Abstract
Antiplatelet therapy including aspirin and thienopyridine agents (such as clopidogrel, prasugrel and ticagrelor) are often used in patients with coronary disease. Pulmonary hemorrhage due to antiplatelet therapy although very rare, when excessive, is a life-threatening event. So far, there is lack of specific guidelines for the management of these patients. We report a case series of 5 patients receiving antiplatelet therapy who were admitted to the hospital due to pulmonary hemorrhage related to antiplatelet therapy. We also propose an algorithm on the management of these patients taking into consideration the balance between thrombotic and bleeding risk and the severity of the hemorrhage.
Keywords: Antiplatelet therapy, Pulmonary hemorrhage, Hemoptysis, Algorithm
Abbreviations: ENT, Otolaryngologist; LRTI, Lower respiratory tract infection; CT, Computerized tomography; BAL, Broncho-alveolar lavage; ADP, Thienopyridine adenosine diphosphate; COX-1, Cyclooxygenase-1
1. Introduction
Antiplatelet therapy including aspirin and/or thienopyridine agents (such as clopidogrel, prasugrel and ticagrelor) are often used in patients with coronary disease, while dual therapy, is the most common treatment used in patients undergone percutaneous coronary intervention [1]. Bleeding complications although minor in their great majority (such as easy bruising, petechia and ecchymosis), are still frequent, appearing in up to 32.4% [2]. The commonest major bleeding complication is gastrointestinal bleeding. Whereas pulmonary hemorrhage is very rare among people with no respiratory sequelae or diseases represents a life-threatening event being fatal in approximately 0.9% of cases [3].
The diagnosis of pulmonary hemorrhage in a patient receiving antiplatelets is often challenging and raises safety concerns [4]. Even when diagnosed, its management is often complex especially in patients who require antiplatelet therapy and in whom antiplatelet therapy should be reconsidered after the cessation of the hemorrhage. In such cases it is necessary not only to identify promptly the cause of the pulmonary hemorrhage and counteract it accordingly, but also to discover the critical balance between patients' risk of bleeding and thrombosis, especially for those with coronary stents, who require antiplatelet treatment.
Here we report a case series of 5 patients receiving antiplatelet therapy (either single or dual) who were admitted to the hospital due to pulmonary hemorrhage. We also suggest an algorithm on the management of these patients regarding the way antiplatelet therapy be ceased and readmitted when indicated.
2. Case 1
A 79-year-old male patient, current smoker (100pys), with a medical history of arterial hypertension, aortic aneurism and left carotid stenting performed 9 months ago, for which he received dual antiplatelet therapy with aspirin and clopidogrel, presented to the emergency department due to hemoptysis (total blood volume approximately 10ml) of 24 hours of onset accompanied by epistaxis. He denied any other symptoms. Physical examination was normal and oxygen saturation was 95% on room air. On laboratory tests, the patient had elevated D-Dimers values: 1834ng/mL (normal values < 500ng/mL). Hematocrit was 36%. Urinalysis was normal. Chest X-ray on admission was normal. The patient underwent computerized tomography (CT) angiography which excluded both pulmonary embolism and enlarged bronchial arteries and revealed ground glass opacities mainly in the right upper, right lower and left upper lobes (Fig. 1). Otolaryngologist (ENT) evaluation was normal. A working-diagnosis of pulmonary hemorrhage was set, and dual antiplatelet therapy was discontinued after expert vascular-surgery consultation.
Fig. 1.
Chest computerized tomography (CT) angiography showing ground glass opacities in both lower lobes.
The patient was admitted to the hospital and received empiric treatment for lower respiratory tract infection (LRTI) with intravenous antimicrobials (ampicillin-sulbactam). Flexible bronchoscopy revealed obstruction of the right superior lobar bronchus and the middle lobar bronchus by blood clots. Sputum cultures were positive for Pseudomonas aeruginosa. The patient remained asymptomatic and antiplatelet therapy was initiated solely with aspirin in the 4th day of hospitalization without recurrence of hemoptysis. Hemoptysis did not re-appear, and the patient was discharged 3 days later. Upon discharge the patient was advised to receive monotherapy with aspirin and to perform a second bronchoscopy one month later. One month later, the patient remained stable under antiplatelet monotherapy, whereas repeat bronchoscopy revealed complete remission of abnormal endobronchial findings.
