Abstract
Background
Sleep problem is a highly prevalent health issue among pediatric populations across the world. In this review, we aimed to identify risk factors contributing to sleep deficiency and poor sleep hygiene in children. Potential biological, psychosocial, and environmental mechanisms as well as research gaps in the literature are also discussed.
Data sources
A comprehensive search for relevant English language full-text, peer-reviewed publications was performed focusing on pediatric sleep studies from prenatal to childhood and adolescence in a variety of indexes in PubMed, SCOPUS, and Psych Info. Both relevant data based and systematic reviews are included.
Results
This paper summarizes many risk factors for childhood sleep problems, including biological (e.g., genetics, gender, age and puberty, prenatal factors, postnatal factors); nutritional (e.g., macronutrients, micronutrients, omega-3 fatty acids, obesity); environmental (e.g., heavy metals, noise, light, air pollution); interpersonal (e.g., family, exposure to violence, screen media use, physical injury); and community/socioeconomic variables (e.g., racial/ethnicity and cultural factors, neighborhood conditions and socioeconomic status, school factors, public health disasters/emergencies), to better understand the development of sleep problems in children.
Conclusions
Poor childhood sleep is a multifactorial issue affected by a wide range of prenatal and early-life biological, environmental, and psychosocial risk factors and contributors. A better understanding of these risk factors and their mechanisms is an important first step to develop future research and prevention programs focusing on pediatric sleep problems.
Keywords: Child sleep, Pediatrics, Risk factor, Mechanisms
Introduction
Sleep, the primary brain activity during development, encompasses about 40% of a child’s day throughout childhood and adolescence [1] and is vitally important to children’s health and well-being. However, sleep deficiency has become a rising public health concern [2], affecting 20%–60% of all children globally [3–5]. Sleep deficiency includes insufficient sleep duration, irregular timing of sleep, poor sleep quality (e.g., perceived poor sleep, objectively assessed sleep fragmentation), and sleep/circadian disorders (e.g., insomnia, obstructive sleep apnea) [6].
Many factors contribute to a child’s sleep deficiency, including early childhood risk factors such as genetic, prenatal, postnatal, environmental, psychosocial, and other risk factors. Furthermore, sleep deficiency has been shown to adversely impact physical health [7], behavior [8–10], emotional well-being [9, 11, 12], cognition [13, 14], psychopathology [13, 15, 16], and familial relationships [7, 17].
While several previous studies have systematically reviewed individual factors related to childhood sleep, this review aims to integrate many different aspects into one paper and provide a comprehensive overview. The review focused on analyzing the current literature and knowledge syntheses on particular risk factors. Potential biological, psychosocial, and environmental mechanisms and current literature gaps are also briefly discussed. Understanding the risk factors will inform public health practice for sleep screening and prevention/intervention, thus improving sleep-related child development and health.
Search strategies
A comprehensive literature search for relevant English language full text, peer-reviewed publications was performed focusing on pediatric sleep studies from prenatal to childhood and adolescence in a variety of indexes in PubMed, SCOPUS, and Psych Info. Searches were conducting using keywords such as “child”, “adolescent”, “pediatric”, “sleep deficiency”, “sleep hygiene”, “risk factors”, and “mechanisms”. We grouped our findings from the literature on risk factors for childhood sleep problems into five broad categories, and we further conducted searches specific to each category that we found, with additional keywords including biological (e.g., “genetics”, “prenatal”, “postnatal”), nutritional (e.g., “obesity”), environmental (e.g., “noise”, “light”), interpersonal (e.g., “family”, “screen media”), and community/socioeconomic variables (e.g., “socioeconomic status”, “school”).
Eligibility criteria
We included relevant empirical studies (cross-sectional, longitudinal studies or clinical trials) and systematic reviews on sleep health in infants, children and adolescents published in English. While we focus our search on literature from the past two decades, we also include that which was published earlier if highly relevant and well-cited.
Exclusion criteria
We excluded following types of articles: narrative review, expert opinion, and case report. We also excluded studies focused on participants >18 years of age.
Childhood sleep and measurement
Sleep deficiency in children encompasses several different manifestations, such as altered sleep duration (e.g., short sleep), poor sleep quality, and sleep disorders. Of them, common sleep disorders include insomnia, hypersomnolence (excessive sleepiness), sleep-related breathing and movement disorders, circadian rhythm sleep–wake disorders and parasomnias (disturbances during sleep, e.g., sleep walking). Table 1 summarizes the definitions and manifestations of common sleep deficiency types in childhood. These sleep problems occur differentially across development. For instance, whereas nighttime awakening is most prevalent in infancy and early childhood, older children and adolescents more commonly have difficulty falling asleep [18]. Sleep deficiency problems have also been shown to persist through development, with sleep deficiency manifestations in infancy continuing into early childhood, those from early childhood into middle school, and those from middle school into later adolescence [19].
Table 1.
Definitions and manifestations of common childhood sleep deficiency problems
| Sleep deficiency | Definition and manifestation |
|---|---|
| Sleep duration | The national sleep foundation [200] recommends newborn (0–3 mon) and infant (4–11 mon) to spend 14–17 h and 12–15 h a day asleep, respectively. The suggested duration subsequently decreases with age: 11–14 h for toddlers, 10–13 h for preschoolers, 9–11 h for school-age children, and 8–10 h for adolescents |
| Sleep quality |
Despite no consensus, sleep quality is usually defined based on sleep continuity, sleepiness, sleep architecture and daytime behaviors. A global approach for indexing sleep quality often involves self-rating indices that reflect an individual’s satisfaction with sleep Objectively, the National Sleep Foundation identifies various factors that indicate overall sleep quality, including spending at least 85% of time in bed asleep, falling asleep within 30 min, waking at most once per night, and being awake for 20 min or less after falling [201] |
| Sleep disorders |
Insomnia is defined as difficulty initiating and maintaining sleep, or waking up earlier than desired with daytime impairment despite adequate opportunity to sleep [202]. Childhood insomnia is usually characterized by the child’s inability or unwillingness to fall asleep or return to sleep in the absence of specific conditions (e.g. parent rocking) or when parents fail to set appropriate limits [203]. Sleep disordered breathing, characterized by respiration irregularities during sleep [204], is expressed most frequently as obstructive sleep apnea (OSA). OSA includes symptoms of snoring, labored/obstructed breathing, or daytime consequences such as sleepiness and hyperactivity. PSG is the gold standard for the diagnosis and classification of severity Parasomnias such as sleepwalking, sleep talking, nightmares, and sleep terrors, and affect up to 50% of children [203]. Sleepwalking, sleep talking, and sleep terrors (e.g. perceived intense fear, difficult to awaken from episode) usually occur in slow wave sleep (deep sleep). Nightmares, which may be associated with mood disorders or posttraumatic stress disorders, occurs during rapid eye movement (REM) sleep [203] Excessive daytime sleepiness: The AASM defines this as daily episodes of an irrepressible need to sleep or daytime lapses into sleep. While tiredness during the day is common, excessive sleepiness interferes with a child’s daily activities and function despite receiving sufficient sleep at night [205]. There is substantial overlap between pathological sleepiness (e.g. sleep disorder: narcolepsy) and sleep deprivation-related sleepiness Delayed sleep phase disorder (DSP) is a circadian rhythm disorder that manifests as a delay of the major sleep episode with respect to the patient’s desired timing or the societal norms (at least two hours of delay) [202]. Sleep quality is typically reported as normal when the individual sleeps at the delayed time. DSP is more common in adolescents and young adults [203] |
Sleep deficiency in children and adolescents can be measured, both objectively and subjectively, via child report and parents’ estimation. Despite discrepancies in sleep time and duration assessment between subjective and objective sleep measures (e.g., overestimation in self/parent reports) [20–23], perceived sleep experiences provide patient- or participant-centered information that cannot be characterized by quantified sleep indicators [24]. Because of cost-effectiveness, ease of use, and practicality, validated subjective instruments (self-report or parent report; Table 2) are widely used to measure sleep problems in community-based studies at scale [25, 26]. Key child sleep measures are outlined in Table 2.
Table 2.
Key measurement tools for sleep-related assessments in children and adolescents
| Reported sleep assessments | |||||
|---|---|---|---|---|---|
| Tools | Population | Measured factors | Report type | Number of total items | Primary use |
| Child behavior checklist (CBCL) [206] |
CBCL/1½ to 5: for children aged 1½ to 5 y CBCL/6 to 18: for children aged 6 to 18 y |
Eight behavioral areas anxious/depressed, withdrawn, somatic complaints, social problems, thought problems, attention problems, rule-breaking behavior, and aggressive behavior | Parent-report | 113 | Assess sleep behaviors and emotional problems and compare with other measures of sleep function to determine associative relationships between behavior and sleep |
| Child sleep health questionnaire [207] | School-aged children | Eight sleep domains: bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night wakings, parasomnias, sleep-disordered breathing, and daytime sleepiness, and total sleep disturbance score | Parent-report | 45 | Assess sleep health and various sleep disorders |
| Sleep disturbance scale for children [208] | School-aged children | Six factors related to sleep disorders: disorders of initiating and maintaining sleep (DIMS), sleep breathing disorders (SBD), disorders of arousal (DA), sleep wake transition disorders (SWTD), disorders of excessive somnolence (DOES), and sleep hyperhidrosis (SHY) | Parent-report | 27 | Assess sleep disorders |
| Pittsburgh sleep quality index [209] | Adolescents and adults | Subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction | Self-report | 19 | Assess sleep quality |
| Sleep diary and maternal report [210, 211] | School-aged children | Cosleeping, sleep quality and duration, and sleep problems including nighttime awakening | Maternal-report | N/A | Track child sleep habits |
| Insomnia severity index [212] | Adolescents (originally designed for adults) |
Perceived severity of insomnia symptoms (initial, middle, terminal), the degree of satisfaction with sleep, interference with daytime functioning, noticeability of impairment, and concern caused by the sleep problems |
Self-report | 7 | Screen insomnia symptoms |
| Pediatric daytime sleepiness scale [213] | Self-report | 8 | Assess daytime sleepiness | ||
| Epworth sleepiness scale (modified) [214] | Adolescents | Replacing the last item ‘‘in a car while stopped for a few minutes in traffic’’ with ‘‘doing homework or taking a test’’ | Self-report | 8 | Assess daytime sleepiness |
| Adolescent sleep hygiene scale [215–217] | Adolescents | Including 4 qualitative items to ascertain usual bedtime and wake time on weekdays and at weekends, and 28 quantitative items that are used to calculate 9 subscale scores: physiological, cognitive, emotional, sleep environment, daytime sleep, substances, sleep stability, bedtime routine and bed sharing | Self-report | 32 | Assess sleep Hygiene practice |
| Children’s report of sleep patterns [218, 219] | Children and adolescents | Three subscales: sleep patterns, sleep hygiene, and sleep disturbances | Self-report | 76 | Assess multiple sleep dimensions that are reflective of sleep disturbances |
| Systematic sleep analysis tools | |||||
| Polysomnography [220, 221] |
Measures sleep and wake states as well as stages, eye movements, and muscle tone during sleep via electroencephalography, electrooculography, and electromyography as well as respiratory disorders, parasomnias, epilepsy, narcolepsy, insomnia, and circadian rhythm disorders during sleep can be assessed using this methodology Requires technical expertise and an overnight stay in a sleep laboratory, is expensive, and does not measure subjective aspects of sleep such as perceptions of sleep and the sleep environment |
||||
| Actigraphy [222] |
Similarly uses objective measures of sleep and wake patterns using motion sensors as polysomnography Measured using a mobile device, actigraphy employs built-in scoring algorithms to detect sleep and wake phases, allowing it to be used in the home environment without excessive set-up or cost requirements. Clinically, 7–14 d of consecutive recording are recommended to capture both weekday and weekend sleep [222] |
||||
Risk factors associated with childhood sleep deficiency
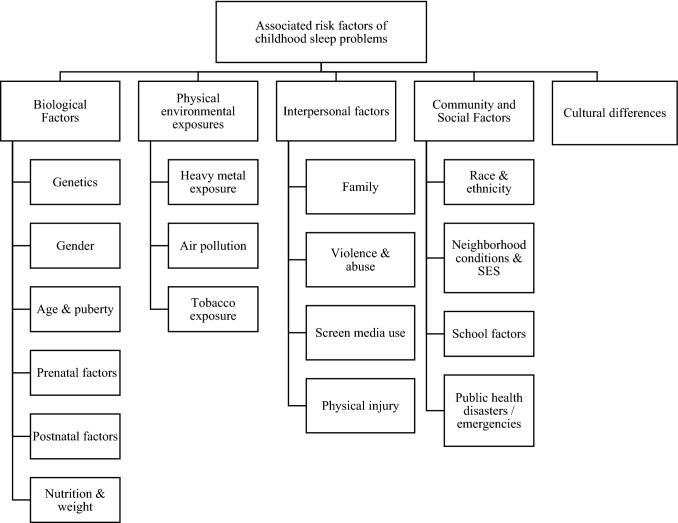
Early childhood is an important period during which a normal sleep-wakefulness cycle is developed. Exposure to biobehavioral, psychosocial, and environmental early-life risk factors could contribute to childhood sleep deficiency. In children, sleep onset latency (the amount of time it takes to fall asleep) may be influenced by bedtime resistance. Sleep problems in adolescents may be due to various adolescent-specific factors, such as pubertal changes in intrinsic sleep regulation (e.g., delayed melatonin onset phase) [27], increased school demands [28], greater access to and use of screen media [29–31], and substance use [30]. Guided by several models (i.e., socioecological/multilevel model [32]; biopsychosocial and contextual model [33]), we synthesized and summarized evidence from the literature on risk factors associated with child/adolescent sleep deficiency in five categories (i.e., biological, physical environmental exposures, interpersonal factors, community and social factors, cultural differences), which are displayed in Fig. 1. These risk factors, along with specific examples for each factor, are briefly discussed in this section.
