Abstract
Objectives
Primary Health Care (PHC) oriented health systems are crucial to accelerate the achievement of Universal Health Coverage. Previous studies have suggested the importance of participatory approaches to improve PHC. This review aimed to identify the available published implementation research in PHC considering participatory approaches in Low and Middle-Income Countries (LMICs).
Study design
A narrative review was conducted following the standard guidelines.
Methods
Three electronic databases were searched where keywords were combined using Boolean operators. Studies were included considering the pre-specified inclusion and exclusion criteria through two-phase screening. The quality of the included studies was assessed using the Joanna Briggs Institution's critical appraisal tools. Data were presented using a narrative synthesis approach.
Results
A total of 13 articles were included that focused on community-based approaches in PHC service, maternal and newborn care, family planning, tuberculosis, and mental health. Three studies focused on mental health and demonstrated the efficacy of community support groups, peer volunteers, and community-based mental education in promoting mental health services. Two studies described community participation to ensure patient safety and risk reduction. Other studies explored the effectiveness of community-based, directly observed treatment for tuberculosis; community health worker-based maternal and child health care; and a community-based package for family planning. Eleven studies were conducted in Africa and the rest were in South Asia.
Conclusion
This review reveals the gap in implementation research incorporating participatory approaches in the field of PHC. Limited studies have been conducted which indicate the need and scope of implementation research with participatory approaches in the PHC field.
Prospero registration
CRD42020150749.
Keywords: PHC, Implementation research, LMICs, Participatory, Community-based
1. Introduction
Primary health care (PHC) can play a pivotal role in achieving universal health coverage (UHC) and the targets oriented around health-related sustainable development goals (SDGs) [1]. Different studies have demonstrated the importance of PHC in achieving the targets of SDG-3 (Good Health and Wellbeing) [1]. Evidence suggests that effective and strategic implementation of PHC interventions can improve maternal, newborn, and child health care and reduce mortality [2]. Globally, lifestyle modification interventions combat the non-communicable disease burden. Strengthening the PHC supports might overcome the challenges of the increased burden of chronic diseases [3]. PHC can play a role in ensuring equitable and accessible services to the majority of the population. It can contribute to promoting health and strengthening the health systems [4]. However, proper measurement and implementation of successful models of care will enhance the quality of service and effectiveness of PHC [5].
Low and Middle-Income Countries (LMICs) struggle with the dual burden of both infectious and chronic diseases in resource-poor settings. PHC offered better access to care in LMICs. PHC also improved health coverage, lowered the service cost, reduced morbidity, and mortality, and improved the overall health systems [6]. The cost-effective interventions harbored by PHC are promising in the context of LMICs [7]. In low-resource settings, engaging the community and utilizing PHC brings positive results in addressing the emerging disease burden caused by non-communicable diseases (NCDs) [8]. Governance is one of the prime building blocks in health systems, and studies suggested that enhanced accountability is vital to improving PHC in LMICs [9]. Most of the research on PHC is focused on service delivery. However, some researchers have explored performance measurement and management at the PHC level. These studies also emphasized the lack of research across accountability and governance [10]. Community engagement is evident to improve service delivery. The most effective measures with supportive supervision and a referral system are community-based services [11]. Community engagement has also emphasized improving accountability and governance through social responsibility [9].
Implementation research (IR) identifies the enablers and barriers to uptake of evidence-based intervention and attempts to address these to enable uptake and further scale-up [12]. IR is one of the efficacious and suitable tools for achieving UHC. IR provides the knowledge base to the policymakers and program managers and contributes to efficient health outcomes at the same time [12]. Community participatory research is an approach that has community members actively engaged in the research process. IR engaging communities and other stakeholders are supposed to be effective in problem identification, finding solutions, and prioritizing actions. Thus, IR can play a role in strengthening the PHC and accelerating the progress to achieve UHC and SDGs. This review, therefore, is an exploration to gather information on two vital factors that might influence the PHC system and service. We aimed to identify the available published researches that incorporated both the implementation research approach and the participatory approach in PHC settings. The specific review question for this review was: “What are the available implementation researches incorporating participatory approaches in Primary Health Care settings in LMICs?” We systematically identified the available evidence on participatory approaches of implementation research in primary health care in LMIC settings. This review also explored the knowledge gap in terms of the availability of published research and future scope of work based on the identified research gap in this field in LMICs.
2. Study design
We conducted a narrative review following the steps of a systematic review. In this review, the screening, data extraction, and quality assessment was conducted by a single author in contrast to a dual activity independently in a systematic review. However, a second review author cross-checked the full-text screening, data extraction, and quality assessment of included studies.
