Abstract
Proliferative diabetic retinopathy (PDR) is a world-wide leading cause of blindness among adults and may be associated with the influence of genetic factors. It is significant to search for genetic biomarkers of PDR. In our study, we collected genomic data about PDR from gene expression omnibus (GEO) database. Differentially expressed gene (DEG) analysis and weighted gene co-expression network analysis (WGCNA) were carried out. The gene module with the highest gene significance (GS) was defined as the key module. Hub genes were identified by Venn diagram. Then we verified the expression of hub genes in validation data sets and built a diagnostic model by least absolute shrinkage and selection operator (LASSO) regression. Enrichment analysis, including gene ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG), gene set enrichment analysis (GSEA) and construction of a protein–protein interaction (PPI) network were conducted. In GSE60436, we identified 466 DEGs. WGCNA established 14 gene modules, and the blue module (GS = 0.64), was the key module. Interferon (IFN)-induced protein 44-like (IFI44L) and complement C1q tumor necrosis factor-related protein 5 (C1QTNF5) were identified as hub genes. The expression of hub genes in GEO datasets was verified and a diagnostic model was constructed by LASSO as follows: index = IFI44L * 0.0432 + C1QTNF5 * 0.11246. IFI44L and C1QTNF5 might affect the disease progression of PDR by regulating metabolism-related and inflammatory pathways. IFI44L and C1QTNF5 may play important roles in the disease process of PDR, and a LASSO regression model suggested that the 2 genes could serve as promising biomarkers of PDR.
Keywords: proliferative diabetic retinopathy, biomarker, IFI44L, C1QTNF5, LASSO, WGCNA
1. Introduction
Diabetes retinopathy (DR) is a major complication of diabetes and the leading cause of blindness in adults.[1,2] As of 2019, there were about 463 million people with diabetes worldwide, and up to 35% of them have DR.[3] Usually, DR is classified into 2 stages: non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).[4] Some known risk factors for DR include the duration of diabetes, hyperglycemia, hypertension, and hyperlipidemia. By controlling these risk factors, many patients with DR could be effectively prevented from developing into the sight-threatening type of PDR or neovascular glaucoma (NVG).[5] However, there is still a high proportion of patients with DR whose disease progression is difficult to control. The pathogenesis of PDR is complex and involves vascular, inflammatory, and neuronal mechanisms.[6] These may be closely associated with the influence of genetic factors.[7]
With the rapid development of genomics, many genes have been found to be related to PDR, such as vascular endothelial growth factor (VEGF),[8] hypoxia-inducible factor 1-α (HIF1A),[9] erythropoietin (EPO),[10] receptor for advanced glycation end product (RAGE),[11] among others. Neovascularization is an important feature of PDR, thus anti-VEGF agents have become a promising therapy for PDR.[12] So far, anti-VEGF therapy has shown poor efficacy for diabetic macular edema (DME), another major factor affecting the prognosis of PDR,[13] and this phenomenon is likely to be related to individual genetic differences. Therefore, it is of great significance to search for genetic biomarkers of PDR.
The development of bioinformatics plays a powerful role in promoting genomics research. Gene expression omnibus (GEO, https://www.ncbi.nlm.nih.gov/geo/) is a public database that contains microarray and high-throughput genomic datasets. It also includes genomic data from human patients with PDR.[14–17] Weighted gene co-expression network analysis (WGCNA) is a well-known systems biology method to identify gene association patterns.[18] Co-expressed genes are clustered into various modules named after colors. These modules are correlated with phenotypic traits, and key genes within the networks should be found.[19] Least absolute shrinkage and selection operator (LASSO) is an effective approach for the regression of high-dimensional parameters and has been broadly applied for diagnostic and prognostic analysis.[20,21]
The objective of our research was to identify genomic biomarkers for PDR. Firstly, we searched the GEO database for genomic data of human patients with PDR. Comprehensive bioinformatics approaches, including WGCNA, were utilized to construct a gene co-expression network (GSE60436), find the key gene module and the hub genes, verify the expression of hub genes in validation datasets (GSE94019, GSE160306 and GSE178721) and analyze the enriched pathways of genes in the key module. Finally, the LASSO regression model was adopted to investigate the diagnostic value of hub genes for PDR.
2. Materials and methods
2.1. Data collection and pre-processing
By searching the GEO database using the key words “proliferative diabetic retinopathy,” we have found 4 datasets, including GSE60436, GSE94019, GSE160306 and GSE178721. GSE60436 included 6 tissues of PDR and 3 normal tissue samples, which were based on GPL6884 (Illumina HumanWG-6 v3.0 expression beadchip).[14] GSE94019 contained 9 PDR tissues and 4 normal tissues based on GPL11154 (Illumina HiSeq 2000).[15] GSE160306 included 5 PDR with DME tissues, 15 NPDR with DME tissues, 19 NPDR tissues, 20 diabetic tissues, and 20 normal tissues based on GPL20301 (Illumina HiSeq 4000).[16] GSE178721 contained 1 PDR serum sample and 1 macular hole (MH) sample based on GPL21290 (Illumina HiSeq 3000, Illumina, San Diego, CA). [17]
Expression profiles of 4 datasets were downloaded. Raw expression data of GSE60436 was obtained and further normalized by the “lumi” package in the R language.[22] Gene reads or gene counts data were acquired and transferred into counts per million (CPM) matrices using the R package “edgeR.”[23]
2.2. Screening for differentially expressed genes (DEGs)
We utilized the R package “limma” to identify the DEGs,[24] by setting the statistical threshold to P < .05 and the absolute value of fold change (FC) > 2. Volcano plots and heatmaps were drawn by the “ggplot 2” and “ggpubr” packages in R.
2.3. Weighted gene co-expression network construction
The WGCNA package in R was used to build a gene co-expression network for GSE64036.[18] We picked out 5000 genes with the largest median values at the beginning. And then we selected a soft threshold using the “pickSoftThreshold” function of the package. Afterwards, genes were classified into multiple gene modules. The gene module with the highest gene significance (GS) value was defined as the key module. Genes in the key module with module membership (MM) > 0.9 and GS > 0.3 were considered interesting genes.
2.4. Identification and verification of hub genes
Hub genes were identified by the overlapping of DEGs in GSE60436 and interesting genes in the key module. And we further verified the expression of hub genes in GSE94019, GSE160306 and GSE178721. We generated Venn diagrams using the Venny tool (https://bioinfogp.cnb.csic.es/tools/venny/index.html) and generated violin plots and box plots using the R packages “ggstatsplot” and “ggpubr.”
