Abstract
Plasma cell granuloma is a rare, benign, space occupying lesions occurring after recurrent infections. It most commonly involves young adults with lungs being the most common site. They are usually rounded masses with bony expansion and destruction without any life threatening complications and surgery being the best choice of treatment. Here we reported a 33 year-old female with plasma cell granuloma of the maxillary sinus treated with surgery and no recurrence has been noted.
Keywords: Xanthoma , Pseudotumour, Granuloma, Plasma cells, Maxillary sinus
Introduction
Various terms have been used for plasma cell granuloma that includes mast cell granuloma, Xanthogranuloma, Xanthoma, Histiocytoma and Inflammatory pseudotumor [1]. Inflammatory pseudotumor or plasma cell granuloma is the benign, chronic inflammatory condition of unknown origin characterized by the presence of plasma cells, acute and chronic inflammatory cells with fibrous tissue without classical granuloma formation. It most commonly occurs in young adults. These mimic as invasive malignant tumours and are expansile with bony changes of erosion, sclerosis and remodellingg [2]. These tumours are more aggressive radiologically than clinically.
Case History
A 33 year-old female presented to our outpatient department with no known comorbidities with complaints of right-sided headache for 6 months, trismus and toothache for 1 month. There was no history of nasal trauma, surgery or any other nasal complaints. There was no history of diminution of vision, diplopia, proptosis, cheek swelling, photophobia or epiphora. On physical examination, the external osseocartilaginous framework and vestibule were normal. Anterior rhinoscopy revealed high deviated nasal septum to right with bilateral inferior turbinate hypertrophy. The posterior rhinoscopy examination was normal. On Oral cavity examination, the patient was having grade 1 trismus with the rest of the examination was normal. Ophthalmological examination was also normal with vision, extraocular movements and corneal reflex.
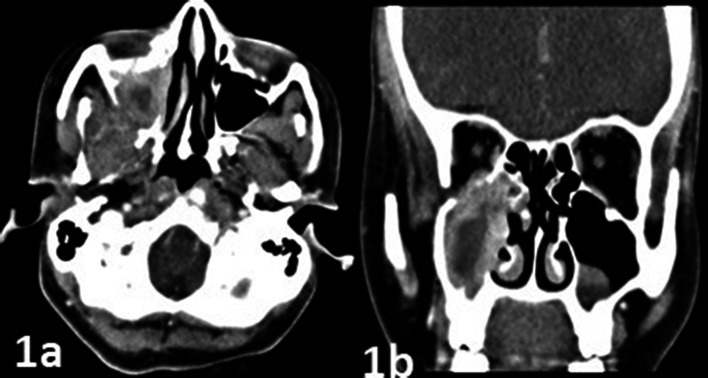
Contrast-Enhanced Computed Tomography nose and paranasal sinuses revealed heterogeneously enhancing mucosal thickening with central non-enhancing areas with widening of osteomeatal complex in the right maxillary sinus. Soft tissue thickening with bony erosion and focal defects were noted in the floor of the orbit and posterior wall of right maxillary sinus indicating the involvement of Orbit (extraconal) and Infratemporal fossa(Fig. 1a and b). There was no intraconal orbital or intracranial extension. Possibilities of fungal sinusitis or malignancy were considered.
Fig. 1.
CECT showing heterogeneously enhancing mucosal thickening with central non enhancing areas with the erosion of the posterior wall of the right maxillary sinus (a); erosion of floor of orbit (extraconal) (b)
The patient underwent right Inferior Meatal Antrostomy with biopsy under local anaesthesia. The biopsy was reported as plasma cell granuloma. X ray of the long bones and skull were normal. Bence Jones protein was negative. Then the patient was planned for right medial maxillectomy under general anaesthesia. On Diagnostic Nasal Endoscopy, reddish infiltrative mass was present in right maxillary sinus extending to anterior ethmoids and inferior turbinate. Using microdebrider, the mass was completely debrided and medial wall of the right maxillary sinus was removed.
The biopsy report was consistent with plasma cell granuloma with diffuse infiltration with sheets of plasma cells along with few lymphocytes, neutrophils and eosinophils with areas of fibrosis and fibroblastic proliferation (Fig. 2a and b). CD38 & 138 was positive for plasma cells and CD 3 & 20 was positive for lymphocytes (Fig. 3a and b). Kappa and lambda were non- contributory. One year follow up of the patient showed no recurrence.
Fig. 2.
Section showing tissue lined by respiratory epithelium showing sheets of plasma cells,10X, HPE (a); sheets of plasma cells,40x, HPE (b) (black arrow)
Fig. 3.
