Abstract
Background
Quality and safety in Australian healthcare is inequitably distributed, highlighted by gaps in the provision of quality care for Aboriginal and Torres Strait Islander children. Burns have potential for long-term adverse outcomes, and quality care, including culturally safe care, is critical to recovery. This study aimed to develop and apply an Aboriginal Patient Journey Mapping (APJM) tool to investigate the quality of healthcare systems for burn care with Aboriginal and Torres Strait Islander children.
Study design
Interface research methodology, using biomedical and cultural evidence, informed the modification of an existing APJM tool. The tool was then applied to the journey of one family accessing a paediatric tertiary burn care site. Data were collected through yarning with the family, case note review and clinician interviews. Data were analysed using Emden’s core story and thematic analysis methods. Reflexivity informed consideration of the implications of the APJM tool, including its effectiveness and efficiency in eliciting information about quality and cultural safety.
Results
Through application of a modified APJM tool, gaps in quality care for Aboriginal and Torres Strait Islander children and families were identified at the individual, service and system levels. Engagement in innovative methodology incorporating more than biomedical standards of care, uncovered critical information about the experiences of culturally safe care in complex patient journeys.
Conclusion
Based on our application of the tool, APJM can identify and evaluate specific aspects of culturally safe care as experienced by Aboriginal and Torres Strait Islander peoples and be used for quality improvement.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-022-08754-0.
Keywords: Patient journey mapping, Aboriginal and Torres Strait Islander, Indigenous, Burn care, Quality, Cultural safety, Disparities
Background
Significant focus and effort are being directed towards ensuring quality healthcare worldwide [1]. In Australia quality standards and accreditation measures [2] influence care provision and regulate healthcare efficiency and effectiveness. Engagement in quality improvement (QI) supports healthcare services and providers to constructively critique the healthcare they provide and implement improvement activities [1]. Often, improvement is focused on performance and limitations of healthcare services, with process mapping and clinical redesign as QI methods [3, 4]. These methods often lack inclusion of patient experiences, with efficiency processes not always enhancing patient experiences or improving health outcomes.
In Australia, quality healthcare for Aboriginal and Torres Strait Islander peoples has increasingly been linked to cultural safety [5] and competency of healthcare services [6, 7]. The revised National Safety and Quality Health Service Standards (2nd edn) [8] for health services now include six actions specific to the health of Aboriginal and Torres Strait Islander peoples’ and the cultural competency of tertiary healthcare services. This is the result of an increasing recognition that quality healthcare must consider both cultural [9, 10] and clinical safety, ensuring that all needs of an individual and family are met. This concept is supported by the Australian Safety and Quality Framework for Health Care [11] which positions consumer-centeredness as one of three key indicators of quality.
Many Aboriginal and Torres Strait Islander peoples have a holistic model of health and healing that is not fully responded to or always understood by Australia’s dominant biomedical health system [10]. The multi-dimensional holistic model includes considerations of physical, psychological, social health and wellbeing, spirituality, and cultural integrity aspects [12]. When cultural and spiritual aspects of health and healing are considered in the context of healthcare, health outcomes for Aboriginal and Torres Strait Islander peoples are improved, and an experience of culturally safe care can be achieved [5]. The theory of cultural safety, originally developed in New Zealand [13], has since been applied to healthcare in Australia [5, 9]. The principles of culturally responsive and respectful care have been adapted further, and have been used both in assessing quality in standards [14] and in Australian healthcare policy [15]. The cultural safety principles (reflexivity, dialogue, power imbalances, decolonisation and regardful care) are developed from First Nations knowledges and generations of lived experience [16].The principle of decolonisation sets cultural safety apart from other cultural frameworks as it is focussed on peoples who have been impacted by colonisation [16], and is different from cultural competency which takes an individualised perspective, and focusses on minority populations more broadly [6]. While many providers in the Australian mainstream healthcare system endeavour to provide culturally competent healthcare [6], it is unclear as to whether this leads to an experience of culturally safe care for consumers.
Reliably accessible patient-centred healthcare is a health inequity Aboriginal and Torres Strait Islander peoples face [17, 18], suggesting racism (in all forms), or at the very least, deficits in quality. Racism can be systemic, interpersonal or internalised [19]. Aboriginal and Torres Strait Islander peoples experiences of being judged, misunderstood, and stereotyped by healthcare providers in Australia’s mainstream healthcare system causes distress and disengagement of both individuals and families [20]. Further, communication breakdown in healthcare environments results in difficulty assessing symptoms, eliciting signs, reaching accurate diagnoses and providing effective care [21]. Institutional racism in health systems creates structural barriers and impacts at a population level. Together, these quality deficits contribute to inequitable health outcomes for Aboriginal and Torres Strait Islander peoples.
Aboriginal and Torres Strait Islander children experience burn injury at disproportionally higher rates than non-Indigenous children, and have in longer lengths of inpatient care [22]. Such disparities are one example of the many multifaceted and complex disparities experienced by Aboriginal and Torres Strait Islander families more broadly. Further, these disparities are intergenerational and need to be understood in the context of the family and community. So, while accreditation processes seek to ensure quality healthcare in tertiary settings [2], including those with specific cultural competency [8] and burn care [23] components, a single tool that specifically assesses both the clinical and cultural quality of burn care for Aboriginal and Torres Strait Islander children and families is lacking.
Patient Journey Mapping (PJM) is a quality assessment method used to better understand and provide a detailed account of patient healthcare journeys [24]. PJM has previously described the journey stages in which the healthcare system fails or succeeds to provide quality and responsive care to patients, and is therefore a useful method to appraise and guide organisations’ approaches to care [3, 4]. It highlights barriers and enablers to care from the perspective of both the recipient and provider of healthcare [3] and enables comparisons of critical points in time with existing best practice models and guidelines. Aboriginal PJM (APJM) can provide mechanisms for identifying gaps and facilitating improvements in Aboriginal patient journeys by depicting the complexities inherent in healthcare, with a focus on QI [25]. APJM may therefore provide an opportunity to investigate the lived experience of families of children with a burn injury within and across the health system and enable a proper exploration of disparities that are not simple in nature. This paper aims to examine the critical components relevant to, and modification of an existing APJM tool [26], specifically for Aboriginal and Torres Strait Islander children to assess quality and cultural safety in the burn care journey of Aboriginal and Torres Strait Islander families for the purpose of QI.