2.5. Functional enrichment analysis of key module
Gene ontology (GO) enrichment analysis and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis of genes in the key module were performed using the R package “ClusterProfiler.”[25] Gene set enrichment analysis (GSEA) and gene set variation analysis (GSVA) are popular tools for analyzing pathways enriched in gene expression profiles. We ran GSVA analysis of GSE60436 by the “GSVA” package in R.[26] Additionally, samples from GSE94019 were divided into high-expression groups and low-expression groups according to the expression levels of single hub genes, and GSEA analysis was performed by the “ClusterProfiler” package.
2.6. Construction of a protein–protein interaction (PPI) network
Genes in the key module were imported into the STRING database (https://string-db.org/).[27] A PPI network was constructed in the Cytoscape software.[28] And we calculated and visualized the Maximum Neighborhood Component (MCC) value of each node in the PPI network by the “Cytohubba” plugin.[29]
2.7. Construction of LASSO model and receiver operating characteristic (ROC) curve analysis
Firstly, GSE94019 and GSE160306 were combined and then randomly assigned to the training set (70%) and the test set (30%). Then we constructed the LASSO model by using the “glmnet” package in R.[30] Using the regression coefficients from LASSO, a model index to weight the expression of hub genes was established with the formula: index = Gene1 * Coefficient1 + Gene2 * Coefficient2. R package “pROC” was utilized to generate ROC curve diagrams in the training set and the test set.[31]
3. Results
3.1. Identification of DEGs in PDR
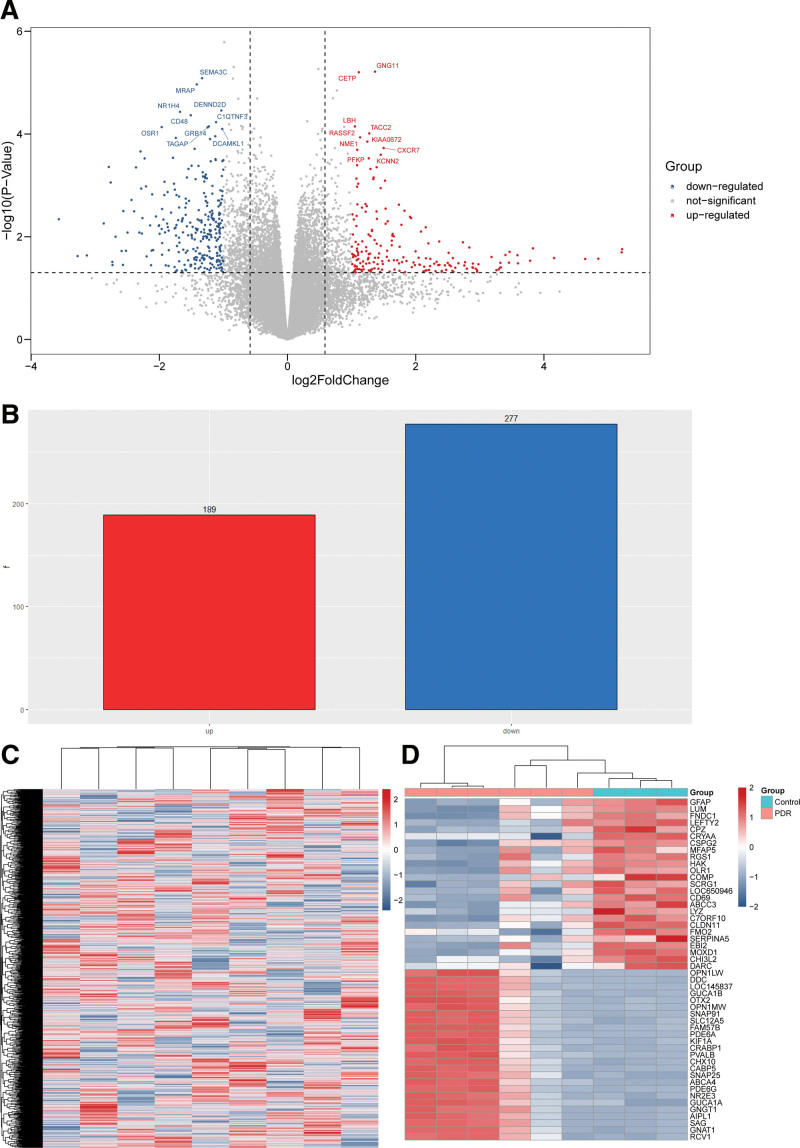
In GSE60436, there were 466 DEGs in the PDR tissue samples compared to control samples, including 189 upregulated genes (RCV1, GNAT1, SAG, AIPL1, GNGT1, among others) and 277 downregulated genes (GFAP, LUM, FNDC1, LEFTY2, CPZ, among others). The results of the DEG analysis were represented as volcano plots and heatmaps (Fig. 1).
Figure 1.
Differentially expressed genes (DEGs) present in the proliferative diabetic retinopathy (PDR) and control groups in GSE60436. (A) Volcano plot showed the distribution of the DEGs between 2 groups. The red and blue dots correspond to the upregulated and downregulated genes, respectively. (B) Bar plot showed the number of upregulated DEGs (red) and downregulated DEGs (blue). (C) Heatmap of the overall gene expression in GSE60436. Red indicates the upregulated genes and blue indicates the downregulated genes. (D) Heatmap of the top 25 upregulated DEGs (red) and the top 25 downregulated DEGs (blue) ranked by fold change.
