Abstract
Links between global levels of maternal depressive symptoms and parenting behavior in early childhood are well established. However, depression is a heterogenous disorder and little is known about how individual differences in depression symptoms may be differentially associated with different types of parenting behavior. We aimed to uncover nuance in the relationship between depression and parenting behavior by examining individual differences in symptoms of maternal depression and associations with parenting behavior with 2- and 3-year-old children. Participants included 714 diverse, low-income mothers and their 2-year-old children. Maternal depression symptoms were self-reported at child age 2. Three domains of parenting behavior (harsh, positive, and disengaged) were coded from mother-child interactions at ages 2 and 3. Individual differences in maternal depressive symptoms at child age 2 comprised five profiles: Low, Interpersonal Rejection, Moderate, High Depressed Affect and Physical, and Severe. Women with the High Depressed Affect and Physical profile demonstrated the greatest risk for parenting challenges with higher levels of harsh parenting at child age 2 compared to all other profiles and higher levels of disengaged parenting at child age 3 compared to the Low, Moderate, and Severe profiles. Unexpectedly, positive parenting did not differ by maternal depression profile at either age. There is wide heterogeneity in symptoms of depression among mothers of 2-year-old children that is clinically relevant for different dimensions of parenting. Physical and depressed affect symptoms in particular may present risk for harsh parenting.
Keywords: Maternal depression, individual differences, parenting, toddlers
Introduction
Symptoms of depression among mothers have long been associated with parenting behaviors detrimental to child well-being, including reduced sensitivity, responsiveness, and engagement, as well as increased harshness and rigidity (Albright & Tamis-LeMonda, 2002; Goodman & Garber, 2017; Lovejoy et al., 2000; Paulson et al., 2006). However, much of the research on depression and parenting is variable-centered, focused on a total count of symptoms, total symptom severity, and/or meeting diagnostic criteria for depression. Variable-centered approaches ignore potential individual differences in symptom presentations, which are particularly important to explore with heterogeneous diagnoses like depression. Conversely, person-centered approaches characterize heterogeneity within a construct, thus highlighting individual differences. Using a person-centered approach to study associations between maternal depression and parenting behavior is an innovative way to assess whether individual differences in symptoms of depression are related to specific dimensions of parenting behavior. Such knowledge could advance our understanding about which clusters of depressive symptoms are most strongly associated with detrimental parenting behaviors.
Individual differences in depression symptoms
There are nine possible symptoms in the diagnostic criteria for major depressive disorder in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013), with three of the symptoms including two different presentations (e.g., appetite has either increased or decreased). Only five of the nine symptoms are required to qualify for a diagnosis of depression. Therefore, there are more than 1,400 possible combinations of symptoms inherent in a diagnosis of depression (Østergaard et al., 2011), which highlights the vast potential for heterogeneity in presentations of depression. Furthermore, many individuals have subthreshold levels of depressive symptoms (i.e., fewer than 5 symptoms), which also have been linked to adverse impacts on parent and child well-being (Conners-Burrow et al., 2016; Lovejoy et al., 2000; Vieites & Reeb-Sutherland, 2017; Weinberg et al., 2001). There is need for greater precision in our understanding of associations between depression and parenting behavior.
A recent systematic review, which included 24 articles published over the past 30 years, highlighted the heterogeneity of symptoms of depression in studies that examined latent profiles of depression using latent-class analysis (LCA) (Ulbricht et al., 2018). LCA is a person-centered statistical technique for identifying heterogeneity within a construct when the latent class indicators are binary (e.g., symptom present or absent). The number of profiles extracted varied from 2 to 7. Profiles based on symptom severity (e.g., low or mild severity, high severity, non-depressed, severely depressed) were the most common. Content-specific profiles were also identified and labeled based on the types of symptoms with elevations (e.g., somatic, cognitive, atypical, melancholic).
Pertinent to the present study, a handful of studies have examined individual differences in symptoms of depression assessed by the CES-D using latent profile analysis (LPA). LPA is a person-centered statistical technique for examining heterogeneity in a construct when latent profile indicators are continuous or non-binary, like the items of the CES-D. A majority of the profiles of depression symptoms on the CES-D in past work have been based on symptom severity (Gaston et al., 2016; Hybels et al., 2011; Saracino et al., 2018), with just one study also identifying profiles based on symptom content (subthreshold symptoms with anhedonia and subthreshold symptoms with anhedonia and negative interpersonal feelings; Mora et al., 2012). Thus, there is a large literature on individual differences in symptoms of depression and profiles of depression symptoms using the CES-D. However, no prior studies investigating heterogeneity in depression symptoms have linked profiles of depressive symptoms to parenting behavior.
Individual differences in depression symptoms and associations with parenting
Past variable-centered research is consistent in linking total symptom counts, severity, or presence of a diagnosis to decreased positive parenting behavior and increased negative/intrusive and unresponsive/withdrawn types of parenting behavior (the three domains of focus in the present study). Past variable-centered work, using total CES-D scores, highlighted associations between greater depression severity and reduced engagement, affection, enrichment, and dyadic reciprocity, and increased rigidity (Albright & Tamis-LeMonda, 2002; Paulson et al., 2006). Theoretically, symptoms of depression lead mothers to be self-focused on their own internal emotions and less focused on their child’s needs, and thus struggle to understand and follow through on their children’s cues (i.e., appear withdrawn) or become agitated, leading to harsh or highly directive interactions with their children (DeJong et al., 2016). However, links between maternal depression and parenting behavior consider depression globally, glossing over the known heterogeneity in depressive symptoms and how specific combinations of symptoms may be linked to parenting behavior in different ways.
Despite the lack of person-centered empirical work on associations between depression and parenting behavior, there is reason to believe there could be individual differences in the ways in which combinations of depressive symptoms are associated with different types of parenting behavior. Past variable-centered work with the CES-D indicated symptom clusters of somatic symptoms, depressed affect, and interpersonal symptoms. We are interested in understanding how different clusters of depressive symptoms are associated with three established dimensions of parenting that are most often explored in relation to symptoms of maternal depression in the literature: harshness, positivity, and disengagement. It is important to note that the linking of individual differences in symptoms of depression to domains of parenting behavior is a novel area of study, thus the following sections are based on a limited amount of available theoretical and empirical work on these associations.
Components of depression: Physical symptoms.
Women reporting high levels of somatic symptoms on the CES-D endorse difficulties with sleeping and eating, low energy, difficulty getting going, and increased agitation (Radloff, 1977). Despite the lack of empirical and theoretical work on associations between specific types of symptoms of depression and parenting behavior, there is support for the premise that some individuals who are depressed show high levels of physical symptoms of depression.
Furthermore, some empirical work has linked physical symptoms associated with depression, such as fatigue and chronic pain, with higher levels of harsh, hostile, or over-reactive parenting behavior and lower levels of parental involvement and engagement (Evans et al., 2006; Giallo et al., 2011a). Another study demonstrated that high levels of depressive symptoms coupled with high levels of physical symptoms are associated with risk for child physical maltreatment and high levels of conflict in co-parenting relationships (Lamela et al., 2017). Conceptually, in interactions with their children, individuals with high levels of physical symptoms of depression may be distracted by internal symptoms and/or lethargic with little energy to engage with their children, and thus may be less attentive or aware of child cues and demonstrate low levels of parent-child engagement. Furthermore, agitation associated with physical symptoms of depression may result in harsh parent-child interactions.
