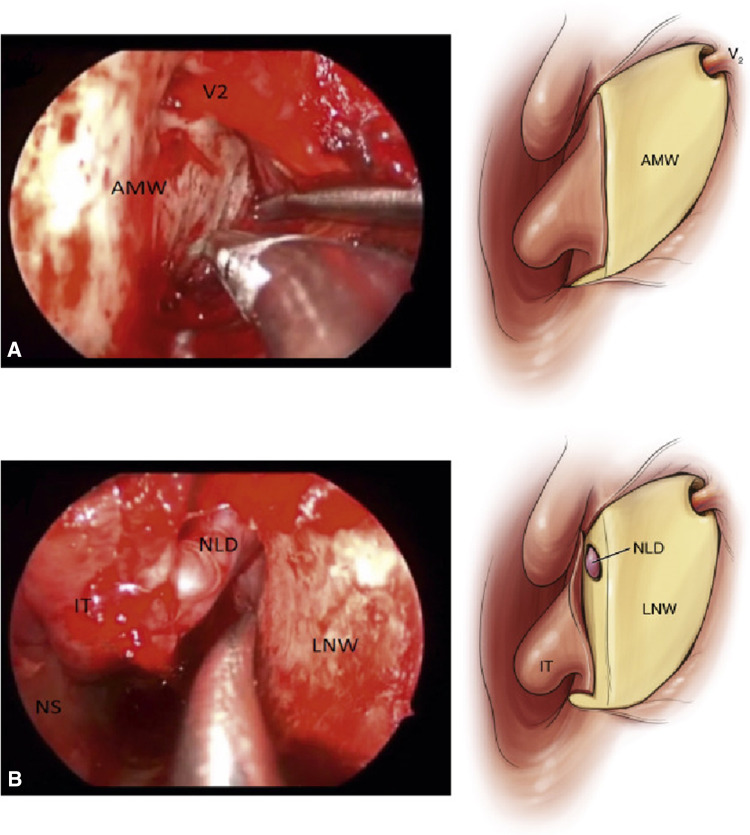
Fig. 2.
a Elevating the mucosa off of the maxilla using a suction Freer. b Elevating the mucosa off of the lateral nasal wall. The nasolacrimal duct is cut sharply once exposed [9]
Fig. 3.
Expose the maxillary sinus. AMW, anterior maxillary sinus wall; IT, inferior turbinate; LNW, lateral nasal wall; NLD, nasolacrimal duct; NS, nasal septum; V2, infraorbital nerva [9]
Fisch Staging for Angiofibroma
STAGE 1—tumor limited to the nasal cavity and nasopharynx; bone destructon is negligible or limited to sphenopalatine foramen.
STAGE 2—tumor extension into the pterygopalatine fossa, or maxillary, sphenoid or ethmoid sinuses with bone destruction.
STAGE 3a—tumor extension into the orbit or infratemporal fossa without intracranial involvement.
STAGE 3b—stage 3a with extradural (parasellar) intracranial involvement.
STAGE 4a—intradural without cavernous sinus, pituitary, or optic chiasma involvement.
STAGE 4b—involvement of the cavernous sinus, pituitary, or optic chiasma.
Surgical technique
Step 1: Mucosal Cuts
Under visualization with a 4-mm 0-degree rod-lens endoscope, 2% lignocaine with 1:200,000 epinephrine is first injected into the anticipated incision sites along the nasal floor, lateral nasal wall, and anterior to the head of the inferior turbinate. A unipolar electrocautery with a guarded needle tip is used to incise the mucosa inferiorly at the junction of the nasal floor and lateral nasal wall, carrying the incision through the periosteum. A second mucosal incision is then made superiorly along the lateral nasal wall and carried anteroinferiorly to lie just in front of the anterior head of the inferior turbinate overlying the edge of the pyriform aperture.
Step 2: Soft Tissue Dissection Over the Maxilla
A subperiosteal dissection is performed with a suction freer elevator to expose the anterior maxilla, the infraorbital foramen, and its neurovascular bundle as well as the lateral nasal wall.
