Abstract
Human papillomavirus (HPV) related oral cancers are increasing and are associated with sexual risk behaviours. An increase in the incidence of oral cancer has been observed in South-central Asian countries. The objective was to systematically review the evidence on the association of HPV and oral squamous cell carcinoma (OSCC) among adults living in South-central Asia. We searched multiple databases and reference lists of relevant articles in December 2018. Quality assessment of the selected articles were done using the Newcastle–Ottawa quality assessment scale. Thirteen out of 150 articles met the eligibility criteria. Most studies were from India (10/13) followed by Pakistan (2/13) and Bangladesh (1/13). Half (7/13) of the studies found a positive association between HPV with OSCC. HPV 16, HPV 18 and HPV 16/18 were found to be the most common types implicated in HPV infection associated with OSCC. Moreover, buccal mucosa was the most common site of oral cancer. The review found equivocal evidence in relation to the association of HPV with oral squamous cell carcinoma among people living in South Asia.
Electronic supplementary material
The online version of this article (10.1007/s12070-020-01842-9) contains supplementary material, which is available to authorized users.
Keywords: Oral cancer, HPV infection, Human papillomavirus
Background
Non-communicable diseases have become a health issue in low or middle-income countries (LMIC). Earlier trends indicated a demographic transition from communicable diseases to non-communicable diseases [1]. The increase in life expectancy, the decline in fertility and mortality rates will accelerate population aging in LMIC [2]. Therefore, cardiovascular and cerebrovascular diseases, diabetes, and cancer are emerging as major health issues [3]. Oral cancer is among the top ten cancers by incidence and deaths for males in LMIC. This is not the case in high income countries [4]. In 2012, lip and oral cancer (10%) were the second most common type of new cancer cases among males in South-central Asia behind only lung cancers (11%) [4]. Oral cavity was the most common cancer site among males [4]. The above fact emphasises the impact of oral cancer on the public health of South-central Asian countries: Afghanistan, Bangladesh, Bhutan, India, Kyrgyzstan, Kazakhstan, Maldives, Nepal, Pakistan, Sri Lanka, Tajikistan, Turkmenistan, and Uzbekistan.
The annual global incidence of oral cancer is more than 650,000 cases and the annual deaths due to oral cancer is more than 330,000 cases [5]. Oral cancer had caused an estimated 97,408 deaths in Asia [6]. Oral cancers occur at the lip, oral cavity, nasopharynx, and pharynx [5]. High exposure to risk factors has resulted in a high burden of oral cancer in South-central Asia [5]. Globally, an increase in oral cancers is seen in younger age groups [7]. Preventive measures are needed to curtail the health issue faced due to oral cancer. The main risk factors for oral cancer include tobacco, alcohol, prolonged sun exposure, human papillomavirus (HPV), male gender, fair skin, old age, poor oral hygiene, poor nutrition, immunodeficiency and marijuana [8].
HPV infection leads primarily to anogenital cancers [9]. However, HPV-related oral cancers are increasingly observed and are associated with sexual risk behaviours [10–12]. Serotype HPV-16 infection was commonly implicated with oral squamous cell carcinoma (OSCC). Oral HPV-16 infection was associated with an increased risk of oropharyngeal cancer, regardless of a history of use of tobacco, alcohol, or both [10].
HPV associated OSCC has been on the rise in United States of America and European countries [13]. Also, there is an increase in the incidence of oral cancer in South-central Asian countries. We conducted a systematic review to review the evidence on HPV-associated OSCC among adults aged ≥ 18 years who live in South-central Asia. The following specific research question was addressed in the review: Do adults aged ≥ 18 years who live in South-central Asia and have human papillomavirus infection show an increased risk for oral squamous cell carcinoma compared to those who do not have the infection during the last 10 years?
Methods
Eligibility Criteria
Published, full text, peer-reviewed, original research articles during the last 10 years were included which assess the above-mentioned research question among adults aged ≥ 18 years and living in South-central Asia. Afghanistan, Bangladesh, Bhutan, India, Kyrgyzstan, Kazakhstan, Maldives, Nepal, Pakistan, Sri Lanka, Tajikistan, Turkmenistan, and Uzbekistan are the countries in South-central Asia. All study designs were included. Non-English language articles were excluded.