Methods
Ethical considerations
Ethics approval for this study was received from the: Aboriginal Health Research Ethics Committee; Women’s & Children’s Health Network Human Research Ethics Committee; Flinders University SBREC; Central Australian Human Research Ethics Committee; Human Research Ethics Committee of Northern Territory; Department of Health and Menzies School of Health; and the Department of Health Human Research Ethics Committee. All participants received a participant information sheet and provided written informed consent.
The research was guided by the National Health and Medical Research Council’s values and ethics for doing research with Aboriginal communities. These strategies were upheld throughout the research. The primary researcher (SF) worked in partnership with Waljen woman, mentor, PhD supervisor and author (TM) to design and undertake the project. Furthermore, this research forms part of a larger study [27] which is guided by an Aboriginal and Torres Strait Islander reference group.
Theoretical framework
Cultural safety and knowledge interface research informs the methodological constructs underpinning this research and provides a space to bring together the health and healing constructs of Aboriginal and Torres Strait Islander peoples and key indicators for western biomedical burn care quality [28–30]. This is a space without notions of dominance or superiority, within which mutual respect, shared benefits, human dignity and discovery provide an opportunity for new and relative knowledge production [28, 29, 31]. This research engages a qualitative study design [32] with Indigenous ways of knowing, being and doing [33] in the context of evaluating the quality and cultural safety of healthcare systems and services for burn care with Aboriginal and Torres Strait Islander children and families using APJM [25, 26].
Modifying the APJM Tool
To modify the APJM tool, we looked at the documented biomedical evidence informing burn care currently in Australia and found that acute burns, including those involving joints or young children, typically require specialist tertiary healthcare [34]. In Australia, these specialist tertiary services are metropolitan. We also found that burn care is best delivered by multi-disciplinary teams [35] comprising many healthcare professionals, who each bring a unique skill set, focus and contribution to care. Key professions in these teams include: nursing, occupational therapy, physiotherapy, medical, dietetics, psychology, and social work [35–38]. We also found that burn care can be separated into distinct critical points in time from a biomedical perspective, evident in the existing models that guide burn care [36] and research evidence [34]. These critical points, whilst referred to differently, include: the injury; emergency care; ambulatory care; admission; in-patient care; discharge; and rehabilitation. We found the evidence base for the models of burn care used in Australia [36–40] varied, however commonalities in treatment existed across the models. All evidence was incorporated into the APJM tool, and to consolidate and gain consensus on inclusion, input from clinicians and policy makers was sought through roundtables and review of the tool.
Consideration of the health and healing constructs of Aboriginal and Torres Strait Islander peoples for inclusion in the APJM tool was through use of the theoretical constructs [13, 29, 41] and engagement of the Aboriginal co-researchers who contributed to knowledge of how these could be applied. We found it was important for holistic philosophies and Indigenous knowledges [41] to be incorporated throughout the APJM tool. We also determined that the critical time points of burn care for families were less rigid points than those associated with biomedical burns care and were reflective of family needs.
The biomedical and cultural evidence was brought together at the knowledge interface, in order to take account different influences at different levels in complex health systems, all of which are interrelated and not independent of one another [29] and are especially important given factors informing burn care in Australia [Fraser]. We found that by developing the APJM tool at the knowledge interface, we were able to bring together, the experience of the recipient of care, the perspective of healthcare service, and the influence of the healthcare system in a manner which encompassed mutual respect, shared benefit, discovery, and dignity [29, 30, 41].
The compilation of this information into a single APJM tool was facilitated by use of a single spreadsheet file with two components: one to assess the provision of quality care compared with the biomedical evidence (Supplementary Material 1); and a second to record the burn care journey in-line with Aboriginal and Torres Strait Islander constructs of health and healing (Supplementary Material 2). A roundtable of researchers, clinicians and Aboriginal healthcare professionals critically refined the tool after which endorsement for application of the tool was sought.
Application of the APJM tool
The mapping process, through application of the APJM tool to investigate the quality of healthcare systems and services for burn care with Aboriginal and Torres Strait Islander families included two phases: recruitment, and data collection and analysis.
Recruitment
An outer metropolitan family was recruited to participate in the application of the APJM tool. The participant, an Aboriginal child whose family (n = 6) accessed tertiary burn care, was chosen from an overarching study investigating burn injury in Aboriginal and Torres Strait Islander children [27]. The role of the main researcher in applying the tool (author SF), was a PhD candidate, external to the tertiary healthcare site, yet linked to the site through their participation in the overarching study [27]. Clinicians identified through case note review and involved in the provision of care were also invited to participate.