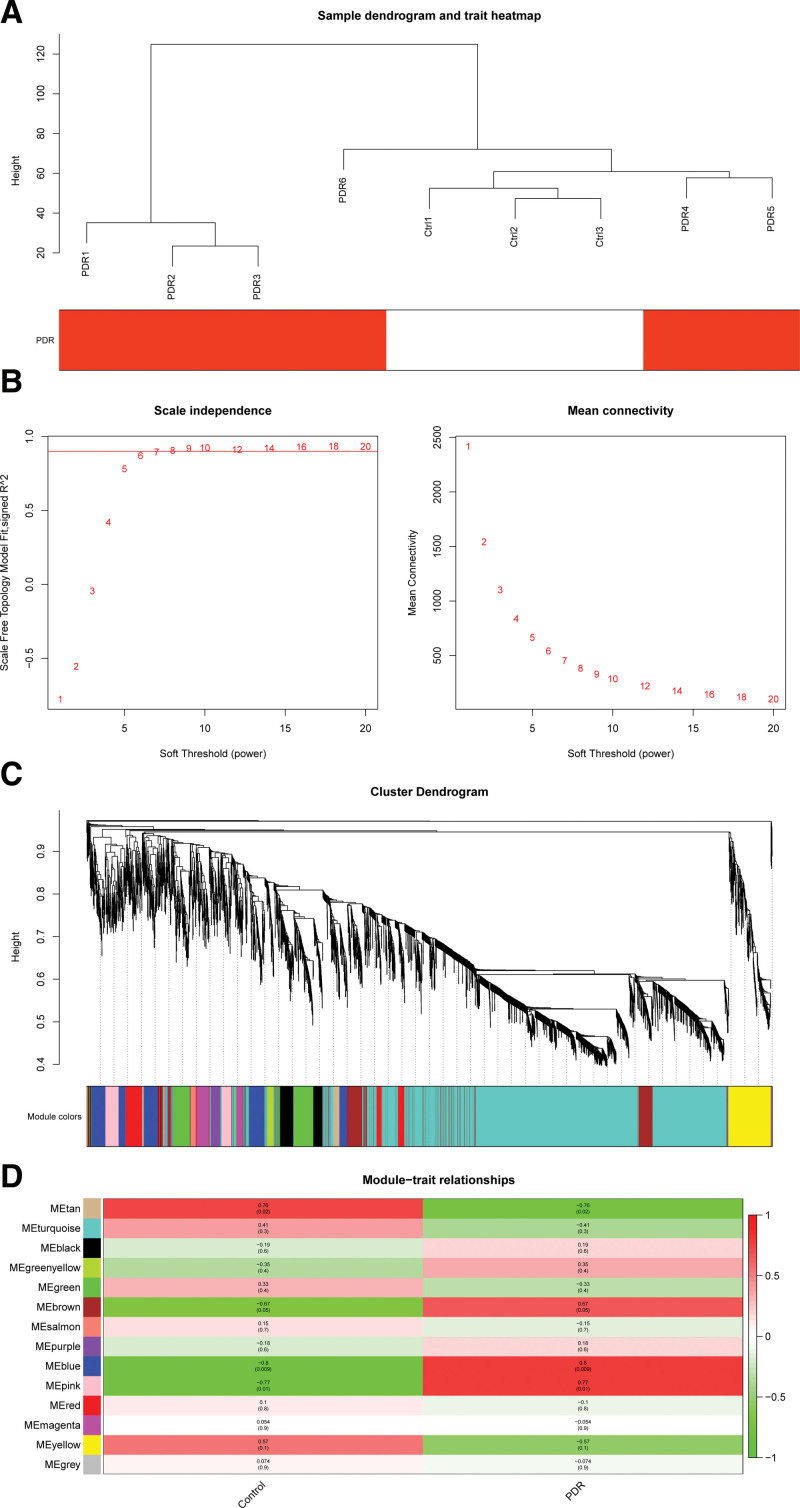
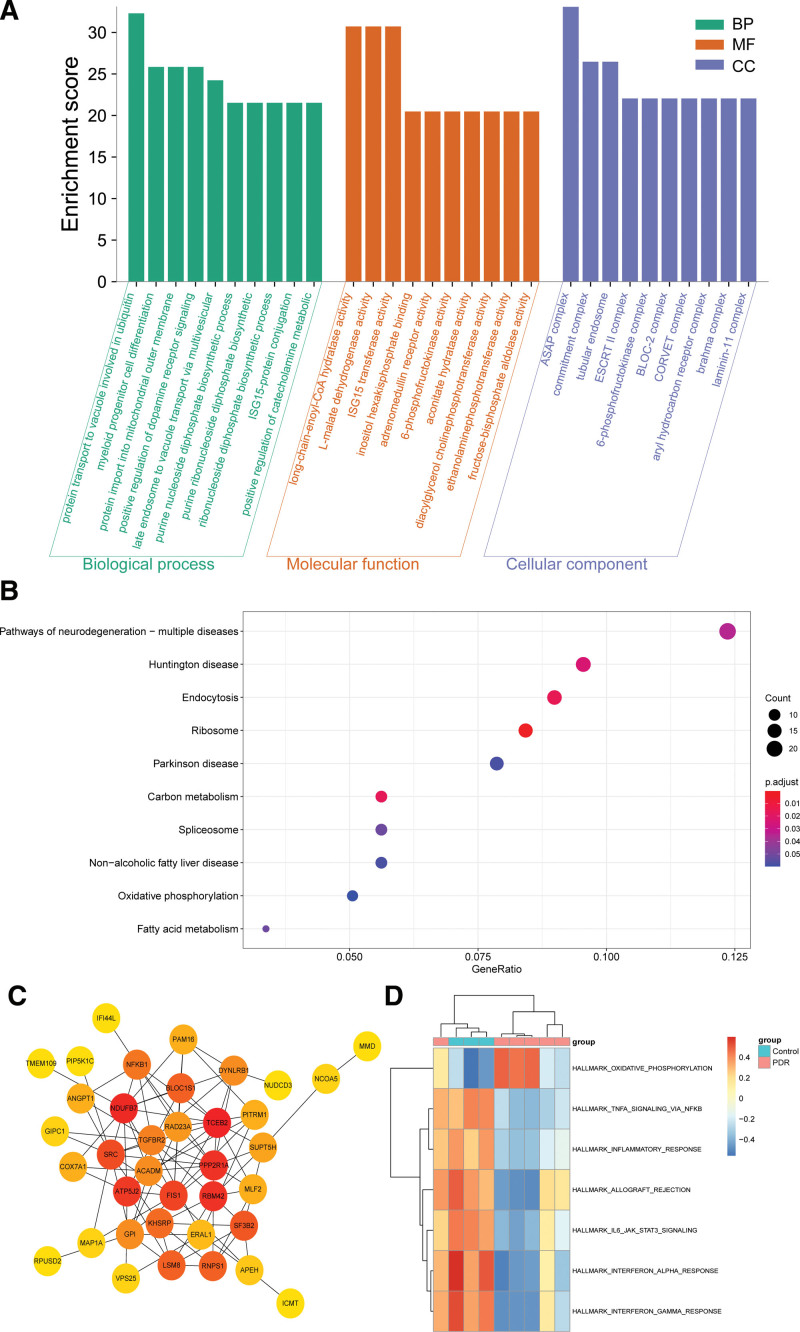
3.2. Identification of the key gene module by WGCNA
Firstly, we screened the top 5000 genes with the highest median to run WGCNA. Then, sample data was clustered, and no outliers were found in our study (Fig. 2A). The soft threshold was set to 6 according to the “pickSoftThreshold” function (Fig. 2B). Then a total of 14 gene modules were generated based on WGCNA (Fig. 2C, and see Table S1, Supplemental Digital Content, http://links.lww.com/MD/H995, which illustrates the statistic of gene modules constructed by WGCNA). The modules were named after different colors. The largest turquoise module was composed of 2568 genes and the smallest gray module was composed of 19 genes. The blue module scored the highest among the gene modules (GS = 0.64, (Figs. 2D, 3A and 3B), so it was identified as the key module. In the blue module, 46 interesting genes whose module membership (MM) > 0.9 and GS > 0.3 were picked out (Fig. 3B). The eigengene dendrogram and adjacency heatmap displayed the correlation between PDR and the modules (Fig. 3C).
