Abstract
Background
In 2015, the emergency department of a municipal hospital in Vienna began to perform noninvasive ventilation (NIV) on patients admitted for acute respiratory failure, given no intubation criteria were met. The intention of this study was to show to which type of hospital unit patients were transferred after undergoing NIV in the emergency department. Additionally, the impact of the underlying disease, a patient’s sex and age and the year of intervention were analyzed.
Methods
A single-center retrospective exploratory study was performed on 371 patients. All patients with acute respiratory failure who were noninvasively ventilated at the study center emergency department from 2015 to 2018 were eligible. Relevant data were extracted from the patient’s medical records.
Results
A total of 43.7% (95% confidence interval, CI 38.8–48.5%) of patients were successfully stabilized in the emergency department through NIV and subsequently transferred to a normal care unit or discharged. This nonintensive care admission rate was significantly associated with certain underlying medical conditions, age and year of intervention. A further 19.7% (95% CI 15.6–23.7%) of patients were transferred to an intermediate care unit instead of an intensive care unit.
Conclusion
These findings emphasize the importance of noninvasive ventilation at the emergency department in reducing load on intensive care units and ensuring an efficient hospital workflow. Nonintensive care admission rate appears to be the highest in patients with pulmonary edema, especially in the higher age range and is also associated with the level of staff training. Prospective trials are needed to accurately confirm these correlations.
Keywords: Emergency medicine, Acute respiratory failure, Critical care, COPD
Introduction
Noninvasive ventilation (NIV) is nowadays frequently implemented in the routine of emergency departments, with a 2009 study at 132 academic hospital emergency departments across the USA reporting 64% of physicians to be very familiar with it, with 41% of sites being able to initiate NIV in less than 10 min [1]. Numerous studies have shown the efficacy of noninvasive ventilation in relieving acute respiratory distress in different conditions, such as chronical obstructive pulmonary disease (COPD) [2] or acute cardiogenic pulmonary edema [3], such as a reduction in mortality and a decreased rate of intubation; however, research on NIV specifically in the context of short-term treatment at an emergency department remains scarce.
In a 2009 trial including 198 patients, the initial application of NIV at an emergency department in patients with acute respiratory failure showed a significant reduction of subsequent in-hospital mortality and length of Intensive-Care-Unit or Intermediate-Care-Unit (ICU/IMC) stay compared to a control group without initial NIV treatment [4]. It was also demonstrated in another study that the average time it takes from the admission of a patient in respiratory failure to the application of NIV is significantly lower (56 min) when implemented at an emergency department than at an intensive care unit (84 min) [5].
To the authors’ knowledge, no study has yet addressed the impact of NIV at an emergency department on admissions to the intensive care unit. In a multitude of countries, intensive care units regularly operate on the limit capacity-wise [6, 7]. Sometimes, ICU bed availability can even influence decisions on ICU admissions of critical care patients [8]. The pending COVID-19 pandemic aggravated this problem further, with guidelines emerging on how to deal with acute shortages of intensive care beds [9]. Additionally, cost per bed per day is substantially higher in intensive care units than in normal care units [10].
The emergency department at the study center, a municipal hospital in Vienna, implemented NIV in the beginning of 2015. Formerly, all arriving patients in acute respiratory failure were admitted directly to the intensive care unit. Now, they are treated with NIV and corresponding medication in the emergency department for several hours. Once a thorough work-up on the patient is done, a decision is made where the patient should be transferred to. This can either be an intensive care unit, an intermediate care unit or a normal care unit in the same hospital. If a patient’s condition improves significantly, there is also the option of an overnight stay directly in the emergency department and subsequent discharge from there. The decision where to transfer a patient to is based on the cardiorespiratory situation of the patient as assessed by interpretation of vital parameters and blood gas analysis by the emergency physician on duty.
The primary outcome of this study was to show to which type of hospital unit the patients were transferred after receiving NIV in the emergency department. As secondary outcomes, we stratified this distribution by medical condition, age, sex and year of intervention. This enables discussion on whether a certain condition, a certain age range or a certain sex responds better to NIV in the emergency department than another. We also deemed the year of intervention interesting as in the later years of the study’s timeframe, the staff became more experienced with the procedure, supposedly raising the quality of NIV application.
Patients, material and methods
Patient recruitment
A single-center retrospective exploratory observational study was performed on 371 patients.