Data collection and analysis
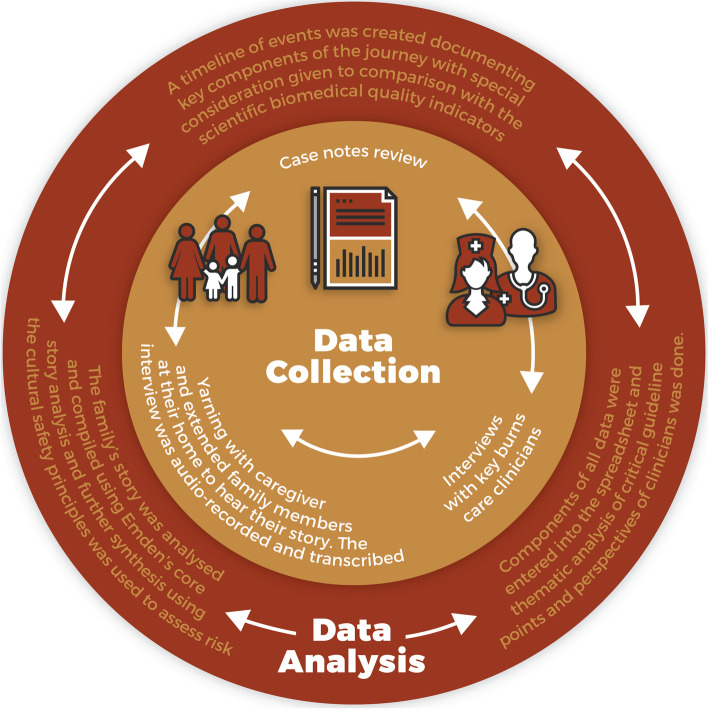
Data collection and analysis for the mapping process entailed four main stages, which were completed iteratively, but not sequentially (Fig. 1). These included yarning with the family, case note review, structured interviews with key burn care clinicians, and collaborative data analysis. In line with interface research [28, 29], Indigenous knowledges and understandings informed research yarning with authors TM and CR. Both of whom are Aboriginal woman and health researchers, linked closely through a cultural mentorship role to the main researcher (Author SF).
Fig. 1.
Data collection and data analysis mapping process
For the yarning with family, author SF was accompanied by author CR into the family’s home. Yarning [42] is an Indigenous cultural form of conversation and data gathering tool in research. This yarn was transcribed verbatim and analysis of this interview was through use of Emden’s core story analysis [26, 43] whereby a series of processes led to the creation of a de-identified core story that the participant confirmed for accuracy. This method of analysis provided a space to articulate the families’ journey holistically. These data were also analysed thematically using deductive methods [32] and input into the APJM tool spread sheets. Further synthesis of the yarning data provided the means to assess cultural safety and associated risk for the participating family. Consistent with the coming together of Indigenous and western knowledge, these processes contribute to reliability of data analysis and demonstrate our application of interface research.
The case note review and structured interviews with key burn care clinicians captured the quality components of the approaches to burn care, and the perspectives of healthcare providers. These data were also input into the APJM tool spreadsheets.
Results
Effectiveness of the modified APJM tool in identifying gaps in quality and cultural safety
Experience of the individual child and family
The APJM tool enabled the assessment of quality regarding the individual family’s experience of care in the healthcare system (Table 1). The family perceived that they experienced disrespectful care; they felt isolated and helpless during their child’s inpatient stay and vulnerable on discharge. The family also identified significant gaps relating to follow-up care and ease of access to rehabilitation. Synthesis of the yarning data (Supplementary Material 3) informed by the principles of cultural safety identified that care was most likely poorly experienced at the ‘sustained interface’ and ‘going home’ phase (Table 2). Such gaps in quality acknowledge the family’s experience of care as a result of fundamental differences in knowledge and understanding as reflected in the burn care health system.
Table 1.
Results of PJM tool Spreadsheet Two. Indigenous concepts of health and healing and family and healthcare professional perspectives
| Points in time—headings to elicit holistic views of health | Crisis | Getting help | Leaving competing obligations | Confronting the system | Sustained Interactions | Being away | Going home | Confronting competing needs |
|---|---|---|---|---|---|---|---|---|
| Caregiver's perspective | Accessible and appropriate care | Accessible and appropriate care | Care arranged for sibling and family contacted |
Identification question asked Felt scared and ignored Social worker provided support |
Communication was inconsistent Felt judged for not staying in the hospital Unable to work with subsequent extreme financial pressure and no access to disability pension Food vouchers infrequent and covered only very minimal amounts |
Difficult to find care for sibling Increased burden on extended family for sibling care and visiting hospital Sibling difficult behaviour Financial support to cover part of fuel costs to drive to hospital each day. No PATS. Home bills left unpaid |
Felt pushed out Discharged without confidence Psychological distress |
Financial support to cover part of fuel costs to drive to hospital each day. No PATS Unable to return to work for almost one year Long appointments that meant whole day trips Sustained burden on extended family for sibling care |
| Child's perspective (6yo or >) | N/A as child < 6yo | N/A as child < 6yo | N/A as child < 6yo | N/A as child < 6yo | N/A as child < 6yo | N/A as child < 6yo | N/A as child < 6yo | N/A as child < 6yo |
| Referring Hospital/GP | N/A |
Not able to speak to Ambulance worker Case Notes: identification question asked |
Case Notes: consideration for care of sibling documented | N/A | N/A | N/A | N/A | N/A |
| AHW | No AHW employed | No AHW employed | No AHW employed | No AHW employed | No AHW employed | No AHW employed | No AHW employed | No AHW employed |
| A/ILO | N/A | N/A | N/A | Not notified child was Aboriginal whilst in ED |
Supported family financially with fuel and food vouchers Helped with access to hospital child care for sibling |
Not resourced to provide support care outside of the hospital or to those family outside of the hospital environment | Arranged by burn team | Not resourced to provide support |
| Ngangkari (Traditional Healer) | Not requested by caregiver. ? availability | Not requested by caregiver. ? availability | Not requested by caregiver. ? availability | Not requested by caregiver. ? availability | Not requested by caregiver. ? availability | Not requested by caregiver. ? availability | Not requested by caregiver. ? availability | Not requested by caregiver. ? availability |
| Burn Nurse | N/A | N/A |
Notified via pager No support care provided |
Attended ED on arrival of family Spent time with caregiver Provided caregiver with clothes to change in to |
Time spent with caregiver M-F to ensure understanding Made caregiver feel comfortable with environment |
Encouraged accessing extended family for support with sibling |
Provided written instructions Gave some dressings |
Attempts to make dual appointments |
| Occupational Therapist | N/A | N/A | N/A | Automatic referral received | Care provided in ICU | Attempts to make dual appointments | Discharge advice given | Attempts to make dual appointments |
| Physiotherapist | N/A | N/A | N/A | Automatic referral received | Positioning in ICU | Attempts to make dual appointments | Discharge advice given | Seen in scar clinic |
| Surgeon (medical staff) | N/A | N/A | N/A | Case Notes: Informed consent and surgical procedures | Case Notes: Informed consent and surgical procedures. Allowed caregiver to give consent over the phone for second and subsequent procedures | Case Notes: noted caregiver seen by social worker | Case Notes: Medical review prior to discharge | Case Notes: Wound and scar review as necessary |
| Psychologist | N/A | N/A | N/A | Case Notes: no input into care | Case Notes: no input into care | Case Notes: no input into care | Case Notes: no input into care | Case Notes: no input into care |
| Social Worker | N/A | N/A | N/A |
Supported and sat with caregiver in ED Explained situation Explained presence of police officer and mandatory notifications |
Supported caregiver with social health and welling Ensured access to fuel and food vouchers |
Provide written evidence to support disability pension claim | Ensured access to fuel vouchers | Not resourced to provide support once discharged |
Table 2.