Components of depression: Depressed affect.
Women reporting high levels of depressed affect symptoms on the CES-D might experience loneliness, helplessness, and frequent crying. In relation to parenting, drawing inferring from Seligman’s (1974) learned helplessness theory and its application to depression, mothers with feelings of helplessness may be withdrawn and lack confidence in their ability to effect positive change on their children or successfully manage difficult child behavior. Therefore, the parenting domains most comprised by high depressed affect are likely to be positive parenting and disengaged parenting, which require parents to not only be actively attuned to their child but confident in their ability to encourage and support their child in play and everyday activities with enthusiasm and encouragement. In a study of mothers of children with attention-deficit/hyperactivity disorder, maternal external locus of control mediated the relation between maternal symptoms of depression and self-reported lax/disengaged parenting behavior (Gerdes et al., 2007). The authors posited that helplessness in the form of external locus of control may lead mothers to feel unable to effectively manage their child’s misbehavior, resulting in a lack of engagement. It is plausible that feelings of helplessness may also lead to reduced levels of parenting behaviors such as praise and encouragement as a result of increased laxness and disengagement. Furthermore, outside the context of depression, mothers of children with conduct disorder who attributed their child’s misbehavior to external causes outside of their own control reported feeling ineffective as parents (Baden & Howe, 1992). Thus, symptoms of depressed affect, particularly helplessness, may be related to higher disengaged parenting and lower positive parenting.
Components of depression: Interpersonal difficulties.
Finally, women reporting elevated levels of interpersonal symptoms of depression on the CES-D endorse that others dislike them and are unfriendly to them. While depression-related social difficulties reflect adult-adult interactions, such dynamics may extend to parent-child relationships. Empirical evidence of the association between interpersonal symptoms of depression and parenting behavior is lacking; however, hypotheses regarding association between depressive symptoms and parenting can be drawn from the theoretical and empirical literature on depression, social support, and parenting behavior. In Belsky’s (1984) multi-determinant model of parenting behavior, social support is a key factor in supporting parenting practices. Accordingly, several studies report links between high levels of social support and higher positive parenting behavior and lower negative parenting behavior (Ceballo & McLoyd, 2002; Crnic & Greenberg, 1990; Hashima & Amato, 1994; Jennings et al., 1991; Lee et al., 2009; Simons et al., 1993). Specific to the context of depression, low levels of social support predict higher levels of depressive symptoms, which in turn predict higher self-reported over-reactive parenting behavior and frustration in the parent-child relationship in a rural, low income sample (Lee et al., 2009). The extensive past body of work on depression and interpersonal functioning is further supported by the well-supported efficacy in interpersonal psychotherapy in the treatment of depression (Cuijpers et al., 2011; Weissman et al., 2008). Therefore, parenting behaviors associated with a profile of elevated interpersonal symptoms of depression might include low levels of positive parenting and high levels of harshness in parent-child interactions.
In sum, although decades of variable-centered research has demonstrated that depression compromises parenting quality, understanding whether individual differences in depression at the cluster (rather than diagnostic) level are associated with specific dimensions of parenting could identify more personalized targets for intervention. Personalized targets could lead to greater engagement in services, and improve wellbeing for parents and children. Further, focusing on early childhood is important because associations between maternal depression and later child outcomes are strongest during early childhood (Goodman et al., 2011; Lovejoy et al., 2000), at least in part because of children’s greater psychological and physical dependence on caregivers during early childhood relative to later ages.
The Present Study
Using LPA, we examined associations between individual differences in depression symptoms and three domains of parenting behavior: harshness, positivity, and disengagement. We expected to identify heterogeneity in depression symptoms captured by profiles based on both symptom severity (e.g., low severity and high severity) and symptom content (e.g., physical symptoms, depressed affect, interpersonal). Based on previous variable-centered research, we expected to identify a profile depicting high severity across all symptoms of depression and such a profile to be associated with higher scores on composites of harshness and disengagement. Similarly, we expected to see lower scores on positive parenting compared to a profile depicting low severity of depression symptoms. We also expected to identify content-specific profiles depicted by differing levels across the clusters of physical, depressed affect, and interpersonal symptoms. Based on theoretical and empirical work reviewed above, we hypothesized that a profile with high physical symptoms of depression would be associated with high levels of disengagement and harshness in parent-child interactions. Second, we hypothesized that the parenting domains most comprised by high depressed affect would be positive and disengaged parenting. Finally, we hypothesized that elevated interpersonal symptoms of depression would be related to low levels of positive parenting and high levels of harsh parenting. In exploratory analyses, we examined prospective associations between profiles of depressive symptoms at child age 2 and parenting at child age 3 (controlling for total depression symptoms score at age 3) to test whether depressive symptom profiles continued to predict parenting longitudinally.
Method
Participants and Procedures
Participants were drawn from the Early Steps Multisite Study (Dishion et al., 2008), a randomized controlled intervention trial of 731 families recruited from centers for the Special Supplemental Nutrition Program for Women Infants and Children in and around Pittsburgh, PA (37% of families), Eugene, OR (37%), and Charlottesville, VA (26%) between 2002 and 2003. Children and their primary caregivers (primarily female and biological mothers) were recruited when children were between 2 years 0 months and 2 years 11 months old based on scores across categories of sociodemographic risk (e.g., poverty, teen parent status), family risk (e.g., depressive symptoms, substance use), and child risk (i.e., conduct problems, parent-child conflict). Eligible families met established clinical cut points or were at least one standard deviation above the normative mean in two of the three categories.
In the present study, only female primary caregivers (N=714) were included in the analyses because of the small number of male primary caregivers (2%, n=17) at the child age 2-year assessment and to aid in generalization of findings to a more narrowly defined population (i.e., female caregivers1). At the child age 2-year assessment, mothers were 27.2 years old on average (SD=7.1 years). The mothers and children included in the present study were racially and ethnically diverse, with mothers belonging to the following racial groups: 28.3% African American, 54.5% Caucasian, 14.7% Biracial, and 2.4% other races (e.g., American Indian, Native Hawaiian). The children belonged to the following racial groups: 28.1% African American, 49.9% Caucasian, 13.2% Biracial, and 8.8% other races (e.g., American Indian, Native Hawaiian). In terms of ethnicity, 10.9% of mothers and 13.8% of children in the sample were Hispanic or Latino. Approximately two-thirds of the sample had an annual income under $20,000 at recruitment. Forty-three percent of primary caregivers lived with their child’s biological father; thirty-one percent were single parents. Half (49.9%) of children were female, and were a mean age of 28.2 months (SD = 3.3) at the time of the first assessment.
At child age 2, families completed a 2.5-hour home assessment comprising questionnaires and caregiver-child interactive tasks2. At the end of the assessment, a subset of families was randomly assigned to participate in the Family Check-Up (FCU) intervention. Intervention status was not a focus of the present study and was included as a covariate in analyses that involved data from the child age 3 assessment, after the intervention began. Ethical approval was granted by the Institutional Review Board at each of the three study sites, and consent was obtained at each annual assessment from the primary caregiver.
Measures
Depression symptoms.