Figure 2.
Gene co-expression network construction by weighted gene co-expression network analysis (WGCNA). (A) Sample data clustering showed no obvious outliers found. Red color represents the proliferative diabetic retinopathy (PDR) group. Ctrl, control group. (B) Determination of soft threshold. Left: scale independence; right: mean connectivity. (C) Cluster dendrogram. Each color represents 1 specific gene module; the above branches represent genes. (D) Module-trait relationships among the 14 gene modules. The GS value of the blue module was the highest. GS = gene significance.
Figure 3.
Screening of interesting genes in the key module. (A) Gene significance (GS) across modules. (B) Module membership (MM) vs. GS in the blue module. The red dotted lines represent the thresholds of MM > 0.9 and GS > 0.3 set for interesting genes. (C) Eigengene dendrogram and adjacency heatmap displayed the correlation between proliferative diabetic retinopathy (PDR) and the modules.
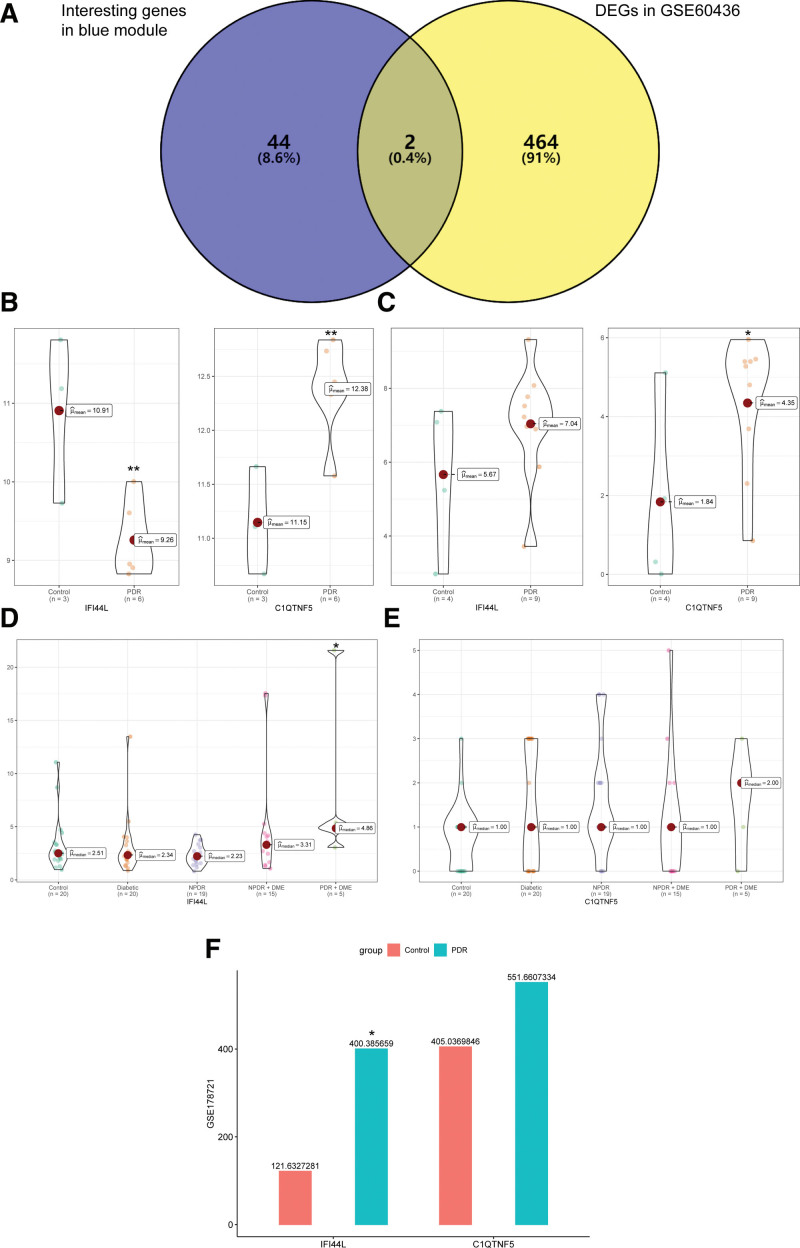
3.3. Identification and verification of hub genes
By taking the intersection of DEGs in GSE60436 and interesting genes in the blue module, interferon (IFN)-induced protein 44-like (IFI44L) and complement C1q tumor necrosis factor-related protein 5 (C1QTNF5) were identified as hub genes (Fig. 4A). We verified the expression of IFI44L and C1QTNF5 in GSE94019, GSE160306, and GSE178721 (Fig. 4B–F). IFI44L was found highly expressed in GSE94019, GSE160306, and GSE178721 but not in GSE60436. C1QTNF5 was highly expressed in all 4 datasets but was not significantly different in GSE160306 and GSE178721. What’s more, we have discovered that high IFI44L expression seemed to have strong associations with the disease status of diabetic retinopathy according to its expression in GSE160306. More importantly, similar trends in IFI44L expression were shown in the tissue samples (GSE94019 and GSE160306) and serum samples (GSE178721).
Figure 4.
Identification and expressions of hub genes in GSE60436, GSE94019, GSE160306 and GSE178721. (A) Venn diagram showed IFI44L and C1QTNF5 in the intersection of 46 interesting genes in the blue module and 466 differentially expressed genes (DEGs) in GSE60436. (B) Violin plots of the expressions of IFI44L and C1QTNF5 in GSE60436. X-axis represented the control group and the proliferative diabetic retinopathy (PDR) group. Y-axis represented the expression of genes. (C) Violin plots of the expressions of IFI44L and C1QTNF5 in GSE94019. (D) Violin plots of the expressions of IFI44L in GSE160306. X-axis represented the control group, diabetic group, non-proliferative diabetic retinopathy (NPDR) group, NPDR with diabetic macular edema (DME) group and PDR with DME group. (E) Violin plots of the expressions of C1QTNF5 in GSE160306. (F) Box plots of the expressions of IFI44L and C1QTNF5 in GSE178721. The green box represented PDR group and the red box represented the control group. **P < .01; *P < .05. C1QTNF5 = complement C1q tumor necrosis factor-related protein 5, IFI44L = interferon (IFN)-induced protein 44-like.
