Abstract
Although several studies and reports have shown the potential analgesic use of serotonergic psychedelics in cancer pain, phantom limb pain and cluster headache, evidence supporting their use for chronic pain is still limited. The past years have seen a considerable renewal of interest toward the therapeutic use of these compounds for mood disorders, resulting in a marked increase in the number of people turning to psychedelics in an attempt to self-medicate a health condition or improve their wellbeing. In western countries particularly, this population of users overlaps substantially with chronic pain sufferers, representing a unique opportunity to evaluate the effects these compounds have on pain and wellbeing. Here, we report results from an online survey conducted between August 2020 and July 2021 in a population of 250 chronic pain sufferers who had experience with psychedelics, either in microdoses (small sub-hallucinogenic doses), macrodoses (hallucinogenic doses), or both. Macrodoses, while less often used for analgesic purposes than microdoses, were reported to induce a higher level of pain relief than both microdoses and conventional pain medications (including opioids and cannabis). Although the effects were weaker and potentially more prone to expectation bias than with macrodoses, our results also suggested some benefits of psychedelics in microdoses for pain management. The reported analgesic effect appeared unrelated to mood improvements associated with psychedelic use, or the advocacy of psychedelic use. Taken together, our findings indicate interesting potential analgesic applications for psychedelics that warrant further clinical research.
Keywords: Survey, psychedelics, chronic pain, self-medication, microdosing
Introduction
Worldwide, the burden caused by chronic pain is escalating. In 2016, an estimated 50 million adults in the United States were living with chronic non-cancer pain, 1 many of whom were prescribed opioid medications. However, when it comes to chronic pain, opioids’ harms (including addiction and overdose) often outweigh their benefits, 2 and their over-prescription has engendered a nationwide opioid crisis. 3 There is now an increasing interest in using novel analgesics to circumvent the harmful side effects of conventional first-line pain medication, such as the addictiveness of opioids or the chronic gastrointestinal and renal harm of non-steroidal anti-inflammatory drugs (NSAIDs). 4 For example, ketamine, an antagonist of the N-methyl-D-aspartate receptor, commonly used as an analgesic in emergency medicine, as an adjuvant drug in the perioperative setting and as a third-line adjuvant drug for opioid-resistant pain in palliative care and for intractable chronic non-cancer pain, also has an established use in neuropathic pain relief at low doses. 5 However, repeated use of ketamine is also associated with adverse effects, such as addiction, amnesia, high blood pressure, bladder cystitis or liver injury.6,7
Interestingly, ketamine shares some of its effects (e.g. altered awareness of self and surroundings, changed in perception of time and meaning) 8 and mechanisms of action (notably, glutamatergic-mediated neuroplasticity and inhibition of pro-inflammatory cytokines) 9 with a class of compounds with a lower harmful profile and considered from a physiological standpoint as one of the safest known classes of CNS drugs: the ‘classic’ serotonergic hallucinogens (psychedelics). These substances, which include among other lysergic acid diethylamide (LSD) and psilocybin, exert their consciousness altering effects primarily by agonism of the serotonin 2A receptors. 10 While recent clinical research has largely focused on their therapeutic potential for the treatment of depression, addiction and end-of-life existential distress,11,12 psychedelic compounds have also shown encouraging analgesic potential, particularly for cancer pain and cluster headache.13,14 Among their most relevant properties, psychedelics may exert analgesic effects by (1) reducing nociceptive sensory input through their interaction with descending inhibitory serotonergic pathways from the raphe nucleus, 15 (2) reducing inflammation through the inhibition of TNF-α signalling, 16 (3) enhancing neuroplasticity through activation of glutamatergic pyramidal neurons 17 and (4) facilitating affective regulation and emotional processing through modulation of the amygdala.18,19
Although no rigorously controlled clinical research has been conducted investigating the efficacy of psychedelic analgesia in patients with chronic pain, a recent double-blind study compared the effects of three single sub-hallucinogenic doses of LSD (5, 10 and 20 μg) to that of a placebo on pain perception and tolerance in healthy volunteers using a Cold Pressor Test. 20 This well-established test has been widely adopted as a model for acute nociceptive pain and is commonly used as a surrogate of clinical efficacy for opioids. 21 Notably, at the highest dose tested, LSD significantly increased pain tolerance and decreased painfulness as well as unpleasantness, without impairing day-to-day functioning.
Despite encouraging evidence, the extent to which psychedelics can exert beneficial effects on chronic pain and whether these effects are primarily mediated by their impact on mood is poorly understood. In the present study, we report the results from a detailed survey of individuals suffering from chronic pain and who have had some experience with psychedelics (whether to relieve pain or not). The intensity and characteristics of the subjective effects induced by psychedelics vary considerably with each psychedelics’ dose-range and with individuals’ own sensitivity.22,23 We therefore examined separately changes in pain attributed to doses of psychedelic inducing a significant alteration to normal consciousness level (‘macrodoses’) and doses that do not impair a person’s ‘normal’ functioning (‘microdoses’). We also compared the analgesic effects reported with these two dosage levels to that of more traditional pain management options.
Methods
Design
Participants were recruited online via social media and the Beckley Foundation Web site between August 2020 and July 2021. Eligible respondents were adult (over 18 years old) chronic pain sufferers who had had at least one experience with psychedelics. Ethical approval was received from the Ethics Review Committee of Psychology and Neuroscience (ERCPN-226_101_08_2020) at Maastricht University, The Netherlands. Qualtrics was used as the platform to create the survey.
Questionnaire
Demographic information
Demographic details included age group, gender and employment/work status.
Psychedelic substance use history
Respondents were asked whether they had experience with psychedelic substances in the past, which compound they had the most experience with (LSD/1p-LSD, psilocybin-containing truffles or mushrooms, DMT, Ayahuasca, 5-MeO-DMT, Mescaline or other) and what dosing best typified their use: ‘Small doses/microdoses only (less than 1/5 of a full dose)’, ‘Small doses/microdoses mostly’, ‘Mixed use of various doses, from small to full doses’, ‘Full doses (hallucinogenic) mostly’, ‘Full doses only’. They were also asked about the frequency of their use of full hallucinogenic doses, and microdoses and how long they had been using psychedelics for.