3. Methods
The review is consistent with the guidelines of preferred reporting items for systematic review and meta-analysis [13]. We registered the review at the international prospective register of systematic reviews - PROSPERO (CRD42020150749). We searched three electronic databases (Medline through Pubmed, Cochrane database, and Web of Science) using a comprehensive search strategy. We combined the keywords using Boolean operators. We applied the truncation and wildcards where necessary. The search strategy for Pubmed was as follows:
# 1: (((("Community-Based Participatory Research") OR Implementation) OR Research) OR “Implementation Research”) OR IR.
# 2: (“Primary Healthcare”) OR PHC.
# 3: (Participat*) OR Embed*
# 4: 1 AND 2 AND 3.
We screened the retrieved articles using title-abstract screening and full-text screening in two phases. We applied the pre-specified inclusion and exclusion criteria. We included the articles describing participatory approaches for PHC-related implementation research in LMICs. LMICs were identified as per the definition provided by the World Bank [14]. The specific inclusion criteria are as follows: 1) the research method should incorporate an implementation research approach, 2) the research should incorporate a participatory approach, 3) the research should be conducted in PHC settings, 4) the research should be conducted in LMICs. We excluded the articles using the following exclusion criteria: 1) not in PHC settings, 2) not conducted in LMICs, 3) not describing participatory or community-based approaches, and 4) not focusing on implementation research. There was no limitation for publication year. However, we excluded the articles written in languages other than English. All research designs were taken into account. Editorials, comments, and letters to editors were not considered. Review authors applied the 'prioritization and sequential exclusion' method throughout the screening process [15]. In this method, the exclusion criteria are prioritized as a priori and articles are excluded sequentially as per the order of prioritization. The details description of the method has been described elsewhere [15]. Data were extracted from the included articles to describe the publication year, study design, geographic region, main health focus, population characteristics including age, gender, urban and rural distribution, the description of the intervention, and outcome. The second review author cross-checked the screening, data extraction, and data analysis. The third review author resolved any dispute between the two reviewers.
The quality of the independent studies was assessed using the Joanna Briggs Institution's critical appraisal tools for randomized controlled trials (RCTs), quasi-experimental studies, cross-sectional studies, and qualitative studies [16]. The main quality assessment points for RCTs were randomization, allocation concealment, blinding at the level of participants, implementers, outcome assessors, the similarity of groups at baseline, completion of follow-up, measurement of outcome using appropriate statistics, and any deviation from the standard design. Quasi-experimental studies were assessed using the points for causal effect, the inclusion of similar participants in both groups, multiple measurements of the outcome, completion of follow-up, and use of reliable and appropriate statistical analysis. For the qualitative studies, congruity between the research question, study objective, methods, analysis, interpretation, and the conclusion was considered. The review authors explored the ethical aspect and influence of the researcher on research as well. Descriptive studies were assessed based on criteria for inclusion, measurement of exposure, addressing confounding, measurement of outcome, and use of appropriate statistical methods. The second review author cross-checked the quality assessment of the articles.
We considered the narrative synthesis to summarize the findings from extracted data. Meta-analysis was not feasible due to heterogeneity and variation of included articles.
4. Results
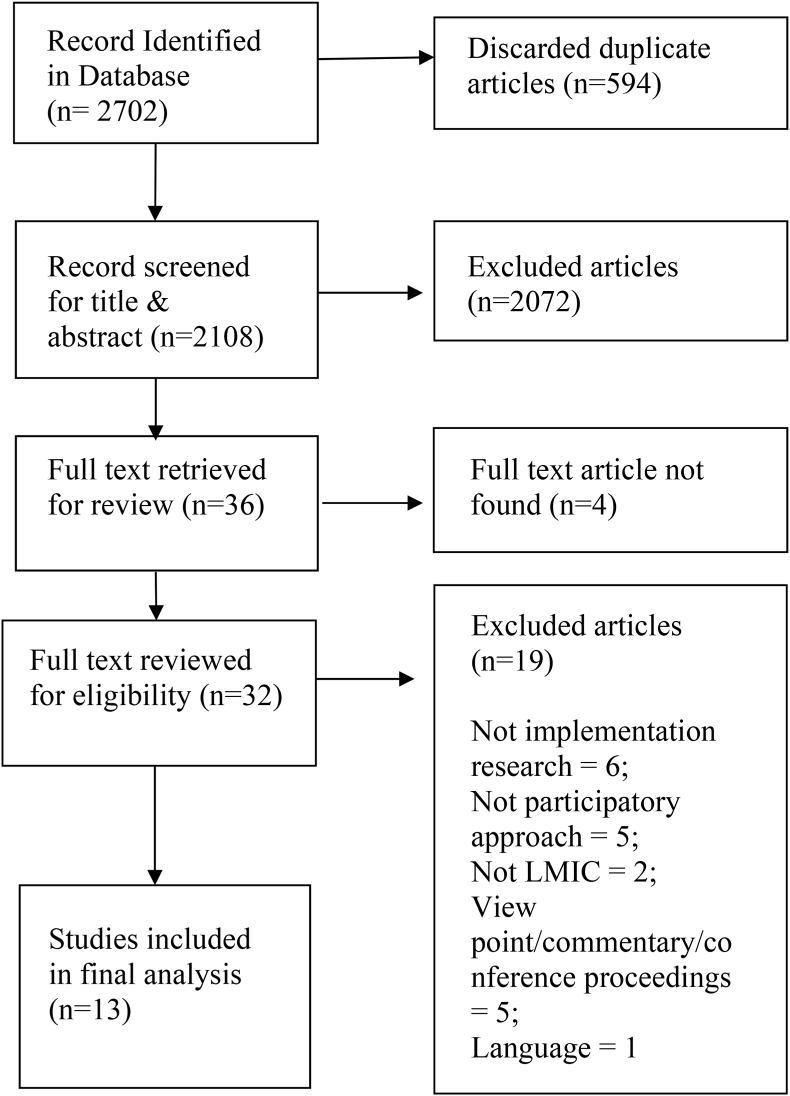
Search outcome: The review authors searched the databases using a comprehensive search strategy in November 2021. Searching three databases retrieved 2702 articles, of which 594 articles were duplicates. Screening for title and abstract included 36 articles, and finally, review authors included 13 articles after a full-text review. Details of the search outcome have been demonstrated in Fig. 1.