Section showing sheet of plasma cells with CD38 positive IHC, 40X (a); CD138 positive IHC, 20X (b)
Discussion
Plasma cell granuloma was first described by Bahadori and Liebowin in 1973 [3]. It most commonly occurs in the lungs; orbit and upper airways in extrapulmonary site. Larynx, particularly glottis (vocal cords) is the most common site for head and neck IMT [2]. The occurrences of inflammatory pseudotumor in the thyroid, periodontal region, esophagus, epiglottis, palatine tonsil and dura have also been reported. Incidence of extrapulmonary cases has been found to be less than 5% [3].
Pettinato et al. first coined the term IMT as the primary component of the lesion are proliferative, inflammatory fibroblastic and myofibroblastic cells, not the specific inflammatory cells [2, 4]. It has been recently proved to be true neoplasms by oncogenetics because it shows positive for Anaplastic Lymphoma Kinase(ALK) in immunohistochemistry [5, 6]. But only 0–4% of cases of sinonasal tract show positivity for ALK [7].
Micheal et al.first reported a case of plasma cell granuloma of the maxillary sinus which was treated with both surgery and radiotherapy [8]. Taskapilioglu reported isolated plasma cell granuloma of sphenoid sinus that presented with abducens nerve palsy [9].
Etiology
Previous surgery, trauma, recurrent regional infections are the precipitating factors for IMT. The exact pathogenesis is not clear but it may be attributed as a post-inflammatory reparative reaction, response to an acute infection or low-grade malignancy of spindle cells. It has been stated that viral aetiology including Epstein Barr Virus and Human Herpes Virus (HHV8) may also be involved in pathogenesis [7].
Clinical Presentation
Though IMT of the maxillary sinus is rare, it often presents as a soft tissue mass filling entire maxillary sinus presenting as nasal obstruction or discharge or epistaxis with anosmia, or with aggressive invasion to nearby regions including orbit, pterygopalatine fossa, infratemporal fossa, cheek or intracranial regions presenting as proptosis, trismus,cheek swelling, tooth ache or pulp necrosis of maxillary teeth [7]. Huang et al. reported two cases of intracranial extension from the disease arising from the nasal cavity [3].
Histology
Macroscopically, these tumours are smooth-surfaced large masses with various degrees of extension into the structure of origin and nearby structures. It mimics malignancy clinically.
In 2002, WHO defined Inflammatory Myofibroblastic Tumour as benign, intermediate, or rarely metastasizing soft tissue tumour composed of myofibroblastic spindle cells admixed with inflammatory plasma cells, eosinophils and lymphocytes [1]. Histopathologically, the lesion is composed mainly of mesenchymal cells and different inflammatory cells on the oedematous, myxoid connective tissue with very thin capillaries background.
Immunohistochemistry reveals almost all tumours are positive for vimentin, 80–90% positive for Smooth Muscle Actin (SMA) and 60–70% for desmin and calponin [1]. The presence of Anti actin antibody reveals the muscular origin of plasma cell granuloma [9].
Coffin et al. [10] described three basic histological patterns of plasma cell granuloma in his study of extrapulmonary inflammatory myofibroblastic tumours. 1. Loosely arranged spindle cells with myxoid background and granulation tissue resembling nodular fasciitis 2. Compactly arranged spindle cells with collagen and various inflammatory cells (plasma cells, lymphocytes and eosinophils) resembling myogenic or fibrohistiocytic neoplasm 3.Sparsely cellular plate-like collagen resembles scar or desmoid fibromatosis.
Radiology
Contrast-Enhanced Computed Tomography shows heterogeneous soft tissue density whereas Magnetic Resonance Imaging shows isointense in T1 imaging and mild hyperintensity in T2 images because of variable tissue components. In T2 imaging, hyperintense or hypointense depends on the amount of fibrous tissue [11].
Imaging modalities can help in the diagnosis of the disease, delineate the extent of the tumour and predict tumour resectability. But a histopathological examination of the disease helps in confirming the diagnosis.
Differential Diagnosis
Maxillary sinus malignancy, fungal sinusitis, granulomatous diseases, sarcoidosis and collagen vascular disorders [12].
Treatment
High dose corticosteroids, surgical treatment by complete excision of the tumour and radiotherapy are the treatment of choices for head and neck plasma cell granuloma. Because of extensive surgical resection, steroids are considered to be the first line of management. But recurrences are reported following steroid therapy. So next comes the complete resection of the tumour followed by RT as last treatment. Newlin reported stereotactic radiosurgery as the treatment of choice in maxillary sinus granuloma [13]. Possibility of local recurrence being around 25% and distant metastasis around 5% have been noted [6]. Incomplete excision of the tumor results in an increased chance of recurrence.Other treatment modalities includes corticosteroids, chemotherapy and radiotherapy. There are few published data about the use of radiotherapy in lung lesions. The doses are speculative but 1.8–2 Gy fractions of total 40-50 Gy appear to be the most appropriate for tumour control in local lesions. Despite having an extensive clinical and radiological presentation, sinonasal IPT has a good prognosis. Malignant transformation of sinonasal IPT to sarcoma has been never reported in the literature [14].
