Abstract
Since the onset of the COVID-19 pandemic, vaccinations have been identified as the most effective mitigation strategy against the deadly virus. This has led developed nations to accelerate research and shorten the licensure process for COVID-19 vaccines, but these changes have caused widespread concerns about vaccine safety. Research literature has long indicated that citizens’ perceptions of protective actions will determine their behaviors, and thus, the relationship between vaccine perception and vaccination intention needs to be assessed. To better understand vaccination willingness, especially in rural populations, this study surveyed 492 households from six townships in the Ya’an region of China’s Sichuan Province in November 2020. The survey followed the Protective Action Decision Model (PADM) framework for collecting perceptions about the influenza and COVID-19 vaccines as protective actions, information sources, emergency preparedness, emotional response, and demographic characteristics. The results showed that influenza vaccine perceptions significantly affected people’s COVID-19 vaccination perceptions and intentions. Unlike previous vaccination willingness and other COVID-19 studies, this study found that perceptions of resource-related attributes and health-related attributes both affected COVID-19 vaccination intentions, but the former were slightly stronger than the latter. Moreover, these effects were strongest among respondents who had the most positive perceptions of their influenza vaccine experience. This study’s findings will benefit local authorities in designing appropriate policies and measures (e.g., hazard education, risk communication, vaccination convenience enhancement) for increasing vaccination compliance for the current and future pandemics.
Keywords: COVID-19; Vaccination willingness; Protective action perceptions; Information sources; rural households; Sichuan townships, China
1. Introduction
The novel coronavirus (COVID-19) pandemic has caused unprecedented human and financial losses across the globe. Reflecting back on the progression of the pandemic two and a half years after its onset, it is observed that national governments across the world quickly agreed with the World Health Organization (WHO) [92] that increasing vaccination coverage against this deadly virus was the most effective mitigation strategy [60]. In the first year of the pandemic, many nations accelerated research and shortened their licensure processes for COVID-19 vaccines in order to achieve herd immunity and reduce the pandemic’s deadly impacts [42], [98]. By the end of 2021, the effort had allowed over 70 % of the population in high-income countries to receive at least one dose of a COVID-19 vaccine [68]. However, the rise in new variants, vaccine shortages in some countries, and low vaccination coverage in rural areas have made achieving herd immunity difficult to achieve (WHO 2022). Nevertheless, recent studies (e.g., [32]) have revealed a significant association between vaccination compliance and patients’ likelihood of overcoming severe symptoms, hospitalization, and death, irrespective of the types of variants. This implies that increasing vaccination uptake continues to be crucial in the battle against COVID-19 or in tackling other emerging contagious diseases of the future. Thus, the present study focuses on vaccine receivers, specifically on rural Chinese populations’ perceptions of the attributes that contribute to their willingness of to get vaccinated, long before the COVID-19 vaccination campaigns were popularized throughout the world. Such research is important for ensuring that health departments can adopt risk communication strategies to increase vaccine uptake by addressing impediments that dissuade populations from getting vaccinated.
Currently, individuals’ vaccination hesitancy (i.e., vaccination delays or vaccination denial) is the greatest obstacle to motivate COVID-19 vaccination [8], [18]. Scholars have published more than 50 articles examining people’s vaccination intentions throughout the world. However, the majority of those articles focused on the relationship between people’s perceptions of the vaccine’s health impacts (efficacy and safety) and their vaccination willingness [66], [87]. Nonetheless, these articles have overlooked other attributes that are likely to affect the Protective Action Decision-Making process [53], [55]. For example, previous literature has indicated that people’s confidence in government health agencies and the perceived uncertainty about vaccine safety are important factors associated with vaccine hesitancy [12]. Similarly, the Andrew Wakefield case reveals a growing concern regarding the social influence of fake information and false experience on vaccine hesitancy [2], [43], [45] while tackling these social influences would require a greater amount of energy than determining how it has been shaped [13], [10]. In this regard, the Chinese population have recently witnessed several vaccine-related scandals including the 2018 scandal in which the biomedical company Changchun Changsheng Biotechnology falsified data and distributed substandard Diphtheria, Pertussis, and Acellular Tetanus (DTaP) vaccines for infants [24]. Other incidents include the illegal sale of Category II vaccines for Rabies and Varicella viruses in the Shandong Province in 2016 [15] and suspicious infant deaths following the use of a Hepatitis B vaccine in 2013 [20]. These incidents are likely to have undermined stakeholders confidence in the new vaccines under development.Additionally, concerns with the COVID-19 vaccine safety rose exponentially when vaccine approvals were fast tracked and emergency use authorizations granted, unlike other time-tested vaccines [23], [48].