Fig. 1.
Childhood sleep disturbances and associated factors
Biological factors
Genetics
Genetic factors may predispose children to various sleep pathologies. Evidence from twin studies illustrates this role of genetics in specific sleep-related issues, which include daytime and nighttime sleep duration as well as nighttime awakening. Notably, in a longitudinal study of 995 monozygotic and dizygotic twins, a strong genetic influence was observed on nighttime sleep duration at 6, 30, and 48 months. Notably, the contribution of genetics to sleep duration was most prevalent among children with persistently short sleep duration over the assessment period [34]. Laboratory studies have documented certain genes (BMAL1/Mop3, ABCC9) as potential biological mechanisms [35, 36]. Another study on a smaller population of monozygotic and dizygotic twins found that while additive genetic effects have a moderate impact on infant sleep duration in both nocturnal and diurnal sleep, shared environmental factors have a much more significant impact, almost double that of genetic factors[37]. Nevertheless, this area of research remains limited and requires further study to parse out how genetic and environmental factors interplay in influencing the physiological nature of childhood sleep.
Gender
Sex differences in child sleep outcomes have been widely studied, but the results remain inconclusive. Most studies report better sleep among girls, as boys have been shown to have lower sleep efficiency (the ratio of total sleep time to time in bed) [38], less time in bed [39], greater risk for sleep problems [40], and increased activity during sleep [38]. However, insomnia prevalence in one study among school-aged children was highest in girls aged 11–12 years [41]. Conversely, many studies report no significant gender differences in sleep onset [42], sleep duration [43], or other objective sleep measures [42], suggesting that further research is needed to elucidate these relationships.
Age and puberty
Sleep behavior changes drastically in early development, from infants to school-aged children to adolescents. Children sleep significantly earlier and for longer periods of time than adolescents [42] due to biological, psychosocial, and lifestyle factors that change with increased age [44]. Pubertal status was associated with changes in intrinsic sleep regulation (e.g., delayed melatonin onset phase) [27] and the tendency toward evening chronotype (e.g., later bed and rise time) [45]. Together with age-specific social/behavioral factors, up to 68.9% of adolescents report insufficient nighttime sleep duration and impaired sleep quality [46, 47], and high school students exhibit > 1-h differences in sleep/wake patterns between school and nonschool days on average [48]. These findings suggest the pervasiveness of chronic circadian misalignment (mismatch between an internal circadian clock and behavioral sleep schedule) in adolescents. These adolescent sleep difficulties translate into poor daytime functioning. Chronic poor adolescent sleepers report increased self-reported rates of feeling depressed, fatigued, moody, irritable, less rested, and more tense than their peers who are good sleepers [49]. Despite the tendency for shorter sleep duration in adolescence, sleep disorders may remain stable over time [50] sleep quality may actually improve with age and puberty status [50].
Prenatal factors
Sleep deficiency in children has been linked to prenatal maternal obesity [51] and maternal exposure to psychoactive substances, namely, alcohol [52, 53]. Specifically, sleep deficiency due to these prenatal exposures includes low sleep efficiency [54, 55], increased nighttime awakenings [55, 56], short sleep duration [54–56] and insomnia [57, 58]. A possible underlying factor may be that alcohol from the mother may alter the functioning of the fetal hypothalamic pituitary adrenal axis, a system involved in the regulation of sleep infrastructure [54, 59], thus disrupting normal sleep behavior. Future research is needed to tease out the trimester during which exposures may have the greatest impact to develop targeted interventions.
Similarly, maternal emotional health during pregnancy may also impact child sleep. Specifically, high levels of prenatal maternal anxiety and depression are associated with increased sleep deficiency [53, 60], including difficulty initiating and maintaining sleep, short sleep duration, and parasomnias [61, 62]. Conversely, higher levels of maternal happiness in the second and third trimesters are associated with fewer child sleep deficiency manifestations [63]. Although mechanistic pathways are not yet fully understood, it is possible that increased maternal stress experienced during the prenatal period increases glucocorticoid secretion, which may disrupt circadian activity of the developing fetus [62, 64].
Postnatal factors
Postnatal variables affecting infant physical health may also affect sleep behavior. Preterm birth affects both short-term and long-term sleep outcomes, resulting in greater arousability from sleep at 2–3 months [65, 66] as well as a greater risk of sleep-disordered breathing in later childhood (ages 8–11 years) [67, 68]. Additionally, breech birth and prolonged labor were associated with infant sleep difficulties [69]. Similarly, low birth weight (LBW) and shorter length at birth are associated with lower sleep efficiency during childhood and into adolescence [54, 69]. LBW can also have long-term consequences, as young adults born with LBW are more likely to snore and report other respiratory-related sleep disorders [70]. Certain birth stressors (i.e., prolonged labor, LBW, nonsingletons, and breech birth) were found to be negative predictors of sleep duration in adolescents [69].
Another possible postnatal contributor is breastfeeding. Currently, breastfeeding infants are reported to have less consolidated sleep [71], wake more frequently [72] and for longer duration [71] during the night, and have more difficulty sleeping alone at night [72]. This relationship may be moderated by parenting practices of nursing to sleep and returning to sleep during the night [71]. Future research is needed to investigate whether breastfed infants wake more frequently due to consuming less milk than bottle-fed infants or whether it is due to another factor involved in breastfeeding.
Postnatal maternal mental health has also been shown to affect child sleep, notably postpartum depression, which may greatly affect child development by parenting style and child‒parent relationships [73, 74]. In general, increased severity of maternal postnatal depression is associated with more deficiency symptoms [75, 76], increased risk of sleep disorders in infancy [75], and more reports of sleep disturbances in childhood [63]. However, the directionality of this relationship is still unknown. Whereas poor childhood sleep outcomes were demonstrated to be an effective predictor of maternal depression scores [76], childhood behavior has been shown to be a significant mediator of the relationship between maternal depression and child sleep [63]. Additionally, poor maternal sleep is associated with poor infant sleep outcomes, maternal postnatal depression, and family dysfunction, suggesting that maternal sleep outcomes could help explain the link between postnatal depression and poor childhood sleep.
Nutrition, dietary intake, and weight
Although prior work has largely focused on how sleep deficiency may be associated with subsequent dietary intake and metabolic outcomes [77], a growing body of work suggests the potential impact of both macronutrients and micronutrients as well as dietary intake factors, such as regularity and timing of eating, on sleep health [78, 79].
Macronutrients
Macronutrients such as carbohydrates and amino acids (e.g., tryptophan), may influence sleep-inducing neurotransmitters, such as serotonin, through tryptophan metabolism [80, 81]. Infants and children (0–6 years) who consume a lower amount of tryptophan at breakfast demonstrate longer sleep latency (the amount of time it takes to go from being fully awake to sleeping), difficulty falling asleep at bedtime, and difficulty being awakened in the morning [82]. Whereas children who ate a high glycemic-index, carbohydrate-based meal in the evening showed longer sleep duration at night [83], eating such a meal near bedtime (e.g., 1 hour before bedtime) was associated with frequent arousals and diminished sleep quality [79].
Micronutrient (e.g., iron and zinc) deficiencies have also been considered risk factors for sleep deficiency [84]. Infants with iron deficiency anemia experience more frequent nighttime awakenings and shorter total sleep duration [85], altered spindle patterns (e.g., reduced density, lower frequency, and longer interspindle intervals) of nonrapid eye movement sleep (NREM) sleep stage 2 and slow wave sleep during infancy [86], and altered distribution of NREM and rapid eye movement sleep at 4 years old [87] compared with better-nourished counterparts. Furthermore, lower serum zinc concentrations at both 3–5 years old and 11–14 years old are associated with insufficient sleep duration, decreased sleep efficiency, poor sleep quality and increased sleep disturbances [88]. Micronutrients are antagonists of excitatory neurotransmitters (wakefulness promoters) in the brain, such as the N-methyl-d-aspartate receptor [78, 89] and dopaminergic neurons [90], as well as agonists of inhibitory neurotransmitters (sleep promoters), such as gamma-aminobutyric acid (GABA) receptors [89], thereby potentially influencing the intrinsic sleep regulation process.
Omega-3 fatty acids
A recent meta-analysis also reported that omega-3 LC-PUFAs (high levels of which can be found in certain fish, seeds, and nuts) may improve sleep health in children with clinical levels of sleep deficiency but not in generally healthy children [91]. Omega-3 deficiency may affect melatonin production and neuronal membrane function in animal models, thus impacting sleep onset and maintenance [92–95]. However, more research is needed in this area to confirm such a relationship.
Obesity
With the increasing prevalence of obesity in children, a majority of studies have focused on the contributing role of sleep deficiency to obesity [96]. However, research also reports that obese adolescents experienced considerably poorer sleep outcomes (i.e., duration, quality, and daytime somnolence) than their peers of normal weight [12]. The exact underlying mechanisms are unclear but involve those at the biological and environmental levels (e.g., dietary intake, media use, physical activity) [12]. Further research should clarify the direction of the relationship between sleep and obesity.