Four items, developed by Haijen et al. 2018, 24 were used to assess the individual’s relationship with psychedelic drugs. Respondents had to rate how strongly they agreed with each of the following statements: ‘I am an active advocate of psychedelic drug use’, ‘I am an active advocate of the therapeutic use of psychedelics’, ‘I have an advanced knowledge about psychedelics’ and ‘I am a highly experienced psychedelic drug user’.
Pain conditions evaluation
Participants were asked to specify the nature of the pain condition(s) they had been or were currently suffering from and if they had received a medical diagnosis (choosing from: Musculoskeletal, Inflammatory, Neuropathic, Headache and orofacial, Pain caused by cancer, Visceral or Other type of pain). They were also asked to rate the severity of the pain induced by this condition on a scale of 0–10 (0: no pain, 10: extreme pain), and how frequently they were experiencing pain due to this condition (All the time; On a daily basis; More than once a week; Less than once a week).
Perceived effectiveness of conventional medication
Respondents were asked to select from a list which conventional pain medication type they used most often (over-the-counter pain relievers, opioids, antidepressants, anticonvulsants, cannabis or other), how frequently and how much pain relief they experienced from it (0–10 scale).
Perceived effectiveness of psychedelics
In order to tease apart the effects of macrodoses to that of microdoses, respondents were asked to separately report their experiences with both types of dosages for all subsequent questions. Because some respondents used both macrodoses and microdoses of psychedelics, there is an overlap between the microdosing and macrodosing groups.
Change in pain perception per pain condition
Respondents were asked if they had ever noticed a change in pain (an increase or a decrease) in any of the conditions they reported, during, or after taking a psychedelic. If respondents reported having experienced a change, they were asked to report in which direction (improvement or worsening), for which condition(s), with which compound and to what extent (0–10 scale; 0: No pain reduction – 10: complete relief).
Characterisation of pain relief
The type of pain relief achieved by the psychedelic the respondent found most effective was rated in the following domains: pain intensity, pain acceptance, pain interference with daily activities and pain-induced emotional distress, using a 0–10 scale (0: No Change – 10: Strong improvement). They were also asked about the duration of pain relief.
Comparison between perceived benefits and side effects of psychedelics and conventional pain medication
Respondents were asked to compare the level of pain reduction achieved with their most effective psychedelic compound to that of their most effective conventional pain medication (including cannabis), and to compare their undesired effects (constipation, nausea, sedation/drowsiness, difficulty focussing, memory impairment, indigestion/stomach problems, anxiety). Psychoactive effects were not listed as side effects as, to most users, these were the main intended effects, and it is unclear to what extent these effects may mediate an analgesic effect.
Psychoactive effects
To gain a better insight into the relationship between psychoactive effects and analgesia, respondents were asked to describe the effects experienced with the psychedelic compound associated with the most pain relief, rating the effects as ‘Not noticeable’, ‘Barely noticeable’, ‘Distinctly noticeable but only by me’ or ‘Very distinctly noticeable by me and others’.
Respondents were also asked about other effects they typically experienced with this psychedelic at this dose, along with pain reduction: changes in mood, vitality, anxiety, attention, ability to perform everyday tasks, ability to interact with others, mindfulness, life satisfaction and body awareness.
Statistical analysis
Data was analysed in SPSS (version 28 0.1.0). Respondents who did not give their consent, were not 18 year or older, did not complete the questionnaire or had never suffered from chronic pain, were not included. Frequencies were calculated for demographic traits, use of psychedelics, experience using psychedelics for pain relief, use of conventional pain relief medication and history of pain-causing conditions. Tests of normality were performed using the Kolmogorov–Smirnov and Shapiro–Wilk tests. Pain relief scores for conventional medications were normally distributed. A multivariate independent measures ANOVA was conducted to compare the magnitude of perceived pain relief, severity of undesirable effects and satisfaction with pain relief between each type of pain medication used. Post-hoc independent sample t-tests were used to compare the different types of conventional medications. None of the variables for psychedelics satisfied the normality criteria, and therefore, non-parametric tests were used for subsequent statistical analysis. Related-samples Friedman’s two-way analysis of variance was used to assess the presence of a treatment effect on pain relief, and Wilcoxon signed-rank pairwise comparisons, Bonferroni corrected, were used for post-hoc comparisons of perceived pain relief between psychedelics and conventional pain medication.
SPSS’s Automatic Linear Modelling (LINEAR) was performed to evaluate the contributions of several factors to reported pain relief scores. The first model assessed the impact of perceived changes in pain characteristics on the overall perceived pain relief, the second model assessed the impact of the psychoactive and psychological effects of psychedelics and the third model assessed the impact of psychedelics advocacy and past experience. 25 Separate models were performed for macrodoses and microdoses. All predictors were included in the models, and resulting coefficients and their associated p-values were reported.
Results
Demographics
Out of 976 respondents, 250 completed the survey and met the inclusion criteria. There were 129 females and 117 males (4 preferred not to say), with the following age distribution: 18–30, n = 60; 31–40, n = 84; 41–50, n = 41; 51–60, n = 36 and 61–70, n = 29.
Psychedelics use
Overall, the most frequently used psychedelic for macrodosing and microdosing was psilocybin, followed by LSD (Psilocybin: N microdose use=51, N macrodose use=25, N mixed use =62; LSD: N microdose use=26, N macrodose use=28, N mixed use=40). Other substances were only marginally represented in our sample (DMT = 4, Ayahuasca = 5, Mescaline = 3).
Self-reported pain conditions
Respondents often reported suffering from more than one pain-inducing condition. The type of conditions most represented in our sample (i.e. with N > 20) is presented in Table 1, along with their typical prevalence in the general population. The values in bold indicate the conditions that are more represented in our respondent sample than in the general population.
Table 1.