Despite accounting for only 36.1 % of the national population, the Chinese rural population’s access to medical resources—including medical staff, operating rooms and surgical equipment—has remained limited with less than 20.0 % of the national health budget earmarked for them [31], [96]. Moreover, rural China is also home to a growing aging population from a lower socio-economic background, increasing their pandemic vulnerability in many ways [58], including lower educational attainment, limited health care infrastructure, greater travel distance, inability to take time off from work. In turn, these factors reduce vaccination compliance in rural areas [61], [82]. Previous studies have also speculated that such vulnerabilities amplify the social influence of fake information and false experiences [41]. It underscores the WHO’s call to mitigate the challenges faced in rural areas across the globe as a key to ending the pandemic. Hence, to better understand rural households’ willingness to get a COVID-19 vaccine and to examine associated factors influencing protective action decision-making, a China-US collaborative team carried out a field study before any of the COVID-19 vaccines became available.
Empirical data based on the PADM [53], [55] were collected by conducting face-to-face interviews with 492 respondents’ from November 24–28, 2020 from six rural townships in the Ya’an region of Sichuan Province. The study addressed three broad questions: 1) What do rural residents think about the COVID-19 vaccine in comparison to the familiar influenza vaccine in terms of health-related (i.e., efficacy and safety) and resource-related (i.e., information and availability) attributes? 2) How do the comprehensive protective action assessments (i.e., influenza vaccine confidence and COVID-19 vaccine perceptions) affect residents’ COVID-19 vaccination willingness? 3) Do perceptions of the influenza vaccine interact with their perceptions of the COVID-19 vaccine to influence COVID-19 vaccination willingness? This line of questioning will help identify how rural populations can be reached with targeted interventions to increase uptake of the current COVID-19 vaccine, as well as vaccines against future pandemics.
2. Literature review
2.1. Theoretical framework
Factors that influence households’ willingness to adopt protective actions are of great interest to disaster researchers and policy makers. Lindell and Perry [55] drew relevant elements from sociological and psychological communication and behavioral models in proposing the PADM to explain people’s decision-making processes in response to environmental hazards. The PADM describes how people typically process information received from community stakeholders through multiple communication channels to decide on whether to take a protective action. Specifically, factors influencing this decision making process include environmental and social cues; social information sources/channels; prior emergency preparedness actions; perceptions of the threat, protective actions, and stakeholders; and demographic characteristics. This current study focuses on protective action perceptions, information sources, emergency preparedness, emotional response, and demographic variables.
2.1.1. Protective action perceptions
When people assess a protective action, they consider two primary groups of attributes—health-related and resource-related attributes. The health-related attributes (more generally known as hazard-related attributes) address whether the protective action will be effective in protecting themselves, their families, and property against a hazard’s impacts. The resource-related attributes are what taking the protective action will require in terms of cost, time/effort, knowledge/skill, specialized tools/equipment, and cooperation with others [54], [55]. Using the PADM framework, Wang et al. [88] investigated people’s willingness to adopt protective actions during the 2013 Chinese H7N9 outbreak and found that health-related attributes were positively related to people’s behavioral expectations for adopting protective actions, whereas resource-related attributes were negatively related to it. However, other studies have indicated that the association between protective action perceptions and behavioral intentions are inconsistent, and that resource-related attributes have small and non-significant correlations with adoption intentions of protective actions [54], [86], [91].
Recent studies on the uptake of COVID-19 vaccines have shown that the health-related attributes (efficacy and safety) are the most important factors influencing vaccination intentions [18], [66]. A vaccine’s resource-related attributes such as cost, convenience, and timeliness are significant, but have smaller effects than the health-related attributes in Bangladesh [1], [12]. However, in Bangladesh and China, the rate of vaccination intention decreased if there was a fee to get it versus if it was free [1], [95]. Nevertheless, to date, vaccination intentions and their determinants remain unexamined in the context of rural China.
Scholars have found that new vaccines usually engender more hesitancy than familiar ones [24], [25]. After the outbreak of the COVID-19 in China, the number of influenza vaccinations increased from 2020 to 2021 [34]. Nonetheless, influenza vaccine coverage was quite low in China, with only 0.4 % coverage for influenza vaccination, compared to 22.8 % coverage for pneumonia vaccination [90]. Also, influenza vaccination uptake in rural areas was lower than in urban areas [90]. These data suggest that, to some members of the rural Chinese population, the influenza vaccine was perceived as a new product, just like the COVID-19 vaccine. An online survey in China revealed that people who had higher confidence in domestic vaccine safety were more likely to accept a COVID-19 vaccine [21]. Hence, it is worth exploring whether influenza vaccination perceptions would influence COVID-19 vaccine acceptance.
2.1.2. Information sources
In the process of protective action decision making against impending threats, information seeking occurs when there is uncertainty and the available information is insufficient to justify immediate actions [6], [55]. Information seeking refers to active and purposeful searching, obtaining, clarifying and confirming information in order to achieve sufficient information for decision making [40]. The early stage of the COVID-19 outbreak was marked by a lack of knowledge about the disease transmission dynamics and divergent views on the effectiveness of non-pharmaceutical interventions (NPIs) [4], [81]. Unsurprisingly, this knowledge gap led to information seeking from multiple sources and through multiple channels to assess the certainty, severity, and immediacy of the threat [29], [62]. Consistent with research on seasonal influenza [91], people were concerned about different exposure paths such as close proximity to infected potentially persons and handling potentially contaminated objects [88]. Scholars have found that individuals exposed to health stressors, who therefore experience greater health concerns, search more frequently for information from various governmental, non-profit, and private information sources to help make decisions to protect themselves and their families [57], [81] Moreover, health information seekers access various information sources such as technology-based sources, print sources, and human sources, depending on channel access and preferences that vary among different groups and likely influence their willingness to get vaccinated [34], [80].