Fig. 1.
PRISMA flow diagram.
Description of studies: All the articles were published between 2002 and 2021. Two studies were RCTs [17,18], five were qualitative in design [[19], [20], [21], [22], [23]], three were quasi-experimental [[24], [25], [26]] two were cross-sectional studies [27,28], and one was program implementation [29]. Almost all the studies were in the African region (four studies in South Africa, two in Ghana, and one study in Sudan, Nigeria, Malawi, Tanzania, and Burkina Faso, and DRC each) and, only two were from South Asia (Bangladesh, Pakistan). Studies focused on quality of care in PHC (n = 5), mental health care (n = 3), maternal and newborn care (n = 3), tuberculosis, and family planning. All the studies were conducted in urban areas except for a peri-urban study. Two studies were focused on females and the rest of the studies included both genders. The characteristics of the included studies have been shown in Table 1.
Table 1.
Characteristics of included studies.
| Author and Publication Year | Country | Health focus | Intervention and target population | Outcome | Lessons learned |
|---|---|---|---|---|---|
| Alhassan et al., 2015 [17] | Ghana | Patient safety and quality of care in PHC | Systematic community engagement (SCE) - both gender, 18 years and older | 1. Efforts towards increasing patient safety and reduced risk improved significantly | SCE increased patient safety and reduced risk reduction. |
| Barker et al., 2007 [27] | South Africa | PHC | Community participation in PHC projects to both gender, all age group | 1. Community participation was broadened. 2. There was minimal shift in power over decision making and resources. | Community participation increased community engagement. |
| Mahmood et al., 2020 [22] | Bangladesh | PHC | Community based community scorecard (CSC) intervention to both gender, all age group | 1. The community scorecard is a practical and accepted method for including the public and healthcare providers in the monitoring and management of health facilities. 2. In order for CSC to be effective at scale, proper contextualization, institutional capacity building, and policy integration will be necessary. | Community scorecards have the potential to improve health service delivery at the community level, especially in countries where health systems confront issues in terms of accountability, quality, and coverage. |
| Sakeah et al., 2021 [23] | Ghana | PHC | Community members and health professionals' participation in PHC projects to both gender,18 years and older | 1. By organizing communities for health initiatives and providing basic healthcare services in rural places, the CHPS program plays a vital role in primary health care. | The involvement of self-motivated community health volunteers and health professionals are Strengthening health service at community level |
| Makaula et al., 2019 [25] | Malawi | PHC | Community-directed intervention (CDI) approach both gender, all age group among villagers | 1. The CDI strategy may be used in rural locations and is feasible, acceptable, and effective. 2.CDI has been shown to increase LLIN in children under the age of five and pregnant women. | Strengthening the primary health care system in rural areas is aided by the introduction of CDI. |
| Tomlinson et al., 2014 [18] | South Africa | Maternal and newborn HIV care | CHW home visit to Pregnant women, 17 years and older |
1. Level of exclusive and appropriate breast feeding. 2. Level of HIV free survival. 3. Uptake of post-natal clinic visit. 4. Coverage of care and behavioral indicators. 5. Level of post intervention maternal depression |
CHW home visit increases level of uptake, coverage of health care and changed behavior of community. |
| Maluka et al., 2020 [26] | Tanzania | Maternal and child health | Community based maternal and child health education to male participants | 1. The participatory approach to male involvement can help the treatments last longer than the project's lifespan. 2. Men rarely attend health facilities, although women have access to health education at ANC clinics. |
By developing culturally acceptable strategies can increase male involvement in MCH. Improving couple relationships will increase male participation in MCH. |
| Eboreime et al., 2019 [24] | Nigeria | Maternal Health and Early Infant care | Community based maternal and child health education to pregnant woman | 1. Using a participatory action research (PAR) approach to execute the Diagnose-Intervene-Verify-Adjust (DIVA) model could be a useful way for managing the challenges of planning and delivering health interventions in similar situations. | Including PAR in maternal and child health intervention can improve the quality of the health service. |
| El-Gaili et al., 2002 [29] | Sudan | Mental Health | Community based mental health education to both gender, all age group | 1. Modify community concept, attitude and practice regarding mental health. 2. Ensure community participation in mental health service delivery. 3. Extend mental health service delivery involving PHC settings and traditional healing centers. 4. Train the staff in PHC settings. 5. Research in community needs and demands | Community based mental health education changed community concept, attitude and practice, ensured community engagement in MH services from PHC and developed capacity. |
| Atif et al., 2016 [19] | Pakistan | Maternal Mental Health | Peer volunteers for maternal mental health care to mother's, 21 years and older | 1. Acceptance of peer volunteers as service delivery staff. | Volunteers may contribute substantially and reduce workload of the health worker. |