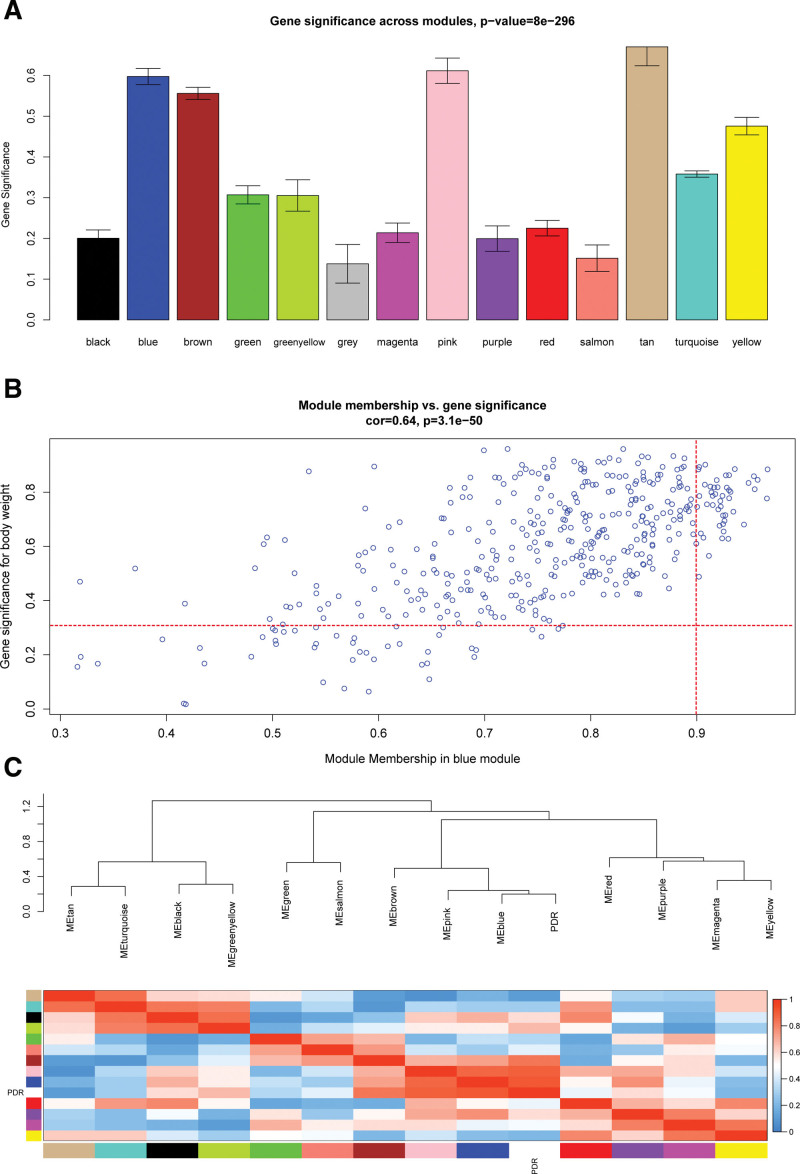
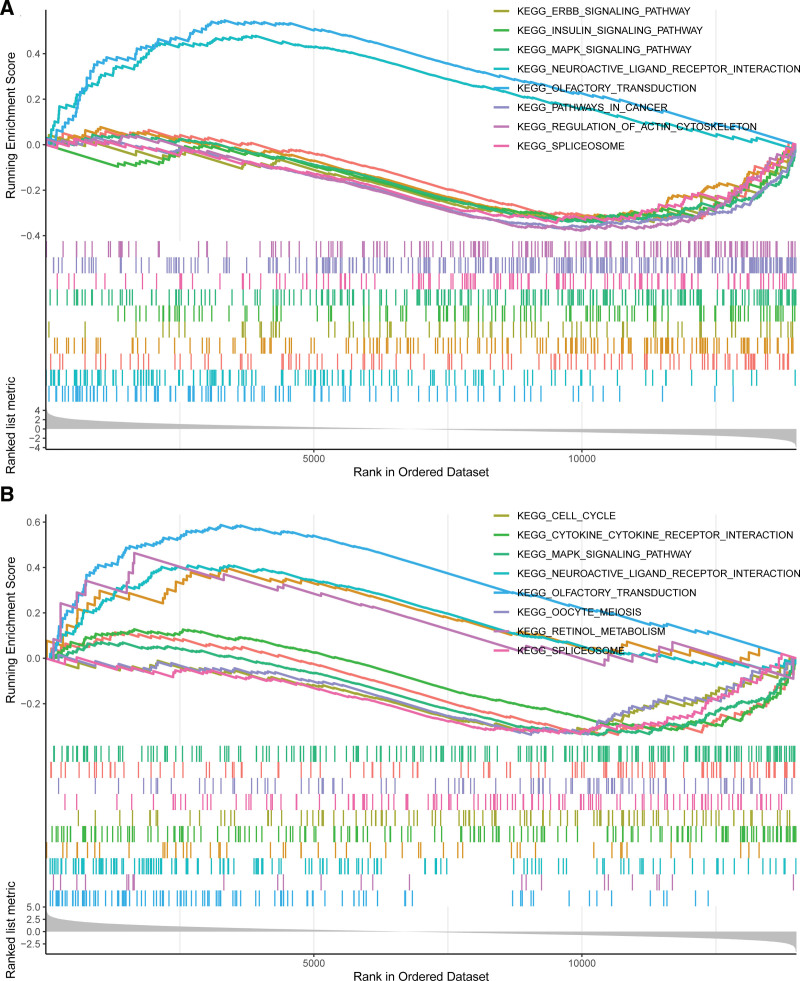
3.4. Enriched biological processes and pathways in the key module and PPI network construction
Genes in the blue module were mainly enriched in protein transport to the vacuole involved in ubiquitin-dependent protein catabolic process via the multivesicular body sorting pathway (GO:0043328) in GO biological process, long chain enoyl-CoA hydratase activity (GO:0016508) in GO molecular function, and 6-phosphofructokinase complex (GO:0005945) in GO cellular component (Fig. 5A), and see Table S2, Supplemental Digital Content, http://links.lww.com/MD/H996, which illustrates GO terms enrichment analysis of the blue module). Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis showed that pathways of neurodegeneration-multiple diseases (hsa05022) and endocytosis (hsa04144) were regulated by the blue module genes (Fig. 5B). Moreover, a PPI network was constructed for interesting genes in the blue module, which consisted of 38 gene nodes (Fig. 5C). GSVA of GSE60436 suggested the importance of the TNF-α signaling pathway and interferon α response for PDR (Fig. 5D). According to GSEA results of GSE94019, IFI44L might act on the insulin signaling pathway and mitogen‐activated protein kinase (MAPK) signaling pathway (Fig. 6A) and C1QTNF5 might affect the retinol metabolism pathway and MAPK signaling pathway (Fig. 6B).