Eligible for this study were all patients admitted to the emergency department from 1 January 2015, through 30 November 2018 by ambulance or self-admission (around 120,000 patients).
An inclusion criterion was the application of NIV in the emergency department. NIV was applied to all patients in acute respiratory failure (defined by either PaO2 < 60 mm Hg or PaCO2 > 50 mm Hg or both in arterial blood gas analysis at the time of admission), given no intubation criteria were met. According to guidelines [11], these are: absence of spontaneous breathing, airway obstruction, gastrointestinal hemorrhage or ileus and non-hypercapnic coma. The second inclusion criterion was the presence of one of four specific admission diagnoses: COPD, pulmonary edema (cardiogenic, hypertensive or combined), pneumonia and asthma. This criterion enables meaningful statistical analysis, but still accounts for the vast majority of NIV indications.
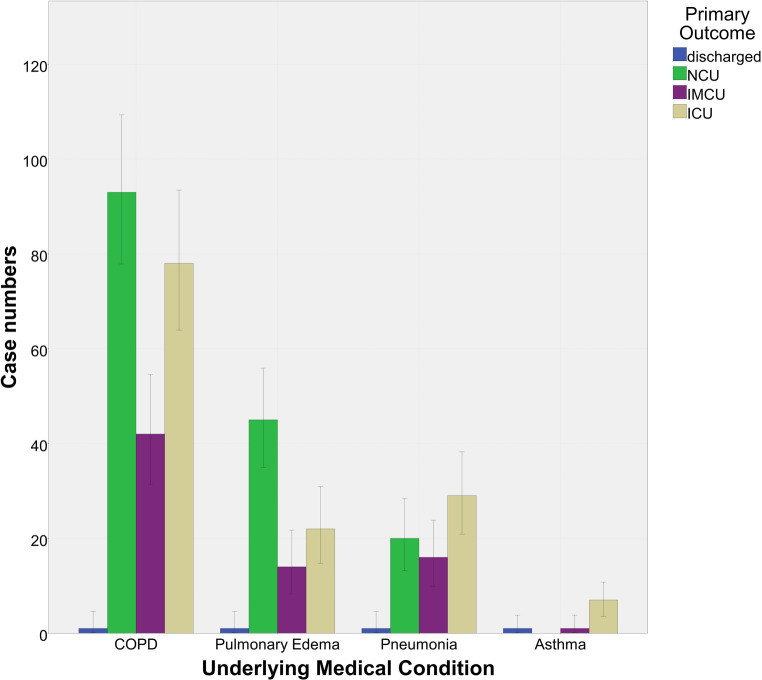
Patients without sufficient documentation were excluded (Fig. 1).
Fig. 1.
Flowchart demonstrating the process of patient selection
Measurements
Data on the following parameters were collected retrospectively by the study’s first author:
-
Primary outcome (categorical)
The primary outcome indicates the course of the patients after having received NIV at the study center’s emergency department and is comprised of the four categories intensive care, intermediate care, normal care and discharged.
-
Primary composite outcome (categorical)
For inferential statistical evaluation, it was decided to facilitate the primary outcome parameter from the four categories intensive care, intermediate care, normal care and discharged to two, intensive care admission and nonintensive care admission. Patients who were transferred to an intensive or intermediate care unit were assigned to the intensive care admission subgroup, patients admitted to a normal care unit or discharged to the nonintensive care admission subgroup.
-
Underlying medical condition (categorical)
The parameter underlying medical condition is defined as the condition that caused the acute respiratory distress which ultimately made noninvasive ventilation necessary. The four categories were acutely exacerbated COPD, pulmonary edema, pneumonia and asthma.
-
Year of intervention (metrical)
The year of intervention parameter identified the year in which the patient was admitted to the emergency department and received noninvasive ventilation. The possible values were 2015, 2016, 2017 and 2018.
-
Age and sex
The age parameter referred to the patient’s age at which noninvasive ventilation occurred, scaled metrically. Sex referred to the patient’s sex assigned at birth, scaled categorically.