Yarning data synthesis of caregivers’ experience of culturally safe care and associated risk
| Cultural safety Principle | Definition | In-Practice examples | Caregiver’s experience at holistic time points and associated level of risk | ||||
|---|---|---|---|---|---|---|---|
| crisis | help | confront | sustain | home | |||
| Reflexivity | Reflect on practice, mutual respect | Respectful interactions | low | low | med | med | med |
| Dialogue | True engagement and consultation | Build rapport and dialogue with family alongside consideration of kinship arrangements and decision-making structures, particularly as they relate to children | low | low | med | med | med |
| Power imbalances | Minimise power differentials and maintain human dignity | Including Indigenous health workers in multidisciplinary teams | low | med | med | med | med |
| Decolonisation | Acknowledging the key role of colonising history in contemporary health outcomes for Aboriginal and Torres Strait Islander peoples | Ensuring equity in healthcare to achieve equity in health outcomes | low | med | med | high | high |
| Regardful care | Provide care that is regardful of culture and challenges the status quo of providing care that is regardless of culture | Patient-centred care; where the context for the child and their family drives care decisions | low | low | high | high | high |
Perspective of health care providers
Mapping data identified that healthcare providers were neither resourced nor supported to provide best care following patient discharge, and there were limited options for referral to community based social workers (Table 1). APJM also showed healthcare providers mostly conform to the evidence underpinning medical aspects of burn care. There was no Aboriginal Health Worker AHW employed at the site, nor was any input from a psychologist involved in the care (Table 3).
Table 3.
Results PJM tool Spreadsheet One. Scientific standards and family and healthcare providers meeting standards
| Burn care standards [30–32, 34, 35] | The injury | Emergency care | Ambulatory care | Admission | In-patient care | Discharge | Rehabilitation |
|---|---|---|---|---|---|---|---|
| Standards achieved by healthcare service and healthcare professionals |
⋅ 20 min cool running water within first 3 h ⋅ Remove jewellery and clothing ⋅ Cover with non-adherent dressing ⋅ Seek medical assistance ⋅ Keep warm ⋅ Provide access to basic online first aid training on burn injury to target the community ⋅ Ensure first aid courses contain burn first aid content |
⋅ Burns greater than 5% in children ⋅ Full Thickness burns greater than 5% ⋅ Burns of special areas ⋅ Burns in very young ⋅ Children up to their 16th birthday should be transferred to a children's burn unit ⋅ Metro clients access tertiary facilities directly, and outer regions require routine links to tertiary facilities ⋅ Access to specialist service |
⋅ Consult with a burn surgeon ⋅ Access to physiotherapy, · occupational therapy, social work, speech pathology, nutritional support, clinical psychology ⋅ Ambulatory burn clinic provides assessment and dressing of minor and non-severe burns, rehabilitation interventions, follow-up burn dressing and skin graft management for patients after discharge ⋅ long-term scar management and symptom control ⋅ patient and family teaching and support ⋅ ongoing complication risk management and treatment ⋅ advisory service to other hospitals, healthcare professionals and community |
⋅ Social worker undertakes thorough psychosocial assessment to review family history and address psychosocial issues in the acute phase ⋅ Accurate assessment undertaken in the ED in accordance with the admission guidelines for individual burn unit ⋅ Laser Doppler Imaging to assess depth ⋅ Rehabilitation starts on admission and whole patient and family are considered when addressing rehabilitation needs ⋅ Care plan is developed and documented and reviewed on a continual basis . Case management is commenced on admission ⋅ Allied health contributes to all stages of continuum of care guided by clinical practice guidelines ⋅ Nurses provide holistic care and are integral to patient care from point of admission to rehabilitation to ambulatory care ⋅ Multi-disciplinary teams coordinate individual clinical pathways ⋅ Each discipline contributes to treatment plan |
⋅ Social work and clinical psychology provide assessment and intervention ⋅ Dietician assessment for burns > 10%, < 1yo, burn to mouth/hands ⋅ Nursing staff work closely with comprehensive pain management service incorporating a range of modalities and including non-pharmacological and complementary therapies ⋅ Care plan incorporates rehabilitation throughout all stages of care starting at time of injury and family are considered when addressing rehabilitation needs ⋅ Major burn patients should be assessed within 24 h of admission by physiotherapy OR occupational therapy ⋅ Multidisciplinary plan of care · Allied health contributes to all stages of continuum of care guided by clinical practice guidelines ⋅ Multi-disciplinary teams coordinate individual clinical pathways ⋅ Receive multi-disciplinary inpatient care ⋅ Each discipline contributes to treatment plan ⋅ Burn injury team liaises with microbiology and infection control ⋅ The burn injury team works closely with the pharmacist in the management of care ⋅ State-wide e-health service supporting consultant-led on-call advisory service ⋅ Patients managed in ICU require coordination of wound care by burn care nurses ⋅ Access to pathology services ⋅ Nursing staff provide holistic care ⋅ 24 h access to operation rooms ⋅ Paediatric treatment rooms · Child protection unit involvement |
⋅ Pharmacist to provide regular information to child, family, carer on medication at admission and discharge ⋅ Allied health contributes to all stages of continuum of care guided by clinical practice guidelines ⋅ Social work and clinical psychology provide assessment and intervention ⋅ Address psychosocial issues, prior to discharge . Case management for complex cases continues throughout long-term care to facilitate periodic re-assessment and monitor changes in functionality ⋅ Patients to receive 'Nutrition for burns' pamphlet prior to discharge |
|
| Standards not achieved by healthcare service and healthcare professionals |
⋅ Provide 7 day/week ambulatory burn service co-located with acute inpatient burn unit ⋅ Burn injury patients have access to ‘hospital-in-the-home’ services post inpatient discharge |
⋅ Clinical psychology provides assessment and intervention at admission | ⋅ Comprehensive nursing care plan developed in consultation with patient and/or caregiver on admission to unit | ⋅ Facilitated early discharge by accessing ‘hospital-in-the-home’ services, and by using a step down to local non-tertiary hospital for transition to rehabilitation |