Physical environmental exposures
Children are especially vulnerable to environmental exposure due to their developing physiology. The relationship between environmental exposures and sleep health is relatively underresearched, but emerging studies are beginning to show a link between the two. A recent comprehensive review summarized empirical evidence demonstrating that different antagonistic exposures, such as lead, pesticides, noise (e.g., road traffic), light, and airborne pollutants, predispose children to sleep deficiency during the prenatal and postnatal periods [97].
Early childhood lead exposure is associated with adolescent sleep deficiency [98]. Exposure during the night has been found to contribute not only to shorter sleep duration and other sleep deficiency manifestations in girls at age 7 [99] but also to later bedtimes in adolescents [100]. An example of such disturbances to sleep onset and duration has been found in continuous exposure to noise in the pediatric intensive care unit, which contributed to poor sleep in patients [101]. Light exposure, especially artificial light before bedtime, has been found to suppress melatonin release and to delay sleep onset, reduce sleep duration, and reduce alertness the next morning [102, 103].
A recent systematic review on air pollution exposure on sleep health across the lifespan highlighted the impact on children [104]. This review concluded that both indoor and outdoor air pollution contributed to respiratory-related sleep disorders (e.g., snoring, wheezing) in children. Evidence has also reflected that children are more susceptible to the effects of air pollution due to the immaturity of their nervous and immune systems as well as their respiratory anatomy [105]. Nevertheless, more research is needed to focus on the long-term effects of these exposures on child sleep.
Interpersonal factors: family, peers, behavior, and immediate environment
In addition to biological and early-life risk factors, a child’s immediate home environment as well as social relationships inside and outside the home may greatly impact sleep outcomes. Many of these factors may be modifiable and thus potential targets for improving child sleep behavior.
Family
Child sleep deficiency may affect parental sleep patterns and daytime functioning, which in turn may affect parental behaviors and bedtime routine as well as subsequent child sleep outcomes [106, 107]. One family-related factor affecting childhood sleep is cosleeping or sharing a bed with a parent [108]. Cosleeping is correlated with higher rates of nighttime sleep deficiency [109], including later bedtimes, shorter sleep duration [110], bedtime resistance, sleep anxiety, parasomnias [111], frequent and disruptive night awakening [112, 113], and behavior problems [114]. Furthermore, long-term children who were cosleepers still maintained sleep problems for an additional year post-initial interview compared to nonco-sleepers and children who stopped cosleeping [113]. Nevertheless, cosleeping is a complex issue that may involve several factors, including socioeconomic status due to lack of bed space, which alone may contribute to sleep deficiency in children. Cosleeping may also involve parental behavior, including lack of awareness of sleep hygiene [115] as well as their own anxiety about sleeping alone [107].
Sleep deficiency manifestations could also be associated with parent behavioral issues and parenting styles. Parental laxness [116] and low parental hardiness (i.e., psychological maturity) [117], or lack of emphasis on child self-regulation and autonomy, are significantly related to child sleep problems in toddlers. Furthermore, such adverse parenting styles (including lack of warmth as well as large inconsistencies in behavior and response to children’s behavior and intelligence) are also associated with low sleep quality and greater daytime sleepiness in adolescents [118]. On the other hand, enforcement of regular household rules, such as caffeine intake and child sleep routines, was associated with better sleep health among children and adolescents [119, 120]. Childhood sleep routines may also involve specific hygiene structures and timelines, communication through reading or storytelling, and physical connections through cuddling or rocking for younger children [121]. Sleep routines for this population can often be sustained through parental intervention. Additionally, improved mother–child and father-child relationship quality is associated with a longer duration of sleep in toddlers [122, 123]. Similarly, greater parental warmth [124] and parental encouragement of social maturity [125] are associated with longer sleep duration in young children, and consistent parenting similarly is a protective factor in children with ADHD [126] (a group that commonly has comorbid sleep disorders such as sleep-disordered breathing, insomnia, and circadian rhythm sleep disorders [127]), resulting in decreased sleep resistance and sleep anxiety. Thus, consistent parenting can especially encourage improved sleep in child populations that require specialized care.
A potential mechanism at the psychosocial and environmental level for the role of parental behavior on child sleep may be due to consistent, warm parenting styles allowing for increased child perception of comfort and security and thus greater ability to easily fall asleep [120]. Additionally, these positive parenting techniques reinforce child self-functioning and promote secure attachment styles, which has been linked to better sleep outcomes and lower risk for internalizing and externalizing behavior problems due to a child’s increased ability to self-soothe [128]. Assessments in primary pediatric care settings should include evaluations of children’s sleep routines and parenting styles and should provide advice to parents to promote child sleep health.
Violence and abuse
Exposure to domestic violence (i.e., partner violence), physical abuse, and/or sexual abuse has been found to be associated with sleep deficiency throughout childhood. In particular, domestic violence is linked to poor sleeping habits in infants and problems with bedwetting at night in children [129–132], and increased maternal psychopathology may be a mediator [132]. Sleep issues may further be a mediator between exposure to domestic violence during childhood and depression during adolescence. Research has shown that the relationship between experiencing domestic violence between household members and subsequent depression may be improved by tackling sleep problems first [133]. Living with domestic violence may result in sleep deficiency that persists even after the abuse has ended [134]. Similarly, children who have experienced either physical and/or sexual abuse report more sleep deficiency issues than children who are not abused [135, 136], and these effects on sleep are long-term [137, 138]. Specifically, victims of abuse demonstrate prolonged sleep latency, decreased sleep efficiency, increased nighttime activity and wakefulness, and decreased sleep duration as measured by surveys [135] and polysomnography [139, 140]. Physically abused children demonstrate worse sleep efficiency than sexually abused children [141]. Additionally, sexually abused children show poorer overall sleep quality, as measured by sleep difficulties [142–144] and daytime sleepiness [141]. Compared with controls, victims of sexual abuse also experience more disturbances during the night, including higher nocturnal activity [145], more parasomnias [146], and frequent nighttime awakening [147]. Furthermore, sexually abused girls report more sleep disturbances than boys [148], and there is a correlation between sleep disturbances in sexually abused girls and revictimization [131]. Future research is needed to investigate other adverse childhood experiences and different mechanisms through which these experiences impact child sleep as well as increase the incorporation of assessments for exposure to violence and abuse.
Screen media use
Current literature reports that sleeping with a screen device (especially a mobile phone) in the bedroom is negatively associated with sleep duration [119, 149]. Greater use of screen media similarly negatively influences sleep outcomes [31]. A cross-sectional study [150] found that increased screen media use was associated with longer sleep onset, shorter sleep duration, and increased daytime sleepiness in infants and toddlers. Several studies reported that sleep duration decreased significantly in infants with each additional hour of screen use [150–152], and in toddlers and young children, both increased screen media use at night and viewing of violent content during the day were associated with increased sleep deficiency issues [153]. For school-aged children, greater screen media use, which includes an increased variety of sources—such as mobile phones, computers, television, Internet browsing, electronic gaming, and more [154]—has most commonly been associated with shorter sleep duration and delayed bedtime [155]. Children and adolescents with longer screen usage times are also more likely to report sleep deficiency [156], and sleep disturbances mediate the relationship between prolonged phone use and depression in adolescents [157].
Potential mechanisms of action include increased physiological arousal and suppressed melatonin production, which results in circadian rhythm delay [158]. These mechanisms may contribute to poor sleep outcomes through later bedtimes, longer sleep onset, shorter sleep duration, and altered sleep architecture. However, the exact underlying mechanisms, which may also involve those at the psychosocial and environmental levels, are not fully clear. Notably, a bidirectional relationship between media use and sleep duration is present, possibly attributable to shorter sleep times leading to fatigue or low energy and promoting sedentary behaviors, such as screen media use [159]. However, research has demonstrated that increased use of screen devices and electronic media increases vigilance and arousal of the nervous system, resulting in disruptions to sleep patterns and overall sleep health [160, 161]. Additional longitudinal or intervention studies are needed to further understand this relationship.
Physical injury
Because the brain is critically involved in sleep regulation [162], research has primarily focused on injury to the head and brain. In children suffering from traumatic brain injury (TBI), an increase in sleep deficiency is observed via parent report, self-report, and actigraphy measures [163, 164]. Furthermore, children with TBI display a variety of sleep–wake disorders, such as difficulty with sleep onset and maintenance, daytime sleepiness, and nightmares [165]. Similarly, in adolescents, minor head injuries are associated with long-term sleep disturbances [166]. Complaints regarding subjective sleep are often severe, and polysomnography measures show lower sleep efficiency as well as more frequent and longer night awakenings compared with control adolescents [167, 168]. Given the importance of regular brain function in controlling sleep behavior, it is vital to understand the relationship between childhood sleep and head and brain injuries.
Social determinants
Racial/ethnicity and cultural factors
Sleep disparity is a known epidemic, especially among minoritized children. African American, Hispanic, and Asian American children report greater sleep deficiency than White children [169–171], such as shorter sleep duration [172] and sleep-disordered breathing [173]. Similarly, Mexican and Central American adolescents are at greater risk of hypersomnia [174]. Racial/ethnic disparities in sleep may be conflated with cultural and socioeconomic factors. Cross-culturally, sleep may differ due to cultural norms, beliefs and parent perception about the function of sleep [175] and the typical daily lifestyle and schedule. Some European cultures, such as in Italy, engage in late-night activities and allow children to stay and participate. As such, children learn to fall asleep naturally without a set bedtime ritual and may have disrupted sleep due to family activities [176]. South American, African, and Asian cultures commonly rely on biphasic sleep patterns, generally involving daytime naps [177]. Specifically, a study conducted in Chinese adolescents demonstrated that the majority frequently nap throughout the week and nap more frequently or for longer durations was associated with better sleep quality at night and improved cognitive function [178]. However, further comparisons between Western and Asian cultures report later bedtimes, shorter sleep duration, and greater parental perception of child sleep deficiency in toddlers [179], preschool [180], and elementary school children [177] in Asian countries. Even within the U.S., variations in where children sleep, how they are put to bed, and parental concern regarding child sleep arise from the many diverse cultural groups within the U.S. population [181, 182]. Understanding cultural differences in both sleep practice and parental perception of children’s sleep may help in assessments and interventions to promote sleep health in pediatric patients.
Neighborhood conditions and socioeconomic status (SES)
While much research has focused on the social determinants of health in the last two decades, attention has only recently begun to be paid to their application to sleep health. Outside of the immediate home environment, the neighborhood in which the child resides and other related indicators of SES may also contribute to childhood sleep outcomes. Neighborhood conditions may include housing quality, safety, cleanliness of the environment, vandalism, sidewalks, and access to public spaces such as parks [156, 183]. Children living in unfavorable environments, characterized by greater poverty and lower SES, are more likely to have lower sleep efficiency [184], shorter sleep duration [185], and serious sleep deficiency [156]. Specifically, living in socioeconomic disadvantage is linked to a greater incidence of obstructive sleep apnea (OSA) in children [186, 187], and these neighborhood variables better account for OSA in children than individual-level indicators [187]. Parental stress, feeling unsafe, noise or other disruptions to sleep during the night, and other psychosocial and environmental mechanisms may serve to explain this relationship [156, 184]. More research is still needed in this area to understand how a broader social environment interacts with the physical environment on children’s sleep.
School factors
Children spend a significant portion of their daily lives in school, which can also contribute to sleep patterns and sleep behavior in childhood. Notably, school start time is frequently identified as an important factor in determining child sleep duration and quality. Earlier school start times are associated with shorter sleep duration [188, 189], increased daytime sleepiness [189, 190], and more frequent tardiness to school [189].