Prevalence of pain-inducing conditions in survey respondents and in the general population.
| N | % Respondents sample | % Prevalence in general population | ||
|---|---|---|---|---|
| Muskuloskeletal | Back pain | 144 | 57.6 | 53 a |
| Bone pain | 46 | 18.4 | N/F | |
| Joint pain | 74 | 29.6 | 46 a | |
| Muscle pain | 91 | 36.4 | N/F | |
| Tendon and ligament pain | 73 | 29.2 | N/F | |
| Arthritis | 70 | 28 | 8–16 a | |
| Headache and orofacial | Cluster headache | 26 | 10.4 | 0.12 a |
| Migraine | 65 | 26 | 14.3 a | |
| Tension headache | 49 | 19.6 | 20.8 b | |
| Orofacial pain | 36 | 14.4 | 26 c | |
| Neuropathic | Complex regional pain syndrome | 29 | 11.6 | 1.2 d |
| Pelvic pain | 21 | 16.3 | 14.2 b | |
| Sciatica | 65 | 26 | 13–40 a | |
| Fibromyalgia | 48 | 19.2 | 5.4 a | |
| Visceral | Irritable bowel syndrome | 26 | 10.4 | 10–20 a |
| Menstrual pain | 25 | 19.4 | 16–91 e |
Perception of pain relief effectiveness with conventional medication
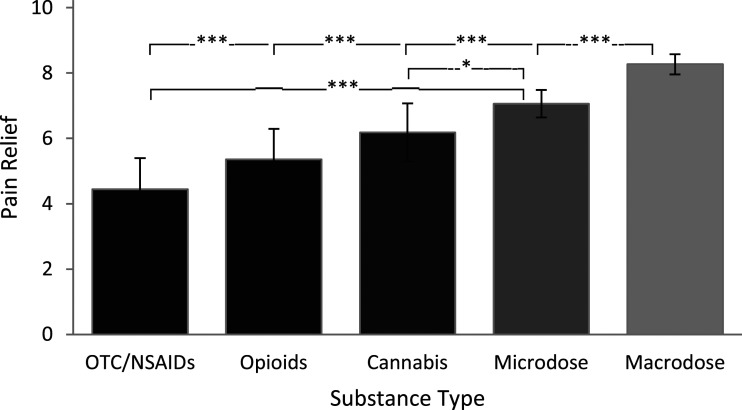
The frequency and perceived pain relief associated with conventional medications used were over-the-counter (OTC) medications/NSAIDs (N = 57, 22.8% of respondents; mean pain relief = 4.44, standard error (SE) = 0.28), opioids (N = 53, 21.1%; mean pain relief = 5.36, SE = 0.31), cannabis (N = 49, 19.6%; mean pain relief = 5.69, SE = 0.24), anticonvulsants (N = 11, 4.4%; mean pain relief = 4.91, SE = 0.64), antidepressants (N = 10, 4.0%; mean pain relief = 5.30, SE = 0.84), triptans/migraine medication (N = 8, 3.2%; mean pain relief = 6.40, SE = 0.51) and ‘other’ (N = 15, 6%; mean pain relief = 6.00, SE = 0.84). Some respondents reported not taking any pain medication (N = 50, 20%).
Significant main effects of conventional treatment types were found for pain relief (F (7, 187) = 3.173, p = 0.003), on severity of side effects (F (7, 170) = 4.82, p ≤ 0.001) and satisfaction with pain relief (F (7, 170 = 3.57, p = 0.001). Post-hoc tests indicated that respondents who used cannabis reported significantly greater pain relief than those using OTC/NSAIDs (p < 0.001) (Figure 2). Those who used opioids reported significantly greater severity of side effects compared with those who used OTC/NSAIDs (p ≤ 0.001). Respondents who used cannabis reported significantly greater satisfaction with pain relief than those who used OTC/NSAIDs (p = 0.001) and than those who used opioids (p = 0.031).
Figure 2.
Comparison between perceived pain relief (0 = no pain relief, 10 = complete pain relief) achieved using microdosing and macrodosing, and the three most frequently reported conventional medications: over-the-counter (OTC)/NSAIDs, opioids and cannabis. Statistically significant differences between groups are denoted by ***(<0.001), **(<0.01) and *(<0.05). Error bars indicate standard error.
Perception of pain relief effectiveness with psychedelics
Microdosing
Of the 187 respondents who reported the use of microdoses of psychedelics (N (microdoses use mostly)=81 or N (mixed use)=106), 67.9% (N = 127) associated it with a reduction in pain, while 5.3% (N = 10) associated it with an increase in pain. Of those using microdoses, 49.2% (N = 92) reported doing it specifically for pain management.
Macrodosing
Of the 163 respondents who reported the use of macrodoses of psychedelics (macrodoses use mostly N = 57 or mixed use N = 106), 72.4% (N = 118) associated it with a reduction in pain, while 14.1% (N = 23) associated it with an increase in pain. Of those using macrodoses, 33.7% (N = 55) reported doing it specifically for pain management.
Comparison of perceived pain relief between psychedelics and conventional pain medication
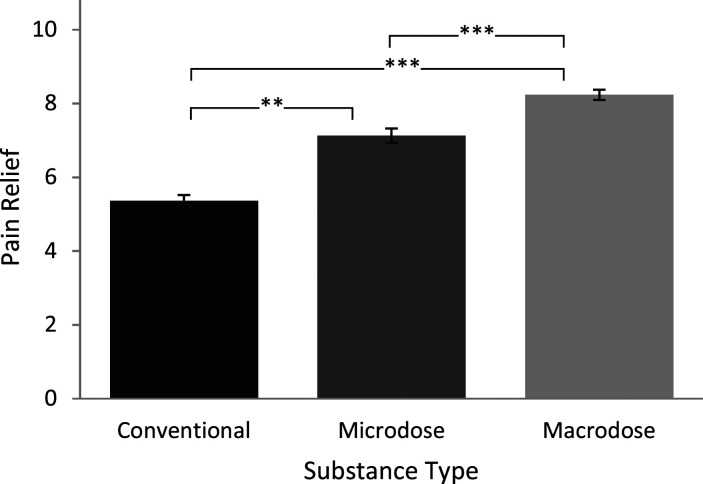
A non-parametric Friedman test of differences among repeated pain relief measures for conventional pain medication, microdoses and macrodoses, indicated a significant effect of treatment on pain relief (Fr (2, 81) = 59.34 p < 0.001). Pairwise comparisons indicated that both macrodoses (mean pain relief = 8.23; p < 0.001) and microdoses (mean pain relief = 7.12; p = 0.004) were perceived as achieving higher pain relief than conventional medications (mean pain relief = 5.36), and pain relief achieved with macrodoses was statistically significantly more pronounced than that achieved with microdoses (p < 0.001) (Figure 1).