Each patient who received NIV at the study center’s emergency department was manually recorded in a documentation booklet. After receiving approval and a waiver from informed consent from the study center’s responsible ethics committee (“Ethikkommission der Stadt Wien”—Ethics Committee of the City of Vienna, reference number EK 18-285-VK), the relevant data were non-anonymously extracted from the hospital’s documentation system and filled into anonymous, numbered case report forms. The data were then entered into a newly created database of the statistics program SPSS 23.0 by IBM (IBM, Armonk, NY, USA), where statistical calculations were executed.
Analysis
No proper sample size calculation was performed due to the exploratory character of this study; however, we deemed a patient number of 371 as high enough to allow for statistically significant results in our study setting.
For the baseline values in our study (age, sex, underlying medical condition and year of intervention) the total number for each subgroup as well as their percentual relation were calculated. For age, we additionally calculated the mean age and its standard deviation. The primary outcome and the primary composite outcome were also descriptively analyzed and 95% confidence intervals were calculated via bootstrapping (replications: 2000). Since the cases that were missing data were eliminated prior to statistical analysis, a complete case analysis was performed and no missing data imputations were used.
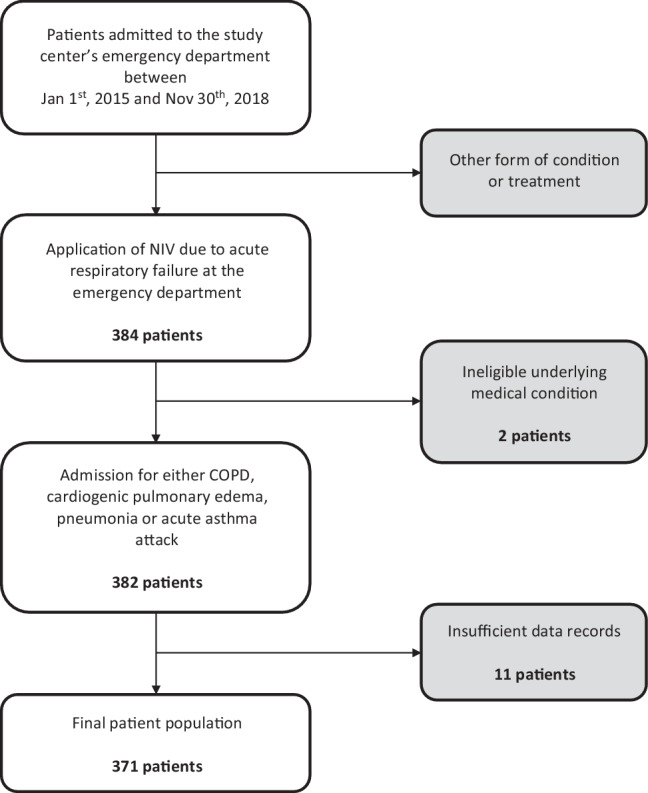
A bar chart was plotted visualizing the primary outcome grouped by underlying medical condition. (Fig. 2).
Fig. 2.
Bar chart representing the primary outcome, clustered by underlying medical condition, with 95% confidence intervals. NCU normal care unit, IMCU intermediate care unit, ICU intensive care unit
The secondary outcomes compare different populations, allowing for inferential statistics. Since this study was of exploratory character, no Bonferroni correction was calculated for the significance values, α remains 0.05.
Our aim was to estimate whether certain circumstances like a patient’s age or the underlying medical condition had an influence on subsequent intensive care admission. We therefore employed a logistic regression model with the dependent variable primary composite outcome and the independent variables underlying medical condition, age, sex and year of intervention.
All statistical assumptions for binary logistic regression were met in our sample. First, null and alternative hypotheses were formulated for each correlation (for example: H0 = age cannot estimate intensive care admission; H1 = age can estimate intensive care admission). For independent parameters that were categorical, dummy variables were coded for each category. For underlying medical condition, asthma was chosen as the reference category, for sex male and for year of intervention the last year of the study’s timeframe, 2018. Finally, the calculation was undertaken in the statistics software. To prove the model’s validity, an omnibus test of model coefficients and subsequently the Hosmer-Lemeshow goodness-of-fit test were performed and 95% confidence intervals were calculated for the odds ratios.
Results
Characteristics of the study subjects
All descriptive data can be found accumulated in (Table 1), the values for the logistic regression are given in (Table 2).
Table 1.