Information Sources and Search Strategy
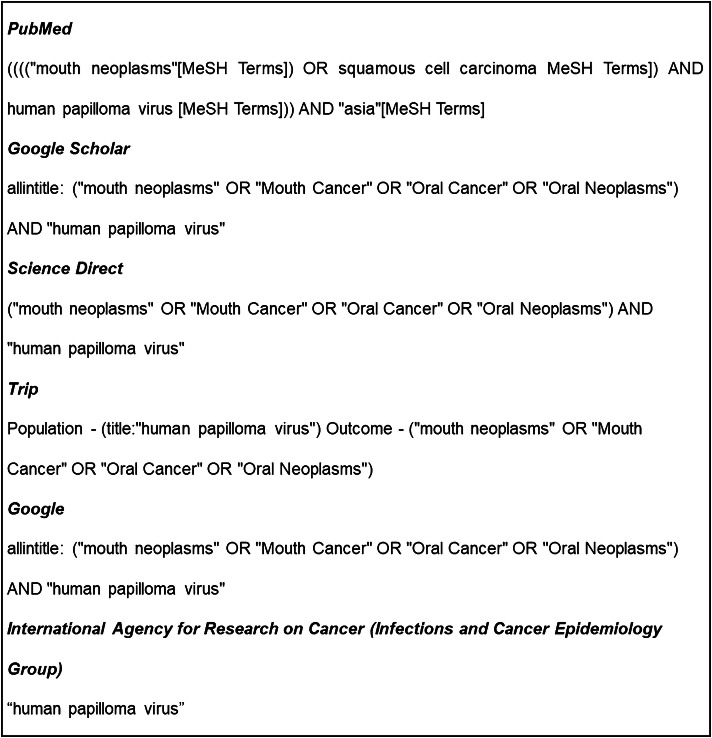
The search was done in December 2018. Specific strings of keywords (Fig. 1) were used for PubMed (Advanced search), Google Scholar (Advanced search), Science Direct (Title, Abstract, Keywords search), Trip (PICO search), Google and International Agency for Research on Cancer (Infections and Cancer Epidemiology Group). MeSH terms were used in PubMed search, and the “allintitle” option was used in Google Scholar and Google search to improve the yield of the selection. MeSH term “Asia” was added to the search string for PubMed to reduce the high number of identified articles. Also, articles relevant to the research question were searched from the reference lists of the selected studies.
Fig. 1.
Keywords for databases and the number of search results
Study Selection
All authors were involved in study selection. DR performed a comprehensive literature search. BW independently screened the titles and abstracts of all identified studies for selection, according to the inclusion criteria. The selected studies were independently reviewed by RK to confirm the eligibility.
Data Collection Process, Data Items and Data Analysis
Demographic data, the degree of association and outcomes of the study were extracted from the selected studies (Additional file 1). The units of measurements were presented in SI units. Descriptive statistics were used to describe the data. Quality assessment of the selected articles were done (Additional file 2) using the scale adapted from the Newcastle–Ottawa quality assessment scale to perform a quality assessment of cross-sectional studies for a systematic review by Hillen et al. [14]. This systematic review was reported according to the preferred reporting items for systematic survey and meta-analysis (PRISMA) statement [15] (Additional file 3).
Results
Sorted Citations
A total of 150 results were found from the databases: PubMed—25, Google Scholar—19, Science Direct—11, Trip—10, Cochrane Library—1 Google—47, and International Agency for Research on Cancer (Infections and Cancer Epidemiology Group)—37 (Fig. 2). Further, 8 articles were found from the reference lists of the selected articles. After removal of duplicates, 71 articles were included for the title and abstract screening. Out of which 48 articles were excluded due to irrelevance to the study objective. Two articles were excluded due to unavailability of full-text, and another article was excluded as it was in the Spanish language. The full-texts of the remaining 20 articles were examined, and 07 were excluded, as it did not fulfil the eligibility criteria of the review [not on an association between HPV and oral cancer (n = 04), results included on all cancers of the head and neck (n = 02), articles published 10 years before (n = 01)]. Following the above screening steps, 13 articles were selected for the review [16–28] (Fig. 2).