Maternal symptoms of depression were assessed at child ages 2- and 3-years using the Center for Epidemiological Studies on Depression Scale (CES-D; Radloff, 1977). The CES-D in an established, widely used measure of depression symptoms. Reliability and validity of the CES-D are well established (Radloff, 1977). Twenty items assess a broad range of symptoms of depression and other related symptoms across 4 domains: Depressed affect (5 items), positive affect (4 items), interpersonal (2 items), and somatic3 (5 items). Additional information about the content of the items within each domain is presented in Figure 1. The four remaining items assess symptoms not included on the domains (e.g., trouble keeping one’s mind on what they were doing) but included in the total score. A total score is created by summing all items (with the positive affect items reverse scored) where higher scores indicate high severity of symptoms. Each item is rated on frequency-based scale covering the past week that ranges from 0 (less than a day) to 3 (5–7 days). Total scores range from 0 to 60. The cutoff score for clinical depression based on the CES-D is 16, while the mean for primary caregivers in this sample at study entry was 16.75 (SD = 10.66), indicating that this sample was experiencing moderate to severe depressive symptoms. In the present study, a total score was used to briefly examine variable-centered associations. For person-centered analyses (LPA), all 20 items were used with the positive items reverse scored. The CES-D demonstrated internal consistency in the current sample (α = .88). We use the term “symptoms of depression” throughout to refer to symptoms assessed on the CES-D, but note that the symptoms assessed are broader than the core symptoms of depression and a high score on the CES-D does not indicate a diagnosis of depression.
Figure 1.
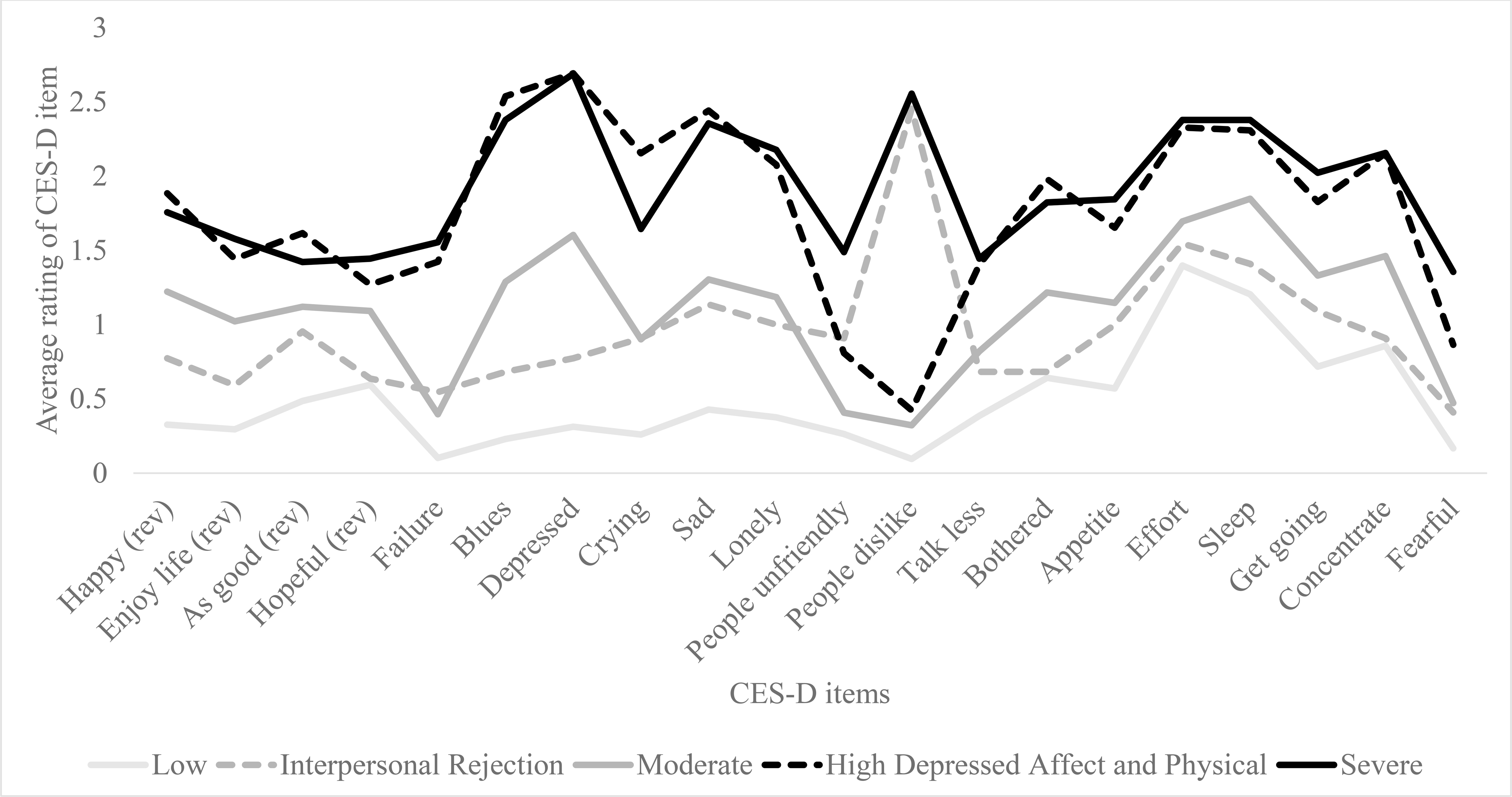
5-profile conditional model of depression symptoms. CES-D=Center for Epidemiological Studies on Depression Scale (CES-D; Radloff, 1977). (rev)=reverse scored item. Positive affect items include Happy, Enjoy life, As good, and Hopeful. Depressed affect items include Blues, Depressed, Crying, Sad, and Lonely. Interpersonal items include People unfriendly and People dislike. Physical items include Bothered, Appetite, Effort, Sleep, and Get going. The items Failure, Talk less, Concentrate, and Fearful do not belong to a subscale on the CES-D but are included in the total score.
Harsh parenting.
Observed maternal harsh parenting was derived from videotaped parent-child interactions at the child ages 2 and 3 home assessments. A composite index of harsh parenting was created using five items from the coder impressions (COIMP) inventory, a macro-social rating scale (Dishion, Hogansen, Winter, & Jabson, 2004) and three duration proportions from the Relationship Process Code (RPC; Jabson, Dishion, Gardner, & Burton, 2004). Intercoder reliability for the COIMP was calculated by having multiple coders re-code a random subset of tapes (15%). Coder agreement was 87% and 84% at ages 2 and 3, respectively. The specific COIMP items used to create the harsh parenting composite included primary caregivers’ displays of anger or annoyance with the child, criticizing or blaming the child for family problems, use of physical discipline, ignoring/rejecting the child, and messages about the child’s worthlessness Moilanen et al., 2010). RPC codes included duration proportions of parental negative verbal, directive, and physical behavior directed toward the child. Inter-coder reliability for the RPC was 87% agreement at age 2 (kappa = .86) and 86% agreement at age 3 (kappa = .86). These 8 items (5 from COIMP, 3 from RPC) were standardized and summed to create the harsh parenting composite (age 2, α = .75; age 3, α = .75).
Positive parenting.