Baseline values and descriptive statistics
| Primary outcome | |||||
| All patients | ICU | IMCU | NCU | Discharged | |
| Cases (%) | 371 | 136 (36.7%) | 73 (19.7%) | 158 (42.6%) | 4 (1.1%) |
| [95% CI] | – | [31.8–41.2] | [15.6–23.7] | [37.7–47.7] | [0.3–2.2] |
| Mean age in years [SD] | 69.7 [11.8] | 66.8 [12.8] | 71.0 [9.1] | 71.2 [11.6] | 66.8 [15.7] |
| Female (%) | 181 (48.8%) | 72 (39.8%) | 35 (19.3%) | 73 (40.3%) | 1 (0.6%) |
| Male (%) | 190 (51.2%) | 64 (33.7%) | 38 (20%) | 85 (44.7%) | 3 (1.6%) |
| Medical condition (%) | |||||
| COPD | 214 | 78 (36.4%) | 42 (19.6%) | 93 (43.5%) | 1 (0.5%) |
| Pulmonary edema | 82 | 22 (26.8%) | 14 (17.1%) | 45 (54.9%) | 1 (1.2%) |
| Pneumonia | 66 | 20 (30.3%) | 16 (24.2%) | 29(43.9%) | 1 (1.5%) |
| Asthma | 9 | 7 (77.8%) | 1 (11.1%) | 0 (0.0%) | 1 (11.1%) |
| Year of intervention (%) | |||||
| 2015 | 11 | 5 (45.5%) | 2 (18.2%) | 3 (27.3%) | 1 (9.1%) |
| 2016 | 53 | 28 (52.8%) | 10 (18.9%) | 15 (28.3%) | 0 (0.0%) |
| 2017 | 148 | 48 (32.4%) | 33 (22.3%) | 67 (45.3%) | 0 (0.0%) |
| 2018 | 159 | 55 (34.6%) | 28 (17.6%) | 73 (45.9%) | 3 (1.9%) |
| Primary composite outcome | |||||
| Intensive care admission | Nonintensive care admission | ||||
| Cases (%) | 209 (56.3) | 162 (43.7) | |||
| [95% CI] | [51.5–61.2] | [38.8–48.5] | |||
| Female (%) | 181 | 107 (59.1) | 74 (40.9) | ||
| Male (%) | 190 | 102 (53.7) | 88 (46.3) | ||
| Medical condition (%) | |||||
| COPD | 214 | 120 (56.1%) | 94 (43.9%) | ||
| Pulmonary edema | 82 | 36 (43.9%) | 46 (56.1%) | ||
| Pneumonia | 66 | 45 (68.2%) | 21 (31.8%) | ||
| Asthma | 9 | 8 (88.9%) | 1 (11.1%) | ||
| Year of intervention (%) | |||||
| 2015 | 11 | 7 (63.6%) | 4 (36.4%) | ||
| 2016 | 53 | 38 (71.7%) | 15 (28.3%) | ||
| 2017 | 148 | 81 (54.7%) | 67 (45.3%) | ||
| 2018 | 159 | 83 (52.2%) | 76 (47.8%) | ||
Percentage values always to be read in line
ICU intensive care unit, IMCU intermediate care unit, NCU normal care unit, SD standard deviation, CI confidence interval
Table 2.
Nonintensive care admission estimation by binary logistic regression
| Logistic regression model | ||||
|---|---|---|---|---|
| χ2-test | Degrees of freedom | p‑value | ||
| Omnibus test | – | 27.61 | 8 | < 0.01 |
| Hosmer-Lemeshow test | – | 5.74 | 8 | 0.68 |
| % correctly estimated | 61.20% | – | – | – |
| Independent variables | Odds ratio | 95% CI for odds ratio | p‑value | |
| Medical condition | ||||
| COPD | – | 5.37 | 0.65–44.69 | 0.12 |
| Pulmonary edema | – | 9.41 | 1.10–80.53 | 0.04 |
| Pneumonia | – | 3.07 | 0.35–26.80 | 0.31 |
| Asthma (ref.) | – | – | – | 0.01 |
| Year of intervention | ||||
| 2015 | – | 0.85 | 0.54–1.34 | 0.48 |
| 2016 | – | 0.40 | 0.20–0.80 | 0.01 |
| 2017 | – | 0.57 | 0.15–2.12 | 0.40 |
| 2018 (ref.) | – | – | – | 0.07 |
| Sex (ref. = male) | ||||
| Female | – | 0.76 | 0.50–1.17 | 0.21 |
| Age (years) | – | 1.03 | 1.00–1.05 | 0.03 |
The dependent variable of this logistic regression model was the primary composite outcome. The odds ratio gives the ratio of the odds for the primary composite outcome being 1 (=non-intensive care admission) in a certain category compared to the reference category in the variable while “controlling” for all other variables (while assuming all other variables stay the same). Values are shown to two decimal points
CI confidence interval
A total of 371 patient cases were analyzed. The median age in our patient population was 70 years with a standard deviation of 11.8 years and a range of 21–98 years. Of the patients 51.2% were male, 48.8% female. 3% of patients were treated in the year 2015, 14.3% in 2016, 39.9% in 2017 and 42.8% in 2018.