Related to trust in information sources, Chen et al. [21] surveyed 3,195 Chinese respondents and reported that those who paid little or no attention to information about COVID-19 vaccine development were less willing (66.3 %) to get the vaccine compared to those who did (85.5 %). Additionally, those that had heard of the Changchun Changsheng Biotechnology Company scandal in 2018 had significantly higher levels of doubt about the domestic vaccines [24]. Similarly, Lahijani et al. [47] found that persons who mistrusted the US healthcare system and the information provided in a commercial broadcast about the human papillomavirus (HPV) prevention strategies were less likely to get the HPV vaccine. Conversely, Latkin et al. [48] reported that those who trusted in information sources like the Centers for Disease Control and Prevention (CDC), Johns Hopkins University, and the State Health Department were more likely to trust the vaccine. However, trust in mainstream news channels such as CNN, and the White House did not show significant correlations with trust in vaccines. Given these mixed results, studies are needed in rural China to elucidate the linkages, if any, between trust in information sources and COVID-19 vaccine uptake are lacking and needed.
2.1.3. Emergency preparedness
Emergency preparedness supports active response when an emergency has occurred. A study of the US Department of Veterans Affairs (VA) Home Based Primary Care (HBPC) program indicated that, the early implementation of preparedness procedures by medical and nursing staff (e.g. categorizing patients into a risk category group, hurricane evacuation planning etc.) limited disruptions in patient care and prevented significant hospitalizations of medically vulnerable populations [93]. However, the immediacy of taking actions varied according to the types of emergency preparedness measures. Nakaya et al. [63] found that the rate of tsunami evacuations was significantly higher amongst people who had participated in tsunami disaster drills during normal times than those who had not. However, as was the case in American Samoa [56], other measures like attending a lecture about tsunamis did not influence evacuation behavior.
In the context of infectious disease outbreaks, emergency preparedness includes stockpiling face masks and disinfectants [50] and proper vaccinations and cross-immune protection, especially for people with increased susceptibility to an epidemic such as chemotherapy for cancer, age and underlying illnesses [72], [70]. However, even though risk management experts put much effort into encouraging emergency preparedness in the pre-crisis stage, until now, preparedness has usually been targeted for natural disasters. For example, residents in earthquake prone areas have long been advised to have a working battery-powered radio with spare batteries, at least 4 gallons of water in plastic containers, a complete first-aid kit, and a 4-day supply of dehydrated or canned food [59]. However, emergency preparedness is rarely targeted at new and unknown public health threats [88]. Thus, many countries throughout the world experienced personal protective equipment shortages in the early stage of COVID-19, especially among medical staffs [27]. With the development of COVID-19 vaccines, it is crucial to examine whether people’s uptake is also related to people’s prior adoption of these simple emergency preparedness measures.
2.1.4. Emotional response
In addition to taking protective actions, emergency response is also characterized by emotional reactions that are experienced after observing environmental or social cues, or receiving warnings [55]). Scholars have tried to interpret the different kinds of emotions such as fear, shock, and uncertainty, that emerge in response to a threat [78]) and their positive or negative impacts on adopting protective actions [44], [97]. The COVID-19 pandemic has caused a heightened state of negative emotions such as fear, depression, and anxiety experienced by students, parents, school teachers, healthcare workers, and medical professionals [30], [97]. Interestingly, W. Cao et al. [16] found that 25.0 % of Chinese college students who experienced anxiety in the early stages of the pandemic reported that living in urban areas helped reduce this anxiety.
Such negative emotional responses caused a greater willingness to get vaccinated by physicians who were in direct contact with infected patients, compared to administrative healthcare assistants who were not [84]. In an earlier US study, women were found to have higher intentions of getting the influenza vaccine, as they also had greater concerns about contracting the virus than men [35]. Such differences in emotional responses and their impacts on vaccine acceptance by varying population demographics needs to be studied in the rural contexts as well.
2.2. Research objectives and hypotheses
The preceding literature review generated three research objectives, five research hypotheses, and one research question.
Objective 1: To better understand how rural respondents assess an unknown COVID-19 vaccine compared to a known influenza vaccine, in terms of health-related and resource-related attributes.
RH1: Respondents’ vaccine ratings will be higher on health-related attributes than on resource-related attributes.
RH2: Respondents’ vaccine ratings on health-related and resource-related attributes will yield higher levels of agreement for the influenza vaccine than for the COVID-19 vaccine.