Observed maternal positive parenting was derived from the same age 2 and age 3 videotaped parent-child interactions used to create the harsh parenting variable. The present study used the positive behavior support (PBS) composite, as described in Waller (et al., 2015), to capture positive parenting behavior. The PBS composite included 3 different observational strategies at child ages 2 and 3: the IT-HOME, the RACS, and the COIMP. A modified version of the IT-HOME (infant/toddler home observation for measurement of the environment; Bradley & Caldwell, 1984) was completed by home visitors during the age 2 and 3 assessments. Thirteen IT-HOME items with satisfactory internal reliability (age 2, α = .73; age 3, α = .76) were used in the PBS composite, including ratings of maternal responsivity, acceptance, child involvement, social skills, and ratings of the home environment. RACS (relationship affect coding system; Peterson, Winter, Jabson, & Dishion, 2008) coding was completed by a team of undergraduates blind to child and family data, using videotapes of the parent-child interactions. The RACS is a micro-social coding system that captures the topography (verbal and physical behaviors) and affect (anger/disgust, validation, distress, positive affect, and ignore) within relationship behaviors. Reliability coefficients for RACS coding were sufficient at both ages. Intercoder agreement on the subset (15%) of randomly selected re-coded videos was 72% at age 2 (kappa = .68) and 94% at age 3 (kappa = .93). The durations of positive and neutral engagement between caregiver and child were included in the PBS variable. Finally, COIMP items (described in the harsh parenting section, above) used in the PBS variable included proactive parenting, structuring of the child’s environment, parental warmth, positive parental reinforcement through praise, and displays of affection. The PBS composite demonstrated reliability at both ages (age 2, α = .85; age 3, α = .84).
Disengaged parenting.
Disengaged parenting was also based on observations of parent-child interactions at ages 2 and 3. The disengaged parenting behavior composite was created for the purposes of the present study, using the RACS, as described in the positive parenting section, above (Jabson, Dishion, Gardner, & Burton, 2004). The disengaged parenting composite included the duration proportions of 3 items: 1) “No talk,” which reflected time the caregiver did not speak, 2) “Ignore,” which reflected times in which the caregiver ignored child bids, and 3) “Non-engagement,” which reflected times in which the dyad was not engaged with each other Internal consistency for the disengaged parenting composite was α = .54.
Sociodemographic characteristics and other covariates.
Dummy codes for study site and an ordinal monthly income variable were included as covariates in the latent profile analysis. Total depression symptom score on the CES-D at age 3 was used as a covariate in longitudinal analyses. Longitudinal analyses also included intervention status as a covariate since the intervention was initiated after the age 2 assessment.
Data analysis
Prior to analyses, descriptive statistics for major study variables were examined with model assumptions in mind (see Supplemental table 1). Unconditional models (i.e., without covariates) were tested to establish the presence of heterogeneity in depression symptoms. Next, income and study site were evaluated as covariates to include in conditional models. Model fit was evaluated using empirically supported fit indices (e.g., Nylund, Asparouhov, & Muthén, 2007) including the Bootstrap Likelihood Ration Test (BLRT), Bayesian Information Criteria (BIC), and Akaike Information Criteria (AIC). Statistically significant (p < .05) BLRT tests and lower BIC and AIC values indicate good model fit. Indices of model classification quality (entropy and posterior probabilities) and interpretability were also considered. All LPA analyses were completed in Mplus.
We first tested variable-centered associations between depression (CES-D total score) and parenting behavior using bivariate correlations. Associations between profiles of maternal depression and differences in parenting behavior composites at ages 2 and 3 were analyzed in SPSS using general linear models. Longitudinal models predicting parenting at age 3 included intervention status as a predictor and parenting at age 2 and total depression at age 3 as covariates. Based on the small size of some profiles (e.g., n = 22 – 45), in addition to reporting traditional indices of statistical significance, we also reported effect sizes using Cohen’s d. Cohen’s d values 0.40 and greater will be recognized as statistically meaningful group differences and interpreted in the results. This study was not preregistered, and materials and data are not publicly available.
Results
Unconditional latent profile models of depression suggested significant heterogeneity in depressive symptoms, with the 5-profile model demonstrating the best fit (see supplemental Table 2), supporting the hypothesis of heterogeneity in depressive symptoms. Prior to testing conditional models, covariates were evaluated. Lower monthly income was associated with higher levels of total depression symptoms (r = −.14, p < .001). Whereas individuals from the rural study site had lower levels of depression compared to individuals living in urban and suburban sites (r = −.12, p = .001), individuals living in the urban site had higher levels of depression compared to individuals from the rural and suburban sites (r = .11, p = .004). Thus, monthly income and site (dummy coded) were included as covariates in conditional models. The 5-profile solution was the best fitting model based on evaluation of model fit indices, classification quality, and interpretability (see Supplemental Table 3).
Consistent with hypotheses, the 5-profile model comprised both content- and severity-level profiles (Figure 1). The largest profile was a severity-based profile (labeled “Low”; n = 410, 57%).) with mild elevations in physical symptoms and few to no symptoms across the other symptoms. Another severity-based profile was characterized by moderate levels across all symptoms (Moderate, n = 185, 26%). The final severity-based profile was characterized by high levels across all symptoms (Severe, n = 45, 6%). The remaining two profiles were content-based. One was characterized by high levels of interpersonal symptoms of depression (Interpersonal Rejection, n = 22, 3%) and another by high levels of depressed affect and physical symptoms but low to moderate levels of other symptoms (High Depressed Affect and Physical, n = 52, 7%). Thus, we identified heterogeneity in depressive symptoms captured by three symptom severity profiles (Low, Moderate, and Severe) and two symptom content profiles (Interpersonal Rejection and High Depressed Affect and Physical). Rather than identifying a physical symptoms profile, a depressed affect profile, and an interpersonal profile, where elevations existed only within those domains, the LPA derived, data-driven profiles were more nuanced.
The profiles differed significantly on CES-D total score (F[4,705] = 675.06, p < .001) with a total score of 38.44 (sd = 6.83) for the Severe profile, 35.29 (sd = 5.37) for the High Depressed Affect and Physical profile, 21.86 (sd = 4.81) for the Moderate profile, 19.09 (sd = 5.86) for the Interpersonal Rejection profile, and 9.71 (sd = 4.51) for the Low profile. All profiles were statistically different from each of the other profiles at the p < .05 level except for the difference between the Interpersonal Rejection and Moderate profiles (p = .088).
Associations between Depression Profiles and Parenting Behavior at Child Age 2
In variable-centered analyses (Supplemental table 1), a modest association was observed between CES-D total score and harsh parenting (r=.12, p=.001); nonsignificant associations were observed between CES-D total score and positive parenting and disengaged parenting.
Harsh parenting.
In person-centered analyses, significant differences in harsh parenting were observed between profiles of maternal depression (F[4,699]=6.92, p<.001, partial η2=.04, see Table 1). The highest mean level of harsh parenting was observed among women with the High Depressed Affect and Physical profile with moderate to large effect size differences compared to all other profiles (compared to Low d=.69, Interpersonal Rejection d=.87, and Moderate d=.52) except the Severe profile (d=.33; Table 2). Women with the Severe profile demonstrated the second highest level of harsh parenting, with a large effect size difference (d=.74) compared only to women with the Interpersonal Rejection profile. Women with the Moderate profile demonstrated the third highest level of harsh parenting with moderate to large effect size differences compared only to women with the Interpersonal Rejection (d=.40) profile. Thus, our hypothesis that the Severe profile would be associated with higher levels of harsh parenting compared to the Low profile was not supported; although women with the Severe profile had the second highest level of harsh parenting, it was not statistically higher than women in the Low profile. Our hypothesis that elevations in physical and interpersonal symptoms would be associated with high levels of harsh parenting was supported for physical symptoms given the highest elevations of harsh parenting were observed among the two profiles with the highest levels of physical symptoms: High Depressed Affect and Physical and Severe.