Figure 1.
Comparison of ratings of perceived pain relief (0 = no pain relief, 10 = complete pain relief) between conventional medication and psychedelics in either microdoses or macrodoses. Statistically significant differences between groups are denoted by ***(<0.001), **(<0.01) and *(<0.05). Error bars indicate standard error.
We next looked separately at how the three most commonly reported conventional medications (OTC/NSAIDs, opioids and cannabis) compared with microdoses or macrodoses of psychedelics, using non-paramtric pairwise comparisons. Pain relief experienced with macrodosing was statistically significantly superior to that achieved with OTC/NSAIDs (N = 35, p < 0.001), opioids (N = 38, p < 0.001) and cannabis (N = 31, p < 0.001). Pain relief experienced with microdoses was only superior to that experienced with OTC/NSAIDs (N = 34, p ≤ 0.001) and cannabis (N = 23, p = 0.042), but not with opioids (N = 34, p = 0.303) (Figure 2).
Comparing different types of psychedelics
The two most frequently used compounds, psilocybin and LSD, were selected to examine the effect of compound type on perceived pain relief. There was no statistically significant difference between the pain relief experienced with psilocybin and LSD, either taken in macrodoses (p = 0.990) or microdoses (p = 0.676).
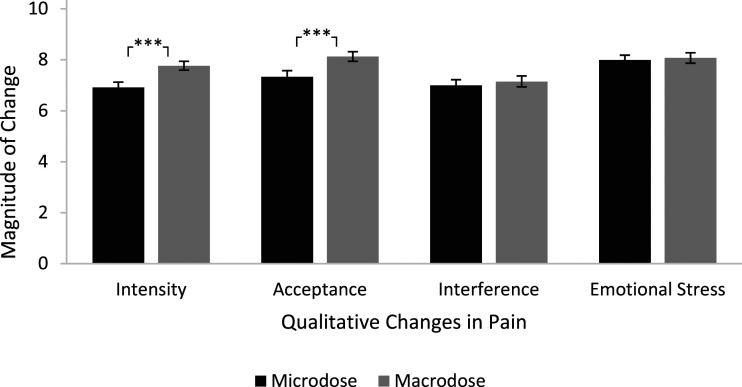
Qualitative changes in pain
Macrodosing and microdosing were both associated with perceived improvements in pain intensity, acceptance of pain, interference caused by pain and emotional stress (Figure 3). Compared with microdosing, macrodosing provided statistically significantly higher perceived reduction in pain intensity (Z = 4.56, N = 107, p < 0.001) and acceptance of pain (Z = 4.58, N = 105, p ≤ 0.001). No other statistically significant differences were observed between microdosing and macrodosing.
Figure 3.
Comparison between qualitative changes in pain following microdosing and macrodosing. Significant differences between groups are denoted by ***(<0.001), **(<0.01) and *(<0.05). Error bars indicate standard error.
To assess which of these qualitative aspects of pain most contributed to the overall experience of pain relief, pain relief scores for macrodoses (N = 118) and microdoses (N = 127) were added as a target in a linear model (LINEAR) with perceived changes in pain intensity, pain acceptance, pain interference with daily activities and emotional stress caused by pain added as predictors. For microdoses and macrodoses, two factors significantly contributed to variance in pain relief: pain intensity (macrodoses: coefficient = 0.314, p < 0.001, microdoses: coefficient = 0.505, p < 0.001) and pain interference with daily life (macrodoses: coefficient = 0.262, p < 0.001, microdoses: coefficient = 0.346, p < 0.001).
Psychological factors
Given the strong association between chronic pain and mood disorders, and the potential impact of psychedelics on mood, we next examined the relationship between pain relief and other subjective effects associated with the use of macrodoses or microdoses of psychedelics (changes in Mood, Vitality, Anxiety, Mindfulness, Life satisfaction and Body awareness). Pain relief scores were used as target in LINEAR, and the subjective effects were added as predictors. For macrodoses, only Life Satisfaction significantly contributed to the resulting model (coefficient=0.383, p = 0.015). For microdoses, none of the factors significantly contributed to the model (Table 2). These results suggest that pain relief achieved with microdoses or macrodoses does not appear to be strongly mediated by psychological factors such as mood, mindfulness or body awareness, but is associated with higher satisfaction with life.
Table 2.
Coefficients and associated p-values resulting from the linear modelling on pain reliefs’ scores achieved with microdoses and with macrodoses of psychedelics.
| Microdoses | Macrodoses | |||
|---|---|---|---|---|
| Coefficient | p-value | Coefficient | p-value | |
| Mood | −0.202 | 0.378 | −0.087 | 0.668 |
| Vitality | 0.023 | 0.906 | 0.191 | 0.166 |
| Anxiety | 0.183 | 0.130 | −0.006 | 0.923 |
| Satisfaction with life | 0.201 | 0.400 | 0.383 | 0.015* |
| Mindfulness | 0.033 | 0.891 | 0.057 | 0.654 |
| Body awareness | 0.136 | 0.481 | 0.072 | 0.519 |
*denotes p value <0.05.
Effects duration
Macrodosing provided statistically significantly longer duration of perceived pain relief than microdosing (Z = 4.697, N = 107, p < 0.001). One-third of those reporting pain reduction with macrodosing still perceived benefits over three days after the dose (33.7%), while only one-fifth (21.4%) of people still experienced benefits of microdoses three days after the dose.
Side effects
Given the intense nature of the psychedelic experience, it is difficult to dissociate side effects from desirable effects with macrodoses, and we therefore only compared side effects experienced with conventional medication with that experienced with microdoses. In all the dimensions assessed, microdoses produced less side effects than conventional medication (One-sample Kolmogorov-Smirnov Normal tests, all tests had p-values <0.001), namely, constipation, nausea, sedation, difficulty focussing, memory impairment, indigestion and anxiety.
