Abstract
Objective:
Understanding public policymakers’ priorities for youth substance use, and the factors that influence priorities, can inform dissemination and implementation of strategies that promote evidence-based decision-making. This study aimed to characterize U.S. state and county substance use agency policymakers’ priorities for youth substance use, the factors that influence these priorities, and to examine differences in priorities and influences between state and county policymakers.
Methods:
A web-based survey was completed by 122 substance use agency policymakers (response rate= 22%) from 35 states in 2020. Respondents rated the priority of 14 issues and the extent to which nine factors influenced these priorities. Data were analyzed as both dichotomous and continuous variables, as well as together and separately for state and county policymakers.
Results:
In the entire sample, the highest priorities for youth substance use were the social determinants of substance use (87%), adverse childhood experiences/childhood trauma (85%), and increasing access to school-based substance use programs (82%). The lowest priorities were increasing access to naloxone for youth (49%), increasing access to medications for opioid use disorder among youth (48.7%), and de-implementing non-evidence-based youth substance use programs (41%). The factors that most influenced priorities were budget issues (80%), state legislature priorities (69%), federal priorities (66.9%), and governor priorities (65%). Issues related to program implementation and de-implementation were significantly (p ≤ .05) higher priorities for state than county policymakers.
Conclusions:
The study findings can inform the tailoring of dissemination and implementation strategies to account for the inner- and outer-setting context of public substance use agencies.
Keywords: Youth, substance use, policymakers, public substance use agencies, implementation science
State and county public substance use agencies are integral to the provision of prevention, treatment, and recovery services for adolescents and young adults (hereafter referred to as “youth”) in the United States.1 These agencies are involved with implementation of the approximately $290 million in youth-focused substance use federal programing that is allocated by Congress annually2 and the $1.8 billion Federal Substance Abuse Prevention and Treatment Block Grant program, which funds services for youth and adults.3 As such, public substance use agency officials are an important stakeholder group to target in dissemination and implementation efforts to increase the reach of youth-focused evidence-based substance use treatments and prevention programs.4,5
Implementation science frameworks suggest that the success of dissemination and implementation strategies could be increased by accounting for the extent to which different youth substance use issues are priorities within these agencies.6,7 Such priorities are conceptualized as “inner-setting” determinants in frameworks such as the Consolidated Framework for Implementation Research (CFIR)8 and the Exploration, Preparation, Implementation, Sustainment (EPIS) framework.9 The impact of dissemination and implementation strategies could also be enhanced by taking into consideration the extent to which different external factors are perceived as influencing agency priorities for youth substance use. Such influences are conceptualized as “outer-setting” determinants in implementation science frameworks. 8–10
Recent reviews suggest that inner- and outer-setting factors are frequently measured in research conducted in public substance use and mental health agency settings.11,12 Prior research has also assessed U.S. state legislators’ and city mayors’ priorities for public health and the factors that influence these priorities.13,14 While national reports have identified strategies substance use agencies can use to address issues related to youth substance use,15–18 no prior research has assessed the extent to which specific issues are perceived as priorities within substance use agencies or factors perceived as influencing these priorities.
Understanding public agency officials’ priorities for youth substance use, and the factors that influence them, is important because doing so can inform the selection and tailoring of dissemination or implementation strategies that target these agencies.19 For example, a non-government organization that conducts trainings to support the implementation of substance use treatments could develop training materials so that the content (e.g., treatments of focus, illustrative case studies) is tailored to align with the priorities of substance use agencies. As another example, dissemination materials about an evidence-based treatment could be tailored to include information about cost-effectiveness if factors related to budget strongly influence priorities; or include a patient testimonial if patient demand strongly influences priorities.20 In addition to informing the selection and tailoring of dissemination and implementation strategies, understanding the priorities of substance use agencies can help align the research questions that researchers ask with the practice contexts in which public agency officials make decisions.
Current Study
This study seeks to advance understanding about the inner-setting priorities and outer-setting influences of public substance use agencies. The study aims are to: 1) characterize U.S. state and county substance use agency officials’ priorities for youth substance use, 2) describe the factors that influence these priorities, and 3) assess differences in priorities and influences between substance use agency officials at state versus county levels. We compare officials at these two levels of government because the contextual factors influencing their work may differ.