Step 3: Bony Cuts to the Maxilla
A high-speed drill or osteotome is utilized to create a bony window into the anterior maxilla, taking care to stay inferior to the infraorbital nerve. Osteotomes are used to connect the window to the inferior bony cut of the medial maxillectomy, thereby allowing access to the anterior portion of the maxillary sinus. Specifically, a superior cut is made at the level of the roof of the maxillary sinus, an inferior cut at the junction of the nasal floor and medial maxillary wall, and a posterior cut along the posterior wall of the maxillary sinus. The lesion can then be resected en bloc along with its bony site of attachment. At the end of the procedure, the nasolacrimal duct is identified, preserved, and sharply cut at an oblique angle to prevent stenosis. Complete exposure of the posterior aspect of the maxillary sinus is also achieved, facilitating use of a 4-handed technique to remove tumors involving the pterygopalatine or infratemporal fossae if needed.
Results
A total of 25 patients, all males, with ages ranging from 11 to 22 years (mean age 17.9 years) were included in the study. 12 patients (48%) presented with right side tumor, while 13 patients (52%) presented with left side tumor. Nasal obstruction with recurrent bouts of spontaneous epistaxis was present in all 25 patients (100%). Rhinorrhea was present in 18 patients (72%). Conductive hearing loss due to Eustachian tube dysfunction was there in 8 patients (32%). Four patients (16%) presented with complaint of diplopia with proptosis of eye. Other symptoms such as rhinolalia clausa and headache was present in 12 (48%) and 6 (24%) patients respectively. All the patients were staged according to Fisch classification as described above. Eight (32%) patients were in Fisch stage 2, 9 (36%) patients were in stage 3a, whereas 8 (32%) patients were in stage 3b (Figs. 4, 5, 6).
Fig. 4.

Pie diagram showing side of presentation of JNA
Fig. 5.

Distribution of patients according to Fisch classification
Fig. 6.
Preoperative CT scan of the patient with JNA in coronal, sagittal and axial cuts respectively
Patients up to stage 3b were included in our study. Treatment approach for all the patients was endonasal endocopic modified Denker’s approach in our study.
Intraoperatively the nasopharynx and pterygopalatine fossa were involve in all 25 patients (100%). The tumor was observed to extend laterally into the infratemporal fossa via pterygomaxillary fissure in 17 patients (68%). Once tumor was present in the infratemporal fossa, it showed multidirectional spread along pathways of low resistance.
Orbital extension through inferior orbital fissure was seen in 15 patients (20.2%). Pterygoid fossa was found to be involved in 5 patients (20%). Greater wing of sphenoid was involved in 8 patients (32%). Tumor was found to be extending posteriorly by erosion of the base of pterygoid and greater wing of sphenoid.
Intraoperative blood loss was observed to be more with higher stages of disease/advanced disease (Figs. 7, 8).
Fig. 7.
Post operative CT scan of the patient in coronal, sagittal and axial cuts respectively
Fig. 8.

Resected specimen by endoscopic modified Denker’s approach
All the patients were followed up to 18–24 months post operatively. In our study we found 2 cases (8%) with residual disease. Most commonly residual tumor was found in the pterygoid wedge. To ensure complete tumor removal, pterygoid wedge was drilled in all the subsequent cases which allowed us to significantly reduce the incidence of residual and recurrent disease (Table 1).
Table 1.