⋅ Use telehealth for ongoing post-acute care of burn patients ⋅ Rehabilitation team provides referral to external rehabilitation facilities for ongoing management ⋅ Be referred to OT/physio at local services where available, with support from burn unit therapists ⋅ Patients and families continue to receive psychosocial intervention and refer to other agencies where required |
||
| Standards not applicable for this burn care journey |
⋅ Inhalation, electrical, circumferential and chemical burns ⋅ Burns with illness ⋅ Burns with major trauma ⋅ Any burn where the referring worker requires management or advice from the paediatric burn service ⋅ Burn injury with suspicion of non-accidental injury ⋅ Appropriate communication and management instigated for interstate transfers within 4 h ⋅ The facility who has first contact with the burn injury contacts the unit for support and advice ⋅ For minor burns, communication with unit regardless of confidence in assessment and plan of care ⋅ For moderate burn, communicate with unit early and adopt recommended guidelines ⋅ Laser Doppler technology is used to assess depth ⋅ Initial assessment in ED where staff communicate with state unit, providing 24-h turnaround service via email images for clinical advice |
· accept patients referred from a hospital emergency department, general practitioners, other hospitals, community health services, or self-referred ⋅ burn injury of up to 10% of total body surface area may be managed on an ambulatory basis · Outpatient community care may include home, school, pre-school and workplace visits ⋅ Referral to dietician if deemed to be at nutritional risk; followed by nutritional assessment for social and cultural needs ⋅ Use of step-down facility to allow access to ambulatory care services for rural and remote families ⋅ patients with a burn who require surgery, with interim burn care until the day of surgery |
⋅ Emergency surgery within 24 h post-deep circumferential burn ⋅ Access to Burn Unit is dependent on post-assessment classification of the burn injury using E-health Outreach Service via non-specialist centres for regional/rural/remote |
⋅ Education teacher on daily basis ⋅ Psychosocial assessment focussing on the accident causing injury and family member’s perceptions around this, past experiences of trauma, family dynamics, cultural and socio-economic factors, barriers to coping and family strengths and supports ⋅ Long term access to psychological support |
⋅ Provide access to sub/acute/step-down facilities ⋅ Referral to community agencies for support at home if required |
||
| Standards unable to be assessed | ⋅ Staff attending burn patients in outpatient setting observe standard precautions at all times, including hand hygiene and aseptic non-touch technique and relevant PPE |
⋅ Step-down facilities are linked to acute services to achieve a seamless continuum of care ⋅ Provide access to burn camps for children ⋅ Contribute to cooperation between family and school ⋅ Visit school with burn team to educate |
|||||
| Data from Case Notes and discussions (where able) regarding how standards were/were not applied | |||||||
| Caregiver | Had completed first aid training | Accessed emergency ambulance care | Travelled in private car to appointments. From daily dressing to once every 6 weeks | Time in emergency department then transferred to ICU | Four days in ICU (and staying at home at nights) and four weeks in surgical unit (staying at home and sometimes in hospital) | Travelled home in private car. Felt hurried out and inadequately prepared to provide necessary at-home care | |
| Family | N/A | Contacted by phone after accident occurred | Travelled in private care with caregiver occasionally | Arrived at hospital after admission to ICU | Visited often in private car | ||
| Aboriginal Health Worker (AHW) | No AHW employed | No AHW employed | No AHW employed | No AHW employed | No AHW employed | No AHW employed | |
| ACCHS | Not accessed by the family | Not utilised by the family | Not accessed by the family | Not utilised by the family | Not utilised by the family | Not utilised by the family | |
| Emergency Care Provider | Not able to contact place of injury or those present at time of injury |
Not able to contact Ambulance worker Case Notes: Mandatory notifications made |
N/A | N/A | N/A | N/A | |
| Surgeon | N/A | N/A | Consults as necessary | Surgical assessment within 4 h of admission to hospital | Surgical intervention | Discharge note made | |
| Burn Nurse | N/A | N/A | Arranged care appointments and supported caregiver in minimising time spent in hospital | Support transition to ICU and then to ward. In regular contact with caregiver and giving constant information | Developed initial care plan. Led case conferences with medical staff. Involved multidisciplinary team. Reviewed at least daily |
Gave information regarding required care Arranged follow-up appointments |
|
| A/ILO | N/A | No support provision | Not notified | On A/ILO list. Seen and offered support. Did not attend case conferences | Seen prior to discharge and support offered | ||
| Traditional Healer | N/A | No traditional healer employed | No traditional healer employed | No traditional healer employed | No traditional healer employed | No traditional healer employed | |
| Occupational Therapist | N/A | N/A | Consults in scar clinic | Assessed within 8 h of admission |
In patient care provided. Attended case conference Input into care plan |
Discharge note made | |
| Physiotherapist | N/A | N/A | Consults in scar clinic | Assessed within 24 h of admission |
In patient care provided. Attended case conference Input into care plan |
Discharge note made | |
| Psychologist | N/A | No input into care. Not able to be contacted | No input into care. Not able to be contacted | No input into care. Not able to be contacted | No input into care. Not able to be contacted | No input into care. Not able to be contacted | |
| Social Worker | N/A | Attended ED. Supported, engaged and explained | No input into care | Able to provide support to caregiver and available for all level 1 trauma | Provided initial assessment of caregiver, supported, engaged and provided intervention where necessary and supported access to fuel and food vouchers. Attended case conference | Discharge note made | |
Assessment of the health system
The APJM tool was able to identify where there are gaps in the healthcare system regarding quality of burn care for Aboriginal and Torres Strait Islander children and families. Burn care was mostly delivered in line with the prescribed indicators of biomedical quality; e.g. first aid was given, burn specialist assessment was within the stipulated time-frame and multi-disciplinary care was provided. However, contribution by the Aboriginal/Indigenous liaison officer (A/ILO) was both late in the timeline of clinical care, and limited. Access to rehabilitation services outside of the tertiary healthcare environment was reduced and did not meet standards (Table 3).