METHODS
We created a contact database of senior-level officials in substance use agencies and directors of youth-focused divisions and programs within these agencies. To do this, we reviewed contact lists maintained by the National Association of State Alcohol and Drug Abuse Directors and the Substance Abuse and Mental Health Services Administration and conducted Internet searches. We identified these officials at the state-level for all 50 states and additionally at the county-level in 15 states that have more de-centralized public behavioral health systems, identified as such through consultation with the National Association of State Mental Health Program Directors. The states used to create the county sample frame were geographically diverse in terms of their U.S. Census Region: West= four states (CA, OR, UT, WA), Midwest= five states (IA, MN, NE, OH, WI), South= three states (FL, NC, TX), and Northeast= three states (CT, NY, PA).
A web-based survey of the state agency officials was conducted between January and March 2020, and a web-based survey of the county agency officials was conducted between July and September 2020. The surveys were identical except for using “state” or “county” language when referring to the respondent’s agency. The surveys were approved by the BLINDED University IRB. Each agency official was sent a personalized e-mail eight times with a survey link, and telephone follow-up was conducted with state officials to ensure that e-mails were received. Respondents were offered a $20 gift card for survey completion. The survey was sent to 112 state officials with valid e-mail addresses and completed by 42 (response rate= 38%) and 473 county officials with valid e-mail addresses and completed by 80 (response rate= 17%). The aggregate sample size was 122 (aggregate response rate= 22%), and at least one respondent completed the survey in 35 states.
Non-response analysis was assessed using geographic, political, and epidemiologic indicators. These analyses revealed that there were no statistically significant differences in the response rate by state U.S. Census region within the state agency (χ2= 5.15, p= .16) or county agency sample (χ2= 4.63, p= .20) nor by the political party of the state’s governor in either sample (χ2= 0.19, p= .66 and χ2 =0.66, p= .42, respectively). The mean opioid overdose death rate among youth ages 0–24 per 10,000 population was slightly lower in states of survey respondents than non-respondents in the state agency sample (mean= 3.53 vs. 4.59, F= 5.50, p= .02) but there was no significant difference in these mean rates between respondents and non-respondents in the county agency sample (F= 0.60, p= .44).
Measures
The survey presented respondents with a list of 14 youth substance use issues and instructed them to “indicate the extent to which you perceive it as currently being a priority for your agency” on a 5-point Likert scale (1= Not a priority/beyond scope of agency,” 5= “Top priority”). The survey also presented respondents with a list of nine factors and instructed them to “indicate how much influence you think it currently has on your agency’s youth substance use priorities in general” (1= “No influence,” 5= “Major influence”). Similar items have been used to assess factors that influence state legislators’ health priorities.14 The lists of priority issues and influencing factors were informed by a review of youth substance use literature and then refined through telephone and e-mail correspondence with former state and county behavioral health agency officials. The order of the items in the priority and influencing factor lists were randomized to reduce the risk of order-effect bias.21
Analysis
Responses were analyzed as both dichotomous and continuous variables. When dichotomized, responses of 4 or 5 were coded as “Priority” and “Influences Priorities.” Descriptive statistics characterized the proportion of respondents that identified each issue as a priority and each factor as an influence. Means and standard deviations were calculated for each item. State and county official data were analyzed together as well as separately. Chi-square and two-tailed independent sample t-tests compared differences in responses between the samples of state and county officials.
RESULTS
Tables 1 and 2 show the proportion of agency officials that identified each youth substance use issue as a priority and each factor as an influence on priorities, respectively, stratified by state/county and for both samples pooled together. Panels A and B in Figure 1, respectively, plot the mean priority ratings and influence ratings among state agency officials (x-axis) and county officials (y-axis). Appendixes A and B, respectively, provide the means, standard deviations, and t-test statistics for the priority and influence ratings.
Table 1.