Fig. 2.
Flow diagram showing the selection process of articles for this review according to PRISMA 2009
Critical Review of the Selected Paper
Additional file 1 summarises the data extracted from the 13 selected studies. It includes details on country of origin, relevant study design, study type, study population, sample size, relevant statistics used, relevant results, bias reported and critical comments related to the review. Most of the studies were based in India (10/13), followed by Pakistan (2/13) and Bangladesh (1/13). Patients with OSCC were the participants and patients with pre-malignant oral lesions and healthy individuals (39%—5/13) were the comparator group. During the past 10 years articles were published from 2011 to 2018 and, 2013 witnessed the highest number of articles (31%—4/13). Variations in reporting made it difficult for summary data of age and gender of the subjects. Half of the studies reported an association between betel chewing habit and oral cancer (54%—7/13).
Ten articles (77%) were cross-sectional studies, and the rest were reported as case–control studies (23%—3/13). However, the three studies mentioned as case–control studies were also noted to be cross-sectional studies. The polymerase chain reaction was used in all studies for the detection of HPV infection. Also, immunohistochemistry was used in 2 studies but, both studies did not mention any special reason for the use of both methods. Kundu et al. [16] considered HPV positive only when found in both methods. Chaudhary et al. [26] presented results separately for both the analysis methods. Nevertheless, both studies had shown a positive association for HPV and oral cancer. The results were comparable to other studies.
Descriptive statistics were used to present details of HPV positive patients among OSCC patients, and appropriate significance tests were used to compare the findings with controls (Additional file 1). However, Zil-e-Rubab et al. [17] used logistic regression analysis (P < 0.05) which would address the confounding of other risk factors for OSCC. Lack of sample size calculation, details of non-respondents and control of confounders were observed in all selected studies while the lack of comparability of groups was observed in 85% (11/13). Sample sizes varied from 23 to 350 OSCC cases. But, none of the articles demonstrated a calculation for sample sizes (Additional file 2). Sampling strategy was not reported clearly in any of the selected articles. Considering the representativeness of the sample, there was only a fair chance of generalisability of the findings.
Summary and Synthesis of the Review
Association Between HPV and OSCC
Half (7/13) of the studies concluded with a positive association for HPV with OSCC (Additional file 1). Six studies in India (6/10) and one study in Pakistan (50%—1/2) reported a possible association. However, the rest of the studies failed to establish an association between HPV infection and OSCC including the study in Bangladesh [24]. Kundu et al. [16] and Dhanapal et al. [22] report HPV infection to be one of the important risk factors for OSCC. Zil-e-Rubab et al. [17] found HPV 16/18 co-infection in the oral rinse to have a higher chance to develop OSCC as compared to those who did not have HPV (adjusted odds ratio: 21.4, 95% CI 5.7–80.2; P < 0.001). Mondal et al. [25] reports a 3.72-fold (95% CI 2.11–6.56; P < 0.0001) increase in the risk of OSCC due to HPV infection. Chaudhary et al. [26] showed a significant association of HPV-16 in higher grade OSCC cases (P < 0.021). Kulkarni et al. [27] and Mathew et al. [28] showed a high prevalence in OSCC.
Common HPV Types and Sites in OSCC
Kundu et al. [16], Singh et al. [20], Khyani [21], Chaudhary et al. [26] and Mathew et al. [28] showed HPV 16 to be the most common type implicated in HPV infection associated with OSCC. However, Dhanapal et al. [22] and Mondal et al. [25] showed HPV 18 infection to be the most common type while Zil-e-Rubab et al. [17] showed HPV 16/18 combined infection to be the most common type. According to Kundu et al. [16], Rajesh et al. [18], Laprise et al. [19], Singh et al. [20], Patel et al. [23] and Mathew et al. [28], buccal mucosa was the most common site of oral cancer. Further, Kundu et al. [16] reported buccal mucosa as the only HPV infected site while Mathew et al. [28] finds that 62.5% of OSCC to be positive for HPV type 16, 56.25% for HPV type 18, and 37.5% for co-infection in the buccal mucosa.