| Meiring et al., 2017 [20] | South Africa | Mental health care | Student facilitated community-based support group for both genders, 23 years and older |
1. The support group offered the participants a sense of belongingand a means of social and emotional support. 2. The support group created opportunity forlearning, encouraged mental and physical mobilization and stimulation. 3. The support group served as anadditional link to professional services. | Support group involved participants socially and emotionally, created opportunity for learning, encouraged mental, physical mobilization and most importantly served as an additional link to professional services. |
| Tran et al., 2018 [21] | Burkina Faso, DRC | Family Planning | N/A; Pregnant or post-partum women, of reproductive age group |
1. Identified a common package of six low-cost, low-technology, and easily-scalable interventions that addressed the main service delivery obstacles related to PPFP. | Community participation is important for contextualization of interventions to address the bottlenecks. |
| Kironde et al., 2002 [28] | South Africa | Tuberculosis | Community based DOT to Confirmed TB patients both gender, | 1. Community-based DOT was equivalent to clinic based and self-administered treatment for new patients. 2. Community based DOT is superior to self-administered treatment for re-treatment patients. | Community based program saves commutation, reduces patient load at health facility and empowers community to take responsibility of own health. |
Description of interventions and outcomes: The interventions were provided to improve the quality of PHC, care for the mother and newborn, mental health, family planning, and tuberculosis treatment. A detailed description and the outcomes have been provided below.
4.1. Interventions to improve quality of PHC
The RCT conducted by Al Hassan et al. evaluated the effect of community engagement on patient safety and risk reduction in primary care facilities [17]. A total of 64 health centers were randomly allocated, and systematic community engagement interventions were provided to the intervention group over one year. Existing community groups were utilized through trained facilitators to explore the service delivery gap. The service utilization rate and health resources were not improved, but there was a significant improvement in leadership and accountability (Coefficient 10.4; p < 0.05) and staff competency (coefficient 7.1; p < 0.05). A descriptive study in South Africa described by Barker et al. explored and evaluated the level of community participation in PHC projects [27]. This study highlighted that community participation would not be much effective until they were engaged in the decision-making process, planning, and resource mobilization.
Mahmood et al. conducted a qualitative pilot study in Bangladesh to explore the feasibility and acceptability of implementing CSC at community clinics that provide primary healthcare [22]. The study focused on the feasibility, acceptability, initial results, and problems of applying CSC in community clinics. The scorecard process resulted in some positive changes in different dimensions, including quality and accountability in health service delivery, community participation in health, revenue generation for health, and raising community awareness, over the course of three cycles over a ten-month period. As an outcome, the community scorecard is a practical and accepted method to engage community and healthcare providers in the monitoring and management of health facilities.
Another qualitative study has recently been done by Sakeah et al. in Ghana that represented the participation of community members and health professionals in PHC projects [23]. Focus group discussions (FGDs) and in-depth interviews (IDIs) with health professionals and community stakeholders were done for this study. A total of 33 focus groups with pregnant women, nursing mothers, and men and women, as well as 51 individual interviews, were held. Females accounted for 63% of the IDIs respondents. This research demonstrated that by organizing communities for health initiatives and providing basic healthcare services in rural places, the CHPS (Community-based Health Planning Services) program plays a vital role in primary health care.
In addition, a quasi-experimental study represented by Makaula et al. to determine the community-based CDI (Community-Directed Interventions) approach for Strengthening primary health care at the district level in Malawi [25]. This was 12-month comparative intervention research involving four health centers and 16 villages having a total population of 20,438 people. The intervention components of this study included home management of malaria (HMM) and fever in children under the age of five, distribution of long-lasting insecticide-treated nets (LLIN) to children under the age of five and pregnant women, vitamin A distribution to children under the age of five, and treatment of urinary schistosomiasis with Praziquantel (PZQ) in those over the age of five. Differences between intervention and control groups were statistically significant for LLIN distribution in children under 5 years of age (p-value 0.003) and pregnant women (p-value 0.0075) but not for the remaining four intervention components. For successful implementation, the study revealed several essential aspects that must be evaluated and tailored to local situations. Overall, the CDI strategy in rural areas is practicable, acceptable, and effective at the community level, resulting in improved PHC service delivery.