Comparing intentional versus non-intentional use of psychedelics for pain management
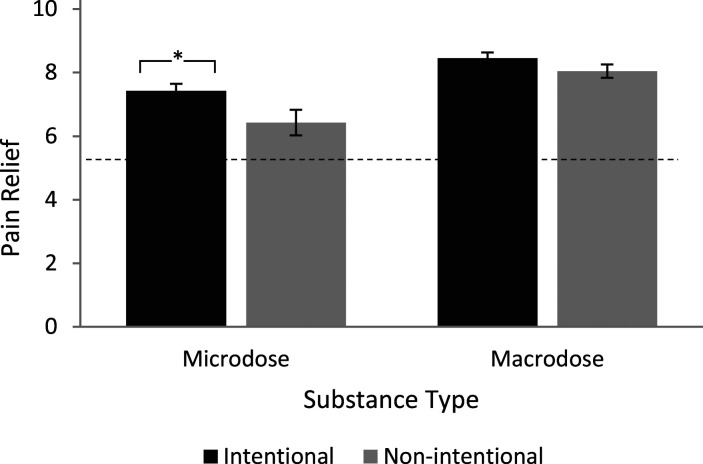
To assess the impact of intentions and expectations on treatment outcome, we compared the benefits experienced between people who used psychedelics for the specific purpose of managing pain, and those who incidentally experienced benefits following psychedelic use.
Microdoses (49.2%) were more frequently reported as having been used for pain management than macrodoses (33.7%). There was no statistically significant difference in the perceived pain relief due to macrodoses between those who used them to manage pain and those who did not (Independent samples Mann–Whitney U test, N = 163, p = 0.263). However, those who microdosed with the purpose of pain management reported statistically significantly higher pain relief than those who did not (Z = 2.12, N = 140, p = 0.034; see Figure 4). When focussing on the group of people who reported microdosing-induced benefits despite not microdosing with pain management in mind, the level of reported pain relief was not significantly different from pain relief achieved using conventional medication (Z = 1.61, N = 32, p = 0.107).
Figure 4.
Comparison of ratings of perceived pain relief (0 = no pain relief, 10 = complete pain relief) between respondents who deliberately used psychedelics microdosing or macrodosing for pain relief and those who did not. Significant differences between groups are denoted by ***(<0.001), **(<0.01) and *(<0.05). Error bars indicate standard error.
Influence of psychedelics advocacy and prior experience with psychedelics
A large proportion of respondents were strong psychedelics advocates (Table 3). Comparatively, the prior experience was more equally distributed between those reporting being highly experienced and those who did not.
Table 3.
Frequency table of psychedelics advocacy and prior experience.
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
|---|---|---|---|---|---|
| 1. ‘I am an active advocate of psychedelic substance use’ | 9 | 6 | 37 | 73 | 123 |
| 1. ‘I am an active advocate of the therapeutic use of psychedelics’ | 9 | 2 | 15 | 55 | 165 |
| 1. ‘I have an advanced knowledge about psychedelics’ | 8 | 22 | 65 | 96 | 58 |
| 1. ‘I am a highly experienced psychedelic substance user’ | 15 | 42 | 65 | 72 | 54 |
To evaluate the impact of psychedelics advocacy and prior experience on reported pain relief, we included the ratings attributed to each of the statements as predictors in an Automatic Linear Model, with pain relief scores entered as target. For pain relief reported from macrodoses, none of the statements achieved significant scores, suggesting that pain relief reports for macrodoses were largely independent of advocacy or prior experience with psychedelics. For microdoses, prior experience with psychedelics (i.e. adhering to the statement: ‘I am a highly experienced psychedelic substance user’) was negatively associated with pain relief (coefficient = −0.798, p = 0.045), suggesting that people who have more experience with psychedelics perceive less pain relief from microdosing.
Discussion
Although a few studies and case reports have shown potential benefits of psychedelics in cancer pain, phantom limb pain and cluster headache, 15 their use for the management of chronic pain has received little clinical attention to date. The aim of this online survey was to shed some light on the perceived analgesic potential of these compounds, whether used in full hallucinogenic doses, or in smaller, sub-hallucinogenic doses, by collecting data from a population of chronic pain sufferers and psychedelics users. Our results indicate that pain relief experienced with these compounds was perceived as superior to that experienced with conventional pain medications.
Effect of psychedelics on pain
A majority of respondents (over two-thirds) reported having experienced some pain relief as a result of their psychedelics use. The use of macrodoses of psychedelics was perceived as producing more effective pain relief than conventional medication (including cannabis and opioids) and microdoses. These results are consistent with those from a survey conducted in people who self-medicate with psychedelics to manage mental and/or physical health conditions. 26 In this study, self-reported effectiveness of microdoses and macrodoses of psychedelics were found to be significantly higher compared with that of conventional treatments, with macrodoses achieving better results than microdoses.
Our findings are also consistent with results from a recent study conducted as part of an upcoming chronic pain trial, in which 11 individuals who reported self-medicating with psychedelic drugs took part in a one-hour semi-structured discussion. 27 In keeping with our results, reported pain scores improved substantially during and after psychedelic experiences across a range of psychedelic substances and doses.
Microdosing versus macrodosing
A microdose has been defined as approximately one-tenth to one-twentieth of a recreational dose, varying within and between substances. However, given the important inter-individual variability in dose-response to psychedelics, 22 we decided to distinguish microdoses and macrodoses in terms of their subjective effects rather than a specific dose-range. A microdose was therefore defined as a dose on which a normal state of consciousness is maintained, while the term ‘macrodose’, corresponded to doses inducing significant alterations to the state of consciousness, with the occurrence of effects characteristics of the psychedelic experience such as complex and elementary imagery, audio-visual synaesthesia and changed meaning of perception.
Are the effects on pain mediated by mood?