HPV Association with Other Factors
Kundu et al. [16] showed that interactions among HPV and NELL1 variant rs1670661 with age and gender could augment the risk of both non-tobacco- and tobacco-related OSCC, respectively. Singh et al. [20] showed HPV presence was significantly associated with male gender, pan masala chewing and the majority (91%) of HPV positive cases had a history of tobacco consumption. Also, Dhanapal et al. [22] showed patients with HPV positivity to have a history of tobacco habits.
Studies Showing No Association Between HPV Infection and OSCC
Singh et al. (North India) [20] and Khyani (Pakistan) [21] did not show any association between HPV infection and OSCC. Rajesh et al. (South India) [18], Laprise et al. (South India) [19] and Patel et al. (West India) [23] did not find any OSCC cases positive for HPV while Akhter et al. [24] found only one case positive out of 34 OSCC cases in Bangladesh. Singh et al. [20] finds a confounding effect of tobacco in HPV positive cases. However, Khyani [21] finds HPV to be a co-factor role rather than just a passenger virus.
Discussion
Only 13 studies on the association of HPV and OSCC were found from the literature review, and all were from South Asia and none from Central Asia. The participants or the samples of the review were recruited from institutions of particular region of a country which did not represent the general population (Additional file 1) making it difficult to generalize the data. The reviewed studies had conflicting evidence on HPV associated OSCC. Further, the findings were not clear if HPV infection occurred before the occurrence of OSCC as the evidence is from cross-sectional studies. Thus, it is impossible to find a causal relationship between HPV and OSCC. The high incidence of tobacco consumption, either chewed or smoked, in South Asia makes it difficult to reach any conclusion on the significance of HPV infection in OSCC. Also, the confounding effects of the well-known risk factors for OSCC (tobacco, chewing tobacco, alcohol, HPV, male gender, old age, immunodeficiency status and poor oral hygiene) were not addressed using an appropriate statistical analysis. Moreover, it was evident that the studies were not sufficiently powered to detect the presence of HPV as an independent risk factor.
All the selected articles were cross-sectional studies which was probably due to the nature of our review question. Further, oral swab HPV detection could have led to over-diagnosis due to the transient presence of the virus. Lack of non-English language studies and the inability to access additional scientific databases could have minimised the chances of obtaining few more articles relevant to the review. Moreover, only articles published on adults aged ≥ 18 years within the last 10 years were included. Therefore, data were limited and did not include details on HPV related OSCC among children and adolescents. However, the present review provides a roadmap towards the preferred study designs like case control studies that may ultimately answer the review question more definitively.
Conclusion
The review had conflicting evidence on human papillomavirus associated oral squamous cell carcinoma among participants of South Asia. Future studies are essential among people of South-central Asian countries who are genetically and culturally different and in places where HPV related cancers are a concern.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1 - Data sheet of the review (DOCX 28 kb)
Additional file 2 - Quality assessment (DOCX 15 kb)
Additional file 3 - PRISMA 2009 checklist (DOCX 28 kb)
Abbreviations
- HPV
Human papillomavirus
- LMIC
Low or middle-income countries
- OSCC
Oral squamous cell carcinoma
- PRISMA
Preferred reporting items for systematic survey and meta-analysis
Author’s Contribution
DR conceived the idea and designed the review. All authors were involved in data collection. DR performed a comprehensive literature search. DR independently screened the titles and abstracts of all identified studies for selection, according to the inclusion criteria. The selected study was independently reviewed by BW and RK to confirm the eligibility. DR performed the data extraction and analysis. DR wrote the manuscript. BW and RK critically revised it. All authors approved the final manuscript.
Funding
The study was self-funded.
Availability of Data and Materials
All data generated or analysed during this study are included in this published article (and its additional files).
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Devarajan Rathish, Email: rathishdeva@gmail.com.
Buddhika Wijerathne, Email: buddhikatbw@gmail.com.
Rabia Khan, Email: rabiaikhan@gmail.com.