Whereas the high prevalence of sleep deprivation in students has demonstrated significant effects of poor sleep on academic performance [191, 192], there have been limited studies investigating the potential implications of academic pressures on child and adolescent sleep. Increased academic pressure may result in more time spent on homework or studying [120], greater exam stress [193], or increased worrying [194], which have been shown to negatively impact sleep. The American Academy of Pediatrics released a policy statement advocating for later school start times to allow children and adolescents to receive an optimal amount of sleep of 8 to 9 hours, which would promote physical and mental well-being [195]. Nevertheless, these policies have not been fully implemented.
Public health disasters/emergencies
In the context of the current COVID-19 pandemic, the once tightly regulated daily schedules of children and adolescents have now been dramatically altered and nearly eliminated due to policies dictating social distancing and online schooling [196]. Notably, prolonged school closures, cancelation of extracurricular activities, and confinement to the home cause reduced light exposure, increased sedentary activity, less healthy diets, and increased screen time. These factors may then impact sleep quality and disrupt normal child sleep patterns as well as result in negative effects on health in general [196]. Furthermore, the uncertainty and stress of this unprecedented situation also negatively affects the psychological well-being of children, as seen through clingy, distracted, irritable, and fearful behaviors. These behaviors may manifest in a greater incidence of mental disorders, such as anxiety and depression, or nightmares [197]. Because both anxious [198] and depressive symptoms [157] are associated with poor sleep outcomes, mitigating the psychological effects of public health disasters may help promote better sleep health among children and adolescents.
Major gaps/limitations and future directions
First, sleep deficiency has multidimensional manifestations in pediatric populations. However, the current literature has focused on sleep duration and sleep quality. More work is needed to understand the influential factors for important sleep aspects such as chronotype and sleep regularity. Additionally, whereas risk factors for unhealthy sleep often coexist in the pediatric population, prior research mainly focused on individual risk factors. Using machine learning algorithms to select the most important predictors and build risk predictive models for poor sleep will inform more meaningful interventions for sleep health. Big data-based datasets (e.g., national surveillance, EHR), biobanks (e.g., genetics, biomarkers), and data from research-used and customer-used sleep monitoring devices can be exploited to examine sleep regulations at the neuronal and molecular levels (sleep omics) and inform interventions at the individual (e.g., biobehavioral factors), family, social and systems levels (e.g., school start time). Furthermore, more researches are needed to investigate the bidirectionality of risk factors associated with poor sleep outcomes [199]. Finally, in terms of the quality of this review, we did not follow the standard guideline for systematic review using Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). Consequently, the quality of the cited research cannot be fully ensured. Nevertheless, this integrated review is an initial step to provide a comprehensive overview of the assessments, risk factors, and potential mechanisms of childhood sleep. More systematic reviews and meta-analyses are needed in the future to provide a more rigorous conclusion.
Conclusions
Many multidimensional factors contribute to child sleep health. Recognizing poor child sleep manifestations and incorporating measurements in practice can help clinicians identify sleep deficiency early on. Furthermore, understanding the risk factors is an important first step to developing targeted prevention/intervention strategies. Gaps in the current literature may help to guide future studies on child sleep.
Author contributions
JL conceptualized and designed the study. JL, XJ, ER, and SP drafted the article. JL, XJ, ER, SP, and TL revised it critically. All authors approve of the final manuscript to be published.
Funding
None.
Declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mindell JA, Owens JA. A clinical guide to pediatric sleep: diagnosis and management of sleep problems. vol Book, Whole. Lippincott Williams and Wilkins; 2015.
- 2.Liu J, Feng R, Ji X, Cui N, Raine A, Mednick SC. Midday napping in children: associations between nap frequency and duration across cognitive, positive psychological well-being, behavioral, and metabolic health outcomes. Sleep. 2019 doi: 10.1093/sleep/zsz126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Honaker SM, Meltzer LJ. Sleep in pediatric primary care: a review of the literature. Sleep Med Rev. 2016;25:31–39. doi: 10.1016/j.smrv.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Ranum BM, Wichstrøm L, Pallesen S, Steinsbekk S. Prevalence and stability of insufficient sleep measured by actigraphy: a prospective community study. Pediatr Res. 2020;88(1):110–116. doi: 10.1038/s41390-020-0768-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chattu VK, Sakhamuri SM, Kumar R, Spence DW, BaHammam AS, Pandi-Perumal SR. Insufficient sleep syndrome: is it time to classify it as a major noncommunicable disease? Sleep Sci. 2018;11(2):56. doi: 10.5935/1984-0063.20180013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laposky AD, Van Cauter E, Diez-Roux AV. Reducing health disparities: the role of sleep deficiency and sleep disorders. Sleep Med. 2016;18:3–6. doi: 10.1016/j.sleep.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.James S, Hale L. Sleep duration and child well-being: a nonlinear association. J Clin Child Adolesc Psychol. 2017;46(2):258–268. doi: 10.1080/15374416.2016.1204920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quach JL, Nguyen CD, Williams KE, Sciberras E. Bidirectional associations between child sleep problems and internalizing and externalizing difficulties from preschool to early adolescence. JAMA Pediatr. 2018 doi: 10.1001/jamapediatrics.2017.4363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williamson AA, Mindell JA, Hiscock H, Quach J. Longitudinal sleep problem trajectories are associated with multiple impairments in child well-being. J Child Psychol Psychiatry. 2020;61(10):1092–1103. doi: 10.1111/jcpp.13303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zuckerman B, Stevenson J, Bailey V. Sleep problems in early childhood: continuities, predictive factors, and behavioral correlates. Pediatrics. 1987;80(5):664–671. doi: 10.1542/peds.80.5.664. [DOI] [PubMed] [Google Scholar]
- 11.Meltzer LJ. Clinical management of behavioral insomnia of childhood: treatment of bedtime problems and night wakings in young children. Behav Sleep Med. 2010;8(3):172–189. doi: 10.1080/15402002.2010.487464. [DOI] [PubMed] [Google Scholar]
- 12.Mazurak N, Cook J, Weiland A, Ritze Y, Urschitz M, Junne F, et al. Impact of childhood obesity and psychological factors on sleep. Front Psych. 2021;12:1089. doi: 10.3389/fpsyt.2021.657322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moulding H, Bartsch U, Hall J, Jones M, Linden D, Owen M, et al. Sleep problems and associations with psychopathology and cognition in young people with 22q11. 2 deletion syndrome (22q11. 2DS) Psych med. 2020;50:1191–1202. doi: 10.1017/S0033291719001119. [DOI] [PubMed] [Google Scholar]
- 14.Hoyniak CP, Bates JE, Staples AD, Rudasill KM, Molfese DL, Molfese VJ. Child sleep and socioeconomic context in the development of cognitive abilities in early childhood. Child Dev. 2019;90(5):1718–1737. doi: 10.1111/cdev.13042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stores G. Practitioner review: assessment and treatment of sleep disorders in children and adolescents. J Child Psychol Psychiatry. 1996;37(8):907–925. doi: 10.1111/j.1469-7610.1996.tb01489.x. [DOI] [PubMed] [Google Scholar]
- 16.Labbate LA, Pollack MH, Otto MW, Langenauer S, Rosenbaum JF. Sleep panic attacks: an association with childhood anxiety and adult psychopathology. Biol Psychiat. 1994;36(1):57–60. doi: 10.1016/0006-3223(94)90063-9. [DOI] [PubMed] [Google Scholar]
- 17.Meltzer LJ, Mindell JA. Behavioral sleep disorders in children and adolescents. Sleep Med Clin. 2008;3(2):269–279. doi: 10.1016/j.jsmc.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 18.Williamson AA, Mindell JA, Hiscock H, Quach J. Child sleep behaviors and sleep problems from infancy to school-age. Sleep Med. 2019;63:5–8. doi: 10.1016/j.sleep.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas AG, Monahan KC, Lukowski AF, Cauffman E. Sleep problems across development: a pathway to adolescent risk taking through working memory. J Youth Adolesc. 2015;44(2):447–464. doi: 10.1007/s10964-014-0179-7. [DOI] [PubMed] [Google Scholar]
- 20.Bertocci MA, Dahl RE, Williamson DE, Iosif A-M, Birmaher B, Axelson D, et al. Subjective sleep complaints in pediatric depression: a controlled study and comparison with EEG measures of sleep and waking. J Am Acad Child Adolesc Psychiatry. 2005;44(11):1158–1166. doi: 10.1097/01.chi.0000179057.54419.17. [DOI] [PubMed] [Google Scholar]
- 21.Wiggs L, Montgomery P, Stores G. Actigraphic and parent reports of sleep patterns and sleep disorders in children with subtypes of attention-deficit hyperactivity disorder. Sleep. 2005;28(11):1437–1445. doi: 10.1093/sleep/28.11.1437. [DOI] [PubMed] [Google Scholar]
- 22.Mazza S, Bastuji H, Rey AE. Objective and subjective assessments of sleep in children: comparison of actigraphy, sleep diary completed by children and parents’ estimation. Front Psych. 2020;11:495. doi: 10.3389/fpsyt.2020.00495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dayyat EA, Spruyt K, Molfese DL, Gozal D. Sleep estimates in children: parental versus actigraphic assessments. Nat Sci Sleep. 2011;3:115. doi: 10.2147/NSS.S25676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blunden S, Galland B. The complexities of defining optimal sleep: empirical and theoretical considerations with a special emphasis on children. Sleep Med Rev. 2014;18(5):371–378. doi: 10.1016/j.smrv.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Brown WJ, Wilkerson AK, Boyd SJ, Dewey D, Mesa F, Bunnell BE. A review of sleep disturbance in children and adolescents with anxiety. J Sleep Res. 2018;27(3):e12635. doi: 10.1111/jsr.12635. [DOI] [PubMed] [Google Scholar]
- 26.Ji X, Liu J. Subjective sleep measures for adolescents: a systematic review. Child Care Health Dev. 2016;42(6):825–839. doi: 10.1111/cch.12376. [DOI] [PubMed] [Google Scholar]
- 27.Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021(1):276–291. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 28.Minges KE, Redeker NS. Delayed school start times and adolescent sleep: a systematic review of the experimental evidence. Sleep Med Rev. 2016;28:86–95. doi: 10.1016/j.smrv.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park M-H, Park S, Jung K-I, Kim JI, Cho SC, Kim B-N. Moderating effects of depressive symptoms on the relationship between problematic use of the internet and sleep problems in Korean adolescents. BMC Psychiatry. 2018;18(1):1–8. doi: 10.1186/s12888-018-1865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bartel K. Protective and risk factors for adolescent sleep health. School of Psychology.: Flinders University; 2017. [Google Scholar]