Depression and chronic pain frequently coexist, with up to 60% of chronic pain patients also presenting with depression. 28 The relationship between the two conditions is bidirectional, as having either disorder increases the risk of developing the other. 29 A growing amount of evidence indicates the high therapeutic potential of psychedelic-assisted therapy for treating mood disorders such as depression and anxiety.30–32 Although less rigorous evidence exists to support the therapeutic benefits associated with this practice, the use of microdoses of psychedelics to self-medicate for a mood disorder is also on the rise.26,33 A study conducted in healthy volunteers reported a significant enhancement of positive mood after 20 μg of LSD – a dose considered in the higher range of microdoses. 34 Regardless of dosages, psychedelic use, in general, has been associated with better mental health.33,35 It is therefore possible that the reported benefits of psychedelics on pain observed in our survey are a consequence of their positive impact on mood. Although both microdoses and macrodoses were associated with self-reported moderate to strong improvements in wellbeing unrelated to pain management, our regression analyses suggested that, whether for macrodoses or microdoses, the direct effect of psychedelics on mood does not appear to mediate perceived pain relief. Rather, macrodoses-mediated pain relief was associated with improvements in life satisfaction, which is perhaps not surprising given the established connection between chronic pain and poor life satisfaction.36,37
Expectancy effect
Patients’ expectations about the therapeutic benefit of a treatment represent a major determinant of the placebo response.38–40 Not only have psychedelics been shown to enhance suggestibility, 41 their perceived benefits have also been associated with positive expectancies, particularly in the case of microdosing.42,43 To evaluate the role played by expectancy in pain relief reports, we asked participants whether or not they had been using psychedelics with the specific intention of managing pain. In the group of respondents who did not use psychedelics for pain management, macrodoses of psychedelics were still perceived as exerting a significant analgesic effect, superior to that of conventional medication, while the analgesic effect of microdoses was reported as similar to that of conventional medication.
Although this analysis confirms that expectation plays a significant role in the analgesic effect of psychedelic microdoses, it also shows that analgesic effects similar to those of potentially more harmful medications can be achieved with small doses of compounds that have a remarkably high safety profile 44 and low toxicity. 45
It should also be noted that our approach of splitting participants based on their intention to treat pain might be overly conservative. Indeed, within the group of people microdosing for the purpose of managing pain, positive expectations are also likely to be driven by real previously experienced benefits.
Respondent sample
The representation of pain conditions in our respondent sample largely matches that of the general population, with the exception of Cluster Headache, Complex Regional Pain Syndrome and Fibromyalgia, which seemed to be more prevalent in our sample of psychedelics users (Table 1). Although we cannot draw any rigorous conclusion from this observation, this could indicate that people suffering from these conditions may experience more benefits from psychedelics use.
Conventional pain medications reported by respondents also represented the most widespread pain medications (OTC, opioids, anticonvulsants and antidepressants). In keeping with results from a study conducted in a large sample of microdosers (N = 4050), our respondents sample included a relatively high percentage of cannabis users. 33 In addition, a relatively large proportion of respondents reported cannabis as their most effective pain management option (19.5%), which is also in keeping with previous reports.46,47 For instance, in the United Kingdom, three-quarters of dispensary members reported that medical cannabis were more effective than their prescribed medications. 48 Noteworthily, the simultaneous use of cannabis and classic psychedelics could be associated with an intensification of the psychedelic experience. 49 Although it would be tempting to hypothesise on a possible intensification of the analgesic effects of cannabis when combined with psychedelics, more research is needed to establish a potential interaction between the effects of these substances.
In congruence with previous surveys conducted in psychedelics users, the two most commonly used psychedelic compounds were psilocybin (in the form of mushrooms or truffles, whose used is legally tolerated in several countries), followed by LSD (which is still largely prohibited worldwide and less accessible). Both belong to the same class of serotonergic psychedelics, exerting their psychoactive effect largely via agonism of the serotonin 2A receptor.
Our survey targeting psychedelics users, a majority of respondents were biased towards perceiving psychedelics and their effects favourably. However, psychedelics advocacy and prior experience with psychedelics did not appear to mediate pain relief scores. If anything, prior experience was negatively associated with pain relief achieved with microdoses.
Survey data: opportunity and limitations
The use of psychedelics is becoming more widespread and is now expanding beyond purely recreational use towards self-medication for a range of mental and physical health conditions. 26 Although more clinical research is needed to rigorously assess the safety and efficacy of psychedelics for specific conditions, surveying this pool of existing users can bring some insight into the validity of users’ claims and guide the development of future clinical research.
However, these types of surveys are not without limitations. The data they provide are entirely subjective, highly vulnerable to bias and preclude causal inference. Reports from participants are based on recollection of past experiences and are likely to suffer from a degree of inaccuracy. In addition, the population assessed was highly heterogeneous and featured a wide range of chronic pain conditions, whose underlying pathophysiology may vary considerably. Although the present results suggest an analgesic potential of psychedelics, more work is needed to evaluate which chronic pain conditions are likely to benefit most. Future research should also attempt to examine what are the most effective and clinically practical dose-range and frequency of use of these types of treatments and whether their mind-altering effect should be considered as a side effect or as a mediator of therapeutic benefits. Future work should also attempt to assess in more detail any potential adverse events associated with psychedelics use in a population of chronic pain sufferers.
Other limitations
Set and setting are well known to play a significant part in the quality of the psychedelic experience and its long term effects.50,51 However, in this survey, we did not collect any data regarding the intention and context in which respondents were using psychedelics. Future research should attempt to elucidate whether these factors also play a role in the putative analgesic effect of psychedelics.
In macrodoses, psychedelics produce such intense effects that it is difficult to compare their ‘side effects’ to that of conventional medication. Although we were mostly interested in the post-acute effects of macrodoses on pain, unfortunately, the question relating to side effects with macrodoses was not framed in a way that allow us to dissociate between the acute experience and the post-acute effects, and we therefore decided to only compare side effects between interventions that do not significantly affect the state of consciousness.
Conclusion
Data collected through this survey produced further insights into the analgesic potential of psychedelics. Hallucinogenic doses, while less often used for analgesic purposes than microdoses, were reported to induce a higher level of pain relief than conventional pain medications (including opioids and cannabis), with perceived benefits lasting for more than a day. This self-reported pain relief appeared unrelated to whether or not the intended use was pain management, prior experience with psychedelics or level of advocacy. Future work should look more closely at the analgesic effect experienced in the days following a psychedelic macrodose, and its relation to other factors, whether physiological, such as neuroplasticity and inflammatory markers or psychological, such as resilience, acceptance and coping strategies.
Although the effects were weaker and potentially more prone to expectation bias, our results also confirm some potential benefits of microdoses of psychedelics for pain management. Low doses of psychedelics do not significantly impact daily functioning 34 and therefore may provide a more practical and accessible way to use these compounds as analgesics. Future work should attempt to identify an optimal trade-off between efficacy and psychoactive effects, as well as elucidating the underlying mechanisms of actions, and identifying which pain condition may benefit most from this class of compounds. Taken together, our results indicate interesting potential analgesic applications for psychedelics and warrant further clinical research.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Valerie Bonnelle https://orcid.org/0000-0002-4673-0549
Mauro Cavarra https://orcid.org/0000-0002-5216-3157
References
- 1.Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep 2018; 67(36): 1001–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prescription Opioid Data | Drug Overdose | CDC Injury Center [Internet]. https://www.cdc.gov/drugoverdose/deaths/prescription/index.html (2021, accessed 20 December 2021).
