Abstract
Diabetic neuropathy (DN) is one of the most prevalent and expensive microvascular consequences of diabetes mellitus (DM), which is noteworthy given that it is frequently both underdiagnosed and undertreated in daily clinical practice. The aim of the current article was to review the efficiency of vitamin B12 supplementation in isolation or in combination therapy for the treatment of diabetic peripheral neuropathy. This meta-analysis was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). A systematic electronic search was performed in PubMed and Cochrane Library to identify randomized controlled trials (RCTs) assessing the impact of vitamin B12 outcomes in patients with diabetic neuropathy without putting restrictions on the year of publication. A combination of the following keywords was used: “diabetic neuropathy,” “vitamin B12,” and “outcomes.” The primary outcomes assessed in the current meta-analysis included neuropathic symptoms and vibration perception threshold (VPT). Secondary outcomes included a change in pain score from baseline, total cholesterol (mg/dL), high-density lipoprotein (HDL), and low-density lipoprotein (LDL). A total of six articles were selected to be included in the current meta-analysis. Patients receiving vitamin B12 showed a greater reduction of mean neuropathic symptoms (standardized mean difference (SMD): -0.39, 95% confidence interval (CI): -0.73, -0.05, p-value: 0.03) and pain score (SMD: -3.60, 95% CI: -4.68, -1.43, p-value<0.001) compared to the control group. No significant effect of vitamin B12 was found on VPT (mean difference (MD): -4.80, 95% CI: -11.03, 1.42, p-value: 0.13), change in HDL (MD: 0.14, 95% CI: -2.37, 2.65, p-value: 0.91), LDL (MD: 2.59, 95% CI: -5.94, 11.12, p-value: 0.55), and total cholesterol (MD: -2.72, 95% CI: -11.52, 6.08, p-value: 0.54). The current meta-analysis found that vitamin B12 can improve neuropathic symptoms and reduce pain in patients with diabetic neuropathy. However, the current study did not report any significant difference between patients who received vitamin B12 and placebo in terms of HDL, LDL, and total cholesterol.
Keywords: meta-analysis, neuropathic symptoms, diabetes, vitamin b12, diabetic neuropathy
Introduction and background
Diabetic neuropathy (DN) is one of the most prevalent and expensive microvascular consequences of diabetes mellitus (DM), which is noteworthy given that it is frequently both underdiagnosed and undertreated in daily clinical practice [1]. Nearly 59% of patients with type 1 diabetes mellitus and 50% of patients with type 2 diabetes mellitus develop diabetic peripheral neuropathy [2]. Some diabetic peripheral neuropathy patients may have excruciatingly painful symptoms, but people with more severe neuropathic deficits might not experience any symptoms [3]. More than 30% of patients develop peripheral diabetic neuropathy with pain and symptoms such as needles, pins, burning and hot or cold sensations, dead feeling and numbness in the contact, and leg and foot pain [4,5]. These can have a significant impact on the quality of life [4].
Lack of methylcobalamin, which is caused by a deficiency in vitamin B12, has been linked to substantial neurological disease, particularly peripheral neuropathy [6]. It also heralds the beginning of diabetic neuropathy. Vitamin B12 insufficiency in diabetic peripheral neuropathic patients may result from the utilization of antidiabetic medications such as metformin [7]. Along with any kind of anti-glycemic therapy pointing at strict glycemic control, vitamin B12 has been the commonly used supplement because vitamin deficiency of vitamin B12 is common in type 2 diabetic patients. Besides this, a deficiency of vitamin B12 is more likely to cause neurological symptoms such as painful neuropathy and autonomic neuropathy [1-8]. Vitamin B12 is regarded as an analgesic medication in several nations. In the descending inhibitory nociceptive system, it has been hypothesized that vitamin B12 may improve the availability and potency of noradrenaline and 5-hydroxytryptamine [9].