Figure 5.
Functional enrichment analysis of genes in the blue module. (A) Gene ontology (GO) terms enrichment analysis of the blue module. Top 10 terms in GO biological process (BP), molecular function (MF) and cellular component (CC) enrichment analysis, sorted by the enrichment score. (B) Significantly enriched KEGG pathways in the blue module, gene count, and –log10 (P-value). (C) Protein-protein interaction network of interesting genes in the blue module, the dots represent proteins, the change of their colors from red to yellow reflect their Maximum Neighborhood Component (MCC) value calculated by “Cytohubba” plugin from high to low, and the lines represent protein interactions. (D) Heatmap of gene set variation analysis (GSVA) in GSE60436, red indicates the upregulated gene sets and blue indicates the downregulated gene sets. KEGG = Kyoto encyclopedia of genes and genomes.
Figure 6.
Gene set enrichment analysis (GSEA) of hub genes in GSE94019. (A) Top 8 gene sets (according to GSEA enrichment score) enriched in the IFI44L high-expressed group. (B) Top 8 gene sets enriched in the C1QTNF5 high-expressed group. C1QTNF5 = complement C1q tumor necrosis factor-related protein 5, IFI44L = interferon (IFN)-induced protein 44-like.
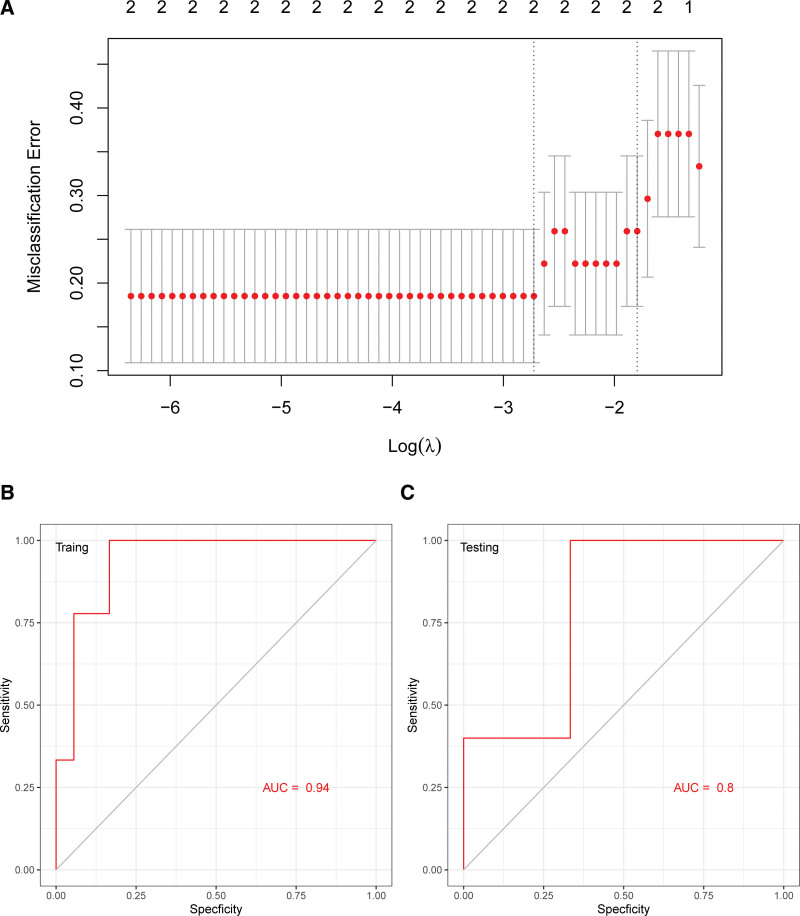
3.5. LASSO model of IFI44L and C1QTNF5
We utilized the LASSO model to identify IFI44L and C1QTNF5 with non-zero regression coefficients. The minimum value of lambda was 0.001245652. Two gene-based model indexes were created as follows: index = IFI44L * 0.0432 + C1QTNF5 * 0.11246 (Fig. 7A). ROC curve analysis indicated that the area under the curve (AUC) of the two-gene-based model was 0.94 in the training set (Fig. 7B) and 0.80 in the test set (Fig. 7C). This suggested that 2 hub genes could serve as potential diagnostic biomarkers of PDR.
Figure 7.
Least absolute shrinkage and selection operator (LASSO) model for predicting PDR and receiver operating characteristic (ROC) curve analysis. (A) LASSO model. (B) ROC curves analysis of training set (GSE94019 and GSE160306 were combined and then 70% of the combined dataset were randomly assigned to the training set). (C) ROC curves analysis of test set (the rest 30% of the combined dataset were assigned to the test set). PDR = proliferative diabetic retinopathy.
4. Discussion
Various proteins, cytokines, deoxyribonucleic acid (DNA) methylation, messenger ribonucleic acid (mRNA), and non-coding RNAs are considered as biomarkers for PDR, for instance, CCDC144NL and ZNF80,[32] MMP-14,[33] extracellular matrix metalloproteinase inducer (EMMPRIN),[34] miR-296,[35] miR-20b, miR-17-3p, HOTAIR, and MALAT1,[36] hsa_circ_0001953.[37] The relationships between IFI44L and C1QTNF5 with PDR have not been reported yet.
In our study, GSE60436 was divided into 14 modules by WGCNA, among which the enriched GO functions of the key module involved a variety of glucose and lipid metabolic pathways similar to those reported.[38,39]
We then identified IFI44L and C1QTNF5 as hub genes and verified their expression in validation data sets. Finally, a diagnostic model was established by LASSO regression, and the diagnostic significance of the 2 genes for PDR was further analyzed.