RH3: Respondents will have lower ratings of health-related attributes and higher perceptions of resource-related attributes for the COVID-19 vaccine compared to the influenza vaccine.
Objective 2: To determine the main effect(s) of respondents’ willingness to take a COVID-19 vaccine in rural contexts.
RH4: Respondents’ willingness to get a COVID-19 vaccine will be significantly correlated with health-related and resource-related attributes, but correlations with health-related attributes will be higher than with resource-related attributes.
RH5: When comprehensively considering the effects of respondents’ demographic characteristics, protective action perceptions, information sources, emergency preparedness, and emotional responses on their willingness to take a COVID-19 vaccine, vaccine attribute variables will have significant effects, but health-related attributes will have the strongest effect.
Objective 3: To explore the possibility that the effect of perceived COVID-19 vaccine attributes on COVID-19 vaccination willingness depends on respondents’ confidence in the influenza vaccine.
RQ1: Does respondents’ confidence in the influenza vaccine moderate the effects of perceived COVID-19 vaccine attributes on COVID-19 vaccination willingness?
3. Method
3.1. Study area
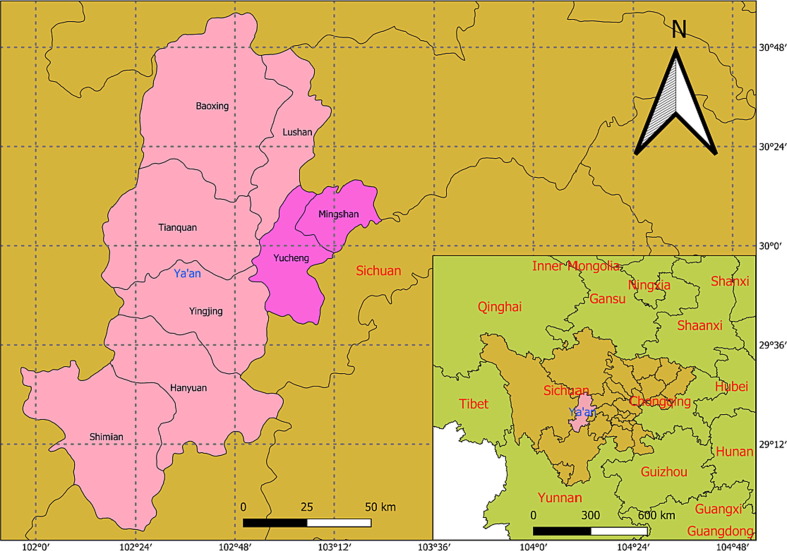
As indicated in Fig. 1 , the study area consists of the rural communities in three administrative districts (i.e., Yucheng District, Lushan County, and Baoxing County) in Ya’an region (which has two districts and six counties), Sichuan, China. As the Sichuan Province Statistical Yearbook revealed, the permanent residential population in the three selected administrative districts in 2020 was 516,700 with approximately 201,100 households yielding an average household size of 2.57 persons. Of these, 261,400 had been identified as rural [75].
Fig. 1.
Location of the Ya’an region in Sichuan Province.
As of December 1, 2021, only eight confirmed COVID-19 cases were reported in the Ya’an region. Similar to other rural regions in China, the Ya’an region had fewer COVID-19 cases compared to Wuhan, which accounted for 48.8 % of China’s total COVID-19 cases [19]. Hence, the rural population in Ya’an region was targeted as a good representative of a rural region to understand factors affecting its population’s vaccine uptake.
3.2. Survey design
This survey was part of a larger study conducted in China and the US, led by a team of university faculty and scholars in the two countries. The measures used in the survey questionnaire (e.g., protective action perception, information sources, emergency preparedness, and emotional response) were adopted from the PADM framework and adapted to suit the COVID-19 vaccine study. Only part of the 27-survey questionnaire is analyzed and presented here. These questions measured demographic characteristics, preparedness levels, information source reliance, emotional responses, NPI adoption, and protective action perceptions of the influenza and the COVID-19 vaccines. A 5-point Likert scale was utilized to capture the responses ranging from “not at all = 1″ to a “very great extent = 5” for all behavioral- and psychological-related questions. As showed in Appendix A, the questionnaire items (except variables of respondents’ and households’ contexts) had been further computed and combined into new scales as a result of factor analyses.
The survey instrument was developed in English, translated into Chinese, and then back translated to English by different researchers. The differences in translations were identified and the questionnaire was revised to ensure that the concepts were not lost in translation. Ethics approval for conducting human subjects research was obtained from both the Chinese and US universities’ ethics committees.
3.3. Sample instruments and data collection
A cluster sampling method, a commonly used strategy when there is no comprehensive list from which respondents could be randomly sampled was adopted (see [74], for a general description, [28], for theoretical details, and [56], for an example). Subsequently, six of the 23 townships from the study areas were randomly selected, which narrowed the sampling pool into an estimated 11,000–14,000 households. Given a confidence level of 95 %, an acceptable sampling error of 0.05, and an expected response rate of 15 percent, the expected sample size was 375 with 2,500 interview attempts. In addition, a quota sampling strategy was applied when picking the respondents to ensure the case pool had sufficient diversity in terms of gender and education levels.