- 3.DeWeerdt S. Tracing the US opioid crisis to its roots. Nature (Internet) 2019; 573(7773): S10–S12. (cited 2021 Dec 20). Available from: https://www.nature.com/articles/d41586-019-02686-2 [DOI] [PubMed] [Google Scholar]
- 4.Yekkirala AS, Roberson DP, Bean BP, et al. Breaking barriers to novel analgesic drug development. Nat Rev Drug Discov (Internet) 2017;16(8):545–564 (cited 2021 Dec 20). Available from: https://www.nature.com/articles/nrd.2017.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bell RF, Kalso EA. Ketamine for pain management. Pain Rep (Internet) 2018; 3(5): e674 (cited 2021 Dec 20). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6181464/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niesters M, Martini C, Dahan A, et al. Ketamine for chronic pain: risks and benefits. Br J Clin Pharmacol (Internet) 2014; 77(2): 357–367 (cited 2021 Dec 20). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4014022/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orhurhu VJ, Vashisht R, Claus LE, et al. Ketamine toxicity. StatPearls Publishing; (Internet). Available from: https://www.ncbi.nlm.nih.gov/books/NBK541087/ (2021, 17 December 2021). [PubMed] [Google Scholar]
- 8.Bowdle AT, Radant AD, Cowley DS, et al. Psychedelic effects of ketamine in healthy volunteers : relationship to steady-state plasma concentrations. Anesthesiology (Internet) 1998; 88(1): 82–88. DOI: 10.1097/00000542-199801000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Kadriu B, Greenwald M, Henter ID, et al. Ketamine and serotonergic psychedelics: common mechanisms underlying the effects of rapid-acting antidepressants. Int J Neuropsychopharmacol (Internet) 2020; 24(1): 8–21. (cited 2022 May 11). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7816692/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nichols DE. Psychedelics. Barker EL. (ed) Pharmacol Rev (Internet) 2016; 68(2): 264–355. (cited 2021 Dec 20). Available from: https://pharmrev.aspetjournals.org/content/68/2/264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson MW, Hendricks PS, Barrett FS, et al. Classic psychedelics: an integrative review of epidemiology, therapeutics, mystical experience, and brain network function. Pharmacol Ther 2019; 197: 83–102. [DOI] [PubMed] [Google Scholar]
- 12.Muttoni S, Ardissino M, John C, et al. Classical psychedelics for the treatment of depression and anxiety: a systematic review. J Affect Disord (Internet) 2019; 258: 11–24. (cited 2021 Dec 20). Available from: https://www.sciencedirect.com/science/article/pii/S0165032719309127 [DOI] [PubMed] [Google Scholar]
- 13.Elman I, Pustilnik A, Borsook D. Beating pain with psychedelics: matter over mind? Neurosci Biobehav Rev 2021; 21: S014900553–S014976344. [DOI] [PubMed] [Google Scholar]
- 14.Whelan A, Johnson MI. Lysergic acid diethylamide and psilocybin for the management of patients with persistent pain: a potential role? Pain Manag 2018; 8(3): 217–229. [DOI] [PubMed] [Google Scholar]
- 15.Castellanos JP, Woolley C, Bruno KA, et al. Chronic pain and psychedelics: a review and proposed mechanism of action. Reg Anesth Pain Med (Internet) 2020; 45(7): 486–494. (cited 2021 Oct 5). Available from: https://rapm.bmj.com/content/45/7/486 [DOI] [PubMed] [Google Scholar]
- 16.Thompson C, Szabo A. Psychedelics as a novel approach to treating autoimmune conditions. Immunol Lett (Internet) 2020; 228: 45–54. (cited 2021 Dec 20). Available from: https://www.sciencedirect.com/science/article/pii/S0165247820303977 [DOI] [PubMed] [Google Scholar]
- 17.Ly C, Greb AC, Cameron LP, et al. Psychedelics promote structural and functional neural plasticity. Cell Rep (Internet) 2018; 23(11): 3170–3182. (cited 2021 Jan 19). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6082376/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barrett FS, Doss MK, Sepeda ND, et al. Emotions and brain function are altered up to one month after a single high dose of psilocybin. Sci Rep (Internet) 2020; 10(1): 2214. (cited 2021 Dec 20). Available from: https://www.nature.com/articles/s41598-020-59282-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kraehenmann R, Preller KH, Scheidegger M, et al. Psilocybin-Induced Decrease in amygdala reactivity correlates with enhanced positive mood in healthy volunteers. Biol Psychiatry 2015; 78(8): 572–581. [DOI] [PubMed] [Google Scholar]
- 20.Ramaekers JG, Hutten N, Mason NL, et al. A low dose of lysergic acid diethylamide decreases pain perception in healthy volunteers. J Psychopharmacol (Internet) 2020; 25: 0269881120940937. DOI: 10.1177/0269881120940937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Staahl C, Olesen AE, Andresen T, et al. Assessing analgesic actions of opioids by experimental pain models in healthy volunteers - an updated review. Br J Clin Pharmacol 2009; 68(2): 149–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Studerus E, Gamma A, Kometer M, et al. Prediction of psilocybin response in healthy volunteers. Plos One (Internet) 2012; 7(2): e30800. (cited 2022 May 12). Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0030800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sweeney GD. Variability in the human drug response. Thromb Res Suppl 1983; 4: 3–15. [DOI] [PubMed] [Google Scholar]
- 24.Haijen ECHM, Kaelen M, Roseman L, et al. Predicting responses to psychedelics: a prospective study. Front Pharmacol (Internet). 2018; 0. (cited 2021 Jul 15). Available from: https://www.frontiersin.org/articles/10.3389/fphar.2018.00897/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang H, Tzeng HY, Chou LS. The case for being automatic: introducing the automatic Linear Modeling (LINEAR) Procedure in SPSS Statistics. Bot Stud 2013; 39: 11. [Google Scholar]