The underlying medical condition that led to admission the most often was acutely exacerbated COPD with 57.1% of patients, followed by pulmonary edema with 22.1%. Pneumonia accounted for 17.8% of admissions and acute asthma attacks for 2.4%.
Primary outcome
Our data show that 43.7% of patients in the study population were not admitted to intensive care, meaning they improved at the emergency department in such a way that they could be transferred to a normal care unit or even discharged. Normal care admissions accounted for 42.6% and discharges for 1.1%.
Of our patients 56.3% had to be admitted to an intensive care (ICU) or intermediate care unit (IMCU), with intensive care admissions of 36.7% and intermediate care admissions of 19.7%.
Secondary descriptive outcomes
For underlying medical condition, the nonintensive care admission rate was the highest in the pulmonary edema subgroup (56.1%), followed by the COPD (43.9%), pneumonia (31.8%) and finally the asthma subgroup (11.1%). The year of intervention showed higher nonintensive care admission rates in the later years (2017: 45.3; 2018: 47.8%) compared to when NIV was first implemented (2015: 36.4%; 2016: 28.3%). Finally, male patients had a slightly higher nonintensive care admission rate (46.3%) than females (40.9%).
Secondary inferential outcomes
The employed logistic regression model was able to estimate 61.2% of the cases correctly. The omnibus test for model coefficients and the Hosmer-Lemeshow goodness-of-fit test further indicated that the logistic regression model was valid.
Regarding underlying medical condition, the data show that patients with pulmonary edema had a significantly higher estimated nonintensive care admission rate than patients with asthma with an odds ratio of 9.41 (95% CI: 1.1–80.53). Asthma itself was also strongly associated with a low nonintensive care admission rate. Patients treated in the year 2018 had a significantly higher chance of not requiring intensive care than patients treated in 2016 (odds ratio: 2.53, 95% CI 1.26–5.05), with the year 2018 itself associated with NIV success.
A patient’s age was also able to estimate the nonintensive care admission rate with an odds ratio of 1025 (95% CI 1003–1047), suggesting that with each additional year, the odds of NIV success increased by 2.5%. A patient’s sex had no significant influence on the estimated nonintensive care admission rate.
Discussion
The results of this study show that an emergency department with NIV capability on site plays an important role in stabilizing patients in acute respiratory failure and therefore reducing the load on the hospital’s intensive care unit.
In the treatment of these patients, simple oxygen masks are often insufficient, however invasive ventilation always goes along with sedation and subsequent admission to the ICU. Noninvasive ventilation seems to be the golden mean on this spectrum: it offers sufficient ventilation assistance but is also very easy to apply with a simple strap-on mask and no obligatory need for sedation. Every patient can undergo a trial of noninvasive ventilation given no contraindications are met, and if invasive ventilation becomes necessary, the patient can be intubated in the emergency department and transferred to the intensive care unit. If noninvasive ventilation combined with adequate medication is sufficient the patient can avoid intensive care admission and be further treated in normal care.
This event is oftentimes referred to as “NIV success” in other studies. While we do think that most of the patients in our nonintensive care admission subgroup experienced NIV success due to their clinical course, we cannot scientifically attribute it to NIV alone due to the lack of a control group that did not receive NIV.
In our study population, the nonintensive care admission rate in either hypertensive or cardiogenic pulmonary edema was the highest. Numerous studies prove the efficacy of noninvasive ventilation in this condition [3] and guidelines strongly suggest using it as the main treatment [11, 12]. It is therefore a prime example of NIV treatment at an emergency department. While acute respiratory distress is alleviated by ventilation support through NIV, the appropriate medication is given. The medication diminishes the pulmonary edema over the course of minutes to hours and NIV can then be terminated. The underlying chronic condition is subsequently treated in a normal care unit. The treatment of acutely exacerbated COPD follows a similar pattern.