Table 1.
Differences in Parenting at Child Ages 2 and 3 by Maternal Depression Symptom Profile at Child age 2
| F(df1,df2) | p-value | Partial η2 | |
|---|---|---|---|
|
| |||
| Child age 2 | |||
|
| |||
| Harsh parenting behavior | 6.92(4,699) | <.001 | .04 |
| Positive parenting behavior | 2.03(4,705) | .088 | .01 |
| Disengaged parenting behavior | 2.36(4,700) | .052 | .01 |
|
| |||
| Child age 3 | |||
|
| |||
| Harsh parenting behavior overall model | 1.52(19,593) | .073 | .05 |
|
| |||
| Depression profile | 0.52(4,593) | .362 | .01 |
| Intervention status | 0.18(1,593) | .672 | .00 |
| Harsh parenting (Age 2) | 2.18(1,593) | .140 | .00 |
| Total maternal depression symptoms (Age 3) | 2.17(1,593) | .141 | .00 |
| Depression profile X Intervention status | 0.96(4,593) | .430 | .01 |
| Depression profile X Harsh parenting (Age 2) | 0.93(4,593) | .445 | .01 |
| Depression profile X Total maternal depression symptoms (Age 3) | 0.44(4,593) | .779 | .00 |
|
| |||
| Positive parenting behavior overall model | 15.76(19,606) | <.001 | .33 |
|
| |||
| Depression profile | 0.39(4,606) | .814 | .00 |
| Intervention status | 6.00(1,606) | .015 | .01 |
| Positive parenting (Age 2) | 61.89(1,606) | <.001 | .09 |
| Total maternal depression symptoms (Age 3) | 11.38(1,606) | <.001 | .02 |
| Depression profile X Intervention status | 2.22(4,606) | .065 | .01 |
| Depression profile X Positive parenting (Age 2) | 0.39(4,606) | .819 | .00 |
| Depression profile X Total maternal depression symptoms (Age 3) | 0.76(4,606) | .550 | .01 |
|
| |||
| Disengaged parenting behavior | 7.57(19,595) | <.001 | .20 |
|
| |||
| Depression profile | 2.93(4,595) | .020 | .02 |
| Intervention status | 1.85(1,595) | .175 | .00 |
| Disengaged parenting (Age 2) | 35.23(1,595) | <.001 | .06 |
| Total maternal depression symptoms (Age 3) | 0.37(1,595) | .543 | .00 |
| Depression profile X Intervention status | 0.70(4,595) | .594 | .01 |
| Depression profile X Disengaged parenting (Age 2) | 1.22(4,595) | .301 | .01 |
| Depression profile X Total maternal depression symptoms (Age 3) | 2.12(4,595) | .077 | .01 |
Table 2.
Post-hoc Comparisons for Associations between Parenting behavior at Child Ages 2 and 3 and Maternal Depression Symptom Profile at Child age 2
| Low | Interpersonal Rejection | Moderate | High Depressed Affect and Physical | Severe | Post-hoc comparisons | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| m | sd | m | sd | m | sd | m | sd | m | sd | ||
|
| |||||||||||
| Child age 2 | |||||||||||
|
| |||||||||||
| Harsh parenting behavior | −.06 | .64 | −.24 | .38 | .02 | .68 | .40 | .84 | .15 | .60 |
H > L*** H > I*** H > M** H > S M > I S > I |
| Positive parenting behavior | .04 | .74 | −.12 | .59 | −.12 | .78 | −.08 | .65 | .08 | .72 | - |
| Disengaged parenting behavior | −.04 | .62 | .14 | .76 | .11 | .93 | −.01 | .67 | −.18 | .59 | I > S |
|
| |||||||||||
| Child age 3 | m | se | m | se | m | se | m | se | m | se | |
|
| |||||||||||
| Harsh parenting behavior | −.02 | .04 | .05 | .16 | .07 | .05 | −.28 | .13 | −.14 | .13 | - |
| Positive parenting behavior | −.01 | .04 | −.08 | .14 | −.01 | .05 | −.06 | .12 | .04 | .13 | - |
| Disengaged parenting behavior | −.02 | .03 | .05 | .13 | −.00 | .05 | .27 | .11 | .17 | .13 |
H > L* H > M* |
p<.001.
p<.01.
p<.05.
Note. L=Low. I=Interpersonal Rejection. M=Moderate. H=High Depressed Affect and Physical. S=Severe. Asterisks depict level of statistical significance for post-hoc comparisons. Underlining depicts post-hoc comparisons that were a moderate to large effect size (Cohen’s d ≥ .40). All mean values are z-scores. Mean and standard errors provided for parenting at child age 3 are estimates adjusted for disengaged parenting at age 2 and maternal depression at age 3.
Positive parenting.
Contrary to our expectations, no statistically significant differences in positive parenting behavior were observed between profiles of maternal depression (F[4,705]=2.03, p=.088, partial η2=.01, see Table 1). Our hypotheses that elevations across all symptoms (i.e., the Severe profile) would have lower levels of positive parenting compared to the Low profile was not supported, nor was our hypothesis that elevations in depressed affect and interpersonal symptoms would be associated with lower levels of positive parenting.
Disengaged parenting.
Statistically significant differences in disengaged parenting behavior were not observed between profiles of maternal depression (F[4,700]=2.36, p=.052, partial η2=.01, see Table 1). However, descriptively, women with the Interpersonal Rejection profile demonstrated the highest levels of disengaged parenting with a moderate effect size difference compared the Severe profile (d=.50; Table 2). These findings are contrary to our hypotheses that women with the Severe profile would have higher levels of disengaged parenting compared to women with the Low profile, and that elevations in physical and depressed affect symptoms would be associated with high levels of disengaged parenting. Despite the modest effect size, the difference in disengaged parenting between women with the Interpersonal Rejection profile and the Severe profile should be interpreted with caution.
Exploratory associations between Depression Profiles and Parenting at Child Age 3
Harsh parenting.
The model examining differences in harsh parenting behavior at child age 3 by depression symptom profile was not significant (Table 1). Our hypotheses that a profile depicting high levels across all symptoms (i.e., the Severe profile) would have higher levels of harsh parenting compared to the Low profile and that elevations in physical and interpersonal symptoms would be associated with high levels of harsh parenting were not supported.
Positive parenting.
The model for age 3 positive parenting behavior was significant, however, depression profile was not a significant predictor (Table 1). Within the model, being in the intervention group, having high levels of positive parenting at age 2, and having lower levels of depression at age 3 each predicted higher levels of positive parenting at age 3. However, only the association between positive parenting at age 2 and positive parenting at age 3 emerged as significant in post-hoc analyses (b=.55, se=.16, p<.001).
Disengaged parenting.
The model for age 3 disengaged parenting behavior was significant (Table 1). Within the model, there were significant main effects for depression profile and disengaged parenting at age 2. Regarding depression profiles, consistent with our hypothesis, women with the High Depressed Affect and Physical profile demonstrated higher levels of disengaged parenting compared to women with the Low and Moderate profiles (Table 2). Regarding disengaged parenting at age 2, higher levels at age 2 were associated with higher levels at age 3 (b=.45, se=.17, p=.009).