Proportion of Public Substance Use Agency Officials Identifying Issues as Priorities for Youth Substance Use, State and County Officials, 2020
| All N= 122 |
State n= 42 |
County n= 80 |
|||
|---|---|---|---|---|---|
| % | % | % | χ2 | p | |
| Addressing the social determinants of youth substance use | 87 | 92 | 84 | 1.43 | 0.23 |
| Adverse childhood experiences/childhood trauma | 85 | 82 | 86 | 0.36 | 0.55 |
| Increasing access to school-based youth substance use disorder prevention/treatment programs | 82 | 83 | 81 | 0.04 | 0.84 |
| Impact of parental substance use disorder on youth | 80 | 83 | 79 | 0.33 | 0.56 |
| Improving the implementation evidence-based youth substance use disorder treatment/prevention programs | 79 | 92 | 73 | 6.05 | 0.01 |
| Increasing access to community-based youth substance use disorder prevention/treatment programs | 79 | 82 | 78 | 0.33 | 0.57 |
| Increasing access to family-focused youth substance use disorder treatment/prevention and treatment programs | 76 | 78 | 75 | 0.07 | 0.79 |
| Coordinating youth substance use disorder services with community-based social services | 76 | 68 | 81 | 2.45 | 0.12 |
| Preventing opioid deaths among youth | 73 | 69 | 74 | 0.34 | 0.56 |
| Increasing/aligning the use of quality measures in youth substance use disorder treatment and prevention programs | 72 | 80 | 68 | 1.76 | 0.18 |
| Increasing access to harm reduction education for young people | 66 | 58 | 70 | 1.73 | 0.19 |
| Increasing access to naloxone for youth in communities and schools | 49 | 55 | 46 | 0.83 | 0.36 |
| Increasing access to medications for opioid use disorder among youth | 49 | 43 | 52 | 0.94 | 0.33 |
| De-implementing youth substance use disorder treatment/prevention programs that are not evidence-based | 41 | 65 | 28 | 15.18 | <0.001 |
An issue was coded as a “priority” if rated of 4 or 5 on 5-point Likert-scale.
Table 2.
Proportion of Public Substance Use Agency Officials Identifying Factors as Influencing Priorities for Youth Substance Use, State and County Officials, 2020
| All N= 122 |
State n= 42 |
County n= 80 |
|||
|---|---|---|---|---|---|
| % | % | % | χ2 | p | |
| Budget issues | 80 | 78 | 81 | 0.18 | 0.68 |
| State legislature priorities | 69 | 83 | 63 | 5.33 | 0.02 |
| Federal government priorities | 67 | 73 | 64 | 1.09 | 0.30 |
| Governor priorities | 65 | 81 | 56 | 6.95 | >0.01 |
| Research evidence | 53 | 68 | 45 | 5.90 | 0.02 |
| State resident demand | 44 | 42 | 45 | 0.14 | 0.71 |
| Provider advocacy organization priorities | 34 | 34 | 34 | 0.00 | 0.97 |
| Consumer advocacy organization priorities | 22 | 20 | 23 | 0.14 | 0.70 |
| Lawsuits/ concerns about litigation | 15 | 20 | 13 | 1.05 | 0.30 |
A factor was coded as an “influence” if rated of 4 or 5 on 5-point Likert-scale.
Figure 1.
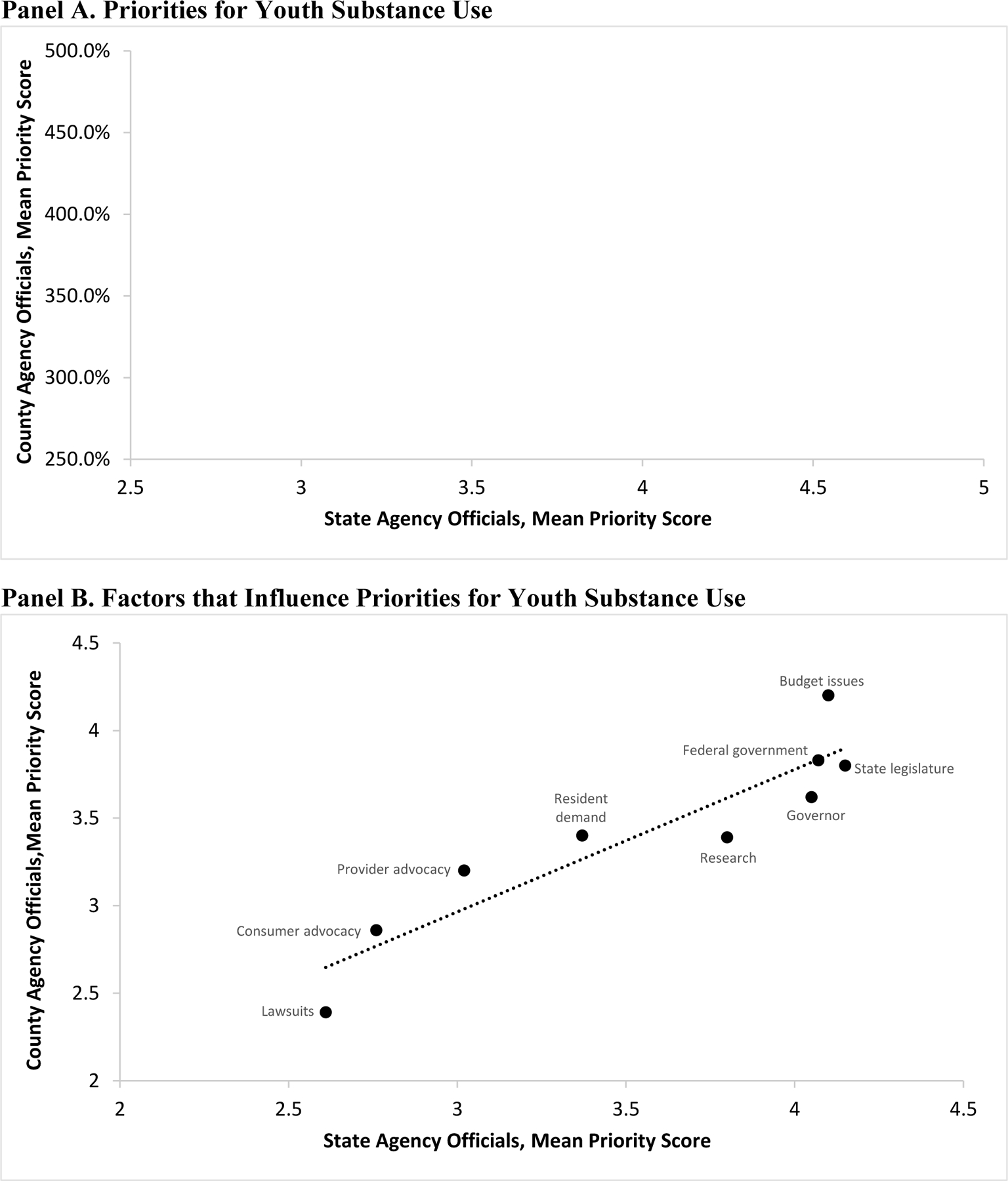
Mean Priority and Factor of Influence Scores for Youth Substance Use Issues, State and County Officials, 2020
OUD= opioid use disorder
Priorities for Youth Substance Youth