The IFI44L gene, is an important paralog of the IFI44 gene. It has been reported that IFI44L is closely associated with tuberculosis,[40] Zika virus infection,[41] hepatitis C[42] and hepatocellular carcinoma.[43] In a study of human retinal pigmented epithelial cells (RPE) in an age-related macular degeneration (AMD) disease model, IFI44L was significantly differentially expressed and may play a role in regulating inflammatory pathways.[44]
Late-onset retinal degeneration has been linked to mutations in the C1QTNF5 gene.[45,46] It belongs to the C1q/TNF-related protein (CTRP) family, a family of genes that link immunity to metabolism by exerting anti-inflammatory and insulin-sensitizing effects.[47] Surprisingly, C1q/TNF-related protein 3 (CTRP3) in the same family might serve as a novel biomarker for DR severity.[48]
The pathogenesis of PDR is related to inflammatory mechanisms and retinol and insulin metabolism.[6,49,50] GSEA suggested that IFI44L could affect the insulin signaling pathway and the MAPK signaling pathway, and that C1QTNF5 could affect the retinol metabolism pathway and the MAPK signaling pathway. The MAPK signaling pathway is among the well-known cellular inflammatory pathways.[51] Therefore, we might hypothesize that IFI44L and C1QTNF5 might affect the disease progression of PDR by regulating metabolism-related pathways and inflammatory pathways.
However, there were several shortcomings in our study. Our study was based on genomic data analysis, but the sample size of public datasets is limited. And 2 hub genes were not statistically significant in all the validation datasets. Moreover, our study was merely a theoretical analysis without experimental verification. In the follow-up study, we will expand the sample size of clinical patients to verify the difference in hub genes in peripheral blood samples and explore the possible mechanism of hub genes in PDR through experiments.
5. Conclusion
IFI44L and C1QTNF5 may play important roles in the disease process of PDR, and a LASSO regression model suggested that the 2 genes could serve as promising biomarkers of PDR.
Acknowledgements
We acknowledge the GEO database for providing their platforms and contributors for uploading their meaningful datasets.
Author contributions
Conceptualization: Tongtong Zhang.
Data curation: Mingxin Shang, Yao Zhang.
Formal analysis: Mingxin Shang.
Funding acquisition: Tongtong Zhang.
Investigation: Yao Zhang.
Methodology: Mingxin Shang.
Software: Mingxin Shang.
Supervision: Tongtong Zhang.
Writing – original draft: Mingxin Shang.
Writing – review & editing: Tongtong Zhang.
All authors reviewed the manuscript.
Supplementary Material
Abbreviations:
- C1QTNF5 =
- complement C1q tumor necrosis factor-related protein 5
- DEG =
- differentially expressed gene
- DME =
- diabetic macular edema
- GEO =
- gene expression omnibus
- GO =
- gene ontology
- GS =
- gene significance
- GSEA =
- gene set enrichment analysis
- GSVA =
- gene set variation analysis
- IFI44L =
- interferon (IFN)-induced protein 44-like
- LASSO =
- least absolute shrinkage and selection operator
- MAPK =
- mitogen-activated protein kinase
- NPDR =
- non-proliferative diabetic retinopathy
- PDR =
- proliferative diabetic retinopathy
- PPI =
- protein–protein interaction
- ROC =
- receiver operating characteristic
- VEGF =
- vascular endothelial growth factor
- WGCNA =
- weighted gene co-expression network analysis
This article does not contain any studies with human participants or animals performed by any of the authors.
The authors have no funding and conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article and its supplementary information files. The raw matrix datasets can be downloaded from the Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/geo/).
Supplemental Digital Content is available for this article.
How to cite this article: Shang M, Zhang Y, Zhang T. IFI44L and C1QTNF5 as promising biomarkers of proliferative diabetic retinopathy. Medicine 2022;101:47(e31961).n
Contributor Information
Mingxin Shang, Email: shangmingxin@hsyk.com.cn.
Yao Zhang, Email: zhangtongtong@hsyk.com.cn.
References
- [1].Joussen AM, Poulaki V, Le ML, et al. A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J. 2004;18:1450–2. [DOI] [PubMed] [Google Scholar]
- [2].Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. [DOI] [PubMed] [Google Scholar]
- [4].Gu C, Lhamo T, Zou C, et al. Comprehensive analysis of angiogenesis-related genes and pathways in early diabetic retinopathy. BMC Med Genomics. 2020;13:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wong TY, Cheung CMG, Larsen M, et al. Diabetic retinopathy. Nat Rev Dis Primers. 2016;2:16012. [DOI] [PubMed] [Google Scholar]
- [6].Rezzola S, Loda A, Corsini M, et al. Angiogenesis-inflammation cross talk in diabetic retinopathy: novel insights from the chick embryo chorioallantoic membrane/human vitreous platform. Front Immunol. 2020;11:581288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lachin JM, Genuth S, Nathan DM, et al. Effect of glycemic exposure on the risk of microvascular complications in the diabetes control and complications trial – revisited. Diabetes. 2008;57:995–1001. [DOI] [PubMed] [Google Scholar]
- [8].Abhary S, Burdon KP, Gupta A, et al. Common sequence variation in the VEGFA gene predicts risk of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2009;50:5552–8. [DOI] [PubMed] [Google Scholar]
- [9].Loukovaara S, Koivunen P, Inglés M, et al. Elevated protein carbonyl and HIF-1α levels in eyes with proliferative diabetic retinopathy. Acta Ophthalmol. 2014;92:323–7. [DOI] [PubMed] [Google Scholar]
- [10].Song Q, Zhang Y, Wu Y, et al. Association of erythropoietin gene polymorphisms with retinopathy in a Chinese cohort with type 2 diabetes mellitus. Clin Exp Ophthalmol. 2015;43:544–9. [DOI] [PubMed] [Google Scholar]
- [11].Kerkeni M, Saïdi A, Bouzidi H, et al. Elevated serum levels of AGEs, sRAGE, and pentosidine in Tunisian patients with severity of diabetic retinopathy. Microvasc Res. 2012;84:378–83. [DOI] [PubMed] [Google Scholar]
- [12].Zhang Y, Gao Z, Zhang X, et al. Effect of intravitreal conbercept injection on VEGF-A and -B levels in the aqueous and vitreous humor of patients with proliferative diabetic retinopathy. Exp Ther Med. 2021;21:332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Jampol LM, Bressler NM, Glassman AR. Revolution to a new standard treatment of diabetic macular edema. JAMA. 2014;311:2269–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ishikawa K, Yoshida S, Kobayashi Y, et al. Microarray analysis of gene expression in fibrovascular membranes excised from patients with proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci. 2015;56:932–46. [DOI] [PubMed] [Google Scholar]