3. Case 2
A 70-year-old male, former smoker (150pys), with a history of laryngectomy and tracheostomy in a background of laryngeal cancer 15 years ago, presented to the emergency department due to cough and expectoration of hemorrhagic secretions from the tracheostomy of 3 days of onset with no other symptoms. The patient's medical history was significant for arterial hypertension, hypothyroidism, surgery for ascending aorta aneurism and coronary artery bypass grafting 4 years ago, for which he was receiving aspirin antiplatelet therapy. Chest X-ray showed enlargement of the right hilum. Clinical examination was normal apart from bilateral crackles, on chest auscultation. Oxygen saturation was 98% on room air. Laboratory results showed slightly elevated D-Dimers: 864ng/mL (normal values < 500ng/mL) and mild thrombocytopenia:145K/μl (normal values 150–400K/μl) while hematocrit was 43%. Urinalysis was normal. CT angiography excluded pulmonary embolism revealing bilateral ground glass opacities in the lower lung lobes. Endoscopic evaluation detected the presence of blood on the left main bronchus. Upon suspicion of pulmonary hemorrhage, the patient was admitted to the hospital where antiplatelet therapy was discontinued and empirical antimicrobial treatment for LRTI with ampicillin-sulbactam plus azithromycin were administered. Repeat endoscopic evaluation the 4th day of hospitalization showed no further bleeding. Sputum cultures grew positive for Pseudomonas aeruginosa and Staphylococcus aureus. The patient was discharged a week later with the instruction to discontinue antiplatelet treatment with aspirin.
4. Case 3
An 80-year-old non-smoker female patient, presented to the ER department complaining of hemoptysis of 24 hours of onset (expectorated blood volume approximately 60ml). The patient reported a medical history of arterial hypertension, gastrointestinal bleeding (30 years ago), tetraplegia due to myelitis (onset on the age of 40), moderate to severe aortic stenosis and transient ischemic attack 4 months ago for which she was receiving antiplatelet therapy with clopidogrel. The patient presented severe dyspnoea in a background of hypoxemic respiratory failure (pO2 = 45 mmHg, pCO2 = 45 mmHg, pH = 7.44, SpO2 = 87.5%, on room air). She was hemodynamically stable (blood pressure: 155/93 mmHg), while auscultation revealed bilateral crackles. D-Dimers were within normal values as well as the rest of the laboratory tests. Chest X-ray showed bilateral alveolar infiltrates. Chest CT angiography was performed revealing bronchiectasis in the middle lobe, the lingula and the left lower lobe (Fig. 2). ENT examination was normal. The patient was admitted to the hospital for pulmonary hemorrhage in a background of bronchiectasis, LRTI and antiplatelet treatment. Intravenous tranexamic acid, cough depressant drugs and iv piperacillin-tazobactam were initiated. As the episode of hemoptysis was clinically severe and due to the fact that bronchiectasis were detected, the patient was also investigated for autoimmune serology including antinuclear antibody (ANA), cyclic citrullinated peptide antibodies (anti-CCP) and anti-neutrophil cytoplasm antibodies (ANCA), which were all negative. Clopidogrel was discontinued. Hemoptysis had fully ceased. The patient was discharged two weeks later after significant clinical and radiologic improvement and complete remission of hemoptysis and respiratory failure. Regarding antiplatelet treatment, based on expert multidisciplinary evaluation (pneumonology-neurology-cardiology) she was instructed to receive only aspirin which was re-administered 3 days before discharge and did not result to reoccurrence of hemorrhage.
Fig. 2.
Chest CT angiography revealed bronchiectasis in the middle lobe, the lingula and the left lower lobe.