4.2. Interventions to improve care for the mother and newborn
A cluster-randomized effectiveness trial in South Africa by Tomlinson et al. evaluated the integrated community-based package for maternal and newborn care [18]. Women in neighboring areas were recruited as community health workers and trained to provide the intervention package including home visits for maternal care, newborn care, and lactation counseling. Mothers in the intervention arm received seven home visits in antenatal and postnatal periods with two extra visits if the newborn was low birth weight. The control arm received one antenatal visit and two post-natal visits where home-based education and assistance were provided for administrative services. As an outcome, the percentage of exclusive breastfeeding increased in the intervention arm (28.6%) in comparison to the control arm (15%) which was statistically significant (Relative risk 1.92; 95% CI: 1.59–2.33). There were no significant differences between intervention and control groups in terms of other outcomes except increased preparation for birth and increased knowledge of newborn danger signs among mothers in the intervention group.
Male participants received community-based mother and child health education was explored in a quasi-experimental study in two districts in Tanzania by Maluka et al. as a part of participatory action research (PAR) [26]. Separately, men and women were asked to identify impediments to male involvement in antenatal care and delivery, and then they were aided in developing initiatives to enhance male participation in local communities. The data were analyzed using thematic analysis. Engaging health facility committees, employing male champions and gatekeepers, and using female champions to sensitize and deliver health information to women were all frequent techniques devised. These methods were confirmed at stakeholder meetings that were held in each neighborhood. The use of a participatory approach not only empowers communities to identify impediments to male participation and design culturally appropriate strategies but also promotes the long-term sustainability of the initiatives.
Another Quasi-Experimental Study conducted by Eboreime et al. evaluated Community based maternal and child health education for pregnant women in Nigeria [24]. In a Nigerian sub-national context, this study showed how incorporating participatory action research (PAR) into a quality improvement model might aid in navigating the intricacies of health system bottleneck analysis, planning, and performance improvement. PAR was incorporated into the DIVA (Diagnose-Intervene-Verify-Adjust) quality improvement paradigm, which was applied to a number of interventions (eMTCT, Antenatal care, skilled birth attendance, immunization, and Integrated Management of Childhood Illnesses). PAR was used to identify and analyze bottlenecks in the healthcare system, as well as establish, monitor, and follow up on action plans to address them. In the first and second DIVA cycles, mean improvements were 20.4%, 14.0%, and 10.8%, 11.2%, 7.5%, and 5.5% (across eMTCT, maternal health, and child health interventions) respectively. This study focuses on the processes and consequences of incorporating PAR into quality improvement design and operations in health intervention programs in Nigeria, with an emphasis on strengthening health systems.
4.3. Interventions to improve mental health
El-Gaili et al. conducted a study in Sudan and described the impact of a community-based medical school on mental health [29]. The aim of establishing the medical school was to the positive transformation of the community concept of mental health by ensuring community participation. There was an improved perception of community people regarding mental health and care. The service utilization, community-based activities, and scope of research were also increased. A qualitative study in Pakistan conducted by Atif, N. et al. explored the barriers to providing maternal mental health care through peer volunteers [19]. This qualitative study was embedded in a larger peer-delivered program where lay women sharing similar sociodemographic characteristics and experiences acted as peer volunteers. Peer volunteers were well accepted as they were local, empathetic, and went through similar experiences. They were self-motivated because of appropriate training, supervision, incentives, and community recognition. Still, there were challenges such as social stigma on depression, cultural norms, lack of autonomy of mothers, and resistance from conservative families. A similar qualitative study was conducted by Meiring et al. in the Tshwane district in South Africa [20]. Psychology students worked as a support group for the mental health nurses at primary care centers who provided support to the mental health care users. The support group could provide emotional support to the participants and supplemented the available professional services.
4.4. Interventions to improve family planning
A qualitative study as a part of participatory action research was conducted by Tran et al. in Burkina Faso and the Democratic Republic of Congo [21]. The barriers and facilitators of post-partum family planning uptake were explored through the participation of different stakeholders. This study identified that refresher training and supportive supervision of service providers could improve the postpartum family planning uptake.
4.5. Interventions to improve tuberculosis treatment
Treatment of tuberculosis provided by the lay volunteers at the community level in primary care settings was explored by Kironde et al. in a descriptive study in South Africa [28]. This study compared the Tuberculosis treatment options namely clinic-based directly observed therapy (DOT), community-based DOT, and self-administered therapy. In this study, treatment outcomes for patients receiving care from lay health workers were as effective as clinic-based supervision. In the case of re-treatment patients, treatment outcome was better than self-administered medication.
Quality assessment of included studies: Both the RCTs mentioned randomization, but there was no information regarding allocation concealment. Treatment groups were similar at baseline in both cases. Blinding of the participants and outcome assessors was mentioned by the study conducted in Ghana [17] but was not mentioned in the cluster-randomized trial [18]. Conversely, implementers were blinded in the cluster-randomized trial but not in the RCT conducted in Ghana. Appropriate design, completion of follow-up, appropriate analysis technique, reliable measurement of outcome, and appropriate statistical analysis were maintained in both trials.