The American Diabetes Association (ADA) suggests that patients with diabetic neuropathy on metformin therapy have their vitamin B12 levels periodically checked once a year [10]. The usage of metformin has been primarily attributed to the deficiency of vitamin B12 in type 2 diabetes mellitus. Since more than 40 years ago, there has been evidence linking metformin to a deficiency of vitamin B12. Several interventional investigations, observational studies, and meta-analyses have supported this association [11,12].
As far as our knowledge is concerned, no previous meta-analysis has been conducted to determine the efficiency of vitamin B12 in patients with diabetic neuropathy. Clinical trials assessing the impact of vitamin B12 enrolled a small sample size. Thus, the current meta-analysis was conducted to assess the impact of vitamin B12 in patients with diabetic neuropathy using a large sample size. The current article aimed to review the efficiency of vitamin B12 supplementation in isolation or combination therapy for the treatment of diabetic peripheral neuropathy.
Review
Methodology
This meta-analysis was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Search Strategy and Study Selection
A systematic electronic search was performed in PubMed and Cochrane Library to identify randomized controlled trials (RCTs) assessing the impact of vitamin B12 outcomes in patients with diabetic neuropathy without putting restrictions on the year of publication. A combination of the following keywords was used: “diabetic neuropathy,” “vitamin B12,” and “outcomes.” The title and abstract were screened for relevancy, and the full text of relevant articles was retrieved to assess for eligibility. The reference lists of all eligible studies were manually screened to search for additional studies. The selection of studies was done by two authors independently.
Studies that assessed any type of vitamin B12 therapy, including coenzyme forms of vitamin B12, in either injection or oral form were eligible to be included in the current meta-analysis. Studies involving combination therapy, for example, if vitamin B12 or its coenzyme forms was one of the treatment agents along with other therapies, were also included in this meta-analysis. Studies involving diabetic neuropathy were part of this meta-analysis. Peripheral large or small fiber neuropathy that causes autonomic or somatic sensory problems is known as diabetic neuropathy. Studies other than RCTs were not included in the current meta-analysis. Besides this, studies that did not report desired outcomes were also not included in the current meta-analysis. Studies published in a language other than English were also not included.
Outcomes
The primary outcomes assessed in the current meta-analysis included neuropathic symptoms and vibration perception threshold (VPT). Neuropathic symptoms were assessed using the Michigan Neuropathy Screening Instrument Questionnaire (MNSIQ) and Neuropathy Symptom Score (NSS). VPT is a simple way of detecting large fiber dysfunction, thus identifying individuals with diabetes at risk of ulceration. Secondary outcomes included a change in pain score from baseline, total cholesterol (mg/dL), high-density lipoprotein (HDL), and low-density lipoprotein (LDL).
Data Extraction
Data were extracted from included studies using predesigned data extraction forms. Data from the included studies were extracted by one author and double-checked and entered into Review Manager (RevMan) software (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) by the second author. Data extracted included author name, publication year, groups, sample size, follow-up period, mean age, and gender.
Risk of Assessment
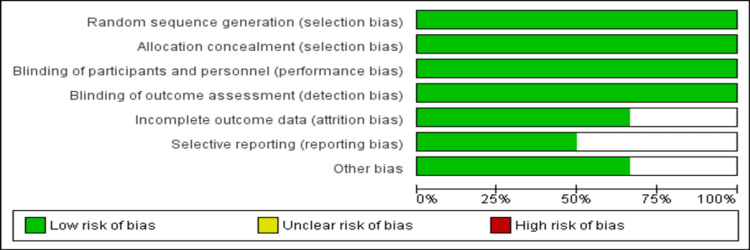
The risk of bias in the current meta-analysis was assessed using the Cochrane risk of bias assessment. The risk of bias was assessed by two authors independently. The risk of bias tool covers six domains of bias including “selection bias,” “performance bias,” “detection bias,” “attrition bias,” “reporting bias,” and “other bias.” Any disagreement between the two authors was resolved through discussion.