5. Case 4
A 60-year-old male patient, current smoker (50pys), with a history of chronic alcohol consumption, arterial hypertension, dyslipidaemia, right iliac artery stenting due to stenosis 7 years ago, and coronary angioplasty and stenting 9 months ago due to myocardial infarction, presented to the emergency (ER) department complaining about hemoptysis and reporting blood volume of approximately 30 ml. The patient was receiving dual antiplatelet therapy (aspirin and clopidogrel). Physical examination revealed bilateral wheezing, no hemodynamical compromise and hypoxemia (pO2 = 61 mmHg, pCO2 = 35 mmHg, pH = 7.51, SpO2 = 93%, on room air). Laboratory tests including urinalysis were abnormal only for D-Dimers values at 770ng/mL (normal values < 500ng/mL). Chest X-ray was normal. Chest CT angiography excluded pulmonary embolism but revealed enlargement of the right bronchial artery (3.5mm) (Fig. 3a) and ground glass opacities in the right lower lobe (Fig. 3b). The patient was admitted to the hospital for pulmonary hemorrhage and empirical antimicrobial treatment with iv ampicillin-sulbactam was initiated for presumptive LRTI. Upon expert cardiology evaluation, the continuation of antiplatelet treatment with clopidogrel was deemed necessary while aspirin was discontinued. Sputum cultures grew positive for multiple common pathogens such as Klebsiella pneumonia, Pseudomonas aeruginosa and Escherichia coli which were evaluated as commensals. The patient was discharged 10 days later significantly ameliorated under monotherapy with clopidogrel.
Fig. 3A.
Chest CT angiography depicted enlargement of the right bronchial artery.
Fig. 3B.
Chest CT showed ground glass opacities in the right lower lobe and enlargement of the right bronchial artery (black arrow).
6. Case 5
A 57-year-old male patient, current smoker (30pys), presented to the ER department complaining about one episode of hemoptysis reporting blood volume of approximately 50 ml. The patient denied any other symptoms. He reported a history of asthma, arterial hypertension, dyslipidaemia, and coronary artery disease diagnosed by coronary angiography, for which he was receiving dual antiplatelet treatment (aspirin and clopidogrel). Upon examination his oxygen saturation was 95% on room air, while the rest of the clinical examination laboratory tests and chest x-ray were normal. A chest CT angiography was performed revealing ground glass opacities at the right upper lobe (Fig. 4). ENT examination was normal. The patient was admitted in the hospital for pulmonary hemorrhage and received intravenous antimicrobials (ampicillin-sulbactam) for presumptive LRTI. Dual antiplatelet treatment was discontinued with regression of symptoms and signs. Broncho-alveolar lavage (BAL) though flexible bronchoscopy was performed revealing no abnormal findings whereas all cultures grew sterile. Aspirin was re-started without hemoptysis relapse based on expert cardiology evaluation. The patient was discharged 8 days later in a good condition while blood expectoration was fully ceased and after cardiologic evaluation with instruction to receive only aspirin.
Fig. 4.
Chest CT angiography revealed ground glass opacities at the right upper lobe.
7. Discussion
In this case series, we report 5 different patients under treatment with antiplatelet therapy who presented with hemoptysis highlighting the need for clinical awareness and proposing a therapeutic algorithm based on the balance between individuals’ ischemic and hemorrhagic risk. Each patient received this therapy for a different period of time and for different cardiovascular diseases. In all patients, the lung origin of the hemorrhage was confirmed by lung imaging and/or bronchoscopy management was based on the current hemoptysis guidelines which include both supportive measures and interventional approaches such as embolization when necessary [5].
Dual antiplatelet therapy has been reported to reduce the incidence of stent thrombosis to less than 1% and currently is the commonest strategy after stent placement [1]. Clopidogrel plus aspirin for at least 12 months [6] has been the standard antiplatelet therapy after stenting [1] and single antiplatelet therapy is suggested thereafter [7]. However, hemorrhagic complications caused by dual antiplatelet therapy occur frequently [8]. In our patients receiving dual antiplatelet therapy due to previous stenting the decision of discontinuation was based on the time from the stent placement and the severity of hemoptysis. Since in both cases the episodes of hemoptysis were not major, the decision was only based on the degree of thrombotic risk. Withholding antiplatelet therapy in order to reduce the bleeding risk is associated, however, with risk of ischemic events, such as life-threatening stent thrombosis, myocardial infarction and stroke [9,10]. Therefore, management of pulmonary hemorrhage in patients receiving antiplatelets raises significant challenges and safety concerns. Defining the ‘Golden Mean’ requires both estimation of the thrombotic risk, as defined by cardiologists and evaluation of the severity of the bleeding event, as determined by pulmonologists.