Discussion
Implications of the APJM tool
The innovation in using the knowledge interface and Indigenous research methods, combined with the principles of cultural safety and guided specifically by the principle of reflexivity [44] as it relates to researchers and health care with Aboriginal and Torres Strait Islander people, enabled the implications of developing and applying the APJM to be considered. Engagement in reflexive practice provided a space to inform this process from a culturally safe and holistic health standpoint.
Through application of the APJM tool, we have shown feasibility of its use in the burn care journeys of Aboriginal and Torres Strait Islander families such that it enables an exploration of the multiple layers of experience in the health care system. This includes the system, service and individual with a holistic model. With the engagement of Indigenous knowledge, we have been able to capture gaps in quality that relate to more than biomedical quality evidence. This APJM research has shown that while complex disparities being experienced by Aboriginal and Torres Strait Islander children and families, quality is able to be explored thoroughly when using tools that address all aspects of quality. With these aspects considered, APJM is time intensive and challenging to engage clinicians.
Application of the APJM tool was undertaken over four months (approximately 120 h) in 2018. The tool was lengthy and could be reduced by the inclusion of only those standards specific to the jurisdiction where the tool is being used. Testing of the tool with regional/remote families and with older children is required. Recruitment and engagement of family members in mapping was enhanced by existing relationships with the mother. Having the grandparents present at the family interview contributed to a deeper understanding. The family interview was facilitated with an Aboriginal woman as a co-researcher, supporting ethical research. The interview was conducted in the family home, on the basis the family were more likely to feel secure in their own space, and dinner was supplied though study funds.
APJM for use in complex quality investigations
Results from this study show existing APJM tools [26] are able to be modified to investigate quality and cultural safety in burn care for Aboriginal and Torres Strait Islander children and families in a tertiary setting. Through application of the tool, new levels of understandings and recommendations for changes in practice which can alter the experience of those receiving the care were able to be identified. The implications of engaging an innovative approach through interface research show quality improvement is able to be considered from more than regulation or performance perspective. An exploration of complex disparities was enabled that incorporated patient experiences at the individual, service and system level. This study was limited due to being only one case with no control, and a similar study with a non-Indigenous family may have generated similar issues.
These findings confirm that retrospective data is useful in assessing healthcare quality in patient journeys, as well as interactions between various components of quality in this setting. The APJM tool enabled assessment of performance, regulatory constraints and patient experience in tandem. Analysis of these data, using Emden’s analysis method [43, 45] and thematic analysis [32] gave insight into the families’ journey of quality in burn care. The tool also gave burn healthcare providers the opportunity to externalise and reflect on their capabilities and the care they provide. As a result, use of APJM provided a space for healthcare providers to consider how to improve and innovate within their own practice through reflexivity. While existing professional relationships with the lead burns nurse made access to relevant clinicians more successful due to this nurse’s influence on facilitating clinician availability, it was sometimes difficult to engage busy clinicians with the mapping process when seeking to clarify and understand key points and interactions within the journey. This reflects the findings of the Managing Two World Together Project where clinician engagement was promoted by collaborative involvement in the research and development of tools, as compared with externally-developed tools imposed upon them [26]. Therefore provision of more information on the processes and aims of APJM may enhance participation by busy clinicians.
This preliminary analysis did not include responding to the findings to improve communication, reduce perceived differential treatment or enhance access to post-discharge care. Further considerations need to be made to determine how best to work with multidisciplinary burns teams and healthcare services to effectively plan and implement improvements in burn care for Aboriginal and Torres Strait Islander children and families. Existing QI frameworks and engagement in reflexivity by healthcare practitioners may be key aspects of future approaches, however there does exist opportunities for immediate QI considerations. This includes the employment of Aboriginal Liaison Officers as part of burn teams, appropriate resource allocations and increased focus on Aboriginal and Torres Strait Islander aspects to burn care in team meetings (clinical and research).
Conclusions
The APJM tool aims to facilitate the exploration of complex patient journeys following a burn injury, the increase in knowledge of what works well and what needs improvement in the healthcare system for Aboriginal and Torres Strait Islander children and families. Whilst many methods and methodological approaches to improve the quality and safety of healthcare exist, very few address the knowledge interface of Indigenous and western health knowledges, nor provide opportunity for children to have a voice. In undertaking this study, we have developed a tool enabling research of burn care quality at the knowledge interface, with explicit consideration of more holistic, fluid and culturally safe models of healthcare.