Face-to-face interviews were conducted during November 24–27, 2020 with one member of each household. The interviewing team comprised six Chinese university staff members and four social workers from non-profit organizations (NPOs). All the interviewers attended a one-hour orientation and training session by the lead researcher on how to conduct the surveys following ethical practices, one day before the survey. Each interviewer was assigned a street block and asked to randomly select one of the first five households in that block, conduct the interview, and then repeat the same household selection and interview procedure with the next set of five households, until the block of units was completed on that street. Interviewers then switched to the next street and stopped when all the street blocks from the study areas were covered. Informed consent was obtained from the respondents before commencing questioning. Every attempt was made to ensure that the respondents alternated between a male and female in successive households and educational attainment levels varied from low to high. Participants were given the choice of filling out the questionnaire by themselves or having their responses filled in by the interviewer. On average each interviewer made 50 to 80 attempts to recruit respondents and successfully completed 12–13 interviews per day. This procedure yielded 492 respondents, generating a response rate of roughly 20.0 percent. The goal of the equal distribution of gender and education level of the respondent was partially achieved ( = 12.44, p <.01), with the data slightly overrepresenting females with lower educational levels by 29.1 percent compared to the expected 25 %.
The summary statistics of the respondents’ demographic characteristics (see Table 1 ) indicate that the respondents tended to be older, with similar levels of education, but lower income compared to the general population of Sichuan Province. Nonetheless, the sample represented the population in Sichuan’s rural areas, despite a slight over-representation of higher educated population [75]. Specifically, 56 % of the respondents were female, 80 % were married, 97 % self-identified as belonging to the Han ethnic group, and 96 % were homeowners. The respondents had an average age of 44.2 years, 11.6 years of education, an annual average household income of 67,114 Yuan (translating to 12,093 Yuan per capita), and 5.55 members per household. compared to the national average of 2.7 members per household and GDP per capita of 18, 931 Yuan in rural areas [64].
Table 1.
Matrix of Means (M), Standard Deviations (SD), and Intercorrelations (rij) among Variables.
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Age | 44.18 | 15.77 | |||||||||||||||||||||
| 2 | Female | 0.56 | 0.50 | -0.09 | ||||||||||||||||||||
| 3 | Married | 0.80 | 0.40 | 0.48 | 0.01 | |||||||||||||||||||
| 4 | Majority | 0.97 | 0.17 | 0.08 | 0.03 | 0.09 | ||||||||||||||||||
| 5 | Household Size | 5.55 | 2.31 | 0.05 | 0.01 | 0.15 | 0.01 | |||||||||||||||||
| 6 | Homeownership | 0.96 | 0.21 | 0.11 | 0.05 | 0.22 | 0.13 | 0.03 | ||||||||||||||||
| 7 | Education Years | 11.60 | 2.67 | -0.50 | -0.02 | -0.24 | -0.14 | -0.07 | -0.08 | |||||||||||||||
| 8 | Income | 67.11 k | 56.14 k | -0.24 | -0.02 | -0.12 | 0.00 | 0.04 | 0.01 | 0.39 | ||||||||||||||
| 9 | Preparedness | 3.86 | 2.15 | -0.12 | -0.06 | 0.00 | 0.00 | 0.07 | -0.06 | 0.12 | 0.10 | |||||||||||||
| 10 | Infor_Authorities | 3.83 | 0.90 | -0.08 | -0.04 | 0.03 | -0.06 | 0.07 | 0.02 | 0.09 | 0.11 | 0.28 | ||||||||||||
| 11 | Infor_Public | 3.86 | 1.00 | -0.40 | -0.01 | -0.07 | -0.09 | -0.01 | -0.02 | 0.24 | 0.15 | 0.21 | 0.55 | |||||||||||
| 12 | Infor_Private | 3.79 | 0.93 | -0.04 | 0.04 | 0.05 | -0.03 | 0.09 | 0.05 | 0.01 | 0.04 | 0.23 | 0.68 | 0.53 | ||||||||||
| 13 | Social Cues | 28.09 | 27.41 | -0.29 | -0.05 | -0.17 | -0.09 | 0.01 | -0.10 | 0.24 | 0.12 | 0.25 | 0.11 | 0.21 | 0.14 | |||||||||
| 14 | Positive Emotion | 2.98 | 1.05 | -0.17 | -0.13 | -0.14 | -0.03 | -0.04 | -0.09 | 0.24 | 0.12 | 0.34 | 0.23 | 0.23 | 0.15 | 0.18 | ||||||||