- 26.Hutten NRPW, Mason NL, Dolder PC, et al. Self-rated effectiveness of microdosing with psychedelics for mental and physical health problems among microdosers. Front Psychiatry (Internet) 2019; 10: 672. (cited 2021 Oct 5). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6753862/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bornemann J, Close JB, Spriggs MJ, et al. Self-medication for chronic pain using classic psychedelics: a qualitative investigation to inform future research. Front Psychiatry 2021; 12: 735427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hooten WM. Chronic pain and mental health disorders: shared neural mechanisms, epidemiology, and treatment. Mayo Clin Proc 2016; 91(7): 955–970. [DOI] [PubMed] [Google Scholar]
- 29.Bondesson E, Larrosa Pardo F, Stigmar K, et al. Comorbidity between pain and mental illness - evidence of a bidirectional relationship. Eur J Pain 2018; 22(7): 1304–1311. [DOI] [PubMed] [Google Scholar]
- 30.Andersen KAA, Carhart-Harris R, Nutt DJ, et al. Therapeutic effects of classic serotonergic psychedelics: a systematic review of modern-era clinical studies. Acta Psychiatr Scand 2021; 143(2): 101–118. [DOI] [PubMed] [Google Scholar]
- 31.Carhart-Harris RL, Goodwin GM. The therapeutic potential of psychedelic drugs: past, present, and future. Neuropsychopharmacology 2017; 42(11): 2105–2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Gregorio D, Aguilar-Valles A, Preller KH, et al. Hallucinogens in mental health: preclinical and clinical studies on LSD, psilocybin, MDMA, and ketamine. J Neurosci 2021; 41(5): 891–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rootman JM, Kryskow P, Harvey K, et al. Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers. Sci Rep 2021; 11(1): 22479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hutten NRPW, Mason NL, Dolder PC, et al. Mood and cognition after administration of low LSD doses in healthy volunteers: A placebo controlled dose-effect finding study. Eur Neuropsychopharmacol 2020; 41: 81–91. [DOI] [PubMed] [Google Scholar]
- 35.Krebs TS, Johansen PØ. Psychedelics and mental health: a population study. Plos One (Internet) 2013; 8(8): e63972. (cited 2021 Dec 3). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3747247/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McNamee P, Mendolia S. The effect of chronic pain on life satisfaction: evidence from Australian data. Soc Sci Med 2014; 121: 65–73. [DOI] [PubMed] [Google Scholar]
- 37.Stålnacke BM. Life satisfaction in patients with chronic pain – relation to pain intensity, disability, and psychological factors. Neuropsychiatr Dis Treat (Internet) 2011; 7: 683–689. (cited 2021 Dec 13). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3225342/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frisaldi E, Shaibani A, Benedetti F. Why we should assess patients’ expectations in clinical trials. Pain Ther (Internet) 2017; 6(1): 107–110. (cited 2021 Dec 8). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447548/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kirsch I. Response expectancy and the placebo effect. Int Rev Neurobiol 2018; 138: 81–93. [DOI] [PubMed] [Google Scholar]
- 40.Sanders AE, Slade GD, Fillingim RB, et al. Effect of treatment expectation on placebo response and analgesic efficacy. JAMA Netw Open (Internet) 2020; 3(4): e202907. (cited 2021 Dec 8). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7163405/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carhart-Harris RL, Kaelen M, Whalley MG, et al. LSD enhances suggestibility in healthy volunteers. Psychopharmacology (Berl) 2015; 232(4): 785–794. [DOI] [PubMed] [Google Scholar]
- 42.Kaertner LS, Steinborn MB, Kettner H, et al. Positive expectations predict improved mental-health outcomes linked to psychedelic microdosing. Sci Rep (Internet) 2021; 11(1): 1941. (cited 2021 Oct 5). Available from: https://www.nature.com/articles/s41598-021-81446-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Szigeti B, Kartner L, Blemings A, et al. Self-blinding citizen science to explore psychedelic microdosing. Elife 2021; 10: e62878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nutt DJ, King LA, Phillips LD, et al. Independent scientific committee on drugs. Drug harms in the UK: a multicriteria decision analysis. Lancet 2010; 376(9752): 1558–1565. [DOI] [PubMed] [Google Scholar]
- 45.Calina D, Carvalho F, Oana Docea A. Chapter 43 - Toxicity of psychedelic drugs. In: Tsatsakis AM. (ed). Toxicological risk assessment and multi-system health impacts from exposure (Internet). Academic Press, 2021, pp. 545–556. (cited 2021 Dec 10). Available from: https://www.sciencedirect.com/science/article/pii/B9780323852159000222 [Google Scholar]
- 46.Piper BJ, Beals ML, Abess AT, et al. Chronic pain patients’ perspectives of medical cannabis. Pain (Internet) 2017; 158(7): 1373–1379. (cited 2022 May 12). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5845915/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bar-Lev Schleider L, Mechoulam R, Sikorin I, et al. Adherence, safety, and effectiveness of medical cannabis and epidemiological characteristics of the patient population: a prospective study. Front Med (Lausanne) (Internet) 2022; 9: 827849. (cited 2022 May 12). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8864967/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ware MA, Adams H, Guy GW, et al. The medicinal use of cannabis in the UK: results of a nationwide survey. Int J Clin Pract 2005; 59(3): 291–295. [DOI] [PubMed] [Google Scholar]
- 49.Kuc J, Kettner H, Rosas F, et al. Psychedelic experience dose-dependently modulated by cannabis: results of a prospective online survey. Psychopharmacology (Internet) 2021; 239: 1425–1440. DOI: 10.1007/s00213-021-05999-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kettner H, Rosas FE, Timmermann C, et al. Psychedelic communitas: intersubjective experience during psychedelic group sessions predicts enduring changes in psychological wellbeing and social connectedness. Front Pharmacol (Internet) 2021; 12: 623985. (cited 2022 May 11). Available from: https://www.frontiersin.org/article/10.3389/fphar.2021.623985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carhart-Harris RL, Roseman L, Haijen E, et al. Psychedelics and the essential importance of context. J Psychopharmacol 2018; 32(7): 725–731. [DOI] [PubMed] [Google Scholar]