- 31.Riesch SK, Liu J, Kaufmann PG, Doswell WM, Cohen S, Vessey J. Preventing adverse health outcomes among children and adolescents by addressing screen media practices concomitant to sleep disturbance. Nurs Outlook. 2019;67(4):492–496. doi: 10.1016/j.outlook.2019.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grandner MA. Addressing sleep disturbances: an opportunity to prevent cardiometabolic disease? Int Review Psychiatry. 2014;26:155–176. doi: 10.3109/09540261.2014.911148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Becker SP, Langberg JM, Byars KC. Advancing a biopsychosocial and contextual model of sleep in adolescence: a review and introduction to the special issue. J Youth Adolesc. 2015;44(2):239–270. doi: 10.1007/s10964-014-0248-y. [DOI] [PubMed] [Google Scholar]
- 34.Touchette E, Dionne G, Forget-Dubois N, Petit D, Perusse D, Falissard B, et al. Genetic and environmental influences on daytime and nighttime sleep duration in early childhood. Pediatrics. 2013;131(6):1874. doi: 10.1542/peds.2012-2284. [DOI] [PubMed] [Google Scholar]
- 35.Laposky A, Easton A, Dugovic C, Walisser J, Bradfield C, Turek F. Deletion of the mammalian circadian clock gene BMAL1/Mop3 alters baseline sleep architecture and the response to sleep deprivation. Sleep. 2005;28(4):395–410. doi: 10.1093/sleep/28.4.395. [DOI] [PubMed] [Google Scholar]
- 36.Allebrandt K, Amin N, Müller-Myhsok B, Esko T, Teder-Laving M, Azevedo R, et al. A KATP channel gene effect on sleep duration: from genome-wide association studies to function in Drosophila. Mol Psychiatry. 2013;18(1):122–132. doi: 10.1038/mp.2011.142. [DOI] [PubMed] [Google Scholar]
- 37.Brescianini S, Volzone A, Fagnani C, Patriarca V, Grimaldi V, Lanni R, et al. Genetic and environmental factors shape infant sleep patterns: a study of 18-month-old twins. Pediatrics. 2011;127(5):e1296–e1302. doi: 10.1542/peds.2010-0858. [DOI] [PubMed] [Google Scholar]
- 38.Gaina A, Sekine M, Hamanishi S, Chen X, Kagamimori S. Gender and temporal differences in sleep-wake patterns in Japanese schoolchildren. Sleep. 2005;28(3):337–342. [PubMed] [Google Scholar]
- 39.Meijer AM, Reitz E, Deković M, Van Den Wittenboer GL, Stoel RD. Longitudinal relations between sleep quality, time in bed and adolescent problem behaviour. J Child Psychol Psychiatry. 2010;51(11):1278–1286. doi: 10.1111/j.1469-7610.2010.02261.x. [DOI] [PubMed] [Google Scholar]
- 40.Uebergang LK, Arnup SJ, Hiscock H, Care E, Quach J. Sleep problems in the first year of elementary school: the role of sleep hygiene, gender and socioeconomic status. Sleep Health. 2017;3(3):142–147. doi: 10.1016/j.sleh.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 41.Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, Liao D, Bixler EO. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep Med. 2014;15(1):91–95. doi: 10.1016/j.sleep.2013.08.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Franco P, Putois B, Guyon A, Raoux A, Papadopoulou M, Guignard-Perret A, et al. Sleep during development: sex and gender differences. Sleep Med Rev. 2020;51:101276. doi: 10.1016/j.smrv.2020.101276. [DOI] [PubMed] [Google Scholar]
- 43.Plancoulaine S, Lioret S, Regnault N, Heude B, Charles MA. Group EMCCS Gender-specific factors associated with shorter sleep duration at age 3 years. J Sleep Res. 2015;24(6):610–620. doi: 10.1111/jsr.12308. [DOI] [PubMed] [Google Scholar]
- 44.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16(3):258–262. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 45.Pieters S, Van Der Vorst H, Burk WJ, Wiers RW, Engels RC. Puberty-dependent sleep regulation and alcohol use in early adolescents. Alcohol Clin Exp Res. 2010;34(9):1512–1518. doi: 10.1111/j.1530-0277.2010.01235.x. [DOI] [PubMed] [Google Scholar]
- 46.Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12(2):110–118. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 47.National Sleep Foundation: 2011 Poll, Technology and Sleep. https://www.sleepfoundation.org/professionals/sleep-americar-polls/2011-poll-technology-and-sleep (2011). Accessed Sep 26, 2018.
- 48.Malone SK, Zemel B, Compher C, Souders M, Chittams J, Thompson AL, et al. Social jet lag, chronotype and body mass index in 14–17 year-old adolescents. Chronobiol Int. 2016;33(9):1255–1266. doi: 10.1080/07420528.2016.1196697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kirmil-Gray K, Eagleston JR, Gibson E, Thoresen CE. Sleep disturbance in adolescents: sleep quality, sleep habits, beliefs about sleep, and daytime functioning. J Youth Adolesc. 1984;13(5):375–384. doi: 10.1007/BF02088636. [DOI] [PubMed] [Google Scholar]
- 50.Pesonen A-K, Martikainen S, Heinonen K, Wehkalampi K, Lahti J, Kajantie E, et al. Continuity and change in poor sleep from childhood to early adolescence. Sleep. 2014;37(2):289–297. doi: 10.5665/sleep.3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mina TH, Lahti M, Drake AJ, Räikkönen K, Minnis H, Denison FC, et al. Prenatal exposure to very severe maternal obesity is associated with adverse neuropsychiatric outcomes in children. Psychol Med. 2017;47(2):353. doi: 10.1017/S0033291716002452. [DOI] [PubMed] [Google Scholar]
- 52.Hanlon-Dearman A, Chen ML, Olson HC. Understanding and managing sleep disruption in children with fetal alcohol spectrum disorder. Biochem Cell Biol. 2018;96(2):267–274. doi: 10.1139/bcb-2017-0064. [DOI] [PubMed] [Google Scholar]
- 53.Alvik A, Torgersen AM, Aalen OO, Lindemann R. Binge alcohol exposure once a week in early pregnancy predicts temperament and sleeping problems in the infant. Early Human Dev. 2011;87(12):827–833. doi: 10.1016/j.earlhumdev.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 54.Pesonen A-K, Räikkönen K, Matthews K, Heinonen K, Paavonen JE, Lahti J, et al. Prenatal origins of poor sleep in children. Sleep. 2009;32(8):1086–1092. doi: 10.1093/sleep/32.8.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mughal R, Hill CM, Joyce A, Dimitriou D. Sleep and cognition in children with fetal alcohol spectrum disorders (FASD) and children with autism spectrum disorders (ASD) Brain Sci. 2020;10(11):863. doi: 10.3390/brainsci10110863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wengel T, Hanlon-Dearman AC, Fjeldsted B. Sleep and sensory characteristics in young children with fetal alcohol spectrum disorder. J Dev Behav Pediatr. 2011;32(5):384–392. doi: 10.1097/DBP.0b013e3182199694. [DOI] [PubMed] [Google Scholar]
- 57.Chen ML, Olson HC, Picciano JF, Starr JR, Owens J. Sleep problems in children with fetal alcohol spectrum disorders. J Clini Sleep Med : JCSM : Off Publ AM Acad of Sleep Med. 2012;8(4):421–429. doi: 10.5664/jcsm.2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goril S, Zalai D, Scott L, Shapiro CM. Sleep and melatonin secretion abnormalities in children and adolescents with fetal alcohol spectrum disorders. Sleep Med. 2016;23:59–64. doi: 10.1016/j.sleep.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 59.Oei JL. Alcohol use in pregnancy and its impact on the mother and child. Addiction. 2020;115(11):2148–2163. doi: 10.1111/add.15036. [DOI] [PubMed] [Google Scholar]
- 60.Ystrom H, Nilsen W, Hysing M, Sivertsen B, Ystrom E. Sleep problems in preschoolers and maternal depressive symptoms: an evaluation of mother-and child-driven effects. Dev Psychol. 2017;53(12):2261. doi: 10.1037/dev0000402. [DOI] [PubMed] [Google Scholar]
- 61.O’Connor TG, Monk C, Burke AS. Maternal affective illness in the perinatal period and child development: findings on developmental timing, mechanisms, and intervention. Curr Psychiatry Rep. 2016;18(3):24. doi: 10.1007/s11920-016-0660-y. [DOI] [PubMed] [Google Scholar]
- 62.Nevarez MD, Rifas-Shiman SL, Kleinman KP, Gillman MW, Taveras EM. Associations of early life risk factors with infant sleep duration. Acad Pediatr. 2010;10(3):187–193. doi: 10.1016/j.acap.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu J, Ji X, Wang G, Li Y, Leung PW, Pinto-Martin J. Maternal emotions during the pre/postnatal periods and children’s sleep behaviors: the mediating role of children’s behavior. J Affect disord. 2020;273:138–145. doi: 10.1016/j.jad.2020.03.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Toffol E, Lahti-Pulkkinen M, Lahti J, Lipsanen J, Heinonen K, Pesonen A-K, et al. Maternal depressive symptoms during and after pregnancy are associated with poorer sleep quantity and quality and sleep disorders in 3.5 year-old offspring. Sleep med. 2019;56:201–210. doi: 10.1016/j.sleep.2018.10.042. [DOI] [PubMed] [Google Scholar]
- 65.Horne RSC, Sly DJ, Cranage SM, Chau B, Adamson TM. Effects of prematurity on arousal from sleep in the newborn infant. Pediatr Res. 2000;47(4):468–474. doi: 10.1203/00006450-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 66.Bennet L, Walker DW, Horne RS. Waking up too early–the consequences of preterm birth on sleep development. J Physiol. 2018;596(23):5687–5708. doi: 10.1113/JP274950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li L, Zhao K, Hua J, Li S. Association between sleep-disordered breathing during pregnancy and maternal and fetal outcomes: an updated systematic review and meta-analysis. Front Neurol. 2018;9:91. doi: 10.3389/fneur.2018.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rosen CL, Larkin EK, Kirchner HL, Emancipator JL, Bivins SF, Surovec SA, et al. Prevalence and risk factors for sleep-disordered breathing in 8–11 year-old children: association with race and prematurity. J Pediatr. 2003;142(4):383–389. doi: 10.1067/mpd.2003.28. [DOI] [PubMed] [Google Scholar]
- 69.Coren S, Searleman A. Birth stress and self-reported sleep difficulty. Sleep. 1985;8(3):222–226. doi: 10.1093/sleep/8.3.222. [DOI] [PubMed] [Google Scholar]
- 70.Paavonen EJ, Strang-Karlsson S, Raikkonen K, Heinonen K, Pesonen AK, Hovi P, et al. Very low birth weight increases risk for sleep-disordered breathing in young adulthood: the Helsinki study of very low birth weight adults. Pediatrics. 2007;120(4):778–784. doi: 10.1542/peds.2007-0540. [DOI] [PubMed] [Google Scholar]
- 71.Ramamurthy MB, Sekartini R, Ruangdaraganon N, Huynh DHT, Sadeh A, Mindell JA. Effect of current breastfeeding on sleep patterns in infants from Asia-Pacific region. J Paediatr Child Health. 2012;48(8):669–674. doi: 10.1111/j.1440-1754.2012.02453.x. [DOI] [PubMed] [Google Scholar]
- 72.Galbally M, Lewis AJ, McEgan K, Scalzo K, Islam FMA. Breastfeeding and infant sleep patterns: an Australian population study. J Paediatr Child Health. 2013;49(2):E147–E152. doi: 10.1111/jpc.12089. [DOI] [PubMed] [Google Scholar]
- 73.Poobalan AS, Aucott LS, Ross L, Smith WCS, Helms PJ, Williams JHG. Effects of treating postnatal depression on mother-infant interaction and child development: systematic review. Br J Psychiatry. 2007;191(5):378–386. doi: 10.1192/bjp.bp.106.032789. [DOI] [PubMed] [Google Scholar]