Statistical Analysis
Review Manager (RevMan) version 5.4.0 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) was used to perform a meta-analysis. A standardized mean difference (SMD) along with a 95% confidence interval (95% CI) was reported to estimate the effect of vitamin B12 on the improvement of neuropathic symptoms, VPT, and pain score. To estimate the effect of vitamin B12 on HDL, LDL, and total cholesterol, the mean difference (MD) and 95% CI were computed. Heterogeneity among the study results was calculated by calculating I-square statistics. In the case of an I-square value of <50%, a fixed-effect model was used.
Results
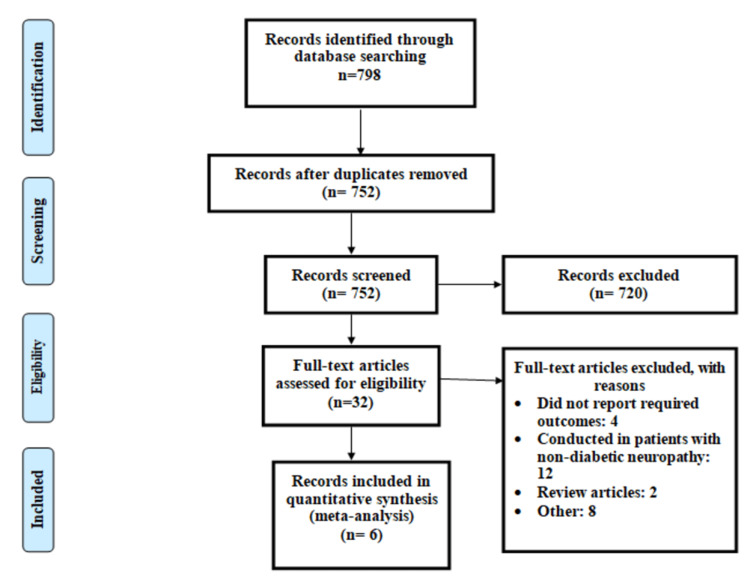
The process of study selection is summarized in Figure 1. Out of 798 articles identified through online searching, title and abstract screening of 752 articles was done to assess for eligibility. Out of 752 articles, 32 articles were retrieved for full-text screening. Six articles were selected to be included in the current meta-analysis [13-18]. Table 1 shows the characteristics of the included studies.
Table 1. Characteristics of the included studies.
SOD: superoxide dismutase; ALA: alpha lipoic acid; ALC: acetyl-carnitine
| Author name | Publication year | Groups | Intervention | Sample size | Follow-up (months) | Mean age (years) | Males (number (%)) |
| Didangelos et al. [13] | 2020 | Vitamin B | SOD, ALA, vitamin B12, and ALC | 43 | 18 | 64.23 | 44 (51.76) |
| Placebo | 42 | ||||||
| Didangelos et al. [14] | 2021 | Vitamin B | Vitamin B12 | 44 | 12 | 62.85 | 48 (53.33) |
| Placebo | 46 | ||||||
| Farvid et al. [15] | 2011 | Vitamin B | Minerals, vitamin B1, vitamin B2, vitamin B6, biotin, vitamin B12, and folic acid | 22 | 4 | 53.55 | 23 (52.27) |
| Placebo | 22 | ||||||
| Fonseca et al. [16] | 2013 | Vitamin B | Methylfolate calcium, methylcobalamin, and pyridoxal-5-phosphate | 106 | 6 | 62.62 | 148 (69.16) |
| Placebo | 108 | ||||||
| Li et al. [17] | 2016 | Vitamin B | Vitamin B12 | 115 | 6 | 57.78 | 122 (52.59) |
| ALC | 117 | ||||||
| Stracke et al. [18] | 1996 | Vitamin B | Vitamin B1, vitamin B6, and vitamin 12 | 11 | 3 | 59 | 14 (58.33) |
| Placebo | 13 |
Figure 1. PRISMA flowchart of the selection of studies.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
The pooled mean age of patients was 60.45 years. The majority of patients were males in all the included studies. In four RCTs, vitamin B12 was given in combination with other vitamins and minerals [13,15,16,18], while in two studies, vitamin B12 was given alone [12,17]. Figure 2 shows the overall risk of bias assessment. The overall quality of the study was high.