| 15 | Negative Emotion | 2.56 | 1.10 | -0.11 | 0.01 | -0.04 | 0.03 | 0.07 | -0.11 | 0.07 | 0.01 | 0.21 | 0.06 | 0.06 | 0.09 | 0.10 | 0.31 | |||||||
| 16 | Alert Emotion | 3.17 | 1.21 | -0.10 | -0.10 | -0.06 | -0.07 | 0.08 | 0.00 | 0.07 | 0.06 | 0.19 | 0.20 | 0.14 | 0.18 | 0.10 | 0.35 | 0.64 | ||||||
| 17 | NPIs | 3.95 | 0.80 | -0.29 | 0.10 | -0.08 | -0.08 | -0.04 | -0.03 | 0.32 | 0.18 | 0.33 | 0.34 | 0.38 | 0.32 | 0.25 | 0.32 | 0.12 | 0.19 | |||||
| 18 | FluShot Confidence | 3.78 | 0.71 | 0.05 | -0.01 | 0.05 | 0.07 | 0.02 | -0.05 | -0.01 | 0.08 | 0.24 | 0.31 | 0.22 | 0.32 | 0.17 | 0.24 | 0.17 | 0.18 | 0.27 | ||||
| 19 | Health | 3.76 | 0.78 | 0.02 | -0.03 | -0.02 | 0.08 | 0.00 | -0.02 | -0.01 | 0.07 | 0.23 | 0.28 | 0.18 | 0.28 | 0.17 | 0.22 | 0.15 | 0.17 | 0.19 | 0.65 | |||
| 20 | RemResource | 3.85 | 0.77 | -0.09 | 0.00 | -0.05 | 0.01 | 0.02 | -0.02 | 0.06 | 0.12 | 0.23 | 0.24 | 0.25 | 0.28 | 0.09 | 0.14 | 0.16 | 0.21 | 0.26 | 0.50 | 0.53 | ||
| 21 | Expense | 3.51 | 0.97 | -0.01 | 0.07 | 0.02 | 0.00 | 0.06 | 0.00 | 0.02 | -0.04 | 0.15 | 0.11 | 0.05 | 0.09 | 0.08 | 0.28 | 0.34 | 0.31 | 0.14 | 0.22 | 0.12 | 0.29 | |
| 22 | Willingness | 3.86 | 0.92 | -0.07 | 0.02 | 0.04 | 0.05 | 0.07 | 0.02 | 0.13 | 0.15 | 0.21 | 0.32 | 0.27 | 0.31 | 0.11 | 0.15 | 0.13 | 0.18 | 0.21 | 0.50 | 0.55 | 0.60 | 0.15 |
* r = 0.07, p <.05; r = 0.11, p <.01; r = 0.14, p <.001.
Note: Age = Age; Female = Female; Married = Married; Majority = Han Ethnicity Identification; Household Size = Household Size; Homeownership = Homeownership; Education Years = Years of Education; Income = Income in $1,000 RMB; Preparedness = Level of Preparedness; Infor_Authority = Information Reliance on Authorities; Infor_Public = Information Reliance on Public Intermediate Sources; Infor_Private = Information Reliance on Private Intermediate Sources; Social Cues = Seeing People Wearing Mask; Positive Emotion = Positive Emotion; Negative Emotion = Negative Emotion; Alert Emotion = Alert Emotion; NPIs = Previous Adoptions of Non-Pharmaceutical Interventions; Flushot Confidence = Confidence in Influenza Vaccine; Health = Health-Related Attributes; RemResource = Remaining Resource-Related Attributes; Expense = Expense-Related Attributes; Willingness = Willingness to Get Vaccinated.
3.4. Statistical analyses
3.4.1. Tests for Pseudo-attitudes
Pseudo-attitudes can occur when respondents have no pre-existing beliefs, but attempt to hide their ignorance by answering questions based upon contextual cues. Hence, the responses are termed ‘pseudo’ as they fail to tap into the respondents’ stable attitudes [22], [73]. Scholars have suggested that in cases where test–retest procedures are not available, psychological studies should test pseudo-attitudes in terms of central tendency bias for those respondents who denote biased ratings by choosing the midpoint of the rating scale [17], [40], and the diversity within subjects [5]. To test whether respondents were affected by central tendency bias, a series of t-tests were conducted, which revealed that all of the 13 vaccine-related variables have ratings significantly different from the mid-point (3) of the 1–5 rating scale, thus indicating a lack of central tendency bias. Furthermore, the results of the interrater agreement rWG tests indicated that the rWG of the 13 psychological ratings (range = 0.51-0.67) were all significantly different from zero but smaller than rWG = 0.70. The results indicate that the ratings do not have the uniform distribution that would be expected if the responses were random [49], yet there is diversity in the ratings. Hence, it is reasonable to conclude that the data are not significantly affected by pseudo-attitudes.
3.4.2. Analyses
To test the hypotheses, multiple analyses were conducted. Specifically, RH1 and RH3 were examined using descriptive statistics, multivariate analysis of variance (MANOVA), and post-hoc t-tests. RH2 was tested using the Dunlap and colleagues’[26] table of statistical significance for rWG, and Levene’s test of equal variances. RH4 and RH5 were tested using correlation analysis. Additionally, a stepwise regression analysis was conducted by selecting key predictors from each category and finally a two-way ANOVA.