References
- 1.Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Bull World Health Organ. 1971;49(4):509–538. [PubMed] [Google Scholar]
- 2.Vithana C, Linhart C, Taylor R, Morrell S, Azim S. Trends in Sri Lankan cause-specific adult mortality 1950–2006. BMC Public Health. 2014;14:644. doi: 10.1186/1471-2458-14-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marshall SJ. Developing countries face double burden of disease. Bull World Health Organ. 2004;82(7):556. [PMC free article] [PubMed] [Google Scholar]
- 4.ACS (2015) 3rd Edition, Global Cancer Facts and Figures. American Cancer Society, Atlanta, Georgia. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/global-cancer-facts-and-figures/global-cancer-facts-and-figures-3rd-edition.pdf. [Cited 31 Oct 2018]
- 5.WHO (2018) Oral Cancer. World Health Organization, Geneva, Switzerland. http://www.who.int/cancer/prevention/diagnosis-screening/oral-cancer/en/. [Cited 28 Oct 2018]
- 6.Gupta N, Gupta R, Acharya AK, Patthi B, Goud V, Reddy S, Garg A, Singla A. Changing trends in oral cancer—a global scenario. Nepal J Epidemiol. 2016;6(4):613–619. doi: 10.3126/nje.v6i4.17255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hussein AA, Helder MN, de Visscher JG, Leemans CR, Braakhuis BJ, de Vet HCW, Forouzanfar T. Global incidence of oral and oropharynx cancer in patients younger than 45 years versus older patients: a systematic review. Eur J Cancer. 2017;82:115–127. doi: 10.1016/j.ejca.2017.05.026. [DOI] [PubMed] [Google Scholar]
- 8.ASCO (2018) Oral and oropharyngeal cancer: risk factors and prevention. American Society of Clinical Oncology, Virginia, United States. https://www.cancer.net/cancer-types/oral-and-oropharyngeal-cancer/risk-factors-and-prevention. [Cited 4 Oct 2018]
- 9.Bansal A, Singh MP, Rai B. Human papillomavirus-associated cancers: a growing global problem. Int J Appl basic Med Res. 2016;6(2):84–89. doi: 10.4103/2229-516X.179027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Souza G, Kreimer AR, Viscidi R, Pawlita M, Fakhry C, Koch WM, Westra WH, Gillison ML. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356(19):1944–1956. doi: 10.1056/NEJMoa065497. [DOI] [PubMed] [Google Scholar]
- 11.Gillison ML, D’Souza G, Westra W, Sugar E, Xiao W, Begum S, Viscidi R. Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst. 2008;100(6):407–420. doi: 10.1093/jnci/djn025. [DOI] [PubMed] [Google Scholar]
- 12.Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, Liu L, Lynch CF, Wentzensen N, Jordan RC, Altekruse S, Anderson WF, Rosenberg PS, Gillison ML. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294–4301. doi: 10.1200/JCO.2011.36.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sathish N, Wang X, Yuan Y. Human papillomavirus (HPV)-associated oral cancers and treatment strategies. J Dent Res. 2014;93(7 Suppl):29S–36S. doi: 10.1177/0022034514527969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hillen MA, Medendorp NM, Daams JG, Smets EMA. Patient-driven second opinions in oncology: a systematic review. Oncologist. 2017;22(10):1197–1211. doi: 10.1634/theoncologist.2016-0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kundu S, Ramshankar V, Verma AK, Thangaraj SV, Krishnamurthy A, Kumar R, Kannan R, Ghosh SK. Association of DFNA5, SYK, and NELL1 variants along with HPV infection in oral cancer among the prolonged tobacco-chewers. Tumor Biol. 2018;40(8):101042831879302. doi: 10.1177/1010428318793023. [DOI] [PubMed] [Google Scholar]