Figure 2. Assessment of risk of bias.
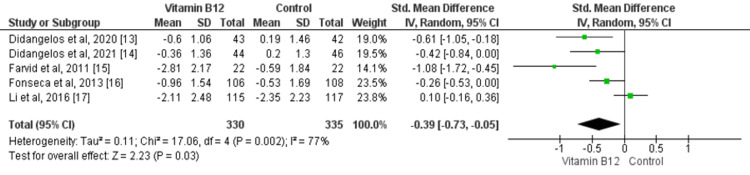
A meta-analysis of the effect of vitamin B12 on neuropathic symptoms is shown in Figure 3. Overall, five studies assessed the effect of vitamin B12 on neuropathic symptoms [13-17]. Patients who received vitamin B12 showed a greater reduction of mean neuropathic symptoms compared to the control group (SMD: -0.39, 95% CI: -0.73, -0.05, p-value: 0.03). Significant heterogeneity was found among the study results (I-square: 77%, p-value: 0.02).
Figure 3. Forest plot of the association between vitamin B12 supplementation and neuropathic symptoms.
SD: standard deviation; 95% CI: 95% confidence interval
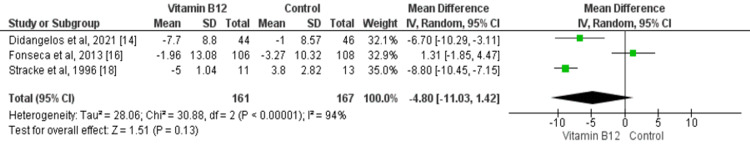
Three studies assessed the impact of vitamin B12 supplementation on VPT [14,16,18]. The random effect model showed that no significant effect of vitamin B12 was found on VPT (mean difference: -4.80, 95% CI: -11.03, 1.42, p-value: 0.13) as shown in Figure 4. Significant heterogeneity was found among the study results (I-square: 94%, p-value: 0.001).
Figure 4. Forest plot of the association between vitamin B12 supplementation and VPT.
VPT: vibration perception threshold; SD: standard deviation; 95% CI: 95% confidence interval
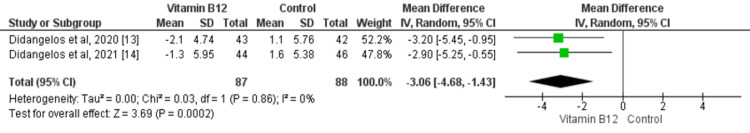
Two studies compared the impact of vitamin B12 on the change in pain score between patients who received vitamin B12 and patients who received placebo [13,14]. Patients who received vitamin B12 experienced greater pain reduction scores compared to patients who received placebo (SMD: -3.60, 95% CI: -4.68, -1.43, p-value<0.001) as shown in Figure 5. No significant heterogeneity was found among the study results (I-square: 0%, p-value: 0.86).
Figure 5. Forest plot of the association between vitamin B12 supplementation and pain score.
SD: standard deviation; 95% CI: 95% confidence interval
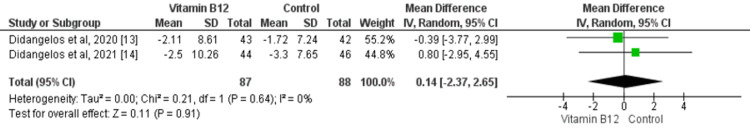
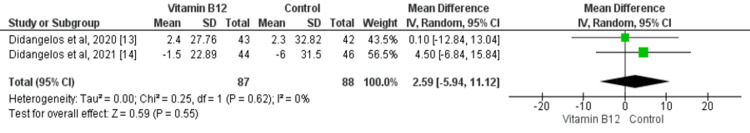
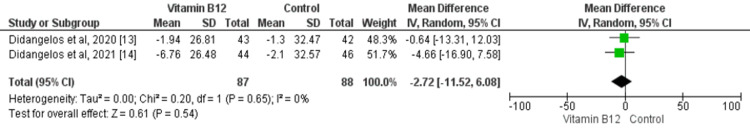
Two studies assessed the impact of vitamin B12 on HDL, LDL, and total cholesterol in patients with diabetic neuropathy. No significant differences were found between two groups in terms of change in HDL (mean difference: 0.14, 95% CI: -2.37, 2.65, p-value: 0.91), LDL (mean difference: 2.59, 95% CI: -5.94, 11.12, p-value: 0.55), and total cholesterol (mean difference: -2.72, 95% CI: -11.52, 6.08, p-value: 0.54) as shown in Figure 6, Figure 7, and Figure 8, respectively. No significant heterogeneity was found among the study results in any of the outcomes.