Distribution of presentation of symptoms in patients with JNA
| Symptoms | Number of patients | Percentage (%) |
|---|---|---|
| Nasal obstruction | 25 | 100 |
| Epistaxis | 25 | 100 |
| Rhinorrhea | 18 | 72 |
| Conductive hearing loss | 8 | 32 |
| Diplopia with proptosis | 4 | 16 |
| Rhinolalia clausa | 12 | 48 |
| Headache | 6 | 24 |
Discussion
With superior surgical instrumentations available, better endoscopic illumination techniques and better direct vascular control methods, complete tumor removal can now be achieved for even advanced cases of JNA [9]. As an endoscope provides a magnified and multi angled viewing opportunity, tumor extensions can be much better visualized. With the modified Denker approach, the entire anterior maxilla and prelacrimal, anterior, inferior, and lateral recesses of the maxillary sinus can be directly accessed without the need for a sublabial and transseptal incision [10]. The entire posterior wall of the maxillary sinus is exposed, allowing the straight entry into the pterygopalatine and infratemporal fossa [10]. For tumors pedicled to the lateral wall, the site of attachment can be drilled without the need of angled instrumentation [11]. The absence of gingivobuccal sulcus incision prevents potential contamination of the sinus cavity with oral flora and possible development of oroantral fistula [11]. These advantages of modified Denker approach were similar to the study done by Lee and Chiu [11]. A variety of other endoscopic procedures have been described in literature. Robinson et al. [12] reported the use of non opposing septal incisions to facilitate endoscopic tumor resection. Harvey et al. [13] presented an anterior transseptal technique to access anterolateral maxillary lesions in a cadaveric study, which had the disadvantage of requiring the use of angled endoscopes, which may be technically difficult to maneuver. Ramakrishnan et al. [14] proposed the use of septal dislocation to increase access to the anterolateral maxillary sinus. Robinson et al. [15] supported the use of canine fossa trephination technique as a port of entry to access maxillary sinus pathology.
Recurrence rate observed in our study was 8%. The results were similar to the study done by Boghani et al. [16], in which recurrence rate was reported to be in range of 0-23% in purely endoscopic approach. Pyror et al. [17], reported no recurrence in 5 patients done by endoscopic approach. Nicolai et al. [18], observed the recurrence rate of 8.7%.
The 4-handed technique with 2 experienced surgeons allowed for the use of four hands in the operating field, considerably improving visualization and reducing the surgical time [9]. Endoscopes provided magnified view, allowing for safe dissection in correct plane under direct vision and preventing any unwanted injury to the surrounding neurovascular structures [9]. The illumination and magnification provided by endoscopes render these techniques superior to external approaches in selected cases [9].
Conclusion
Surgical approaches in the endoscopic era have revolutionized the management of JNA and have improved surgical outcomes for extensive lesions. The endoscopic technique allows the surgeon to achieve an extensive exposure of the sinuses and control of the sphenopalatine and internal maxillary arteries without the risk of palatal dysfunction, oronasal fistula, or facial scarring. In addition, the modified Denkers approach can be an effective and less mutilating technique in managing recurrences.
Compliance with Ethical Standards
Conflict of interest
The authors declares that there is no conflict of interest.
Research Ethics and Patient Consent
Written informed consent for patient information and images to be published was provided by the patients or legally authorized representatives.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hardillo JA, Vander velden LA, Knegt PP. Denker operation is an effective surgical approach in managing juvenile nasopharyngeal angiofibroma. Ann Otol Rhinol Laryngol. 2004;113(12):946–950. doi: 10.1177/000348940411301202. [DOI] [PubMed] [Google Scholar]