Other frequent causes of acute respiratory failure, for example pneumonia, had a lower nonintensive care admission rate, in accordance with studies showing lower overall NIV success rates in this condition [13, 14]. One reason might be that fast alleviation through medical intervention is not possible. Therefore, NIV treatment for pneumonia in the emergency department seems to be less efficient. Acute asthma attacks can happen very fast and are sometimes resistant to medical treatment, resulting in life-threatening situations. To avoid such incidents, the indications for invasive ventilation in an acute asthma attack are set widely [11, 12], which might result in the observed low nonintensive care admission rates in the emergency department.
With age, prior studies show a lower NIV success rate in the higher age range [15] or no significant correlation [16]. In our study, however, older patients had a higher rate of nonintensive care admission than younger ones. We assume that diseases with higher NIV success rates, such as acutely exacerbated COPD or pulmonary edema, are the ones that normally become acute in older people. NIV is very effective in correcting these acute exacerbations back into a steady state. Acute asthma attacks and pneumonia on the other hand, conditions that also occur in the younger age range more often, have lower NIV success. This correlation shows that NIV in the emergency department might be especially effective in older patients. Since our result contradicts earlier studies, further clarification in this area is needed.
Another significant correlation concerns the year of intervention in the emergency department. Studies suggest that the level of staff training is associated with overall NIV success rate [17, 18]. When the emergency department at the study center was inaugurated in 2015, the application of NIV was not daily routine, but in the following months and years, experience in applying this treatment effectively and efficiently grew. Our data confirm that not only was it applied more frequently every year, but also nonintensive care admission rates ascended, showing that the observation made in prior studies is also true for an emergency department. We also think that rising familiarity with NIV at the department made the operators more confident in its effectiveness, leading to less transfers to intensive care units due to insecurity.
The main limitation of this study was its retrospective nature, which restricted the study design and results by available data. Information on ventilation parameters, patient’s physiology and comorbidity scores or treatment goals were not available but would have allowed grouping of patients with similar characteristics. Due to missing blood gas values and vital parameters, a patient’s course of disease could only be defined by the type of hospital care unit they were subsequently transferred to. Since there is no control group that did not receive NIV, it cannot be said with certainty that a reduction of ICU admissions was entirely due to NIV.
As usual in pilot studies, we opted for an exploratory study design. This gave us the opportunity to find interesting correlations more easily but limited the validity of the correlation significance due to missing Bonferroni correction. The sample size (9 cases) in the asthma subgroup was not too small to invalidate statistical analysis, however, we would suggest further research with higher sample sizes in this subgroup.
In conclusion, our study was able to give interesting insights into the impact of NIV application at a municipal emergency department. NIV was most effective in patients suffering from pulmonary edema, as well as patients in the higher age range and patients who were treated later in the study’s timeframe due to more experienced staff.
In order to solidify these results, more research is needed especially in confirming the correlations between nonintensive care admission rates and underlying medical condition and age. We would suggest prospective studies with additional variables such as physiology and comorbidity indices and possibly ventilation parameters.
These results emphasize the importance of an emergency department for an efficient hospital-wide workflow in treating acute care patients and preserving viable intensive care resources. We hope this study can serve as an incentive for care points who do not have NIV in use yet to implement it into their workflow.
Conflict of interest
Y.-T. Abulesz and M. Haugk declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yannic-Tomas Abulesz, Email: yannic-tomas.abulesz@meduniwien.ac.at.
Moritz Haugk, Email: moritz.haugk@gesundheitsverbund.at.