Congruity between the philosophical perspective and research methodology was found in almost all the qualitative studies except one [20]. There was congruity between methodology and research objective, methodology, and data collection and analysis, methodology, and interpretation of results in all five studies. No statement was found regarding the researchers' position or influence in any of the studies except in one study conducted by Meiring et al. The participant's voice was well represented, ethical approval was obtained and conclusions were drawn based on analysis and interpretation in all the qualitative studies.
Both the descriptive studies clearly defined the criteria for inclusion, study settings, measurement of exposures, and measurement of outcome in a valid and reliable way and used appropriate statistical analysis. None of the studies mentioned confounders or the strategies to deal with confounders.
All the quasi-experimental studies clearly stated the “cause” and “effect”, outcomes measured, and appropriate statistical analysis. Comparison's participants and treatment were not applicable in any studies except one study [25]. Out of three studies, one study had a control group [25]. Almost all studies, except one [26], clearly described completing the follow-up and multiple outcome measurements both before and after the intervention. Among three studies two were measured comparisons and the rest of the study was not applicable for this statement [26].
The quality assessment of the article by El-Gaili et al. [29] was not conducted as that was a description of program implementation and didn't suit any quality assessment tool.
5. Discussions
This review was undertaken to systematically explore and identify the available research incorporating implementation research with participatory approaches in PHC. Identified studies covered both infectious diseases and non-communicable diseases, but mostly focused on maternal and newborn care and mental health. Most of the studies were conducted in the Sub Saharan African context and there was no study from East-Asia and Pacific, Europe and Central Asia, Latin America and the Caribbean, and the Middle East and North Africa. There are success stories of PHC in both Latin America and Southeast Asia. Cuba and Chile have exemplary case studies of effective PHC service [30,31]. Another successful implementation of PHC strategies is in Kerala, a state of India [32]. However, no study was found describing any implementation research incorporating a participatory approach from these regions.
The included studies that focused on non-communicable diseases (NCDs), described the participatory approaches of IR in mental health-related programs [19,20,29]. Mental health is very important in today's world and community-based participatory approaches could effectively address the challenges of mental health care. The findings from this review might be replicated in other LMICs including the South Asian and Latin American regions. Surprisingly, none of the studies explained the major four NCDs including cancer or diabetes. Community-based approaches have been proved to be effective in previous studies [33]. Similar findings have been observed in studies exploring diabetic care [34]. Field experience from Samoa shared the effectiveness of community engagement in a campaign for NCD screening [8]. Thus, similar approaches could be adapted to the primary care settings in LMICs. Our findings unveil this gap in available researches on NCDs in LMIC countries. There are some studies in LMIC settings utilizing community-based approaches [35], but they didn't emphasize the PHC perspective.
This review identified the effectiveness of participatory approaches in improving primary health care [22,23,25,27], maternal and child care [18,24,26], care for tuberculosis patients [28], patient safety and quality of care [17], and mental health care [19,20]. It underpins the importance of the community-based participatory approach in service utilization, improving access to care, and improved quality of services. This evidence suggests that similar achievements would be possible in other fields of PHC by applying the same approach. Again, most of the research did not focus on governance and accountability. Only one study reported and demonstrated that despite improved community participation, the decision-making process and overall control were not participatory [27]. It reveals the necessity of continued work on improving accountability and transparency in community-based approaches. There is still a huge scope of implementation research across PHC governance and models of care as suggested by recent studies [9,36]. Most of the identified research was conducted in the African context. Similar implementation research embedding participatory approaches in PHC settings can be conducted in other LMICs including South Asia, and Latin America. The participatory IR can be applied in different domains of health systems such as service delivery, human resources, governance, etc. in PHC settings. The findings of this review have got certain implications at the policy level. Participatory approaches and community engagement might be incorporated for better service delivery of mental health, maternal and child care, tuberculosis care, and family planning. As the approach is found promising, it can be applied to other domains such as reproductive health care, adolescent health, geriatric care, infectious disease care, chronic disease care, etc.
The strength of this review is the rigorous methodology following standard norms of evidence synthesis. However, there are certain limitations. As the articles written in English were considered only, we might have missed some studies published in Latin or Chinese languages. Although, only one article was excluded due to language during screening. Still, there is a possibility that a certain number of articles were not captured through the search. Only one reviewer screened and extracted data in this review. This might increase the possibility of bias in the process. To minimize the possible effect, a second reviewer randomly checked and validated the screening outcome and data synthesis. Only a few studies were included due to the specific focus of the study. The combination of all four inclusion criteria possibly has made the focus very specific and narrowed it down. However, the findings indicate the limited work conducted in participatory implementation research in PHC settings in LMICs.
Funding
The authors did not receive any funding for this study.
Author credit statement
Conceptualization: KMSUR Methodology: KMSUR Data curation: KMSUR, SS, SA First draft preparation: KMSAUR Review and Editing: KMSUR, SS, SA, KI Supervision: KI All authors contributed significantly towards the preparation of manuscript and agreed on the final draft before submission.
Data sharing statement
Available upon reasonable request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
icddr,b is grateful to the Governments of Bangladesh, Canada, Sweden, and the UK for providing core/unrestricted support.