Major bleeding has been recognized as a frequent non-cardiac complication of contemporary therapy for acute coronary syndrome. Factors associated with a higher risk of bleeding include advanced age, female sex, previous history of bleeding, and renal insufficiency [11]. Pulmonary hemorrhage appears as a bilateral alveolar infiltration shadow on chest radiography and can be easily mistaken for acute pulmonary edema especially in patients with concomitant cardiovascular disease [4]. A clinical observation, however, that can be emerged from our cases is that the antiplatelet-provoked pulmonary hemorrhage differed from the classical presentation of diffuse alveolar hemorrhage, being mild with less severe symptoms and not leading to hypoxemia. Also, no hematocrit decrease was observed among our patients. Our observation is compatible with other previously reported cases in which pulmonary hemorrhage was controlled by antiplatelet cessation [12,13]. In the literature only one fatal case due to pulmonary hemorrhage has been so far described concerning a patient receiving combination of dual antiplatelet therapy (clopidogrel and aspirin) with tirofiban a (GPIIb/IIIa receptor inhibitor) [14]. Similarly, the radiological image of our cases also differed from the diffuse pattern that characterizes diffuse alveolar hemorrhage, with the observed infiltrates being more patchy and not so diffuse.
It is important to mention that anti-platelet therapy discontinuation does not immediately lead to the complete cessation of their antithrombotic effect which continues to apply still for several days (a time needed for the re-establishment of normal platelet function) [15,16]. Clopidogrel presents a similar pharmacodynamic pattern to aspirin. Therefore, due to the cumulative inhibition of platelet function with repeated daily administration even of low doses, platelet function does not return to normal until 7–10 days after the last dose. This is the result of the cumulative nature of the inhibitory effects, the slow rate of recovery of platelet thromboxane production (aspirin) or thienopyridine adenosine diphosphate (ADP)-induced platelet aggregation (clopidogrel) and is consistent with the permanent inhibition of cyclooxygenase-1 (COX-1) and the P2Y12 receptor, respectively [15]. However, when a bleeding event is ongoing the discontinuation of administration of these agents is always the first step, and in cases in which the lung is the principal source of bleeding the algorithm of the management of hemoptysis must be followed thereafter to control bleeding [17].
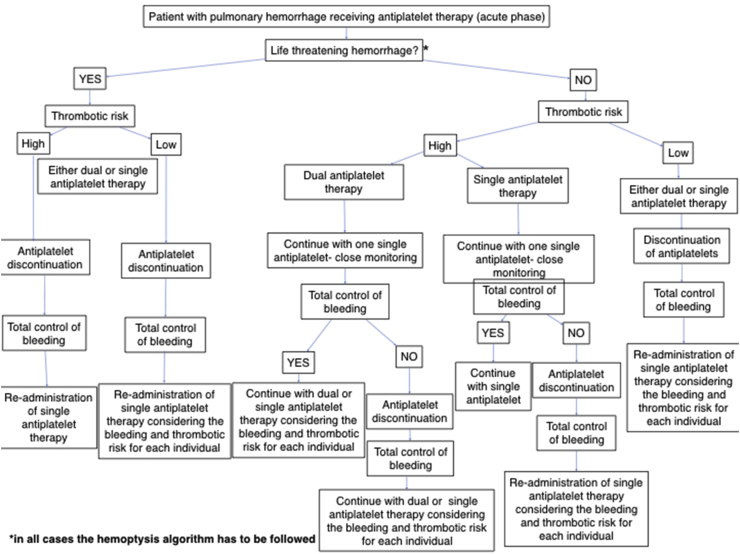
The first step in our algorithm (Fig. 5) is to evaluate the severity of the bleeding episode and apply the current hemoptysis guidelines and all the necessary supportive measures in order to achieve bleeding cessation and aspiration prevention. As with any potentially serious health condition, evaluation of the airway, breathing, and circulation, known as ‘ABC’, remains a critical step. Life-threatening hemoptysis was considered when bleeding occurred at a rate of at least 200 ml/h in a patient [5]. In not life-threatening events, the choice of discontinuation of the antiplatelet treatment is based on the individual's thrombotic risk. For instance, in our first case, due to the compatible history of recent carotid stent implantation, it was decided to continue treatment with a single antiplatelet agent instead of two, after outweighing the potential risks and complications. In the 2nd case, however, antiplatelet discontinuation was decided after taking into consideration that his bleeding risk was higher compared to the thrombotic, as the patient had a permanent tracheostomy and was not able to handle his secretions including a possible bleeding due to absence of the ability of expectoration. In the 3rd case, pulmonary hemorrhage was life-threatening leading to severe hypoxemia. Furthermore, the neurological