Discussion
High levels of maternal depressive symptoms and meeting diagnostic criteria for depression are widely established predictors of poor parenting outcomes in past variable-centered work. Using person-centered techniques (LPA), we examined individual differences in maternal depressive symptoms when children were 2 years old and three factors of parenting behavior measured when children were ages 2 and 3 years old: harshness, positivity, and disengagement. Notable significant individual differences in maternal depressive symptoms emerged, characterized by five distinct profiles: 1) Low, 2) Interpersonal Rejection, 3) Moderate, 4) High Depressed Affect and Physical, and 5) Severe. Meaningful differences in parenting behavior at child ages 2 and 3 were observed among profiles of maternal depression, particularly for harsh parenting behavior at age 2 and disengaged parenting at age 3.
Associations between maternal depression and harsh parenting
The association between profiles of maternal depressive symptoms and harsh parenting behavior at age 2 is consistent with variable-centered work. Our work extends these findings by demonstrating that women with high levels of depressed affect and physical symptoms in particular may be at highest risk for demonstrating harsh parenting. However, it is important to note that the associations between the High Depressed Affect and Physical profile and harsh parenting are exploratory and could be alternatively accounted for by other unobserved mechanisms beyond the scope of this study (e.g., genetics, other aspects of mental health).
The association between maternal depression and harsh parenting behavior is consistent with past work demonstrating that physical symptoms outside the context of depression, such as maternal chronic pain and fatigue, have been associated with higher levels of over-reactive parenting and hostility in parent-child interactions (Evans et al., 2006; Giallo et al., 2011b). Furthermore, the combination of high levels of depression and physical symptoms has been associated with risk for child maltreatment (Lamela et al., 2017). The association between maternal depression and parenting behavior has implications for mothers of young children identified in medical clinics based on the presence of physical symptoms, which may be indicative of or coupled with depressive symptoms. The association between maternal depression and parenting behavior is also relevant for depressed mothers of young children identified in mental health or other medical settings, who may also have co-occurring physical symptoms. We did not measure physical symptoms outside of depressive symptoms, such as pain, in the present study. An important future direction of this work is to better understand the scope of physical symptoms beyond the context of depression that may be common among this group of women.
The Severe and High Depressed Affect and Physical profiles have similar levels of depressed affect and physical symptoms, yet the Severe profile was not associated with elevations in harsh parenting at ages 2 or 3. Perhaps the difference between profiles is due to the presence of higher levels of interpersonal symptoms in the Severe profile that are not elevated in the High Depressed Affect and Physical profile. In fact, women with the Interpersonal Rejection profile descriptively demonstrated the lowest levels of harsh parenting. Therefore, the addition of interpersonal symptoms to the Severe profile may qualitatively change the mother’s experience of depression and her relationship to her child. The potential explanation for the addition of interpersonal symptoms is all speculative, and the novel nature of these findings strongly suggests that more work is needed to further explore these idiosyncratic findings.
The High Depressed Affect and Physical profile at age 2 was associated with concurrent harsh parenting behavior, but not harsh parenting at age 3. A concurrent association may not be surprising based on the episodic nature of depressive symptoms. High levels of depression symptoms wax and wane over time. Thus, women reporting high levels of depressed affect and physical symptoms at child age 2 may not continue to report such high levels a year later. For example, the bivariate correlation between total depression symptoms child ages 2 to 3 was moderate (r = .42, p<.001). Whereas longitudinal associations between maternal depression and parenting behavior have been noted in prior research, including in the present sample (Errázuriz Arellano et al., 2012; Taraban et al., 2017; Taraban & Shaw, 2018), the lack of predictive validity from depression profiles at child age 2 to parenting at child age 3 mirrors the dearth of predictive validity found for depression profiles in the present study. Furthermore, intervention families engaged in the Family Check-Up (FCU) intervention following initial assessments of parenting and depression symptoms at age 2, thus, the intervention may have influenced both levels of harsh parenting and maternal depression symptoms at age 3. Although neither the intervention, nor total depression symptoms, predicted harsh parenting at age 3 in our model, the model was large and statistically complex which could have impacted statistical power to detect associations. Thus, although global levels of maternal depression have been shown to predict parenting across time, individual differences in maternal depressive symptoms may not. More research is needed to further understand the longitudinal associations between individual differences in maternal depression and later parenting behavior.
Associations between depression and positive parenting
Positive parenting at child ages 2 and 3 was not differentiated by any maternal depression profile. In fact, levels of positive parenting among women with higher-risk profiles depicting various combinations of moderate to high levels of depression symptoms were comparable to and not statistically different from women reporting little to no symptoms of depression. The pattern of findings is contrary to past variable-centered work demonstrating that positive parenting behaviors such as sensitivity, warmth, and responsiveness are negatively related to high levels of maternal depressive symptoms (e.g., Lovejoy, Graczyk, O’Hare, & Neuman, 2000). However, our measure of positive parenting was a large composite comprised of multiple dimensions, including warmth, responsivity, positive praise, structuring of the child’s environment, and proactive parenting (e.g., planning ahead to prevent behavior problems). The multidimensional nature of the composite may gloss over important differences in abilities to engage in more behaviorally-oriented versus warmth/responsivity-oriented aspects of positive parenting behavior. However, in a post-hoc examination of associations between profiles of maternal depression and behavioral aspects of our positive parenting composite (e.g., proactive parenting and structuring) no differences were found among groups. Thus, our findings indicate that women with moderate to high levels of depression symptoms, though coping with other parenting challenges, can engage in the more behavioral aspects of positive parenting and did so at levels similar to women in the Low profile.
If women with symptoms of depression can engage in behavioral aspects of positive parenting, it would be notable for parenting interventions that target improving positive praise and reinforcement, both of which are associated with positive child outcomes, particularly lower levels of behavior problems during early childhood (Dishion et al., 2008). The capacity for women presenting with symptoms of depression to engage in behavioral elements of positive parenting at levels similar to women reporting little to no symptoms of depression may be an important strength to highlight and reinforce when working with women with high levels of depression symptoms to support the further development of these important parenting skills. FCU is an appropriate intervention for mothers with symptoms of depression given its strengths-based framework and demonstrated outcomes including improved positive parenting and reduced maternal depression (Dishion et al., 2008; Shaw et al., 2009).
Associations between depression and disengaged parenting
There was a non-significant but marginal trend for differences in depression symptom profile at age 2 and disengaged parenting at age 2. Conversely, at age 3, women with the High Depressed Affect and Physical profile at age 2 demonstrated statistically higher levels of disengaged parenting at age 3 compared to women with the Low and Moderate profiles. Taken together with cross-sectional findings at child age 2, the associations between profiles of maternal depression at age 2 and disengaged parenting at age 3 were not consistent. Women with the High Depressed Affect and Physical profile at child age 2 displayed high levels of harsh parenting concurrently at age 2 but not at age 3, where they instead displayed high levels of disengaged parenting. It may be that high or severe levels of depressive symptoms, particularly depressed affect and physical symptoms, are more acutely associated with agitation and negativity that transpire to harsh interactions with one’s children. If symptoms wane overtime, the association may weaken. Supporting this notion, past meta-analytic evidence suggests that the association between maternal depression and harsh/hostile parenting is strongest concurrently (Lovejoy et al., 2000).