References
- 1.Pettigrew L.M., De Maeseneer J., Anderson M.-I.P., Essuman A., Kidd M.R., Haines A. Primary health care and the sustainable development goals. Lancet. 2015;386(10009):2119–2121. doi: 10.1016/S0140-6736(15)00949-6. [DOI] [PubMed] [Google Scholar]
- 2.Bhutta Z.A., Ali S., Cousens S., Ali T.M., Haider B.A., Rizvi A., et al. Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make? Lancet. 2008;372(9642):972–989. doi: 10.1016/S0140-6736(08)61407-5. [DOI] [PubMed] [Google Scholar]
- 3.Beaglehole R., Epping-Jordan J., Patel V., Chopra M., Ebrahim S., Kidd M., et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372(9642):940–949. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 4.Starfield B., Shi L., Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walraven G. The 2018 Astana declaration on primary health care, is it useful? J. Global Health. 2019;9(1) doi: 10.7189/jogh.09.010313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kruk M.E., Porignon D., Rockers P.C., Van Lerberghe W. The contribution of primary care to health and health systems in low- and middle-income countries: a critical review of major primary care initiatives. Soc. Sci. Med. 2010;70(6):904–911. doi: 10.1016/j.socscimed.2009.11.025. (1982) [DOI] [PubMed] [Google Scholar]
- 7.Lewin S., Lavis J.N., Oxman A.D., Bastías G., Chopra M., Ciapponi A., et al. Supporting the delivery of cost-effective interventions in primary health-care systems in low-income and middle-income countries: an overview of systematic reviews. Lancet. 2008;372(9642):928–939. doi: 10.1016/S0140-6736(08)61403-8. [DOI] [PubMed] [Google Scholar]
- 8.Bollars C., Naseri T., Thomsen R., Varghese C., Sørensen K., de Vries N., et al. Adapting the WHO package of essential noncommunicable disease interventions. Samoa Bullet. World Health Org. 2018;96(8):578. doi: 10.2471/BLT.17.203695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saif-Ur-Rahman K.M., Mamun R., Nowrin I., Hossain S., Islam K., Rumman T., et al. Primary healthcare policy and governance in low-income and middle-income countries: an evidence gap map. BMJ Glob Health. 2019;4(Suppl 8) doi: 10.1136/bmjgh-2019-001453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Munar W., Snilstveit B., Aranda L.E., Biswas N., Baffour T., Stevenson J. Evidence gap map of performance measurement and management in primary healthcare systems in low-income and middle-income countries. BMJ Glob Health. 2019;4(Suppl 8) doi: 10.1136/bmjgh-2019-001451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dodd R., Palagyi A., Jan S., Abdel-All M., Nambiar D., Madhira P., et al. Organisation of primary health care systems in low- and middle-income countries: review of evidence on what works and why in the Asia-Pacific region. BMJ Glob Health. 2019;4(Suppl 8) doi: 10.1136/bmjgh-2019-001487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Binagwaho A., Frisch M.F., Udoh K., Drown L., Ntawukuriryayo J.T., Nkurunziza D., et al. Implementation research: an efficient and effective tool to accelerate universal health coverage. Int. J. Health Pol. Manag. 2020;9(5):182–184. doi: 10.15171/ijhpm.2019.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Bank . The World Bank; 2007. Country Groups,” Data and Statistics. [Google Scholar]
- 15.Saif-Ur-Rahman K.M., Hasan M., Hossain S., Anwar I., Hirakawa Y., Yatsuya H. Prioritization and sequential exclusion of articles in systematic reviews. Campbell Syst. Rev. 2022;18(2):e1229. doi: 10.1002/cl2.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Porritt K., Gomersall J., Lockwood C. JBI's systematic reviews: study selection and critical appraisal. AJN Am J. Nurse. 2014;114(6):47–52. doi: 10.1097/01.NAJ.0000450430.97383.64. [DOI] [PubMed] [Google Scholar]
- 17.Alhassan R.K., Nketiah-Amponsah E., Spieker N., Arhinful D.K., Ogink A., van Ostenberg P., et al. Effect of community engagement interventions on patient safety and risk reduction efforts in primary health facilities: evidence from Ghana. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0142389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomlinson M., Doherty T., Ijumba P., Jackson D., Lawn J., Persson L.A., et al. Goodstart: a cluster randomised effectiveness trial of an integrated, community-based package for maternal and newborn care, with prevention of mother-to-child transmission of HIV in a South African township. Trop. Med. Int. Health. 2014;19(3):256–266. doi: 10.1111/tmi.12257. [DOI] [PubMed] [Google Scholar]
- 19.Atif N., Lovell K., Husain N., Sikander S., Patel V., Rahman A. Barefoot therapists: barriers and facilitators to delivering maternal mental health care through peer volunteers in Pakistan: a qualitative study. Int. J. Ment. Health Syst. 2016;10 doi: 10.1186/s13033-016-0055-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meiring L., Visser M., Themistocleous N. A student-facilitated community-based support group initiative for Mental Health Care users in a Primary Health Care setting. Health SA Gesondheid. 2017;22:307–315. [Google Scholar]