The issues most frequently identified as priorities for youth substance use, with ≥ 80% of the sample identifying them as such, were the social determinants of youth substance use (87%), adverse childhood experiences/childhood trauma (85%), increasing access to school-based substance use programs (82%), and the impact of parental substance use on youth (80%). Increasing access to community-based youth substance use programs was identified as a priority by (79%) of respondents and was the issue with the highest mean priority rating (4.29). The issues least frequently identified as priorities, with < 50% of the sample identifying them as such, were increasing access to naloxone for youth (49%), increasing access to medications for opioid use disorder among youth (49%), and de-implementing youth substance use programs that are not evidence-based (41%).
As shown in Table 1 and Panel A of Figure 1, state and county officials were generally similar in terms of the extent to which they perceived the various youth substance use issues as priorities. The only exceptions to this, however, were for issues explicitly related to program implementation. A significantly larger proportion of state than county officials identified improving the implementation of evidence-based youth substance use programs as a priority (92% vs. 73% p= 0.01) as well as de-implementing youth substance use programs that are not evidence-based (65% vs. 28% p< 0.001). Improving the implementation of youth substance use programs had the highest mean priority score among state officials and this was significantly higher than the mean score for this issue among county officials (4.67 vs. 3.97, p< 0.001).
Factors that Influence Priorities for Youth Substance Use
The factors most frequently identified as influencing priorities for youth substance use, with > 60% of the sample identifying them as such, were budget issues (80%), state legislature priorities (69%), federal government priorities (67%), and governor priorities (65%). The factors least frequently identified as having influence, with < 40% of the sample identifying them as such, were provider advocacy organization priorities (34%), consumer advocacy organization priorities (22%), and lawsuits/concerns about litigation (15%). Only about half (53%) of respondents identified research evidence as influencing youth substance use priorities.
As shown in Table 2 and Panel B of Figure 1, similar factors influenced the youth substance use priorities of state and county officials. A significantly larger proportion of state than county officials identified research evidence as influencing their agency’s priorities (68% vs. 45%, p= 0.02). As to be expected given their respective levels of government, a significantly larger proportion of state than county officials identified state legislature priorities (83% vs. 63%, p= 0.02) and governor priorities (81% vs. 56%, p= 0.008) as influencing agency priorities for youth substance use.