Conclusion
Plasma cell granuloma presents with features of malignancy both clinically and radiologically but histopathology provides the definite diagnosis. Surgery with Complete removal of tumour is the best treatment of choice. Recurrences are uncommon with complete removal but that can be treated with radiotherapy or corticosteroids. Despite their recurrence following treatment, they usually follow benign course.
Funding
The authors did not receive support from any organization for the submitted work.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent.
Obtained from the patient for participation.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fletcher CD, Unni KK, Mertens F, editors. Pathology and genetics of tumours of soft tissue and bone. Iarc; 2002.
- 2.Yuan X-P, Li C-X, Cao Y, Singh S, Zhong R. Inflammatory myofibroblastic tumour of the maxillary sinus: CT and MRI findings. Clin Radiol. 2012;67(12):e53–e57. doi: 10.1016/j.crad.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Ajibade DV, Tanaka IK, Paghda KV, Mirani N, Lee HJ, Jyung RW. Inflammatory pseudotumor (plasma cell granuloma) of the temporal bone. Ear Nose Throat J. 2010;89(7):E1–3. doi: 10.1177/014556131008900701. [DOI] [PubMed] [Google Scholar]
- 4.Pettinato G, Manivel JC, De Rosa N, Dehner LP. Inflammatory myofibroblastic tumor (plasma cell granuloma) Clinicopathologic study of 20 cases with immunohistochemical and ultrastructural observations. Am J Clin Pathol. 1990;94(5):538–546. doi: 10.1093/ajcp/94.5.538. [DOI] [PubMed] [Google Scholar]
- 5.Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: where are we now? J Clin Pathol. 2008;61(4):428–437. doi: 10.1136/jcp.2007.049387. [DOI] [PubMed] [Google Scholar]
- 6.Coffin CM, Hornick JL, Fletcher CDM. Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol. 2007;31(4):509–520. doi: 10.1097/01.pas.0000213393.57322.c7. [DOI] [PubMed] [Google Scholar]
- 7.Werner RL, Castle JT. Inflammatory myofibroblastic tumor of the nasal cavity. Head Neck Pathol. 2015;10(3):336–339. doi: 10.1007/s12105-015-0662-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seider MJ, Cleary KR, van Tassel P, Alexanian R, Schantz SP, Frias A, et al. Plasma cell granuloma of the nasal cavity treated by radiation therapy. Cancer. 1991;67(4):929–932. doi: 10.1002/1097-0142(19910215)67:4<929::AID-CNCR2820670412>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 9.Taskapilioglu O, Yurtogullari S, Yilmaz E, Hakyemez B, Yilmazlar S, Tolunay S, et al. Isolated sixth nerve palsy due to plasma cell granuloma in the sphenoid sinus: case report and review of the literature. Clin Neuroradiol. 2011;21(4):235–238. doi: 10.1007/s00062-011-0054-9. [DOI] [PubMed] [Google Scholar]
- 10.Coffin CM, Humphrey PA, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor: a clinical and pathological survey. Semin Diagn Pathol. 1998;15(2):85–101. [PubMed] [Google Scholar]
- 11.Som PM, Brandwein MS, Maldjian C, Reino AJ, Lawson W. Inflammatory pseudotumor of the maxillary sinus: CT and MR findings in six cases. Am J Roentgenol. 1994;163(3):689–692. doi: 10.2214/ajr.163.3.8079869. [DOI] [PubMed] [Google Scholar]
- 12.Soysal V, Yiğitbaşı OG, Kontaş O, Kahya H, Guney E. Inflammatory myofibroblastic tumor of the nasal cavity: a case report and review of the literature. Int J Pediatr Otorhinolaryngol. 2001;61(2):161–165. doi: 10.1016/S0165-5876(01)00561-4. [DOI] [PubMed] [Google Scholar]
- 13.Newlin HE, Werning JW, Mendenhall MW. Plasma cell granuloma of the maxillary sinus: a case report and literature review. Head Neck. 2005;27(8):722–728. doi: 10.1002/hed.20196. [DOI] [PubMed] [Google Scholar]
- 14.Ruaux C, Noret P, Godey B. Inflammatory pseudotumour of the nasal cavity and sinuses. J Laryngol Otol. 2001;115(7):563–566. doi: 10.1258/0022215011908234. [DOI] [PubMed] [Google Scholar]