Abstract
The incidence of the Pfannenstiel incisional hernia (IH) is the lowest of all IHs, it can occur due to patient-related factors or faulty technique in closure of the deeper layer. The use of prosthetic mesh repair is heralding a new era of tension-free herniorrhaphy, while the optimal location for its implantation remains controversial. As a result, no strategy or technique has become the gold standard for its repair. We report our first experience with an IH through Pfannenstiel in a 49-year-old obese female patient. Inlay polypropylene open mesh repair was performed. As the only complication, the patient presented with a seroma in the wound, which was aspirated, and she is currently asymptomatic with outpatient consultation follow-up. Pfannenstiel IHs have received minimal attention on the optimal surgical approach and postoperative results, making this case a good starting point for future studies.
INTRODUCTION
In 1900, Hermann Johannes Pfannenstiel (1862–1910) described a low transverse abdominal incision to prevent incisional hernia (IH); it is the incision of choice for gynecologic procedures; [1] and it is credited with the lower incidence of IH, [2, 3] it can occur due to patient-related factors or faulty technique in closure of the deeper layer [2]. The most common presentation is localized swelling and pain along the previous incision scar [4]. Small defects can be repaired anatomically, while major defects require tension-free repair using synthetic mesh [2] that decreases recurrence. [2, 5–7]. Polypropylene mesh is the implant of choice for hernia repair, but its placement on or under the rectus sheath is debatable [7, 8]. Currently, no technique has gained wide acceptance as the gold standard for the repair of IHs, and little has been published on this subject. Seroma formation is a common complication after IH repair, especially with mesh. Its frequency ranges from 30 to 50% after open mesh repair [9]. This article talks about our first experience fixing a Pfannenstiel IH (PIH) with an inlay mesh technique and a seroma that formed after the surgery.
CASE PRESENTATION
A 49-year-old obese female patient came to our outpatient clinic complaining of an inferior abdominal swelling that had been growing for the past 5 years following a hysterectomy performed through a Pfannenstiel incision due to uterine fibroid. She was a known hypertensive on amlodipine treatment. No smoking or alcoholic history was recorded.
On the physical examination, the abdomen looked full, a Pfannenstiel scar at the suprapubic region with an obvious swelling 3 cm above it was found with a visible and palpable cough impulse, and it was painful to reduce (Fig. 1). Abdominopelvic ultrasonography validated the clinical diagnosis of PIH. Blood tests, ECG and chest X-ray were all normal before surgery.
Figure 1.

Pfannenstiel incisional hernia (front view of the abdomen).
Antibiotic prophylaxis used. Intraoperatively, a hernia sac was discovered between the subcutaneous tissue and the anterior layer of the rectus sheath at around 3 cm above the pubis symphysis and 8 cm below the umbilicus, projecting through the splitting rectus fibers in the midline (Fig. 2); normal small bowels were reduced following adhesion lysis, extra sac was excised, and closed. An open inlay mesh repair was performed. A 15 x 15 cm polypropylene mesh was implanted; the fascial defect was not closed, and a continuous suture was placed all around the fascial defect to the underlaying mesh (Fig. 3). A Penrose drain was left subcutaneous.
Figure 2.
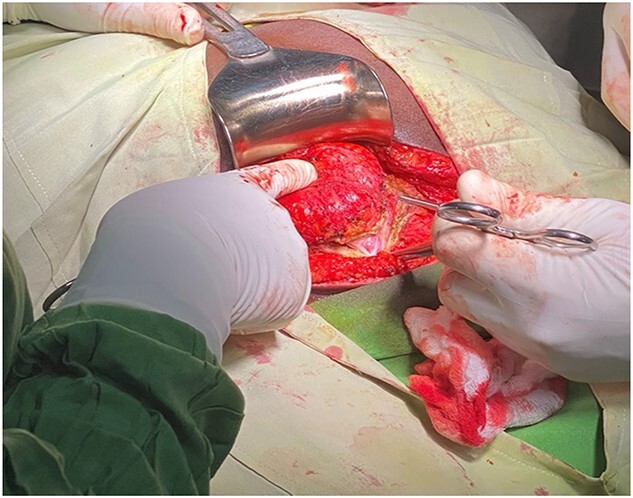
Hernia sac protruding through the splitting fibers of the rectus muscle.
Figure 3.