comorbidities of the patient leaded to disability of handling pulmonary secretions due to reduced ability for expectoration. However, the history of moderate to severe aortic stenosis and the recent transient ischemic attack (4 months ago), also increased the thrombotic risk. For that reason, when bleeding was totally controlled and imaging was improved, it was decided to continue treatment with one single antiplatelet with close monitoring and follow up. In the 4th case, the thrombotic risk (recent myocardial infraction and coronary stenting) was greater compared to bleeding risk and since hemorrhage was not life threatening it was decided to continue therapy with a single antiplatelet with close monitoring of the patient. Also in this case, hemorrhage was controlled and there was no need for further intervention. However, in this case there was a possible source of hemorrhage [enlargement of the right bronchial artery (3.5mm)] and embolization was scheduled in case bleeding was not controlled with best supportive care. Since hemorrhage was controlled, continuation of therapy with a single antiplatelet was decided. Finally in the fifth we also decided to continue treatment with a single antiplatelet due to the fact that again hemorrhage was not life threatening and thrombotic risk was considered greater compared to the bleeding risk.
Fig. 5.
Algorithmic approach for the management of pulmonary hemorrhage in patients receiving antiplatelets.
Therefore, we suggest in patients with low thrombotic risk who present not life-threatening hemorrhage temporary discontinuation of antiplatelet therapy (either dual or single) and consider re-administration of a single antiplatelet agent (Fig. 5). In cases with high thrombotic risk and not life-threatening hemorrhage, we suggest continuing single antiplatelet therapy with close monitoring of the patient and follow the hemoptysis algorithm until cessation of bleeding (Fig. 5). When hemorrhage is totally controlled, the patient can continue treatment with dual or single antiplatelet agent after considering the bleeding and thrombotic risk ratio. In case the hemorrhage is not totally controlled, temporary discontinuation of antiplatelets has to be performed with close follow up of the patient and dual or single antiplatelet treatment can be readministered after cessation of hemorrhage. On the other hand, in cases of life-threatening hemorrhage, we propose antiplatelet therapy to be temporarily ceased until bleeding is controlled regardless the level of thrombotic risk and the hemoptysis algorithm to be followed. After cessation of hemorrhage, single antiplatelet therapy may be administered in patients with high thrombotic risk while in patients with low thrombotic risk we suggest that the decision of re-administrating or not a single antiplatelet agent should be based on the evaluation of the ratio of bleeding and thrombotic risk and on multidisciplinary approach among pulmonologists and cardiologists.
Our algorithm has some limitations. First, deciding whether temporarily discontinuing or continuing antiplatelet therapy is based on the treating physician's judgment and the individuals' risk of thrombosis and hemorrhage. However, we have tried to give some general instructions regarding how to handle these patients outweighing the bleeding and thrombotic risk. Moreover, bleeding control is based on the current hemoptysis guidelines which include both supportive measures and interventional approaches such as embolization in cases where the source of bleeding is revealed. Finally, another limitation of our algorithm could be that it does not take into consideration any history significant for pulmonary diseases, however, we suggest that the critical steps in the management of pulmonary hemorrhage due to antiplatelet therapy should be followed as described in the algorithm independently of the presence of potential underlying pulmonary disorders.