Supplementary Information
Acknowledgements
We acknowledge the Aboriginal people and communities who were part of this research and contributed to author SF’s learnings in this area. In particular we acknowledge the family who shared their story and the clinicians who participated in the application of the APJM tool presented here.
Abbreviations
- ILO
Indigenous Liaison Officer
- ALO
Aboriginal Liaison Officer
- APJM
Aboriginal Patient Journey Mapping
- QI
Quality Improvement
Authors’ contributions
SF designed the study in conjunction with TM, JG, KH and RI. TM and CR mentored SF throughout the project and provided input into project design, data collection and data analysis. SF and CR collected the data and analysed it in conjunction with all other authors. SF, TM, JG, KH, CR and RI contributed to the review of the literature that informed the paper. JK, AH, BG, KC, WT and AD all provided specific technical advice in developing the tool. SF and TM wrote the first draft of the manuscript and all authors read and approved the manuscript.
Funding
The project is funded by the National Health and Medical Research Council of Australia (grant number APP1059038). Author KH is supported by a NSW Health Early Mid-Career Fellowship. The researchers were independent from the funder.
Availability of data and materials
The datasets generated during and/or analysed during the study are not publicly available due to ethical restrictions but may be available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Aboriginal Health Research Ethics Committee 04–14-572; Women’s & Children’s Health Network Human Research Ethics Committee HREC/14/WCH/65; Flinders University SBREC Project OH-00065; Northern Territory. Central Australian Human Research Ethics Committee HREC-14–253. Human Research Ethics Committee of Northern Territory Department of Health and Menzies School of Health 2014–2214; National. Department of Health Human Research Ethics Committee 39/2014. All methods were performed in accordance with the NHMRC 2018 National Statement on Ethical Conduct in Human Research and participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sarah Fraser, Email: sarah.fraser@unsw.edu.au.
Tamara Mackean, Email: tamara.mackean@flinders.edu.au.
Julian Grant, Email: jugrant@csu.edu.au.
Kate Hunter, Email: khunter@georgeinstitute.org.au.
Courtney Ryder, Email: courtney.ryder@flinders.edu.au.
Janet Kelly, Email: janet.kelly@adelaide.edu.au.
Andrew J. A. Holland, Email: andrew.holland@health.nsw.gov.au
Bronwyn Griffin, Email: bronwyn.griffin@griffith.edu.au.
Kathleen Clapham, Email: kclapham@uow.edu.au.
Warwick J. Teague, Email: warwick.teague@rch.org.au
Anne Darton, Email: anne.darton@health.nsw.gov.au.
Rebecca Q. Ivers, Email: rebecca.ivers@unsw.edu.au
References
- 1.Hayes CW, Batalden PB, Goldmann D. A ‘work smarter, not harder’ approach to improving healthcare quality. BMJ Qual Saf. 2015;24(2):100–102. doi: 10.1136/bmjqs-2014-003673. [DOI] [PubMed] [Google Scholar]
- 2.The Australian Council on Healthcare Standards. Available from: https://www.achs.org.au/.
- 3.Ben-Tovim DI, et al. Patient journeys: the process of clinical redesign. Med J Aust. 2008;188(S6):S14–S17. doi: 10.5694/j.1326-5377.2008.tb01668.x. [DOI] [PubMed] [Google Scholar]
- 4.Johnson JK, et al. Searching for the missing pieces between the hospital and primary care: mapping the patient process during care transitions. BMJ Qual Saf. 2012;21(Suppl 1):i97–i105. doi: 10.1136/bmjqs-2012-001215. [DOI] [PubMed] [Google Scholar]
- 5.Laverty M, McDermott DR, Calma T. Embedding cultural safety in Australia’s main health care standards. Med J Aust. 2017;207(1):15–16. doi: 10.5694/mja17.00328. [DOI] [PubMed] [Google Scholar]
- 6.Bainbridge, R., et al., Cultural competency in the delivery of health services for Indigenous people. 2015.
- 7.Commonwealth of Australia, National Aboriginal and Torres Strait Islander Health Plan 2013 -2023. 2013.
- 8.Australian Commission on Safety and Quality in Health Care, The National Safety and Quality Health Service Standards, 2nd Edition, 2017: Sydney.
- 9.Taylor, K., and Guerin, P., Health care and Indigenous Australians: cultural safety in practice, 2nd edition. 2014, Australia: Macmillan Education.
- 10.Best, O. and B. Fredericks, Yatdjuligin: Aboriginal and Torres Strait Islander nursing and midwifery care. 2017: Cambridge University Press.
- 11.Australian Commission on Safety and Quality in Healthcare, Australian Safety and Quality Framework for Health Care 2010.
- 12.Australian Indigenous Doctors’ Association and Centre for Health Equity Training Research and Evaluation, Health Impact Assessment of the Northern Territory Emergency Response. Canberra: Australian Indigenous Doctors’ Association, 2010.
- 13.Ramsden, I., Cultural safety and nursing education in Aotearoa and Te Waipounamu. 2002, Victoria University of Wellington Wellington.
- 14.Fraser S, et al. Burn injury models of care: a review of quality and cultural safety for care of Indigenous children. Burns. 2018;44(3):665–677. doi: 10.1016/j.burns.2017.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Mackean, T., et al., A framework to assess cultural safety in Australian public policy. Health Promotion International, 2019. [DOI] [PubMed]
- 16.Ryder C, Mackean T, Ullah S, Burton H, Halls H, McDermott D, Edmondson W. Development and validation of a questionnaire to measure attitude change in health professionals after completion of an Aboriginal health and cultural safety training Programme. The Australian Journal of Indigenous Education. 2019;48(1):24–38. doi: 10.1017/jie.2017.37. [DOI] [Google Scholar]
- 17.Dwyer J, et al. Equitable care for indigenous people: Every health service can do it. Asia Pacific Journal of Health Management. 2016;11(3):11. doi: 10.24083/apjhm.v11i3.143. [DOI] [Google Scholar]
- 18.Cunningham J. Diagnostic and therapeutic procedures among Australian hospital patients identified as Indigenous. Med J Aust. 2002;176(2):58–62. doi: 10.5694/j.1326-5377.2002.tb04284.x. [DOI] [PubMed] [Google Scholar]
- 19.Paradies Y. Racism and Indigenous Health. Oxford University Press; 2018.