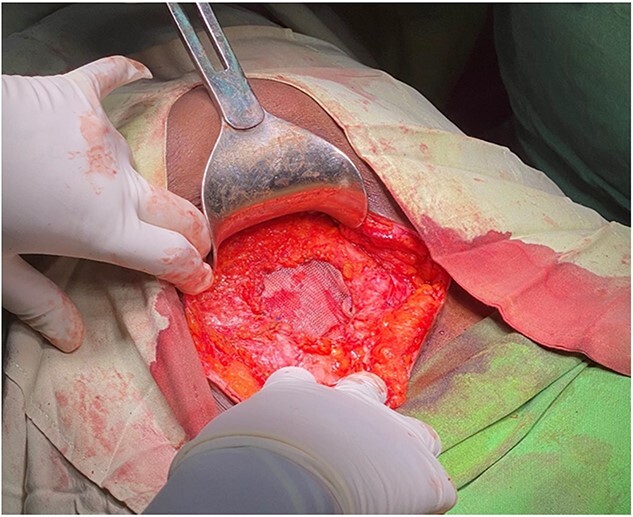
Inlay mesh fixation ended.
Non-postoperative early complications were found, drainage was removed on day 2 postoperative because it was not draining any fluid, and she was discharged home, with follow-up at day 8 postoperative where stitches were removed; on day 12 postoperative, she complained of surgical site pain and a fluctuant swelling was found on physical examination (Fig. 4); abdominal ultrasound confirmed seroma (Fig. 5). The decision to aspirate was based on the amount of fluid and the patient’s discomfort. 500 ml of serous-hematic fluid was aspirated. The patient is currently symptom-free.
Figure 4.

Front view of the patient with the seroma of the wound.
Figure 5.
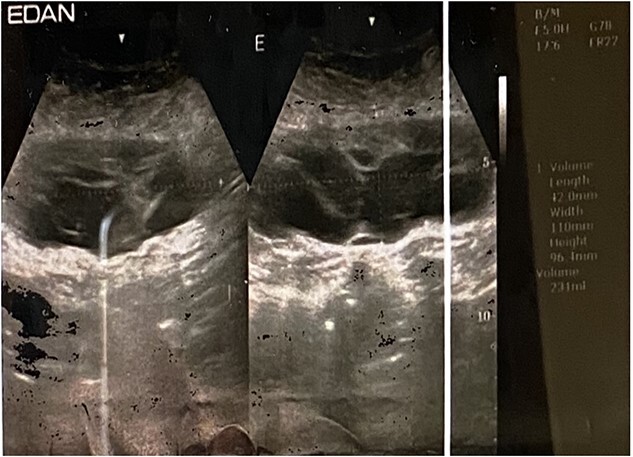
Ultrasound showing fluid collection.
DISCUSSION
IH following Pfannenstiel incision is associated with a lower incidence of 0–2% than midline incision [3]. It still occurs due to faulty technique in closure of deeper layer, age, obesity, chronic cough, prostatism, constipation, diabetes mellitus and the use of corticosteroids [2]. In the last decade, only five cases have been published in the medical literature, five in case series [10] and one case report of acute appendicitis in PIH [11]. We reported our first case in 6 years.
Repair method, mesh type and mesh plane are all important in IH repair. Positioning the mesh determines the repair’s integrity, [12] no technique or strategy has become the gold standard for it repair; [6] after the introduction of polypropylene mesh repair, recurrence rates decreased to 10–20% [12] and 8–24%, [8] heralding a new era of tension-free herniorrhaphy; [6] although there is still controversy regarding the best site of its placement [7]. Onlay and sublay repair are the two most common IH surgical methods, but it is unclear which is better. Sublay repair is associated with fewer complications and a lower recurrence rate, whereas onlay repair is associated with a higher incidence of SSI [6, 12].
Due to the difficulty of closing the hernia orifice without creating tension in our patient, we adopted the inlay approach. The inlay technique defined by Parket et al., is characterized by an approach that places the mesh within the hernia/fascial defect with the mesh fixated to the edges of the neck of the hernia. The placement of the mesh requires a bridging mesh regardless of where the mesh is fixated [12]. This technique can be performed open, as we did in our patient, as well as minimally invasively. A systemic review reported an infection rate of 12% and a mean hematoma/seroma rate of 12.2%, which did not significantly differ among the other techniques; the hernia recurrence rate was 21.6%, showing the highest hernia recurrence rate [13]. Seroma is a common complication after mesh repair. 30–50% of open mesh repairs result in seroma [9]. Most seromas develop above the mesh. The mean incidence of seroma in reported series at a range of 4–8 weeks is 11.4%; [12] Our diagnosis came 12 days after surgery. Seroma rarely causes long-term morbidity, whether aspirated or allowed to settle. Aspiration may increase mesh infection risk, although it is recommended if they grow or persist [12] as we did in our case due to the patient’s size and discomfort.