In conclusion, the management of pulmonary hemorrhage in patients receiving antiplatelets requires specific instructions. We suggest a clear algorithm based on the severity of pulmonary hemorrhage and the individuals' thrombotic risk. Multidisciplinary agreement in such cases seems critical. Potential re-administration of antiplatelets is suggested to take place before discharge and according to the patients’ risk.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Valgimigli M., et al. ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS) Eur. Heart J. 2017;39(3):213–260. doi: 10.1093/eurheartj/ehx419. 2018. [DOI] [PubMed] [Google Scholar]
- 2.Roy P., et al. Impact of "nuisance" bleeding on clopidogrel compliance in patients undergoing intracoronary drug-eluting stent implantation. Am. J. Cardiol. 2008;102(12):1614–1617. doi: 10.1016/j.amjcard.2008.07.063. [DOI] [PubMed] [Google Scholar]
- 3.Ohkubo K., et al. Incidence of side-effects of dual antiplatelet therapy with clopidogrel and aspirin after coronary stent implantation. Cardiovasc. Interv. Ther. 2011;26(1):33–37. doi: 10.1007/s12928-010-0031-2. [DOI] [PubMed] [Google Scholar]
- 4.Fernández-Perez G.C., et al. Pulmonary hemorrhage in a patient with acute coronary syndrome. AJR Am. J. Roentgenol. 2007;189(3):W135–W137. doi: 10.2214/AJR.05.0786. [DOI] [PubMed] [Google Scholar]
- 5.Sakr L., Dutau H. Massive hemoptysis: an update on the role of bronchoscopy in diagnosis and management. Respiration. 2010;80(1):38–58. doi: 10.1159/000274492. [DOI] [PubMed] [Google Scholar]
- 6.Wilson S.J., et al. Duration of dual antiplatelet therapy in acute coronary syndrome. Heart. 2017;103(8):573–580. doi: 10.1136/heartjnl-2016-309871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Capodanno D., et al. ACC/AHA versus ESC guidelines on dual antiplatelet therapy: JACC guideline comparison. J. Am. Coll. Cardiol. 2018;72(23 Pt A):2915–2931. doi: 10.1016/j.jacc.2018.09.057. [DOI] [PubMed] [Google Scholar]
- 8.Costa F., et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. 2017;389:1025–1034. doi: 10.1016/S0140-6736(17)30397-5. 10073. [DOI] [PubMed] [Google Scholar]
- 9.Douketis J.D., et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e326S–e350S. doi: 10.1378/chest.11-2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rossini R., et al. A multidisciplinary approach on the perioperative antithrombotic management of patients with coronary stents undergoing surgery: surgery after stenting 2. JACC Cardiovasc. Interv. 2018;11(5):417–434. doi: 10.1016/j.jcin.2017.10.051. [DOI] [PubMed] [Google Scholar]
- 11.Moscucci M., et al. Predictors of major bleeding in acute coronary syndromes: the global registry of acute coronary events (GRACE) Eur. Heart J. 2003;24(20):1815–1823. doi: 10.1016/s0195-668x(03)00485-8. [DOI] [PubMed] [Google Scholar]
- 12.Kilaru P.K., et al. Diffuse alveolar hemorrhage after clopidogrel use. J. Invasive Cardiol. 2001;13(7):535–537. [PubMed] [Google Scholar]
- 13.Onuk T., et al. Diffuse alveolar hemorrhage after clopidogrel use. Balkan Med. J. 2016;33(6):719–720. doi: 10.5152/balkanmedj.2016.151545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill D.S., Ng K., Ng K.S. Massive pulmonary haemorrhage complicating the treatment of acute coronary syndrome. Heart. 2004;90(3):e15. doi: 10.1136/hrt.2003.028589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eikelboom J.W., et al. Antiplatelet drugs: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e89S–e119S. doi: 10.1378/chest.11-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weber A.A., et al. Recovery of platelet function after discontinuation of clopidogrel treatment in healthy volunteers. Br. J. Clin. Pharmacol. 2001;52(3):333–336. doi: 10.1046/j.0306-5251.2001.01453.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quigley N., Gagnon S., Fortin M. Aetiology, diagnosis and treatment of moderate-to-severe haemoptysis in a North American academic centre. ERJ. Open Res. 2020;6(4) doi: 10.1183/23120541.00204-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]