- 17.Zil-e-Rubab, Baig S, Zaman U, Lucky MH. Human papilloma virus 16/18: fabricator of trouble in oral squamous cell carcinoma. Int J Infect Dis. 2018;69:115–119. doi: 10.1016/j.ijid.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 18.Rajesh D, Mohiyuddin SMA, Kutty AVM, Balakrishna S. Prevalence of human papillomavirus in oral squamous cell carcinoma: a rural teaching hospital-based cross-sectional study. Indian J Cancer. 2017;54(3):498–501. doi: 10.4103/ijc.IJC_272_17. [DOI] [PubMed] [Google Scholar]
- 19.Laprise C, Madathil SA, Allison P, Abraham P, Raghavendran A, Shahul HP, ThekkePurakkal A-S, Castonguay G, Coutlée F, Schlecht NF, Rousseau M-C, Franco EL, Nicolau B. No role for human papillomavirus infection in oral cancers in a region in southern India. Int J Cancer. 2016;138(4):912–917. doi: 10.1002/ijc.29827. [DOI] [PubMed] [Google Scholar]
- 20.Singh V, Husain N, Akhtar N, Kumar V, Tewari S, Mishra S, Misra S, Khan MY. Do human papilloma viruses play any role in oral squamous cell carcinoma in North Indians? Asian Pacific J Cancer Prev. 2015;16(16):7077–7084. doi: 10.7314/APJCP.2015.16.16.7077. [DOI] [PubMed] [Google Scholar]
- 21.Khyani IAM, Qureshi MA, Mirza T, Farooq MU. Salivary detection of human papilloma virus 16 and 18 in pre-malignant and malignant lesions of oral cavity: is it feasible in Pakistani context of socio-cultural taboos? Pak J Med Sci. 2015;31(5):1104–1109. doi: 10.12669/pjms.315.7093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dhanapal R, Ranganathan K, Kondaiah P, Devi RU, Joshua E, Saraswathi TR. High-risk human papilloma virus in archival tissues of oral pathosis and normal oral mucosa. Contemp Clin Dent. 2015;6(2):148–152. doi: 10.4103/0976-237X.156033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel KR, Vajaria BN, Begum R, Desai A, Patel JB, Shah FD, Shukla SN, Patel PS. Prevalence of high-risk human papillomavirus type 16 and 18 in oral and cervical cancers in population from Gujarat, West India. J Oral Pathol Med. 2014;43(4):293–297. doi: 10.1111/jop.12147. [DOI] [PubMed] [Google Scholar]
- 24.Akhter M, Ali L, Hassan Z, Khan I. Association of human papilloma virus infection and oral squamous cell carcinoma in Bangladesh. J Health Popul Nutr. 2013;31(1):65–69. doi: 10.3329/jhpn.v31i1.14750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mondal R, Ghosh SK, Choudhury JH, Seram A, Sinha K, Hussain M, Laskar RS, Rabha B, Dey P, Ganguli S, NathChoudhury M, Talukdar FR, Chaudhuri B, Dhar B. Mitochondrial DNA copy number and risk of oral cancer: a report from Northeast India. PLoS ONE. 2013;8(3):e57771. doi: 10.1371/journal.pone.0057771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaudhary AK, Pandya S, Singh M, Singh M, Mehrotra R. Identification of high-risk human papillomavirus-16 and -18 infections by multiplex PCR and their expression in oral submucous fibrosis and oral squamous cell carcinoma. Head Neck Oncol. 2013;5(1):4. [Google Scholar]
- 27.Kulkarni SS, Kulkarni SS, Vastrad PP, Kulkarni BB, Markande AR, Kadakol GS, Hiremath SV, Kaliwal S, Patil BR, Gai PB. Prevalence and distribution of high risk human papillomavirus (HPV) Types 16 and 18 in Carcinoma of cervix, saliva of patients with oral squamous cell carcinoma and in the general population in Karnataka, India. Asian Pac J Cancer Prev. 2011;12(3):645–648. [PubMed] [Google Scholar]
- 28.Mathew A, Mody R, Patait M, Razooki A, Varghese N, Saraf K. Prevalence and relationship of human papilloma virus type 16 and type 18 with oral squamous cell carcinoma and oral leukoplakia in fresh scrappings: a PCR study. Indian J Med Sci. 2011;65(5):212. doi: 10.4103/0019-5359.106612. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 - Data sheet of the review (DOCX 28 kb)
Additional file 2 - Quality assessment (DOCX 15 kb)
Additional file 3 - PRISMA 2009 checklist (DOCX 28 kb)
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its additional files).