- [15].Lam JD, Oh DJ, Wong LL, et al. Identification of RUNX1 as a mediator of aberrant retinal angiogenesis. Diabetes. 2017;66:1950–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Becker K, Klein H, Simon E, et al. In-depth transcriptomic analysis of human retina reveals molecular mechanisms underlying diabetic retinopathy. Sci Rep. 2021;11:10494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wang YY, Zhang H-Y, Jiang W-J, et al. Genetic polymorphisms in pri-let-7a-2 are associated with ischemic stroke risk in a Chinese Han population from Liaoning, China: a case-control study. Neural Regen Res. 2021;16:1302–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinf. 2008;9:559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Langfelder P, Zhang B, Horvath S. Defining clusters from a hierarchical cluster tree: the dynamic tree cut package for R. Bioinformatics. 2008;24:719–20. [DOI] [PubMed] [Google Scholar]
- [20].Tibshirani R. The lasso method for variable selection in the Cox model. Stat Med. 1997;16:385–95. [DOI] [PubMed] [Google Scholar]
- [21].Sauerbrei W, Royston P, Binder H. Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med. 2007;26:5512–28. [DOI] [PubMed] [Google Scholar]
- [22].Du P, Kibbe WA, Lin SM. lumi: a pipeline for processing Illumina microarray. Bioinformatics. 2008;24:1547–8. [DOI] [PubMed] [Google Scholar]
- [23].Robinson MD, McCarthy DJ, Smyth GK. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010;26:139–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ritchie ME, Phipson B, Wu D, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Yu G, Wang L-G, Han Y, et al. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS J Integr Biol. 2012;16:284–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hänzelmann S, Castelo R, Guinney J. GSVA: gene set variation analysis for microarray and RNA-seq data. BMC Bioinf. 2013;14:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Szklarczyk D, Gable AL, Lyon D, et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 2019;47:D607–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Shannon P, Markiel A, Ozier O, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Chin CH, Chen S-H, Wu H-H, et al. cytoHubba: identifying hub objects and sub-networks from complex interactome. BMC Syst Biol. 2014;8(Suppl 4):S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Engebretsen S, Bohlin J. Statistical predictions with glmnet. Clin Epigenetics. 2019;11:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Robin X, Turck N, Hainard A, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinf. 2011;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Pan J, Liu S, Farkas M, et al. Serum molecular signature for proliferative diabetic retinopathy in Saudi patients with type 2 diabetes. Mol Vis. 2016;22:636–45. [PMC free article] [PubMed] [Google Scholar]
- [33].Abu El-Asrar AM, Mohammad G, Allegaert E, et al. Matrix metalloproteinase-14 is a biomarker of angiogenic activity in proliferative diabetic retinopathy. Mol Vis. 2018;24:394–406. [PMC free article] [PubMed] [Google Scholar]
- [34].Abu El-Asrar AM, Ahmad A, Alam K, et al. Extracellular matrix metalloproteinase inducer (EMMPRIN) is a potential biomarker of angiogenesis in proliferative diabetic retinopathy. Acta Ophthalmol. 2017;95:697–704. [DOI] [PubMed] [Google Scholar]
- [35].Smit-McBride Z, Nguyen AT, Yu AK, et al. Unique molecular signatures of microRNAs in ocular fluids and plasma in diabetic retinopathy. PLoS One. 2020;15:e0235541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Shaker OG, Abdelaleem OO, Mahmoud RH, et al. Diagnostic and prognostic role of serum miR-20b, miR-17-3p, HOTAIR, and MALAT1 in diabetic retinopathy. IUBMB Life. 2019;71:310–20. [DOI] [PubMed] [Google Scholar]
- [37].Wu Z, Liu B, Ma Y, et al. Discovery and validation of hsa_circ_0001953 as a potential biomarker for proliferative diabetic retinopathy in human blood. Acta Ophthalmol. 2021;99:306–13. [DOI] [PubMed] [Google Scholar]
- [38].Tyni T, Palotie A, Viinikka L, et al. Long-chain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency with the G1528C mutation: clinical presentation of thirteen patients. J Pediatr. 1997;130:67–76. [DOI] [PubMed] [Google Scholar]
- [39].Liu Z, Xu J, Ma Q, et al. Glycolysis links reciprocal activation of myeloid cells and endothelial cells in the retinal angiogenic niche. Sci Transl Med. 2020;12:eaay1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Liu S, Ren W, Yu J, et al. Identification of hub genes associated with diabetes mellitus and tuberculosis using bioinformatic analysis. Int J Gen Med. 2021;14:4061–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Robinson CL, Chong ACN, Ashbrook AW, et al. Male germ cells support long-term propagation of Zika virus. Nat Commun. 2018;9:2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Brochado-Kith O, Martínez I, Berenguer J, et al. HCV cure with direct-acting antivirals improves liver and immunological markers in HIV/HCV-coinfected patients. Front Immunol. 2021;12:723196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Huang WC, Tung S-L, Chen Y-L, et al. IFI44L is a novel tumor suppressor in human hepatocellular carcinoma affecting cancer stemness, metastasis, and drug resistance via regulating met/Src signaling pathway. BMC Cancer. 2018;18:609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kurji KH, Cui JZ, Lin T, et al. Microarray analysis identifies changes in inflammatory gene expression in response to amyloid-beta stimulation of cultured human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 2010;51:1151–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Vincent A, Munier FL, Vandenhoven CC, et al. The characterization of retinal phenotype in a family with C1QTNF5-related late-onset retinal degeneration. Retina. 2012;32:1643–51. [DOI] [PubMed] [Google Scholar]
- [46].Chekuri A, Zientara-Rytter K, Soto-Hermida A, et al. Late-onset retinal degeneration pathology due to mutations in CTRP5 is mediated through HTRA1. Aging Cell. 2019;18:e13011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Schäffler A, Buechler C. CTRP family: linking immunity to metabolism. Trends Endocrinol Metab. 2012;23:194–204. [DOI] [PubMed] [Google Scholar]
- [48].Yan Z, Zhao J, Gan L, et al. CTRP3 is a novel biomarker for diabetic retinopathy and inhibits HGHL-induced VCAM-1 expression in an AMPK-dependent manner. PLoS One. 2017;12:e0178253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Rostamkhani H, Mellati AA, Tabaei BS, et al. Association of serum zinc and vitamin A levels with severity of retinopathy in type 2 diabetic patients: a cross-sectional study. Biol Trace Elem Res. 2019;192:123–8. [DOI] [PubMed] [Google Scholar]
- [50].Speicher MA, Danis RP, Criswell M, et al. Pharmacologic therapy for diabetic retinopathy. Expert Opin Emerg Drugs. 2003;8:239–50. [DOI] [PubMed] [Google Scholar]
- [51].Yeung YT, Aziz F, Guerrero-Castilla A, et al. Signaling pathways in inflammation and anti-inflammatory therapies. Curr Pharm Des. 2018;24:1449–84. [DOI] [PubMed] [Google Scholar]