- 74.Letourneau NL, Dennis CL, Cosic N, Linder J. The effect of perinatal depression treatment for mothers on parenting and child development: a systematic review. Depress Anxiety. 2017;34(10):928–966. doi: 10.1002/da.22687. [DOI] [PubMed] [Google Scholar]
- 75.Pinheiro KAT, Pinheiro RT, da Silva RA, da Cunha Coelho FM, de Ávila QL, Godoy RV, et al. Chronicity and severity of maternal postpartum depression and infant sleep disorders: a population-based cohort study in southern Brazil. Infant Behav Dev. 2011;34(2):371–373. doi: 10.1016/j.infbeh.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 76.Swanson LM, Flynn HA, Wilburn K, Marcus S, Armitage R. Maternal mood and sleep in children of women at risk for perinatal depression. Arch Womens Ment Health. 2010;13(6):531–534. doi: 10.1007/s00737-010-0177-z. [DOI] [PubMed] [Google Scholar]
- 77.Córdova FV, Barja S, Brockmann PE. Consequences of short sleep duration on the dietary intake in children: a systematic review and metanalysis. Sleep Med Rev. 2018;42:68–84. doi: 10.1016/j.smrv.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 78.Ji X, Grandner MA, Liu J. The relationship between micronutrient status and sleep patterns: a systematic review. Public Health Nutr. 2017;20(4):687–701. doi: 10.1017/S1368980016002603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jalilolghadr S, Afaghi A, O’Connor H, Chow CM. Effect of low and high glycaemic index drink on sleep pattern in children. JPMA-J Pak Med Associ. 2011;61(6):533. [PubMed] [Google Scholar]
- 80.Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality. Nutr Res. 2012;32(5):309–319. doi: 10.1016/j.nutres.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 81.Ursin R. Serotonin and sleep. Sleep Med Rev. 2002;6(1):55–67. doi: 10.1053/smrv.2001.0174. [DOI] [PubMed] [Google Scholar]
- 82.Harada T, Hirotani M, Maeda M, Nomura H, Takeuchi H. Correlation between breakfast tryptophan content and morningness–eveningness in Japanese infants and students aged 0–15 yrs. J Physiol Anthropol. 2007;26(2):201–207. doi: 10.2114/jpa2.26.201. [DOI] [PubMed] [Google Scholar]
- 83.Diethelm K, Remer T, Jilani H, Kunz C, Buyken AE. Associations between the macronutrient composition of the evening meal and average daily sleep duration in early childhood. Clin Nutr. 2011;30(5):640–646. doi: 10.1016/j.clnu.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 84.Ji X, Compher CW, Irving SY, Kim J, Dinges DF, Liu J. Serum micronutrient status, sleep quality and neurobehavioural function among early adolescents. Public Health Nutr. 2021;24(17):5815–5825. doi: 10.1017/S1368980021002329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kordas K, Siegel EH, Olney DK, Katz J, Tielsch JM, Chwaya HM, et al. Maternal reports of sleep in 6–18 month-old infants from Nepal and Zanzibar: association with iron deficiency anemia and stunting. Early Human Dev. 2008;84(6):389–398. doi: 10.1016/j.earlhumdev.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 86.Peirano P, Algarín C, Garrido M, Algarín D, Lozoff B. Iron-deficiency anemia is associated with altered characteristics of sleep spindles in NREM sleep in infancy. Neurochem Res. 2007;32(10):1665–1672. doi: 10.1007/s11064-007-9396-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Peirano PD, Algarín CR, Garrido MI, Lozoff B. Iron deficiency anemia in infancy is associated with altered temporal organization of sleep states in childhood. Pediatr Res. 2007;62(6):715–719. doi: 10.1203/PDR.0b013e3181586aef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ji X, Liu J. Associations between blood zinc concentrations and sleep quality in childhood: a cohort study. Nutrients. 2015;7(7):5684–5696. doi: 10.3390/nu7075247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Takeda A, Minami A, Seki Y, Oku N. Differential effects of zinc on glutamatergic and GABAergic neurotransmitter systems in the hippocampus. J Neurosci Res. 2004;75(2):225–229. doi: 10.1002/jnr.10846. [DOI] [PubMed] [Google Scholar]
- 90.Beard JL, Erikson KM, Jones BC. Neurobehavioral analysis of developmental iron deficiency in rats. Behav Brain Res. 2002;134(1–2):517–524. doi: 10.1016/S0166-4328(02)00092-X. [DOI] [PubMed] [Google Scholar]
- 91.Dai Y, Liu J. Omega-3 long-chain polyunsaturated fatty acid and sleep: a systematic review and meta-analysis of randomized controlled trials and longitudinal studies. Nutri Rev. 2020;79(8):847–868. doi: 10.1093/nutrit/nuaa103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Catalá A. (2010) The function of very long chain polyunsaturated fatty acids in the pineal gland. Biochimi et Biophysica Acta (BBA) Mol Cell Bio Lipids. 1801;2:95–99. doi: 10.1016/j.bbalip.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 93.Zhang H, Hamilton JH, Salem N, Jr, Kim H-Y. N–3 fatty acid deficiency in the rat pineal gland: effects on phospholipid molecular species composition and endogenous levels of melatonin and lipoxygenase products. J Lipid Res. 1998;39(7):1397–1403. doi: 10.1016/S0022-2275(20)32520-7. [DOI] [PubMed] [Google Scholar]
- 94.Yehuda S, Rabinovitz S, Mostofsk D. Essential fatty acids and sleep: mini-review and hypothesis. Med Hypotheses. 1998;50(2):139–145. doi: 10.1016/S0306-9877(98)90200-6. [DOI] [PubMed] [Google Scholar]
- 95.Kim HY, Edsall L, Garcia M, Zhang H. The release of polyunsaturated fatty acids and their lipoxygenation in the brain. Lipoxygenases and their Metabolites. 1999:75–85. [DOI] [PubMed]
- 96.Liu J, Zhang A, Li L. Sleep duration and overweight/obesity in children: review and implications for pediatric nursing. J Spec Pediatr Nurs. 2012;17(3):193–204. doi: 10.1111/j.1744-6155.2012.00332.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu J, Ghastine L, Um P, Rovit E, Wu T. Environmental exposures and sleep outcomes: a review of evidence, potential mechanisms and implications. Environ Res. 2021;2020(196):110406. doi: 10.1016/j.envres.2020.110406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Liu J, Liu X, Pak V, Wang Y, Yan C, Pinto-Martin J, et al. Early blood lead levels and sleep disturbance in preadolescence. Sleep. 2015;38(12):1869–1874. doi: 10.5665/sleep.5230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Weyde KV, Krog NH, Oftedal B, Evandt J, Magnus P, Øverland S, et al. Nocturnal road traffic noise exposure and children’s sleep duration and sleep problems. Int J Environ Res Public Health. 2017;14(5):491. doi: 10.3390/ijerph14050491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rudolph KE, Shev A, Paksarian D, Merikangas KR, Mennitt DJ, James P, et al. Environmental noise and sleep and mental health outcomes in a nationally representative sample of urban US adolescents. Environ Epidemio (Philadelphia, PA). 2019;3(4):e056. doi: 10.1097/EE9.0000000000000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kawai Y, Weatherhead JR, Traube C, Owens TA, Shaw BE, Fraser EJ, et al. Quality improvement initiative to reduce pediatric intensive care unit noise pollution with the use of a pediatric delirium bundle. J Intensive Care Med. 2019;34(5):383–390. doi: 10.1177/0885066617728030. [DOI] [PubMed] [Google Scholar]
- 102.De La Iglesia HO, Fernández-Duque E, Golombek DA, Lanza N, Duffy JF, Czeisler CA, et al. Access to electric light is associated with shorter sleep duration in a traditionally hunter-gatherer community. J Biol Rhythms. 2015;30(4):342–350. doi: 10.1177/0748730415590702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chang A-M, Aeschbach D, Duffy JF, Czeisler CA. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci. 2015;112(4):1232–1237. doi: 10.1073/pnas.1418490112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liu J, Wu T, Liu Q, Wu S, Chen J-C. Air pollution exposure and adverse sleep health across the life course: a systematic review. Environ Pollut. 2020;262:114263. doi: 10.1016/j.envpol.2020.114263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sánchez T, Gozal D, Smith DL, Foncea C, Betancur C, Brockmann PE. Association between air pollution and sleep disordered breathing in children. Pediatr Pulmonol. 2019;54(5):544–550. doi: 10.1002/ppul.24256. [DOI] [PubMed] [Google Scholar]
- 106.Meltzer LJ, Montgomery-Downs HE. Sleep in the family. Pediatr Clin North Am. 2011;58(3):765–774. doi: 10.1016/j.pcl.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14(2):89–96. doi: 10.1016/j.smrv.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 108.Schachter FF, Fuchs ML, Bijur PE, Stone RK. Cosleeping and sleep problems in Hispanic-American urban young children. Pediatrics. 1989;84(3):522–530. doi: 10.1542/peds.84.3.522. [DOI] [PubMed] [Google Scholar]
- 109.Tan TX, Marfo K, Dedrick RF. Preschool-age adopted Chinese children’s sleep problems and family sleep arrangements. Inf Child Develop: An Int J Res Practice. 2009;18(5):422–440. doi: 10.1002/icd.630. [DOI] [Google Scholar]
- 110.Cortesi F, Giannotti F, Sebastiani T, Vagnoni C, Marioni P. Cosleeping versus solitary sleeping in children with bedtime problems: child emotional problems and parental distress. Behav Sleep Med. 2008;6(2):89–105. doi: 10.1080/15402000801952922. [DOI] [PubMed] [Google Scholar]
- 111.Li S, Jin X, Yan C, Wu S, Jiang F, Shen X. Bed-and room-sharing in Chinese school-aged children: prevalence and association with sleep behaviors. Sleep Med. 2008;9(5):555–563. doi: 10.1016/j.sleep.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 112.Keller MA, Goldberg WA. Co-sleeping: Help or hindrance for young children’s independence? Inf Child Develop: An Int J Res Practice. 2004;13(5):369–388. doi: 10.1002/icd.365. [DOI] [Google Scholar]
- 113.Madansky D, Edelbrock C. Cosleeping in a community sample of 2–3 year-old children. Pediatrics. 1990;86(2):197–203. doi: 10.1542/peds.86.2.197. [DOI] [PubMed] [Google Scholar]
- 114.Chen Z, Dai Y, Liu X, Liu J. Early Childhood co-sleeping predicts behavior problems in preadolescence: a prospective cohort study. Behavioral Sleep Med. 2021;19:563–576. doi: 10.1080/15402002.2020.1818564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chen Z, Dai Y, Liu X, Liu J. Early childhood co-sleeping predicts behavior problems in preadolescence: a Prospective cohort study. Behav Sleep Med. 2021;19(5):563–576. doi: 10.1080/15402002.2020.1818564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Owens-Stively J, Frank N, Smith A, Hagino O, Spirito A, Arrigan M, et al. Child temperament, parenting discipline style, and daytime behavior in childhood sleep disorders. J Dev Behav Pediatrics. 1997;18(5):5–314. doi: 10.1097/00004703-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 117.Johnson N, McMahon C. Preschoolers’ sleep behaviour: associations with parental hardiness, sleep-related cognitions and bedtime interactions. J Child Psychol Psychiatry. 2008;49(7):765–773. doi: 10.1111/j.1469-7610.2007.01871.x. [DOI] [PubMed] [Google Scholar]
- 118.Brand S, Hatzinger M, Beck J, Holsboer-Trachsler E. Perceived parenting styles, personality traits and sleep patterns in adolescents. J Adolesc. 2009;32(5):1189–1207. doi: 10.1016/j.adolescence.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 119.Buxton OM, Chang A-M, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: protective family routines for child and adolescent sleep. Sleep Health. 2015;1(1):15–27. doi: 10.1016/j.sleh.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Adam EK, Snell EK, Pendry P. Sleep timing and quantity in ecological and family context: a nationally representative time-diary study. J Fam Psychol. 2007;21(1):4. doi: 10.1037/0893-3200.21.1.4. [DOI] [PubMed] [Google Scholar]