DISCUSSION
State and county substance use agency officials perceive a range of issues to be high priorities for youth substance use, with upstream causes of substance use (i.e., social determinants, adverse childhood experiences/childhood trauma) most frequently identified as top priorities. Evidence-supported policy recommendations to address these root causes exist22–25 and our findings suggest that dissemination and implementation strategies that are tailored to include information that helps substance use agency officials address these issues—either directly or via advocating for legislative changes—may be well-received. Large proportions of state (92%) and county (73%) officials also identify improving the implementation of evidence-based youth substance use treatment programs as a priority. This indicates that inner-setting context may be supportive of implementation strategies that help facilitate the delivery of evidence-based, youth-focused treatments in public substance use agencies.
Findings about the issues that are least frequently considered priorities are interesting when considered within the context of youth substance use treatment literature. This is particularly true in regard to the issues related to opioids. For example, only half of respondents identify increasing access to medications for opioid use disorder (OUD) among youth as a priority. Medication for OUD among youth is an evidence-based treatment26 recommended by the American Academy of Pediatrics, yet barriers to accessing medication for OUD among youth exist28,29 and the prevalence of OUD among youth has been increasing.30 Furthermore, only half of respondents identify increasing access to naloxone among youth as a priority despite naloxone being a recommended evidence-based intervention and uptake being low.31,32
In light of these findings, we conducted post-hoc analysis to assess whether the 2019 youth opioid overdose death rate among youth ages 0–24 in each respondent’s state was correlated with their priority rating of each of the three opioid-specific youth issues. We find no correlation in the state agency sample (r ≤ .182, p ≥ .335 for all three correlations) nor in the county agency sample (r between −.165 and .122, p ≥ .162 for all three correlations). These findings in our sample of administrative policymakers are in contrast to studies of state legislators which indicate that state opioid overdose death rates are associated with these elected policymakers’ opinions about opioid-related issues.33,34 Taken together, these results highlight a need to better understand the extent to which youth opioid-related issues are, and are not, priorities for substance use agency officials.
Only about two-thirds of state agency officials and one-quarter of county officials identify de-implementing non-evidence-based substance use programs for youth as a priority. While de-implementation is largely regarded as a priority area among implementation science researchers,35–38 it may be a low priority for substance use agency officials because there is insufficient workforce or program capacity to meet the need for youth substance use services in the United States.39,40 Thus, de-implementing programs might not be a priority because it could exacerbate treatment capacity issues by reducing the supply of programs. It is also possible that many respondents did not rate de-implementing non-evidence-based programs as a high priority because they did not perceive any of their programs to be non-evidence-based. There could be value in future research that explores how notions of “evidence-based” and de-implementation are conceptualized among substance use agency officials.
The finding that budget issues are perceived as having substantial influence on substance use agency priorities at state and county levels is consistent with prior research indicating that information about the budget impact and cost-effectiveness of substance use treatments is of paramount importance to policymakers.41–45 Such economic evidence exists46,47 and findings suggest that there could be benefit to tailoring dissemination materials to include this information. There could also be benefit to tailoring dissemination materials to include information about the costs of implementation strategies,48,49 especially because improving the implementation of evidence-based youth substance use programs was identified as a top agency priority.
The findings that state legislature and governor priorities have major influences on state substance use agencies’ priorities are not surprising given that these agencies are directly accountable to these entities. However, the finding is still important because it supports the notion that elected officials, such as state legislators and governors, are major outer-setting stakeholders and populations to target with dissemination and implementation efforts.10,41,42,45,50 Dissemination strategies that affect these elected officials’ perceptions of priorities for youth substance use could subsequently influence the priorities and practices of executive branch officials in substance use agencies. The finding that a moderate proportion (53%) of substance use agency officials perceive research evidence as influencing priorities is consistent with prior research45,51 and underscores the importance of selecting and tailoring implementation strategies to account for outer-setting contextual factors that influence decision-making.
Comparison of survey responses between state and county substance use agency officials generally revealed more similarities than differences. The most notable difference was that improving the implementation of evidence-based programs and de-implementing non-evidence-based programs were higher priorities among state than county officials. This finding could reflect county agency officials being more focused on the direct provision of substance use treatments while state agency officials also function in a strategic and planning capacity. However, the difference could also reflect the fact that the state agency survey was fielded immediately before the COVID-19 pandemic while the county agency survey was fielded during the pandemic.