Figure 6. Forest plot of the association between vitamin B12 supplementation and HDL change.
HDL: high-density lipoprotein; SD: standard deviation; 95% CI: 95% confidence interval
Figure 7. Forest plot of the association between vitamin B12 supplementation and LDL change.
LDL: low-density lipoprotein; SD: standard deviation; 95% CI: 95% confidence interval
Figure 8. Forest plot of the association between vitamin B12 supplementation and total cholesterol change.
SD: standard deviation; 95% CI: 95% confidence interval
Discussion
The current meta-analysis provided an updated overview of the impact of vitamin B12 on clinical outcomes in patients with diabetic neuropathy. The current meta-analysis showed that patients who received B12 alone or in combination with other drugs experience a greater reduction of mean neuropathic symptoms compared with placebo. In addition, they experienced greater pain reduction scores compared to patients who received placebo.
Diabetic neuropathy is a serious complication of type 2 diabetes mellitus, and it can lead to devastating symptoms such as unbearable and unremitting pain and can have severe life-threatening outcomes including the “diabetic foot” [19]. Strict glycemic control is now the only known non-symptomatic treatment for diabetic neuropathy; however, its effectiveness in treating diabetic peripheral neuropathy is quite limited, and it must be maintained for years [20]. Thus, there is an urgent requirement for an efficient drug therapy that would act casually through the modification of the diabetic neuropathy pathophysiology. Among other supplements and drugs such as superoxide dismutase, folate, carnitine, and alpha lipoic acid, vitamin B12 has been the most often used drug [21]. This is due to the fact that deficiency of vitamin B12 is commonly found in individuals with type 2 diabetes mellitus, and deficiency of vitamin B12 may lead to several neurological disorders accelerating diabetic neuropathy [22].
The current meta-analysis supported the point that vitamin B12 resulted in an improvement in pain. A systematic review conducted by Li et al. showed similar effects [23]. These findings can assure the analgesic action of vitamin B12 that is potentially arbitrated by a rise in the effectiveness and availability of 5-hydroxytryptamine and noradrenaline [24]. Vitamin B12 occurs in different forms called cobalamins. The main form of cobalamin utilized in vitamin supplements is cyanocobalamin, while methylcobalamin is a coenzyme form that is a crucial cofactor for the function of vitamin B12-dependent methyltransferases [25].
Among five studies that assessed the improvement of neuropathic symptoms, a study conducted by Li et al. [17] found no significant difference in relation to neuropathic symptom improvements. This study used acetyl-L-carnitine (ALC) as a control group and reported that in both groups (vitamin B12 and ALC), neuropathic symptom score was significantly lower at 24 weeks as compared to the baseline [18], and no significant difference was observed between the two groups. Another study that used vitamin B12 alone reported that vitamin B12 significantly reduced neuropathic symptoms [14].