- 121.Mindell JA, Li AM, Sadeh A, Kwon R, Goh DY. Bedtime routines for young children: a dose-dependent association with sleep outcomes. Sleep. 2015;38(5):717–722. doi: 10.5665/sleep.4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bordeleau S, Bernier A, Carrier J. Longitudinal associations between the quality of parent−child interactions and children’s sleep at preschool age. J Fam Psychol. 2012;26(2):254. doi: 10.1037/a0027366. [DOI] [PubMed] [Google Scholar]
- 123.El-Sheikh M, Kelly RJ, Philbrook LE. Family contexts of sleep and health across the life course. Cham: Springer; 2017. Sleep and development Familial and socio-cultural considerations; pp. 25–49. [Google Scholar]
- 124.Meijer AM, Reitz E, Dekoviċ M. Parenting matters: a longitudinal study into parenting and adolescent sleep. J Sleep Res. 2016;25(5):556–564. doi: 10.1111/jsr.12406. [DOI] [PubMed] [Google Scholar]
- 125.Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner HL, Redline S. Effects of the home environment on school-aged children’s sleep. Sleep. 2005;28(11):1419–1427. doi: 10.1093/sleep/28.11.1419. [DOI] [PubMed] [Google Scholar]
- 126.Sciberras E, Song JC, Mulraney M, Schuster T, Hiscock H. Sleep problems in children with attention-deficit hyperactivity disorder: associations with parenting style and sleep hygiene. Eur Child Adolesc Psychiatry. 2017;26(9):1129–1139. doi: 10.1007/s00787-017-1000-4. [DOI] [PubMed] [Google Scholar]
- 127.Owens JA. The ADHD and sleep conundrum: a review. J Dev Behav Pediatr. 2005;26(4):312–322. doi: 10.1097/00004703-200508000-00011. [DOI] [PubMed] [Google Scholar]
- 128.Troxel WM, Trentacosta CJ, Forbes EE, Campbell SB. Negative emotionality moderates associations among attachment, toddler sleep, and later problem behaviors. J Fam Psychol. 2013;27(1):127. doi: 10.1037/a0031149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hash JB, Oxford ML, Fleming CB, Ward TM, Spieker SJ, Lohr MJ. Impact of a home visiting program on sleep problems among young children experiencing adversity. Child Abuse Negl. 2019;89:143–154. doi: 10.1016/j.chiabu.2018.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lewin M, Lopachin J, Delorme J, Opendak M, Sullivan RM, Wilson DA. Early life trauma has lifelong consequences for sleep and behavior. Sci Rep. 2019;9(1):1–14. doi: 10.1038/s41598-019-53241-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol. 2006;31(5):469–480. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- 132.Insana SP, Foley KP, Montgomery-Downs HE, Kolko DJ, McNeil CB. Children exposed to intimate partner violence demonstrate disturbed sleep and impaired functional outcomes. Psychol Trauma Theory Res Pract Policy. 2014;6(3):290. doi: 10.1037/a0033108. [DOI] [Google Scholar]
- 133.Li X, Wang Y, Tang J, Li J, Zhou Y, Wang Y, et al. Exposure to domestic violence and depressive symptoms in Chinese adolescents: sleep problems as a mediator. J Affect Disord. 2022;310:17–24. doi: 10.1016/j.jad.2022.04.114. [DOI] [PubMed] [Google Scholar]
- 134.April-Sanders A, Duarte CS, Wang S, McGlinchey E, Alcántara C, Bird H, et al. Childhood adversity and sleep disturbances: longitudinal results in Puerto Rican children. Int J Behav Med. 2021;28(1):107–115. doi: 10.1007/s12529-020-09873-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chae W, Jang J, Park EC, Jang SI. Changes in child abuse experience associated to sleep quality: results of the Korean Children & Youth Panel Survey. BMC Public Health. 2021;21:1210. doi: 10.1186/s12889-021-11309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Usta J, Farver J. Child sexual abuse in Lebanon during war and peace. Child care health dev. 2010;36(3):361–368. doi: 10.1111/j.1365-2214.2010.01082.x. [DOI] [PubMed] [Google Scholar]
- 137.Chapman DP, Liu Y, Presley-Cantrell LR, Edwards VJ, Wheaton AG, Perry GS, et al. Adverse childhood experiences and frequent insufficient sleep in 5 US states, 2009: a retrospective cohort study. BMC Public Health. 2013;13(1):1–9. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Park E-J, Kim S-Y, Kim Y, Sung D, Kim B, Hyun Y, et al. The relationship between adverse childhood experiences and sleep problems among adolescent students: mediation by depression or anxiety. Int J Environ Res Public Health. 2021;18(1):236. doi: 10.3390/ijerph18010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nielsen T, Carr M, Picard-Deland C, Marquis L-P, Saint-Onge K, Blanchette-Carrière C, et al. Early childhood adversity associations with nightmare severity and sleep spindles. Sleep Med. 2019;56:57–65. doi: 10.1016/j.sleep.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 140.Collado-Corona MÁ, Loredo-Abdalá A, Serrano-Morales JL, Shkurovich-Bialik P, Shkurovich-Zaslavsky M, Arch-Tirado E. Sleep alterations in childhood victims of sexual and physical abuse. Cir Cir. 2005;73(4):297–301. [PubMed] [Google Scholar]
- 141.Tracy EL, Tracy CT, Kim JJ, Yang R, Kim E. Cascading effects of childhood abuse on physical health issues in later adulthood through trait anxiety and poor daily sleep quality. J health psy. 2020;26(12):2342–2348. doi: 10.1177/1359105320909876. [DOI] [PubMed] [Google Scholar]
- 142.Hébert M, Langevin R, Guidi E, Bernard-Bonnin AC, Allard-Dansereau C. Sleep problems and dissociation in preschool victims of sexual abuse. J Trauma Dissociation. 2017;18(4):507–521. doi: 10.1080/15299732.2016.1240739. [DOI] [PubMed] [Google Scholar]
- 143.Briere J. The long-term clinical correlates of childhood sexual victimization. Ann N Y Acad Sci. 1988;528(1):327–334. doi: 10.1111/j.1749-6632.1988.tb50874.x. [DOI] [PubMed] [Google Scholar]
- 144.Briere J, Runtz M. Post sexual abuse trauma: data and implications for clinical practice. J Interpers Violence. 1987;2(4):367–379. doi: 10.1177/088626058700200403. [DOI] [Google Scholar]
- 145.Cecil CAM, Viding E, McCrory EJ, Gregory AM. Distinct mechanisms underlie associations between forms of childhood maltreatment and disruptive nocturnal behaviors. Dev Neuropsychol. 2015;40(3):181–199. doi: 10.1080/87565641.2014.983636. [DOI] [PubMed] [Google Scholar]
- 146.Demirci E. Non suicidal self-injury, emotional eating and insomnia after child sexual abuse: are those symptoms related to emotion regulation? J Forensic Leg Med. 2018;53:17–21. doi: 10.1016/j.jflm.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 147.Steine IM, Skogen JC, Krystal JH, Winje D, Milde AM, Grønli J, et al. Insomnia symptom trajectories among adult survivors of childhood sexual abuse: a longitudinal study. Child Abuse Negl. 2019;93:263–276. doi: 10.1016/j.chiabu.2019.05.009. [DOI] [PubMed] [Google Scholar]
- 148.Edgardh K, Ormstad K. Prevalence and characteristics of sexual abuse in a national sample of Swedish 17 year-old boys and girls. Acta Paediatr. 2000;89(3):310–319. doi: 10.1111/j.1651-2227.2000.tb01333.x. [DOI] [PubMed] [Google Scholar]
- 149.Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015;135(2):367. doi: 10.1542/peds.2014-2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Cheung CH, Bedford R, De Urabain IRS, Karmiloff-Smith A, Smith TJ. Daily touchscreen use in infants and toddlers is associated with reduced sleep and delayed sleep onset. Sci Rep. 2017;7:46104. doi: 10.1038/srep46104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cespedes EM, Gillman MW, Kleinman K, Rifas-Shiman SL, Redline S, Taveras EM. Television viewing, bedroom television, and sleep duration from infancy to mid-childhood. Pediatrics. 2014;133(5):e1163. doi: 10.1542/peds.2013-3998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Vijakkhana N, Wilaisakditipakorn T, Ruedeekhajorn K, Pruksananonda C, Chonchaiya W. Evening media exposure reduces night-time sleep. Acta Paediatr. 2015;104(3):306–312. doi: 10.1111/apa.12904. [DOI] [PubMed] [Google Scholar]
- 153.Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: literature review and case study. Environ Res. 2018;164:149–157. doi: 10.1016/j.envres.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 154.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med. 2010;11(8):735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 155.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–58. doi: 10.1016/j.smrv.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Singh GK, Kenney MK. Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents. Sleep disorders. 2013;2013:2003–2012. doi: 10.1155/2013/394320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Liu J, Liu C, Wu T, Liu B-P, Jia C-X, Liu X. Prolonged mobile phone use is associated with depressive symptoms in Chinese adolescents. J Affect Disord. 2019;259:128–134. doi: 10.1016/j.jad.2019.08.017. [DOI] [PubMed] [Google Scholar]
- 158.Hersh C, Sisti J, Richiutti V, Schernhammer E. The effects of sleep and light at night on melatonin in adolescents. Hormones. 2015;14(3):399–409. doi: 10.14310/horm.2002.1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Magee CA, Lee JK, Vella SA. Bidirectional relationships between sleep duration and screen time in early childhood. JAMA Pediatr. 2014;168(5):465–470. doi: 10.1001/jamapediatrics.2013.4183. [DOI] [PubMed] [Google Scholar]
- 160.Demirci K, Akgönül M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict. 2015;4(2):85–92. doi: 10.1556/2006.4.2015.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Thomée S. Mobile phone use and mental health. a review of the research that takes a psychological perspective on exposure. Inter J Env Res Public Health. 2018;15(12):2692. doi: 10.3390/ijerph15122692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Krueger JM, Obál F, Jr, Kapás L, Fang J. Brain organization and sleep function. Behav Brain Res. 1995;69(1–2):177–185. doi: 10.1016/0166-4328(95)00015-L. [DOI] [PubMed] [Google Scholar]
- 163.Sumpter RE, Dorris L, Kelly T, McMillan TM. Pediatric sleep difficulties after moderate–severe traumatic brain injury. J Int Neuropsychol Soc. 2013;19(7):829–834. doi: 10.1017/S1355617713000465. [DOI] [PubMed] [Google Scholar]
- 164.Viola-Saltzman M, Musleh C. Traumatic brain injury-induced sleep disorders. Neuropsychiatr Dis Treat. 2016;12:339. doi: 10.2147/NDT.S69105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Luther M, Poppert Cordts KM, Williams CN. Sleep disturbances after pediatric traumatic brain injury a systematic review of prevalence risk factors and association with recovery. Sleep. 2020;43(10):zsaa083. doi: 10.1093/sleep/zsaa083. [DOI] [PubMed] [Google Scholar]
- 166.Pillar G, Averbooch E, Katz N, Peled N, Kaufman Y, Shahar E. Prevalence and risk of sleep disturbances in adolescents after minor head injury. Pediatr Neurol. 2003;29(2):131–135. doi: 10.1016/S0887-8994(03)00149-8. [DOI] [PubMed] [Google Scholar]
- 167.Kaufman Y, Tzischinsky O, Epstein R, Etzioni A, Lavie P, Pillar G. Long-term sleep disturbances in adolescents after minor head injury. Pediatr Neurol. 2001;24(2):129–134. doi: 10.1016/S0887-8994(00)00254-X. [DOI] [PubMed] [Google Scholar]