Limitations
Our aggregate response rate of 22% is moderate for a sample public agency officials.52 Although respondents and non-respondents did not differ in terms of the U.S. Census region of their state or the political party of their governor, the mean youth opioid overdose death rate was slightly lower among respondents than non-respondents in the state agency official sample. However, it is unlikely that this substantially influenced the representativeness of results because we found no association between state youth opioid overdose death rates and substance use agency officials’ perceptions of youth opioid-related issues as priorities. Nevertheless, it is possible that respondents have different perceptions of priorities for youth substance use, and the factors that influence them, than non-respondents.
The survey asked about the relative priority of fourteen youth substance use issues and nine factors that could influence these priorities. By no means were these lists exhaustive inventories of all youth substance use issues that may be perceived as priorities or the factors that influence them. The survey was also limited to substance use agency officials, and a much wider range of public sector agencies (e.g., child welfare, criminal justice, education) address youth substance use issues.53 Lastly, it should be emphasized that the study focused on substance use agency officials’ perceptions and thus the unit of analysis is substance use agency officials themselves, not their agencies.
CONCLUSIONS
Social determinants of youth substance use, adverse childhood experiences/childhood trauma, increasing access to substance use programs in school and community settings, and the impact of parental substance use on youth are top priorities for substance agency officials. Improving the implementation of evidence-based substance use programs for youth is also perceived as a high priority, especially among state agency officials. However, de-implementing youth substance use programs that are not evidence-based is not a high priority at the state or county level. Budget issues and the priorities of state legislatures and governors are factors perceived as having substantial influence on the priorities for youth substance use in public substance use agencies, while research evidence is perceived as having only moderate influence. These survey findings can inform how dissemination and implementation strategies are selected and tailored to account for the contexts in which public substance use agency officials make policy decisions.
Supplementary Material
HIGHLIGHTS.
Addressing the upstream causes of youth substance use, such as social determinants and adverse childhood experiences/childhood trauma, is a high priority for substance use agency policymakers.
Improving the implementation of evidence-based youth substance use programs is a high priority for substance use agency policymakers, but de-implementing non-evidence-based substance use programs is a low priority.
Budget issues, state legislature priorities, federal priorities, and governor priorities have the most influence on substance use agency policymakers’ priorities for youth substance use.
Contributor Information
Jonathan Purtle, Department of Health Management and Policy, Drexel University Dornsife School of Public Health, Philadelphia.
Katherine L Nelson, Department of Health Management and Policy, Drexel University Dornsife School of Public Health, Philadelphia.
Rosie Mae Henson, Department of Health Management and Policy, Drexel University Dornsife School of Public Health, Philadelphia.
Sarah McCue Horwitz, Department of Child and Adolescent Psychiatry, New York University School of Medicine, New York City.
Mary M McKay, Brown School of Social Work at Washington University in St. Louis, St. Louis.
Kimberly E Hoagwood, Department of Child and Adolescent Psychiatry, New York University School of Medicine, New York City.
REFERENCES
- 1.Cavanaugh D, Kraft MK, Muck R, Merrigan DM. Toward an effective treatment system for adolescents with substance use disorders: The role of the states. Children and Youth Services Review 2011;33:S16–S22. [Google Scholar]
- 2.Government Accountability Office. Adolescent and Young Adult Substance Use: Federal Grants for Prevention, Treatment, and Recovery Services and for Research, GAO-18–606 2018. https://www.gao.gov/products/GAO-18-606.