In sum, we did not find support for our hypothesis that severe levels of depression would be associated with high levels of disengaged parenting at ages 2 and 3. It is possible that severe levels of symptoms are not as strongly related to disengaged parenting as they are to other forms of parenting. Past literature on associations between depression and parenting more strongly supports associations between depression and harsh parenting than depression and withdrawn/disengaged parenting (e.g., Lovejoy et al., 2000).
Limitations
The present study has numerous strengths including the large, ethnically diverse sample, prospective assessment of depression symptoms and parenting behavior, observational assessment of parenting, and use of novel person-centered methods to uncover nuance in relation to previously established, variable-centered analyses. However, the study is not without limitations. First, symptoms of depression were measured via self-report and thus subject to reporter bias, which may be particularly prevalent among individuals with depression (e.g., Hunt, Auriemma, & Cashaw, 2003). Although we used a well-established measure of depressive symptoms, the CES-D, future work in this area would be strengthened by the use of diagnostic clinical interviews to measure symptoms of depression. Furthermore, our assessment of depression symptoms and the relation to parenting was specific to the moment of assessment. Based on the dynamic nature of depression, an intriguing line of future work is to explore relationships between depressive symptoms and parenting using ecological momentary assessment methods to minimize such momentary changes.
Second, although diverse in many ways, the characteristics of our low-income, community sample may limit generalizability. Although our participants reported a wide range of depressive symptoms, our findings may not be generalizable to clinical samples. Further, we restricted our sample to include only female primary caregivers. Thus, findings may not generalize to fathers. The issue of a restricted sample is noteworthy because fathers are incredibly important figures in children’s lives and paternal depression has be noted to be associated with father’s parenting (e.g., Wilson & Durbin, 2010). We simply did not have enough fathers participate in the study to conduct a parallel analysis with fathers. There is great need for future work on depression among fathers and associations with parenting.
Finally, we examined associations between profiles of depression and parenting across a very short 1-year span of the toddler period. A remaining question for future study is whether associations between individual differences in symptoms of depression and parenting differ across development, as both children and their parents grow and their interactions change.
Conclusion
In conclusion, there is wide heterogeneity in symptoms of depression among mothers of 2-year-old children and these differences hold clinically relevant implications for different dimensions of parenting. Physical and depressed affect symptoms in particular may present risk for harsh parenting. As individual differences in profiles of depression were not associated with an aggregate of positive parenting, the findings suggest that mothers of toddlers with moderate to elevated levels of depressive symptoms and other symptoms (e.g., interpersonal, physical), may show normative levels of behavioral aspects of positive behavior. Based on the novelty of this study, much more work is needed to replicate and extend these findings to other samples.
Supplementary Material
Acknowledgements:
This research was supported by the National Institute on Drug Abuse (DA01610; PIs Shaw, Wilson, & Dishion). During the preparation of this manuscript, Dr. Guyon-Harris was supported by the Health Resources and Services Administration (T32 HP22240).
Footnotes
The vast majority of these female caregivers were the child’s biological mother (97.9%). Slightly less than two percent of children in the sample were being raised by another female relative, most often the child’s grandmother (n = 13; 1.8%). The terms “maternal” and “mother” are used throughout.
Interactive tasks included a free-play task (15 minutes), a clean-up task (5 minutes), four teaching tasks (3 minutes each), and a meal task (20 minutes). These tasks were videotaped and used for observational coding of parenting behavior.
The somatic domain of items will hereafter be referred to as “physical”
This study was not preregistered, and materials and data are not publicly available.
Contributor Information
Katherine L. Guyon-Harris, University of Pittsburgh School of Medicine, Department of Pediatrics, Children’s Hospital Office Building, 3414 5th Avenue, Pittsburgh, PA 15213
Lindsay Taraban, University of Pittsburgh.
Debra L. Bogen, Allegheny County Health Department
Melvin N. Wilson, University of Virginia
Daniel S. Shaw, University of Pittsburgh
References
- Albright MB, & Tamis-LeMonda CS (2002). Maternal depressive symptoms in relation to dimensions of parenting in low-income mothers. Applied Developmental Science, 6(1), 24–34. 10.1207/S1532480XADS0601_03 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). DSM-5: Diagnostic and Statistical Manual of Mental Disorders, 5th edition. In Diagnostic and Statistical Manual of Mental Disorders 4th edition TR. American Psychiatric Publishing. https://books.google.com/books?hl=de&lr=&id=-JivBAAAQBAJ&pgis=1 [Google Scholar]
- Baden AD, & Howe GW (1992). Mothers’ attributions and expectancies regarding their conduct-disordered children. Journal of Abnormal Child Psychology, 20(5), 467–485. 10.1007/BF00916810 [DOI] [PubMed] [Google Scholar]
- Belsky J (1984). The determinants of parenting: A process model. Child Development, 55(1), 83–96. 10.1111/j.1467-8624.1984.tb00275.x [DOI] [PubMed] [Google Scholar]
- Bradley RH, & Caldwell BM (1984). The HOME Inventory and family demographics. Developmental Psychology, 20(2), 315–320. 10.1037/0012-1649.20.2.315 [DOI] [Google Scholar]
- Ceballo R, & McLoyd VC (2002). Social support and parenting in poor, dangerous neighborhoods. Child Development, 73(4), 1310–1321. 10.1111/1467-8624.00473 [DOI] [PubMed] [Google Scholar]
- Conners-Burrow NA, McKelvey L, Perry D, Whiteside-Mansell L, Kraleti S, Mesman G, Holmes K, & Kyzer A (2016). Low-Level Symptoms of Depression in Mothers of Young Children are Associated with Behavior Problems in Middle Childhood. Maternal and Child Health Journal, 20(3), 516–524. 10.1007/s10995-015-1849-0 [DOI] [PubMed] [Google Scholar]
- Crnic KA, & Greenberg MT (1990). Minor Parenting Stresses with Young Children. Child Development, 61(5), 1628–1637. 10.1111/j.1467-8624.1990.tb02889.x [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Geraedts AS, van Oppen P, Andersson G, Markowitz JC, & van Straten A (2011). Interpersonal psychotherapy for depression: a meta-analysis. American Journal of Psychiatry, 168(6), 581–592. 10.1176/appi.ajp.2010.10101411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeJong H, Fox E, & Stein A (2016). Rumination and postnatal depression: A systematic review and a cognitive model. Behaviour Research and Therapy, 82, 38–49. 10.1016/J.BRAT.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Hogansen J, Winter C, & Jabson J (2004). The coder impressions inventory. Unpublished coding manual. Available from the Child and Family Center, 6217. [Google Scholar]