The statistical tests mentioned above generated a total number of 356p-values in this study, including 61 statistics from mean or variance comparison tests, 256 statistics from correlation analyses, and 39 statistics from regression analyses. To eliminate the concern of an experiment-wise error rate[69], this study adopted the Benjamini and Hochberg (B&H) approach to determine the critical p-value and its associated false rate [9], [33]. The B&H approach starts with the specification of a false discovery rate (d) for the entire study, followed by sorting the pi significance values for the individual tests in ascending order 1 ≤ i ≤ n, and classifying each pi ≤ d × i/n as statistically significant. These results suggested a critical value of pi = 0.033 with a false discovery rate of 0.05. The study rounded up the critical value to p =.05 which yielded a false discovery rate of 0.073 with the expected number of false-positive test results FP (=α × n) = 26 (=356 × 0.073).
4. Results
4.1. Perceptions on vaccine attributes (Tests of RH1-RH3)
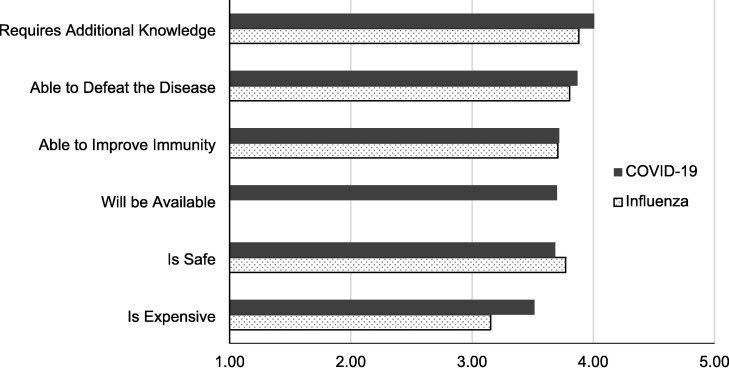
RH1 (Respondents’ vaccine ratings will be higher on health-related attributes than on resource-related attributes) is only partially supported. Results of the MANOVA reveal significant effects for attributes (Wilks Λ = 0.79, F 5,487 = 25.73, p <.001), for within-subjects (F 4,1811 = 27.96, p <.001), and for between-subjects (F 1,491 = 17,606.01, p <.001). As indicated in Fig. 2 , one of the resource-related attributes, requiring additional knowledge, surprisingly received ratings (M = 4.01) that were significantly higher than any other attributes. Of the three health-related attributes, defeating disease and improving immunity received the next highest ratings (M = 3.87 and 3.72, respectively). However, only the ratings for defeating disease were significantly different from the rest of the attributes, while the ratings for improving immunity were generally similar to the ratings of availability concerns (M = 3.70) and safety concerns (M = 3.68). Finally, the remaining resource-related attribute, expense concerns, received ratings (M = 3.51) that were significantly lower than all attributes other than safety concerns (Mdiff = 0.17, p <.05).
Fig. 2.
Perceived attributes of COVID-19 vaccine and influenza vaccine, * “Will be available” was not appliable for the influenza vaccine.
In response to RH2 (Respondents’ ratings on health-related and resource-related attributes will yield higher levels of agreement for the influenza vaccine than for the COVID-19 vaccine), interrater agreement values for the influenza vaccine attributes were generally similar to those for the COVID-19 vaccine. Specifically, the range of interrater agreement values for the health-related attributes ranged 0.59-0.66 ( = 0.62) for the COVID-19 vaccine, while rWG for the influenza vaccine ranged 0.61-0.67 ( = 0.64). Similarly, the range of rWG values for the resource-related attributes was 0.53-0.62 ( = 0.57) on the COVID-19 vaccine and 0.51-0.53 ( = 0.52) on the influenza vaccine. Of these, only the interrater agreement of safety concerns for the influenza vaccine was significantly larger than for the COVID-19 vaccine (F = 10.97, p <.001). On the other hand, the interrater agreement of requiring additional knowledge revealed a reverse tendency; respondents’ ratings on the COVID-19 vaccine were more similar than for the influenza vaccine (F = 5.77, p <.05).
Partially consistent with RH3 (Respondents will have lower perceptions of health-related attributes and higher perceptions of the resource-related attributes for the COVID-19 vaccine compared to the influenza vaccine), the results of the MANOVA revealed significant effects for vaccines (Wilks Λ = 0.97, F 1,491 = 17.62, p <.001), attributes (Wilks Λ = 0.71, F 4,488 = 50.95, p <.001), and interaction (Wilks Λ = 0.89, F 4,488 = 15.11, p <.001). However, the results of the post-hoc pairwise comparisons supported RH3 on the resource-related attributes, but not on the health-related attributes. As indicated in Fig. 2, two of the health-related attributes (defeating disease and improving immunity) had nonsignificant differences on the ratings between the COVID-19 and influenza vaccines (t491 = 1.85, 0.34, ns., respectively). As expected, respondents’ perceptions of the COVID-19 vaccine’s safety was slightly lower (M = 3.68) than their confidence on the influenza vaccine’s safety (M = 3.77; t491 = -2.40, p <.05), but the difference was only 2.3 % of the response scale. Conversely, concerns of requiring additional knowledge and expense for COVID-19 vaccine were significantly higher than concerns for influenza vaccine (t491 = 3.27, 7.64, p <.001), respectively. However, these differences were also relatively small at, 0.1 % and 6.1 % of the response scale respectively.