- 20.Larson A, et al. It's enough to make you sick: the impact of racism on the health of Aboriginal Australians. Aust N Z J Public Health. 2007;31(4):322–329. doi: 10.1111/j.1753-6405.2007.00079.x. [DOI] [PubMed] [Google Scholar]
- 21.Artuso S, et al. Factors influencing health care utilisation among Aboriginal cardiac patients in central Australia: a qualitative study. BMC Health Serv Res. 2013;13(1):83. doi: 10.1186/1472-6963-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ryder C, Mackean T, Hunter K, Towers K, Rogers K, Holland AJA, et al. Factors contributing to longer length of stay in Aboriginal and Torres Strait Islander children hospitalised for burn injury. Inj Epidemiol. 2020;7(1):52. doi: 10.1186/s40621-020-00278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Burn Association. Burn Center Verification. Available from: http://ameriburn.org/quality-care/verification/.
- 24.McCarthy S, et al. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decis Syst. 2016;25(sup1):354–368. doi: 10.1080/12460125.2016.1187394. [DOI] [Google Scholar]
- 25.Kelly J, et al. Bottling knowledge and sharing it - using patient journey mapping to build evidence and improve Aboriginal renal patient care. Renal Society of Australasia Journal. 2016;12(2):48–55. [Google Scholar]
- 26.Kelly J, et al. Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care. Aust J Prim Health. 2017;23:536–542. doi: 10.1071/PY16069. [DOI] [PubMed] [Google Scholar]
- 27.Ivers RQ, et al. Understanding burn injuries in Aboriginal and Torres Strait Islander children: protocol for a prospective cohort study. BMJ Open. 2015;5(10):e009826. doi: 10.1136/bmjopen-2015-009826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Durie M. Indigenous knowledge within a global knowledge system. High Educ Pol. 2005;18(3):301–312. doi: 10.1057/palgrave.hep.8300092. [DOI] [Google Scholar]
- 29.Durie M. Understanding health and illness: research at the interface between science and indigenous knowledge. Int J Epidemiol. 2004;33(5):1138–1143. doi: 10.1093/ije/dyh250. [DOI] [PubMed] [Google Scholar]
- 30.Ryder C, Mackean T, Coombs J, Williams H, Hunter K, Holland AJ, et al. Indigenous research methodology–weaving a research interface. Int J Soc Res Methodol. 2020;23(3):255–267. doi: 10.1080/13645579.2019.1669923. [DOI] [Google Scholar]
- 31.Pyrch, T. and M.T. Castillo, The sights and sounds of indigenous knowledge. Handbook of action research: Participative inquiry and practice, 2001: p. 379–385.
- 32.Patton MQ. Qualitative evaluation and research methods. United States of America: SAGE Publications inc.; 2014. [Google Scholar]
- 33.Martin KL, Mirraboopa B. Ways of knowing, being and doing: A theoretical framework and methods for indigenous and indigenist re-search. Journal of Australian Studies. 2003;27(76):203–214. doi: 10.1080/14443050309387838. [DOI] [Google Scholar]
- 34.Kim LK, Martin HC, Holland AJ. Medical management of paediatric burn injuries: best practice. J Paediatr Child Health. 2012;48(4):290–295. doi: 10.1111/j.1440-1754.2011.02128.x. [DOI] [PubMed] [Google Scholar]
- 35.D'cruz R, Martin HC, Holland AJ. Medical management of paediatric burn injuries: Best practice part 2. J Paediatr Child Health. 2013;49(9):E397–E404. doi: 10.1111/jpc.12179. [DOI] [PubMed] [Google Scholar]
- 36.Women's and Children's Hospital Paediatric Burns Service, Women's and Children's Hospital Paediatric Burns Service Guidelines, Women's and Children's Hospital Paediatric Burns Service, Editor. 2014.
- 37.Department of Health Western Australia, Burn Injury Model of Care. Perth: Health Networks Branch, Department of Health Western Australia, Editor. 2009.
- 38.Agency for Clinical Innovation, Model of Care NSW Statewide Burn Injury Service, Agency for Clinical Innovation, Editor. 2011.
- 39.Australian & New Zealand Burns Association. ANZBA Referral Criteria. Available from: http://anzba.org.au/care/referral-criteria/.
- 40.Australian & New Zealand Burns Association. First Aid. Available from: https://anzba.org.au/care/first-aid/
- 41.Milroy, H., Children are our future: Understanding the needs of aboriginal children and their families, in Infants of Parents with Mental Illness : Developmental, Clinical, Cultural and Personal Perspectives. 2008, Australian Academic. p. 121–140.
- 42.Bessarab D, Ng'andu B. Yarning about yarning as a legitimate method in Indigenous research. International Journal of Critical Indigenous Studies. 2010;3(1):37–50. doi: 10.5204/ijcis.v3i1.57. [DOI] [Google Scholar]
- 43.Emden C. Conducting a narrative analysis. Collegian. 1998;5(3):34–39. doi: 10.1016/S1322-7696(08)60299-1. [DOI] [PubMed] [Google Scholar]
- 44.Wilson, A., Addressing Uncomfortable Issues: Reflexivity as a Tool for Culturally Safe Practice in Aboriginal and Torres Strait Islander Health, 2014, The Australian Journal of Indigenous Education, Volume 43 Issue 2, DOI: 10.1017/jie.2014.24.
- 45.Kelly, J., et al., Managing two worlds together: Stage 2-patient journey mapping tools. 2012.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analysed during the study are not publicly available due to ethical restrictions but may be available from the corresponding author on reasonable request.