- 2.Bremer JW, Neel HB, III, Desanto LW, Jones GC. Angiofibroma: treatment trends in 150 patients during 40 years. The Laryngoscope. 1986;96(12):1321–1329. doi: 10.1288/00005537-198612000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Conley J, Healey WV, Blaugrund SM, Erzin KH. Nasopharyngeal angiofibroma in the juvenile. Surg Gynecol Obstet. 1968;126(4):825–837. [PubMed] [Google Scholar]
- 4.Andrews JC, Fisch U, Aeppli U, Valavanis A, Makek MS. The surgical management of extensive nasopharyngeal angiofibromas with the infratemporal fossa approach. The Laryngoscope. 1989;99(4):429–437. doi: 10.1288/00005537-198904000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Batsakis JG (1979) Tumors of the head and neck: clinical and pathological considerations. Williams & Wilkins
- 6.Neel HB, Whicker JH, Devine KD, Weiland LH. Juvenile angiofibroma: review of 120 cases. Am J Surg. 1973;126(4):547–556. doi: 10.1016/S0002-9610(73)80048-0. [DOI] [PubMed] [Google Scholar]
- 7.Janakiram TN, Bhatia Sharma S, Nahata Gattani V. Multiport combined endoscopic approach to nonembolized juvenile nasopharyngeal angiofibroma with parapharyngeal extension: an emerging concept. Int J Otolaryngol. 2016;2016:4203160. doi: 10.1155/2016/4203160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danesi G, Panizza B, Mazzoni A, Calabrese V. Anterior approaches in juvenile nasopharyngeal angiofibromas with intracranial extension. Otolaryngol Head Neck Surg. 2000;122(2):277–283. doi: 10.1016/S0194-5998(00)70256-7. [DOI] [PubMed] [Google Scholar]
- 9.Janakiram TN, Sharma SB, Kasper E, Deshmukh O, Cherian I. Comprehensive preoperative staging system for endoscopic single and multicorridor approaches to juvenile nasal angiofibromas. Surg Neurol Int. 2017;8:55. doi: 10.4103/sni.sni_295_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JT, Suh JD, Carrau RL, Chu MW, Chiu AG. Endoscopic Denker’s approach for resection of lesions involving the anteroinferior maxillary sinus and infratemporal fossa. The Laryngoscope. 2017;127(3):556–560. doi: 10.1002/lary.26237. [DOI] [PubMed] [Google Scholar]
- 11.Lee JT, Chiu AG (2019) Endoscopic Denker approach for anterior maxilla tumors. In: Atlas of endoscopic sinus and skull base surgery, pp 183.e1–190.e1. 10.1016/B978-0-323-47664-5.00022-5
- 12.Robinson S, Patel N, Wormald PJ. Endoscopic management of benign tumors extending into the infratemporal fossa: a two-surgeon transnasal approach. The Laryngoscope. 2005;115(10):1818–1822. doi: 10.1097/01.mlg.0000174956.90361.dc. [DOI] [PubMed] [Google Scholar]
- 13.Harvey RJ, Sheehan PO, Debnath NI, Schlosser RJ. Transseptal approach for extended endoscopic resections of the maxilla and infratemporal fossa. Am J Rhinol Allergy. 2009;23(4):426–432. doi: 10.2500/ajra.2009.23.3333. [DOI] [PubMed] [Google Scholar]
- 14.Ramakrishnan VR, Suh JD, Chiu AG, et al. Septal dislocation for endoscopic access of the anterolateral maxillary sinus and infratemporal fossa. Am J Rhinol Allergy. 2011;25:128–130. doi: 10.2500/ajra.2011.25.3559. [DOI] [PubMed] [Google Scholar]
- 15.Robinson SR, Baird R, Le T, Wormald PJ. The incidence of complications after canine fossa puncture performed during endoscopic sinus surgery. Am J Rhinol. 2005;19(2):203–206. doi: 10.1177/194589240501900215. [DOI] [PubMed] [Google Scholar]
- 16.Boghani Z, Husain Q, Kanumuri VV, Khan MN, Sangvhi S, Liu JK, Eloy JA. Juvenile nasopharyngeal angiofibroma: a systematic review and comparison of endoscopic, endoscopic-assisted, and open resection in 1047 cases. The Laryngoscope. 2013;123(4):859–869. doi: 10.1002/lary.23843. [DOI] [PubMed] [Google Scholar]
- 17.Pryor SG, Moore EJ, Kasperbauer JL. Endoscopic versus traditional approaches for excision of juvenile nasopharyngeal angiofibroma. The Laryngoscope. 2005;115(7):1201–1207. doi: 10.1097/01.MLG.0000162655.96247.66. [DOI] [PubMed] [Google Scholar]
- 18.Nicolai P, Villaret AB, Farina D, Nadeau S, Yakirevitch A, Berlucchi M, Galtelli C. Endoscopic surgery for juvenile angiofibroma: a critical review of indications after 46 cases. Am J Rhinol Allergy. 2010;24(2):e67–e72. doi: 10.2500/ajra.2010.24.3443. [DOI] [PubMed] [Google Scholar]