References
- 1.Hess DR, Pang JM, Camargo CA., Jr. A survey of the use of noninvasive ventilation in academic emergency departments in the United States. Respir Care. 2009;54(10):1306–1312. [PubMed] [Google Scholar]
- 2.Osadnik CR, Tee VS, Carson-Chahhoud KV, Picot J, Wedzicha JA, Smith BJ. Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017 doi: 10.1002/14651858.CD004104.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weng CL, Zhao YT, Liu QH, Fu CJ, Sun F, Ma YL, et al. meta-analysis: noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152(9):590–600. doi: 10.7326/0003-4819-152-9-201005040-00009. [DOI] [PubMed] [Google Scholar]
- 4.Tomii K, Seo R, Tachikawa R, Harada Y, Murase K, Kaji R, et al. Impact of noninvasive ventilation (NIV) trial for various types of acute respiratory failure in the emergency department; decreased mortality and use of the ICU. Respir Med. 2009;103(1):67–73. doi: 10.1016/j.rmed.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Horvath CM, Brutsche MH, Schoch OD, Schillig B, Baty F, vonOw D, et al. NIV by an interdisciplinary respiratory care team in severe respiratory failure in the emergency department limited to day time hours. Intern Emerg Med. 2017;12(8):1215–1223. doi: 10.1007/s11739-016-1546-z. [DOI] [PubMed] [Google Scholar]
- 6.OECD. Hospital beds (indicator). 2020. https://data.oecd.org/healtheqt/hospital-beds.htm. Accessed 11 June 2020.
- 7.Ma X, Vervoort D. Critical care capacity during the COVID-19 pandemic: global availability of intensive care beds. J Crit Care. 2020;58:96–97. doi: 10.1016/j.jcrc.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robert R, Coudroy R, Ragot S, Lesieur O, Runge I, Souday V, et al. Influence of ICU-bed availability on ICU admission decisions. Ann Intensive Care. 2015;5(1):55. doi: 10.1186/s13613-015-0099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maves RC, Downar J, Dichter JR, Hick JL, Devereaux A, Geiling JA, et al. Triage of scarce critical care resources in COVID-19 an implementation guide for regional allocation: an expert panel report of the task force for mass critical care and the American college of chest physicians. Chest. 2020;158(1):212–225. doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norris C, Jacobs P, Rapoport J, Hamilton S. ICU and non-ICU cost per day. Can J Anaesth. 1995;42(3):192–196. doi: 10.1007/BF03010674. [DOI] [PubMed] [Google Scholar]
- 11.Westhoff M, Schonhofer B, Neumann P, Bickenbach J, Barchfeld T, Becker H, et al. Noninvasive mechanical ventilation in acute respiratory failure. Pneumologie. 2015;69(12):719–756. doi: 10.1055/s-0034-1393309. [DOI] [PubMed] [Google Scholar]
- 12.Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 13.Confalonieri M, Potena A, Carbone G, Porta RD, Tolley EA, Meduri UG. Acute respiratory failure in patients with severe community-acquired pneumonia. A prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med. 1999;160(5 Pt 1):1585–1591. doi: 10.1164/ajrccm.160.5.9903015. [DOI] [PubMed] [Google Scholar]
- 14.Jolliet P, Abajo B, Pasquina P, Chevrolet JC. Non-invasive pressure support ventilation in severe community-acquired pneumonia. Intensive Care Med. 2001;27(5):812–821. doi: 10.1007/s001340100869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antonelli M, Conti G, Moro ML, Esquinas A, Gonzalez-Diaz G, Confalonieri M, et al. Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intensive Care Med. 2001;27(11):1718–1728. doi: 10.1007/s00134-001-1114-4. [DOI] [PubMed] [Google Scholar]
- 16.Poponick JM, Renston JP, Bennett RP, Emerman CL. Use of a ventilatory support system (BiPAP) for acute respiratory failure in the emergency department. Chest. 1999;116(1):166–171. doi: 10.1378/chest.116.1.166. [DOI] [PubMed] [Google Scholar]
- 17.Lopez-Campos JL, Garcia PC, Jimenez LA, Arnedillo A, Gonzalez-Moya E, Fenandez BJJ. Staff training influence on non-invasive ventilation outcome for acute hypercapnic respiratory failure. Monaldi Arch Chest Dis. 2006;65(3):145–151. doi: 10.4081/monaldi.2006.560. [DOI] [PubMed] [Google Scholar]
- 18.Yalcinsoy M, Salturk C, Oztas S, Gungor S, Ozmen I, Kabadayi F, et al. Can patients with moderate to severe acute respiratory failure from COPD be treated safely with noninvasive mechanical ventilation on the ward? Int J Chron Obstruct Pulmon Dis. 2016;11:1151–1160. doi: 10.2147/COPD.S104801. [DOI] [PMC free article] [PubMed] [Google Scholar]