The current meta-analysis is associated with certain limitations. Firstly, less number of included studies considered homocysteine levels and methylmalonic acid as potential confounders for the response of vitamin B12 therapy. Secondly, due to the lack of individual-level data, we were not able to perform subgroup analyses of age, gender, and comorbidities. Thirdly, among all the included studies, two used vitamin B12 alone, while six studies involved combination therapy in which one of the components was vitamin B12. Besides this, there was a great variation in these studies in terms of mode of administration, molecular form, dose, duration of follow-up, and baseline blood levels. Lastly, only six studies were included in the current meta-analysis, and the sample size is relatively small in all the included studies, which impacts the power of the study findings. However, this is the first meta-analysis conducted on the impact of vitamin B12 on clinical outcomes in patients with diabetic neuropathy that can give some idea of the utilization of vitamin B12 in patients with diabetic neuropathy. In the future, more prospective randomized controlled trials are required to guide clinical practice.
Conclusions
The current meta-analysis was conducted with the aim to assess the impact of vitamin B12 alone or in combination with other treatments in patients with diabetic neuropathy. The current meta-analysis found that vitamin B12 can improve neuropathic symptoms and reduce pain in patients with diabetic neuropathy. However, the current study did not report any significant difference between patients who received vitamin B12 and placebo in terms of HDL, LDL, and total cholesterol.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Diabetic neuropathies: a statement by the American Diabetes Association. Boulton AJ, Vinik AI, Arezzo JC, et al. Diabetes Care. 2005;28:956–962. doi: 10.2337/diacare.28.4.956. [DOI] [PubMed] [Google Scholar]
- 2.Diabetic neuropathies. Russell JW, Zilliox LA. Continuum (Minneap Minn) 2014;20:1226–1240. doi: 10.1212/01.CON.0000455884.29545.d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vitamin B supplementation for diabetic peripheral neuropathy. Jayabalan B, Low LL. Singapore Med J. 2016;57:55–59. doi: 10.11622/smedj.2016027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Painful diabetic neuropathy: clinical aspects. Didangelos T, Doupis J, Veves A. Handb Clin Neurol. 2014;126:53–61. doi: 10.1016/B978-0-444-53480-4.00005-9. [DOI] [PubMed] [Google Scholar]
- 5.Update on the neurophysiology of pain transmission and modulation: focus on the NMDA-receptor. Bennett GJ. J Pain Symptom Manage. 2000;19:0–6. doi: 10.1016/s0885-3924(99)00120-7. [DOI] [PubMed] [Google Scholar]
- 6.Vitamin B12 (cobalamin) deficiency in elderly patients. Andrès E, Loukili NH, Noel E, et al. CMAJ. 2004;171:251–259. doi: 10.1503/cmaj.1031155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Risk factors of vitamin B(12) deficiency in patients receiving metformin. Ting RZ, Szeto CC, Chan MH, Ma KK, Chow KM. Arch Intern Med. 2006;166:1975–1979. doi: 10.1001/archinte.166.18.1975. [DOI] [PubMed] [Google Scholar]
- 8.Vitamin B12 deficiency is associated with cardiovascular autonomic neuropathy in patients with type 2 diabetes. Hansen CS, Jensen JS, Ridderstråle M, Vistisen D, Jørgensen ME, Fleischer J. J Diabetes Complications. 2017;31:202–208. doi: 10.1016/j.jdiacomp.2016.08.025. [DOI] [PubMed] [Google Scholar]
- 9.[Analgesic and analgesia-potentiating action of B vitamins] [Article in German] Jurna I. Schmerz. 1998;12:136–141. doi: 10.1007/s004829800054. [DOI] [PubMed] [Google Scholar]
- 10.Influence of duration and dose of metformin on cobalamin deficiency in type 2 diabetes patients using metformin. Beulens JW, Hart HE, Kuijs R, Kooijman-Buiting AM, Rutten GE. Acta Diabetol. 2015;52:47–53. doi: 10.1007/s00592-014-0597-8. [DOI] [PubMed] [Google Scholar]