- Dishion TJ, Shaw D, Connell A, Gardner F, Weaver C, & Wilson M (2008). The family check-up with high-risk indigent families: Preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Development, 79(5), 1395–1414. 10.1111/j.1467-8624.2008.01195.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Errázuriz Arellano PA, Harvey EA, & Thakar DA (2012). A Longitudinal Study of the Relation Between Depressive Symptomatology and Parenting Practices. Family Relations, 61(2), 271–282. 10.1111/j.1741-3729.2011.00694.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Shipton EA, & Keenan T (2006). The Relationship Between Maternal Chronic Pain and Child Adjustment: The Role of Parenting as a Mediator. Journal of Pain, 7(4), 236–243. 10.1016/j.jpain.2005.10.010 [DOI] [PubMed] [Google Scholar]
- Gaston S, Nugent N, Peters ES, Ferguson TF, Trapido EJ, Robinson WT, & Rung AL (2016). Exploring heterogeneity and correlates of depressive symptoms in the Women and Their Children’s Health (WaTCH) Study. Journal of Affective Disorders, 205, 190–199. 10.1016/j.jad.2016.03.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerdes AC, Hoza B, Arnold LE, Pelham WE, Swanson JM, Wigal T, & Jensen PS (2007). Maternal depressive symptomatology and parenting behavior: Exploration of possible mediators. Journal of Abnormal Child Psychology, 35(5), 705–714. 10.1007/s10802-007-9134-3 [DOI] [PubMed] [Google Scholar]
- Giallo R, Rose N, & Vittorino R (2011a). Fatigue, wellbeing and parenting in mothers of infants and toddlers with sleep problems. Journal of Reproductive and Infant Psychology, 29(3), 236–249. 10.1080/02646838.2011.593030 [DOI] [Google Scholar]
- Giallo R, Rose N, & Vittorino R (2011b). Fatigue, wellbeing and parenting in mothers of infants and toddlers with sleep problems. Journal of Reproductive and Infant Psychology, 29(3), 236–249. 10.1080/02646838.2011.593030 [DOI] [Google Scholar]
- Goodman SH, & Garber J (2017). Evidence-based interventions for depressed mothers and their young children. Child Development, 88(2), 368–377. 10.1111/cdev.12732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal Depression and Child Psychopathology: A Meta-Analytic Review. In Clinical Child and Family Psychology Review (Vol. 14, Issue 1, pp. 1–27). Springer. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Hashima PY, & Amato PR (1994). Poverty, Social Support, and Parental Behavior. Child Development, 65(2), 394–403. 10.1111/j.1467-8624.1994.tb00758.x [DOI] [PubMed] [Google Scholar]
- Hybels CF, Blazer DG, Landerman LR, & Steffens DC (2011). Heterogeneity in symptom profiles among older adults diagnosed with major depression. International Psychogeriatrics, 23(6), 906–922. 10.1017/S1041610210002346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabson JM, Dishion TJ, Gardner FEM, & Burton J (2004). Relationship Process Code v-2.0. training manual: A system for coding relationship interactions. Child and Family Center, 160, 97401–2426. [Google Scholar]
- Jennings KD, Stagg V, & Connors RE (1991). Social Networks and Mothers’ Interactions with Their Preschool Children. Child Development, 62(5), 966–978. 10.1111/j.1467-8624.1991.tb01583.x [DOI] [Google Scholar]
- Lamela D, Jongenelen I, Morais A, & Figueiredo B (2017). Cognitive-affective depression and somatic symptoms clusters are differentially associated with maternal parenting and coparenting. Journal of Affective Disorders, 219, 37–48. 10.1016/j.jad.2017.05.006 [DOI] [PubMed] [Google Scholar]
- Lee C-YS, Anderson JR, Horowitz JL, & August GJ (2009). Family Income and Parenting: The Role of Parental Depression and Social Support. Family Relations, 58(4), 417–430. 10.1111/j.1741-3729.2009.00563.x [DOI] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, & Neuman G (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 10.1016/S0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- Moilanen KL, Shaw DS, Dishion TJ, Gardner F, & Wilson M (2010). Predictors of Longitudinal Growth in Inhibitory Control in Early Childhood. Social Development, 19(2), 326–347. 10.1111/J.1467-9507.2009.00536.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mora PA, Beamon T, Preuitt L, DiBonaventura M, Leventhal EA, & Leventhal H (2012). Heterogeneity in depression symptoms and health status among older adults. Journal of Aging and Health, 24(5), 879–896. 10.1177/0898264312440323 [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Østergaard SD, Jensen SOW, & Bech P (2011). The heterogeneity of the depressive syndrome: When numbers get serious. In Acta Psychiatrica Scandinavica (Vol. 124, Issue 6, pp. 495–496). 10.1111/j.1600-0447.2011.01744.x [DOI] [PubMed] [Google Scholar]
- Paulson JF, Dauber S, & Leiferman JA (2006). Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics, 118(2), 659–668. 10.1542/peds.2005-2948 [DOI] [PubMed] [Google Scholar]
- Peterson J, Winter C, Jabson J, & Dishion TJ (2008). Relationship affect coding system. Unpublished coding manual. Eugene, OR: University of Oregon, Child and Family Center. [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Saracino RM, Cham H, Rosenfeld B, & Nelson J, C. (2018). Latent Profile Analyses of Depressive Symptoms in Younger and Older Oncology Patients. Assessment. 10.1177/1073191118784653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman ME (1974). Depression and learned helplessness. In Friedman RJ & Katz MM (Eds.), The Psychology of Depression: Contemporary Theory and Research (pp. 83–113). Winston. [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, & Gardner F (2009). Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology, 21(2), 417–439. 10.1017/S0954579409000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons RL, Lorenz FO, Wu CI, & Conger RD (1993). Social Network and Marital Support as Mediators and Moderators of the Impact of Stress and Depression on Parental Behavior. Developmental Psychology, 29(2), 368–381. 10.1037/0012-1649.29.2.368 [DOI] [Google Scholar]
- Taraban L, & Shaw DS (2018). Parenting in context: Revisiting Belsky’s classic process of parenting model in early childhood. In Developmental Review (Vol. 48, pp. 55–81). Mosby Inc. 10.1016/j.dr.2018.03.006 [DOI] [Google Scholar]
- Taraban L, Shaw DS, Leve LD, Wilson MN, Dishion TJ, Natsuaki MN, Neiderhiser JM, & Reiss D (2017). Maternal depression and parenting in early childhood: Contextual influence of marital quality and social support in two samples. Developmental Psychology, 53(3), 436–449. 10.1037/dev0000261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulbricht CM, Chrysanthopoulou SA, Levin L, & Lapane KL (2018). The use of latent class analysis for identifying subtypes of depression: A systematic review. In Psychiatry Research (Vol. 266, pp. 228–246). Elsevier Ireland Ltd. 10.1016/j.psychres.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieites V, & Reeb-Sutherland BC (2017). Individual differences in non-clinical maternal depression impact infant affect and behavior during the still-face paradigm across the first year. Infant Behavior and Development, 47, 13–21. 10.1016/j.infbeh.2017.02.005 [DOI] [PubMed] [Google Scholar]
- Waller R, Gardner F, Dishion T, Sitnick SL, Shaw DS, Winter CE, & Wilson M (2015). Early Parental Positive Behavior Support and Childhood Adjustment: Addressing Enduring Questions with New Methods. Social Development, 24(2), 304–322. 10.1111/sode.12103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg MK, Tronick EZ, Beeghly M, Olson KL, Kernan H, & Riley JM (2001). Subsyndromal depressive symptoms and major depression in postpartum women. American Journal of Orthopsychiatry, 71(1), 87–97. 10.1037/0002-9432.71.1.87 [DOI] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JC, & Klerman G (2008). Comprehensive guide to interpersonal psychotherapy. Basic Books. [Google Scholar]
- Wilson S, & Durbin CE (2010). Effects of paternal depression on fathers’ parenting behaviors: A meta-analytic review. Clinical Psychology Review, 30(2), 167–180. 10.1016/J.CPR.2009.10.007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