- 21.Tran N.T., Yameogo W.M.E., Langwana F., Gaffield M.E., Seuc A., Cuzin-Kihl A., et al. Participatory action research to identify a package of interventions to promote postpartum family planning in Burkina Faso and the Democratic Republic of Congo. BMC Wom. Health. 2018;18(1):122. doi: 10.1186/s12905-018-0573-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahmood S.S., Rasheed S., Chowdhury A.H., et al. Feasibility, acceptability and initial outcome of implementing community scorecard to monitor community level public health facilities: experience from rural Bangladesh. Int. J. Equity Health. 2020 Nov 2;19(1):155. doi: 10.1186/s12939-020-01265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakeah E., Aborigo R.A., Debpuur C., Nonterah E.A., Oduro A.R., Awoonor-Williams J.K. Assessing selection procedures and roles of community health volunteers and community health management committees in Ghana's community-based health planning and services program. PLoS One. 2021;16(5) doi: 10.1371/journal.pone.0249332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eboreime E.A., Idika O., Omitiran K., Eboreime O., Ibisomi L. Primary healthcare planning, bottleneck analysis and performance improvement: an evaluation of processes and outcomes in a Nigerian context. Eval. Progr. Plann. 2019;77 doi: 10.1016/j.evalprogplan.2019.101712. [DOI] [PubMed] [Google Scholar]
- 25.Makaula P., Funsanani M., Mamba K.C., Musaya J., Bloch P. Strengthening primary health care at district-level in Malawi - determining the coverage, costs and benefits of community-directed interventions. BMC Health Serv. Res. 2019;19(1):509. doi: 10.1186/s12913-019-4341-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maluka S., Japhet P., Fitzgerald S., Begum K., Alexander M., Kamuzora P. Leaving no one behind: using action research to promote male involvement in maternal and child health in Iringa region, Tanzania. BMJ Open. 2020;10(11) doi: 10.1136/bmjopen-2020-038823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barker M., Klopper H. Community participation in primary health care projects of the Muldersdrift Health and Development Programme. Curationis. 2007;30(2):36–47. doi: 10.4102/curationis.v30i2.1070. [DOI] [PubMed] [Google Scholar]
- 28.Kironde S., Kahirimbanyi M. Community participation in primary health care (PHC) programmes: lessons from tuberculosis treatment delivery in South Africa. Afr. Health Sci. 2002;2(1):16–23. [PMC free article] [PubMed] [Google Scholar]
- 29.El-Gaili D.E., Magzoub M.M., Schmidt H.G. The impact of a community-oriented medical school on mental health services. Educ. Health. 2002;15(2):149–157. doi: 10.1080/13576280210138661. [DOI] [PubMed] [Google Scholar]
- 30.Spiegel J.M., Yassi A. Lessons from the margins of globalization: appreciating the Cuban health paradox. J. Publ. Health Pol. 2004;25(1):85–110. doi: 10.1057/palgrave.jphp.3190007. [DOI] [PubMed] [Google Scholar]
- 31.Penaloza B., Leisewitz T., Bastias G., Zarate V., Depaux R., Villarroel L., et al. Methodology for evaluating cost-effectiveness in primary health care centers in Chile. Rev. Panam. Salud Públic. 2010;28(5):376–387. [PubMed] [Google Scholar]
- 32.Nair V.M., Thankappan K.R., Vasan R.S., Sarma P.S. Community utilisation of subcentres in primary health care--an analysis of determinants in Kerala. Indian J. Publ. Health. 2004;48(1):17–20. [PubMed] [Google Scholar]
- 33.McCaskill-Stevens W., Lyss A.P., Good M., Marsland T., Lilenbaum R. American Society of Clinical Oncology educational book American Society of Clinical Oncology Annual Meeting; 2013. The NCI Community Oncology Research Program: what Every Clinician Needs to Know. [DOI] [PubMed] [Google Scholar]
- 34.Smith J., Greaves C., Thompson J., Jones M., Walsh A., Sewell L., et al. Taking Control programme; 2015. Community-based Prevention of Diabetes (ComPoD): A Randomised, Waiting List Controlled Trial of the Voluntary Sector-Led Living Well. [Google Scholar]
- 35.Shirinzadeh M., Afshin-Pour B., Angeles R., Gaber J., Agarwal G. The effect of community-based programs on diabetes prevention in low-and middle-income countries: a systematic review and meta-analysis. Glob. Health. 2019;15(1):1–13. doi: 10.1186/s12992-019-0451-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goodyear-Smith F., Bazemore A., Coffman M., Fortier R.D.W., Howe A., Kidd M., et al. 5search gaps in the organisation of primary healthcare in low-income and middle-income countries and ways to address them: a mixed-methods approach. BMJ Glob Health. 2019;4(Suppl 8) doi: 10.1136/bmjgh-2019-001482. [DOI] [PMC free article] [PubMed] [Google Scholar]