- 11.Long-term metformin use and vitamin B12 deficiency in the Diabetes Prevention Program outcomes study. Aroda VR, Edelstein SL, Goldberg RB, et al. J Clin Endocrinol Metab. 2016;101:1754–1761. doi: 10.1210/jc.2015-3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diabetes as a cause of clinically significant functional cobalamin deficiency. Solomon LR. Diabetes Care. 2011;34:1077–1080. doi: 10.2337/dc11-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Efficacy and safety of the combination of superoxide dismutase, alpha lipoic acid, vitamin B12, and carnitine for 12 months in patients with diabetic neuropathy. Didangelos T, Karlafti E, Kotzakioulafi E, Kontoninas Z, Margaritidis C, Giannoulaki P, Kantartzis K. Nutrients. 2020;12 doi: 10.3390/nu12113254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vitamin B12 supplementation in diabetic neuropathy: a 1-year, randomized, double-blind, placebo-controlled trial. Didangelos T, Karlafti E, Kotzakioulafi E, et al. Nutrients. 2021;13 doi: 10.3390/nu13020395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Improving neuropathy scores in type 2 diabetic patients using micronutrients supplementation. Farvid MS, Homayouni F, Amiri Z, Adelmanesh F. Diabetes Res Clin Pract. 2011;93:86–94. doi: 10.1016/j.diabres.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Metanx in type 2 diabetes with peripheral neuropathy: a randomized trial. Fonseca VA, Lavery LA, Thethi TK, et al. Am J Med. 2013;126:141–149. doi: 10.1016/j.amjmed.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 17.Effects of acetyl-L-carnitine and methylcobalamin for diabetic peripheral neuropathy: a multicenter, randomized, double-blind, controlled trial. Li S, Chen X, Li Q, et al. J Diabetes Investig. 2016;7:777–785. doi: 10.1111/jdi.12493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.A benfotiamine-vitamin B combination in treatment of diabetic polyneuropathy. Stracke H, Lindemann A, Federlin K. Exp Clin Endocrinol Diabetes. 1996;104:311–316. doi: 10.1055/s-0029-1211460. [DOI] [PubMed] [Google Scholar]
- 19.Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Tesfaye S, Boulton AJ, Dyck PJ, et al. Diabetes Care. 2010;33:2285–2293. doi: 10.2337/dc10-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Improvement in neuropathy outcomes with normalizing HbA1c in patients with type 2 diabetes. Ishibashi F, Taniguchi M, Kosaka A, Uetake H, Tavakoli M. Diabetes Care. 2019;42:110–118. doi: 10.2337/dc18-1560. [DOI] [PubMed] [Google Scholar]
- 21.Nutritional management of patients with diabetic peripheral neuropathy with L-methylfolate-methylcobalamin-pyridoxal-5-phosphate: results of a real-world patient experience trial. Trippe BS, Barrentine LW, Curole MV, Tipa E. Curr Med Res Opin. 2016;32:219–227. doi: 10.1185/03007995.2015.1103215. [DOI] [PubMed] [Google Scholar]
- 22.Effects of oral crystalline cyanocobalamin 1000 μg/d in the treatment of pernicious anemia: an open-label, prospective study in ten patients. Andrès E, Henoun Loukili N, Noel E, et al. Curr Ther Res Clin Exp. 2005;66:13–22. doi: 10.1016/j.curtheres.2005.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Acetyl-L-carnitine in the treatment of peripheral neuropathic pain: a systematic review and meta-analysis of randomized controlled trials. Li S, Li Q, Li Y, Li L, Tian H, Sun X. PLoS One. 2015;10:0. doi: 10.1371/journal.pone.0119479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vitamin B12 for herpetic neuralgia: a meta-analysis of randomised controlled trials. Wang JY, Wu YH, Liu SJ, Lin YS, Lu PH. Complement Ther Med. 2018;41:277–282. doi: 10.1016/j.ctim.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 25.Holotranscobalamin, a marker of vitamin B-12 status: analytical aspects and clinical utility. Nexo E, Hoffmann-Lücke E. Am J Clin Nutr. 2011;94:359–365. doi: 10.3945/ajcn.111.013458. [DOI] [PMC free article] [PubMed] [Google Scholar]