- 168.Ouellet M-C, Beaulieu-Bonneau S, Morin CM. Sleep-wake disturbances after traumatic brain injury. The Lancet Neurology. 2015;14(7):746–757. doi: 10.1016/S1474-4422(15)00068-X. [DOI] [PubMed] [Google Scholar]
- 169.Peña M-M, Rifas-Shiman SL, Gillman MW, Redline S, Taveras EM. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep. 2016;39(9):1653–1661. doi: 10.5665/sleep.6086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sheares BJ, Kattan M, Leu C-S, Lamm CI, Dorsey KB, Evans D. Sleep problems in urban, minority, early-school-aged children more prevalent than previously recognized. Clin Pediatr. 2013;52(4):302–309. doi: 10.1177/0009922813476573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Johnson DA, Billings ME, Hale L. Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Current epidemiology reports. 2018;5(2):61–69. doi: 10.1007/s40471-018-0139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Biggs SN, Lushington K, Martin AJ, van den Heuvel C, Kennedy JD. Gender, socioeconomic, and ethnic differences in sleep patterns in school-aged children. Sleep Med. 2013;14(12):1304–1309. doi: 10.1016/j.sleep.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 173.Chervin RD, Clarke DF, Huffman JL, Szymanski E, Ruzicka DL, Miller V, et al. School performance, race, and other correlates of sleep-disordered breathing in children. Sleep Med. 2003;4(1):21–27. doi: 10.1016/s1389-9457(02)00243-5. [DOI] [PubMed] [Google Scholar]
- 174.Roberts RE, Roberts CR, Chen IG. Ethnocultural differences in sleep complaints among adolescents. J Nerv Ment Dis. 2000;188(4):222–229. doi: 10.1097/00005053-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 175.Dai Y, Liu J. Parental perceived child sleep problems: a concept analysis. J Spec Pediatr Nurs. 2021;26(2):e12327. doi: 10.1111/jspn.12327. [DOI] [PubMed] [Google Scholar]
- 176.Harkness S, Super CM. Parents’ cultural belief systems: Their origins, expressions, and consequences. Whole: Guilford Press; 1996. [Google Scholar]
- 177.Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;115(Supplement 1):241–249. doi: 10.1542/peds.2004-0815F. [DOI] [PubMed] [Google Scholar]
- 178.Ji X, Li J, Liu J. The relationship between midday napping and neurocognitive function in early adolescents. Behav Sleep Med. 2019;17(5):537–551. doi: 10.1080/15402002.2018.1425868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Meltzer LJ, Johnson C, Crosette J, Ramos M, Mindell JA. Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics. 2010;125(6):e1410–e1418. doi: 10.1542/peds.2009-2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Mindell JA, Sadeh A, Kwon R, Goh DYT. Cross-cultural differences in the sleep of preschool children. Sleep Med. 2013;14(12):1283–1289. doi: 10.1016/j.sleep.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 181.Milan S, Snow S, Belay S. The context of preschool children’s sleep: racial/ethnic differences in sleep locations, routines, and concerns. J Fam Psychol. 2007;21(1):20. doi: 10.1037/0893-3200.21.1.20. [DOI] [PubMed] [Google Scholar]
- 182.Jeon M, Dimitriou D, Halstead EJ. A systematic review on cross-cultural comparative studies of sleep in young populations: the roles of cultural factors. Int J Environ Res Public Health. 2021;18(4):2005. doi: 10.3390/ijerph18042005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Troxel WM, DeSantis A, Richardson AS, Beckman R, Ghosh-Dastidar B, Nugroho A, et al. Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration. Sleep. 2018;41(10):zsy140. doi: 10.1093/sleep/zsy140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Bagley EJ, Fuller-Rowell TE, Saini EK, Philbrook LE, El-Sheikh M. Neighborhood economic deprivation and social fragmentation: associations with children’s sleep. Behav Sleep Med. 2018;16(6):542–552. doi: 10.1080/15402002.2016.1253011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sheehan C, Powers D, Margerison-Zilko C, McDevitt T, Cubbin C. Historical neighborhood poverty trajectories and child sleep. Sleep Health. 2018;4(2):127–134. doi: 10.1016/j.sleh.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Spilsbury JC, Storfer-Isser A, Kirchner HL, Nelson L, Rosen CL, Drotar D, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr. 2006;149(3):342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 187.Wang R, Dong Y, Weng J, Kontos EZ, Chervin RD, Rosen CL, et al. Associations among neighborhood race and sleep apnea severity in children. a six-city analysis. Annals Am Thoracic Soc. 2017;14(1):76–84. doi: 10.1513/AnnalsATS.201609-662OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Paksarian D, Rudolph KE, He J-P, Merikangas KR. School start time and adolescent sleep patterns: results from the US national comorbidity survey—adolescent supplement. Am J Public Health. 2015;105(7):1351–1357. doi: 10.2105/AJPH.2015.302619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bowers JM, Moyer A. Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: a meta-analysis. Sleep Health. 2017;3(6):423–431. doi: 10.1016/j.sleh.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 190.Owens JA, Belon K, Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch Pediatr Adolesc Med. 2010;164(7):608–614. doi: 10.1001/archpediatrics.2010.96. [DOI] [PubMed] [Google Scholar]
- 191.Owens J, Au R, Carskadon M, Millman R, Wolfson A, Braverman PK, et al. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–e932. doi: 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10(5):323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 193.Zunhammer M, Eichhammer P, Busch V. Sleep quality during exam stress: the role of alcohol, caffeine and nicotine. PLoS ONE. 2014;9(10):e109490. doi: 10.1371/journal.pone.0109490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Ginsberg J. Academic worry as a predictor of sleep disturbance in college students. J Young Investigators. 2006.
- 195.Au R, Carskadon M, Millman R, Wolfson A, Braverman PK, Adelman WP, et al. School start times for adolescents. Pediatrics. 2014;134(3):642–649. doi: 10.1542/peds.2014-1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet (London, England) 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, Somekh E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J Pediatr. 2020;221:264-6.e1. [DOI] [PMC free article] [PubMed]
- 198.Alfano CA, Ginsburg GS, Kingery JN. Sleep-related problems among children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(2):224–232. doi: 10.1097/01.chi.0000242233.06011.8e. [DOI] [PubMed] [Google Scholar]
- 199.Liu J, Glenn AL, Cui N, Raine A. Longitudinal bidirectional association between sleep and behavior problems at age 6–11 years. Sleep Med. 2021;83:290–298. doi: 10.1016/j.sleep.2021.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 201.What is sleep quality? https://www.thensf.org/what-is-sleep-quality/. Accessed 1 Feb 2021.
- 202.Sateia MJ. International classification of sleep disorders. Chest. 2014;146(5):1387–1394. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 203.Carter KA, Hathaway NE, Lettieri CF. Common sleep disorders in children. Am Fam Physician. 2014;89(5):368–377. [PubMed] [Google Scholar]
- 204.Shen Y-L, Liu W-T, Lee K-Y, Chuang H-C, Chen H-W, Chuang K-J. Association of PM2 5 with sleep-disordered breathing from a population-based study in Northern Taiwan urban areas. Env Poll. 2018;233:109–113. doi: 10.1016/j.envpol.2017.10.052. [DOI] [PubMed] [Google Scholar]
- 205.Liu Y, Zhang J, Li SX, Chan NY, Yu MWM, Lam SP, et al. Excessive daytime sleepiness among children and adolescents: prevalence, correlates, and pubertal effects. Sleep Med. 2019;53:1–8. doi: 10.1016/j.sleep.2018.08.028. [DOI] [PubMed] [Google Scholar]
- 206.Becker SP, Ramsey RR, Byars KC. Convergent validity of the child Behavior checklist sleep items with validated sleep measures and sleep disorder diagnoses in children and adolescents referred to a sleep disorders center. Sleep Med. 2015;16:79–86. doi: 10.1016/j.sleep.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 207.Owens JA, Spirito A, McGuinn M. The children’s sleep habits questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep-New York- 2000;23:1043–1052. [PubMed] [Google Scholar]
- 208.Bruni O, Ottaviano S, Guidetti V, Romoli M, Innocenzi M, Cortesi F, et al. The sleep disturbance scale for children (SDSC) construct ion and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251–261. doi: 10.1111/j.1365-2869.1996.00251.x. [DOI] [PubMed] [Google Scholar]
- 209.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 210.Iii SA. Sleep assessment methods. Monogr Soc Res Child Dev. 2015;80:33–48. doi: 10.1111/mono.12143. [DOI] [PubMed] [Google Scholar]
- 211.Sadeh A, Lavie P, Scher A. Sleep and temperament: maternal perceptions of temperament of sleep-disturbed toddlers. Early Educ Dev. 1994;5:311–322. doi: 10.1207/s15566935eed0504_6. [DOI] [Google Scholar]
- 212.Chung K-F, Kan KK-K, Yeung W-F. Assessing insomnia in adolescents: comparison of insomnia severity index, athens insomnia scale and sleep quality index. Sleep Med. 2011;12:463–470. doi: 10.1016/j.sleep.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 213.Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Badia P. The pediatric daytime sleepiness scale (PDSS): sleep habits and school outcomes in middle-school children. Sleep. 2003;26:455–458. [PubMed] [Google Scholar]
- 214.Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Ancoli-Israel S, et al. Relationships among sleepiness, sleep time, and psychological functioning in adolescents. J Pediatr Psychol. 2009;34:1175–1183. doi: 10.1093/jpepsy/jsp039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115:257–265. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Storfer-Isser A, Lebourgeois MK, Harsh J, Tompsett CJ, Redline S. Psychometric properties of the a dolescent sleep hygiene scale. J Sleep Res. 2013;22:707–716. doi: 10.1111/jsr.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.de Bruin EJ, van Kampen RK, van Kooten T, Meijer AM. Psychometric properties and clinical relevance of the adolescent sleep hygiene scale in Dutch adolescents. Sleep Med. 2014;15:789–797. doi: 10.1016/j.sleep.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 218.Meltzer LJ, Avis KT, Biggs S, Reynolds AC, Crabtree VM, Bevans KB. The children’s report of sleep patterns (CRSP): a self-report measure of sleep for school-aged children. J Clin Sleep Med. 2013;9:235–245. doi: 10.5664/jcsm.2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Meltzer LJ, Brimeyer C, Russell K, Avis KT, Biggs S, Reynolds AC, et al. The children’s report of sleep patterns: validity and reliability of the sleep hygiene index and sleep disturbance scale in adolescents. Sleep Med. 2014;15:1500–1507. doi: 10.1016/j.sleep.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Bartel K. Protective and Risk Factors for Adolescent Sleep Health. Flinders University, School of Psychology. 2017.
- 221.Rundo JV, Downey R., III Polysomnography. Clin Neur. 2019;160:381–392. doi: 10.1016/B978-0-444-64032-1.00025-4. [DOI] [PubMed] [Google Scholar]
- 222.Ancoli-Israel S, Martin JL, Blackwell T, Buenaver L, Liu L, Meltzer LJ, et al. The SBSM guide to actigraphy monitoring: clinical and research applications. Behav Sleep Med. 2015;13:S4–S38. doi: 10.1080/15402002.2015.1046356. [DOI] [PubMed] [Google Scholar]