- 3.Winters KC, Botzet AM, Stinchfield R, et al. Adolescent substance abuse treatment: A review of evidence-based research. Adolescent Substance Abuse: Springer; 2018:141–171. [Google Scholar]
- 4.Miller WR, Sorensen JL, Selzer JA, Brigham GS. Disseminating evidence-based practices in substance abuse treatment: A review with suggestions. Journal of substance abuse treatment 2006;31(1):25–39. [DOI] [PubMed] [Google Scholar]
- 5.McGovern MP, Saunders EC, Kim E. Substance abuse treatment implementation research. Journal of substance abuse treatment 2013;44(1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nilsen P. Making sense of implementation theories, models and frameworks. Implementation science 2015;10(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Damschroder LJ, Hagedorn HJ. A guiding framework and approach for implementation research in substance use disorders treatment. Psychology of addictive behaviors 2011;25(2):194. [DOI] [PubMed] [Google Scholar]
- 8.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science 2009;4(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research 2011;38(1):4–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raghavan R, Bright CL, Shadoin AL. Toward a policy ecology of implementation of evidence-based practices in public mental health settings. Implementation Science 2008;3(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implementation Science 2019;14(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McHugh S, Dorsey CN, Mettert K, Purtle J, Bruns E, Lewis CC. Measures of outer setting constructs for implementation research: A systematic review and analysis of psychometric quality. Implementation Research and Practice 2020;1:2633489520940022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Godinez Puig L, Lusk K, Glick D, et al. Perceptions of Public Health Priorities and Accountability Among US Mayors. Public Health Reports. 2020:0033354920966050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Purtle J, Dodson EA, Brownson RC. Uses of research evidence by State legislators who prioritize behavioral health issues. Psychiatric Services 2016;67(12):1355–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Academies of Sciences E, Medicine. Fostering healthy mental, emotional, and behavioral development in children and youth: A national agenda National Academies Press; 2019. https://www.nap.edu/catalog/25201/fostering-healthy-mental-emotional-and-behavioral-development-in-children-and-youth. [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration: Substance Misuse Prevention for Young Adults. Publication No. PEP19-PL-Guide-1 Rockville, MD: National Mental Health and Substance Use Policy Laboratory. Substance Abuse and Mental Health Services Administration, 2019. https://store.samhsa.gov/sites/default/files/d7/priv/pep19-pl-guide-1.pdf [Google Scholar]
- 17.Reaching Youth At Risk for Substance Use and Misuse. National Association of State Alcohol and Drug Abuse Directors. ND https://nasadad.org/wp-content/uploads/2021/01/NASADAD-Hilton-EI-resource-guide-3.pdf.
- 18.National Association of Counties. Addressing Youth Substance Use at the County Level 2019. https://www.naco.org/sites/default/files/documents/NACo%20Report_Addressing%20Youth%20Substance%20Abuse.pdf.
- 19.Powell BJ, Beidas RS, Lewis CC, et al. Methods to improve the selection and tailoring of implementation strategies. The journal of behavioral health services & research 2017;44(2):177–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Purtle J, Marzalik JS, Halfond RW, Bufka LF, Teachman BA, Aarons GA. Toward the data-driven dissemination of findings from psychological science. American Psychologist 2020;75(8):1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perreault WD. Controlling order-effect bias. The Public Opinion Quarterly 1975;39(4):544–551. [Google Scholar]
- 22.Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public health reports 2002;117(Suppl 1):S135. [PMC free article] [PubMed] [Google Scholar]
- 23.Wu S, Yan S, Marsiglia FF, Perron B. Patterns and social determinants of substance use among Arizona Youth: A latent class analysis approach. Children and Youth Services Review 2020;110:104769. [Google Scholar]
- 24.Purtle J, Nelson KL, Counts NZ, Yudell M. Population-Based approaches to mental health: history, strategies, and evidence. Annual Review of Public Health 2020;41:201–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dopp AR, Lantz PM. Moving upstream to improve children’s mental health through community and policy change. Administration and Policy in Mental Health and Mental Health Services Research 2019:1–9. [DOI] [PubMed] [Google Scholar]
- 26.Steele DW, Becker SJ, Danko KJ, et al. Brief behavioral interventions for substance use in adolescents: a meta-analysis. Pediatrics 2020;146(4). [DOI] [PubMed] [Google Scholar]
- 27.Committee on Substance Use and Prevention. Medication-assisted treatment of adolescents with opioid use disorders. Pediatrics 2016;138(3):e20161893. [DOI] [PubMed] [Google Scholar]