PIH is extremely rare and has received little attention regarding its best surgical approach and postoperative implications, so it is necessary to delve deeper into the subject, making this case an excellent starting point for future research. The inlay technique could be taken into consideration, especially in defects that cannot be closed, and the available mesh is not big.
FUNDING
I declare that I have not received any financial support.
Contributor Information
Barbara Yordanis Hernandez Cervantes, Department of Surgery, School of Medicine, University of Health and Allied Sciences, Ho, Volta Region, Ghana.
Fernando Almager Acevedo, Department of Surgery, School of Medicine, University of Health and Allied Sciences, Ho, Volta Region, Ghana.
Duniesky Martinez Lopez, Department of Internal Medicine and Therapeutics, School of Medicine, University of Health and Allied Sciences, Ho, Volta Region, Ghana.
Radisnay Guzman Lambert, Department of Surgery, School of Medicine, University of Health and Allied Sciences, Ho, Volta Region, Ghana.
Mariuska Rodriguez Gonzalez, Department of Internal Medicine and Therapeutics, School of Medicine, University of Health and Allied Sciences, Ho, Volta Region, Ghana.
CONFLICT OF INTEREST STATEMENT
No conflict of interest present.
References
- 1. Luijendijk RW, Jeekel J, Storm RK, Schutte PJ, Hop WC, Drogendijk AC, et al. The low transverse Pfannenstiel incision and the prevalence of incisional hernia and nerve entrapment. Ann Surg 1997;225:365–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thekdi PI, Sutariya PK. Unusual presentation of two defects in a non-vertical incisional hernia. Int J Res Med 2013;2:189–19. [Google Scholar]
- 3. Kerstin B, Johanna Ö, Mats L, et al. Incisional hernias following open gynecological surgery: a population-based study. Arch Gynecol Obstet 2019;299:1313–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bakale N, Suryawanshi SA. A study of etiology, clinical presentation, and management of incisional hernia. Int J Surg Sci 2021;5:626–9. [Google Scholar]
- 5. Kshirsagar AY, Patil RK, Chotai T, Bane P, Agarwal S, Patil M. Case series of complicated incisional hernia. Int J Sci Res Publ 2013;3:1–3. [Google Scholar]
- 6. Saber A, Bayumi EK. Onlay versus sublay mesh repair for ventral hernia. J Surg 2015;4:1–4. [Google Scholar]
- 7. Raghuveer MN, Muralidhar S, Shetty H, Veena V. Onlay versus sublay mesh repair for ventral hernia. Int Surg J 2018;5:823–6. [Google Scholar]
- 8. Memon AA, Khan A, Zafar H, Murtaza G, Zaidi M. Repair of large and giant incisional hernia with onlay mesh: perspective of a tertiary care hospital of a developing country. Int J Surg 2013;11:41–5. [DOI] [PubMed] [Google Scholar]
- 9. Ibrahim R, Abounozha S, Kheder A, Alshahri T. Incidence of seroma in sublay versus onlay mesh repair of incisional hernia. Ann Med Surg 2021;61:155–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Patil A, Davies HO, Coulston J, Alves R, Chambers A, Lawrence R. Atypical incisional hernia following Pfannenstiel incision. Hernia 2013;17:479–82. [DOI] [PubMed] [Google Scholar]
- 11. Paudyal N, Sah S. Incisional hernia appendicitis: a unique case report. Int J Surg Case Rep 2021;89:106549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alimi Y, Merle C, Sosin M, Mahan M, Bhanot P. Mesh, and plane selection: a summary of options and outcomes. Plast Aesthet Res 2020;7:5. [Google Scholar]
- 13. Sosin M, Nahabedian MY, Bhanot P. The perfect plane: a systematic review of mesh location and outcomes. Plast Reconstr Surg 2018;142:S107–16. [DOI] [PubMed] [Google Scholar]