- 28.Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA pediatrics 2017;171(8):747–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saloner B, Feder KA, Krawczyk N. Closing the medication-assisted treatment gap for youth with opioid use disorder. JAMA pediatrics 2017;171(8):729–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gaither JR, Shabanova V, Leventhal JM. US national trends in pediatric deaths from prescription and illicit opioids, 1999–2016. JAMA network open 2018;1(8):e186558–e186558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chadi N, Hadland SE. Youth Access to Naloxone: The Next Frontier? Journal of Adolescent Health 2019;65(5):571–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jimenez DE, Singer MR, Adesman A. Availability of naloxone in pharmacies and knowledge of pharmacy staff regarding dispensing naloxone to younger adolescents. Journal of Adolescent Health 2019;65(5):698–701. [DOI] [PubMed] [Google Scholar]
- 33.Stokes DC, Purtle J, Meisel ZF, Agarwal AK. State Legislators’ Divergent Social Media Response to the Opioid Epidemic from 2014 to 2019: Longitudinal Topic Modeling Analysis. Journal of General Internal Medicine 2021; 29:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nelson KL, Purtle J. Factors associated with state legislators’ support for opioid use disorder parity laws. International Journal of Drug Policy 2020;82:102792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Norton WE, Chambers DA. Unpacking the complexities of de-implementing inappropriate health interventions. Implementation Science 2020;15(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prasad V, Ioannidis JP. Evidence-based de-implementation for contradicted, unproven, and aspiring healthcare practices Springer; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nilsen P, Ingvarsson S, Hasson H, von Thiele Schwarz U, Augustsson H. Theories, models, and frameworks for de-implementation of low-value care: A scoping review of the literature. Implementation Research and Practice 2020;1:2633489520953762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McKay VR, Morshed AB, Brownson RC, Proctor EK, Prusaczyk B. Letting go: Conceptualizing intervention de‐implementation in public health and social service settings. American journal of community psychology 2018;62(1–2):189–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levy S. Youth and the opioid epidemic. Pediatrics 2019;143(2):e20182752. [DOI] [PubMed] [Google Scholar]
- 40.Hoge MA, Stuart GW, Morris J, Flaherty MT, Paris M Jr, Goplerud E. Mental health and addiction workforce development: Federal leadership is needed to address the growing crisis. Health Affairs 2013;32(11):2005–2012. [DOI] [PubMed] [Google Scholar]
- 41.Purtle J, Brownson RC, Proctor EK. Infusing science into politics and policy: The importance of legislators as an audience in mental health policy dissemination research. Administration and Policy in Mental Health and Mental Health Services Research 2017;44(2):160–163. [DOI] [PubMed] [Google Scholar]
- 42.Purtle J, Dodson EA, Nelson K, Meisel ZF, Brownson RC. Legislators’ sources of behavioral health research and preferences for dissemination: variations by political party. Psychiatric services 2018;69(10):1105–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Meisel ZF, Mitchell J, Polsky D, et al. Strengthening partnerships between substance use researchers and policy makers to take advantage of a window of opportunity. Substance abuse treatment, prevention, and policy 2019;14(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Purtle J, Lê-Scherban F, Wang X, Shattuck PT, Proctor EK, Brownson RC. Audience segmentation to disseminate behavioral health evidence to legislators: an empirical clustering analysis. Implementation Science 2018;13(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Purtle J, Nelson KL, Bruns EJ, Hoagwood KE. Dissemination strategies to accelerate the policy impact of children’s mental health services research. Psychiatric services 2020;71(11):1170–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murphy SM, Polsky D. Economic evaluations of opioid use disorder interventions. Pharmacoeconomics 2016;34(9):863–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.French MT, Zavala SK, McCollister KE, Waldron HB, Turner CW, Ozechowski TJ. Cost-effectiveness analysis of four interventions for adolescents with a substance use disorder. Journal of substance abuse treatment 2008;34(3):272–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saldana L, Chamberlain P, Bradford WD, Campbell M, Landsverk J. The cost of implementing new strategies (COINS): a method for mapping implementation resources using the stages of implementation completion. Children and youth services review 2014;39:177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoomans T, Severens JL. Economic evaluation of implementation strategies in health care Springer; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hoagwood KE, Purtle J, Spandorfer J, Peth-Pierce R, Horwitz SM. Aligning dissemination and implementation science with health policies to improve children’s mental health. American Psychologist 2020;75(8):1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bogenschneider K, Corbett TJ. Evidence-based policymaking: Insights from policy-minded researchers and research-minded policymakers Routledge; 2011. [Google Scholar]
- 52.Fisher SH III, Herrick R. Old versus new: the comparative efficiency of mail and internet surveys of state legislators. State Politics & Policy Quarterly 2013;13(2):147–163. [Google Scholar]
- 53.Aarons GA, Brown SA, Hough RL, Garland AF, Wood PA. Prevalence of adolescent substance use disorders across five sectors of care. Journal of the American Academy of Child & Adolescent Psychiatry 2001;40(4):419–426. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