4.2. Main effect analyses on vaccination intention (Tests of RH4-RH5)
To reduce collinearity effects, two factor analyses were conducted on the vaccine attributes before assessing the effects of those attributes on vaccination willingness. As expected, the factor analysis of the COVID-19 vaccine attributes suggested a two-factor solution in which defeating disease, improving immunity, and safety concerns were assigned to one scale—Health (α = 0.87, = 0.70), while requiring additional knowledge and availability concerns were assigned to another scale—Rem-Resource (remaining resource-related attribute; α = 0.62, = 0.45). However, Expense (expense concerns) was left as an independent variable because it did not load strongly on either factor. The factor analysis of the influenza vaccine attributes yielded a similar result. Hence, defeating disease, improving immunity, and safety concerns of the influenza vaccine were assigned to the scale Flu shot confidence (α = 0.84, = 0.70).
Table 1 displays the means, standard deviations, and intercorrelations among the variables needed to test RH4 (Respondents' willingness to get a COVID-19 vaccine will be significantly correlated with health-related and resource-related attributes, but correlations with health-related attributes will be higher than with resource-related attributes). Consistent with the hypothesis, Health (r = 0.55) and Rem-Resource (r = 0.60) have strong correlations with willingness while, despite being much lower, expense (r = 0.15) also has a significant correlation with COVID-19 vaccination willingness. However, although the effects of Health and Rem-Resource on COVID-19 vaccination willingness were generally similar, Rem-Resource had a slightly stronger correlation than Health. Hence, RH4 was partially supported.
Although not hypothesized, Flu shot confidence (r = 0.50) also had a strong correlation with COVID-19 vaccination willingness, while NPIs (r = 0.21), information sources ( = 0.30), and emergency preparedness (r = 0.21) also had moderate correlations with COVID-19 vaccination willingness. Besides, age (r = -0.07), household size (r = 0.07), education year (r = 0.13), income (r = 0.15), social cues (r = 0.11), and emotional response ( = 0.16) also had some weak but significant correlations with COVID-19 vaccination willingness. It is also noteworthy that Health (r = 0.65) and Rem-Resource (r = 0.50) were strongly correlated to Flu shot confidence, which suggests that respondents’ perceptions of the COVID-19 vaccine might be based on their experience with the influenza vaccine.
As indicated in Table 2 , the test of RH5 (When comprehensively considering the effects of respondents’ demographic characteristics, protective action perceptions, information sources, emergency preparedness, and emotional responses on their willingness to take a COVID-19 vaccine, vaccine attribute variables will have significant effects, but health-related attributes will have the strongest effect) partially supported the PADM by examining variables in five blocks and adding each block variables stepwise. As expected, contextual, information source, emotional variables—income, emergency preparedness, Info_authorities, and Info_private—have some significant effects in the beginning steps (i.e., Models I, II, and III). However, when previous experience (e.g., NPIs, Flu shot confidence) and emotional response are entered in Model IV, only income (β = 0.09, p <.05) and Flu shot confidence (β = 0.54, p <.001) remain significant. When COVID-19 vaccination attributes are added in Model, Income turns nonsignificant (β = 0.07, ns.) while the effect of Flu shot confidence decreases (β = 0.11, p <.05). Consistent with RH5, Health and Rem-Resource have significant effects on COVID-19 vaccination willingness. However, Rem-Resource surprisingly has a stronger effect (β = 0.38, p <.001) than Health (β = 0.24, p <.001).
Table 2.
Regression of COVID-19 Vaccine Willingness on Predictor Variables.
| DV = Willingness | Model I | Model II | Model III | Model IV | Model V | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | B | SE | β | B | SE | β | B | SE | β | B | SE | β | B | SE | β |
| Respondents’ and Households’ Contexts | |||||||||||||||
| Age | 0.00 | 0.00 | -0.03 | ||||||||||||
| Female | 0.05 | 0.08 | 0.03 | ||||||||||||
| Married | 0.17 | 0.12 | 0.07 | ||||||||||||
| Majority | 0.28 | 0.24 | 0.05 | ||||||||||||
| Household Size | 0.02 | 0.02 | 0.05 | ||||||||||||
| Homeownership | 0.07 | 0.20 | 0.02 | ||||||||||||
| Education Years | 0.03 | 0.02 | 0.08 | ||||||||||||
| Income | 0.00* | 0.00 | 0.10* | 0.00* | 0.00 | 0.10* | 0.00* | 0.00 | 0.11* | 0.00* | 0.00 | 0.09* | 0.00 | 0.00 | 0.07 |
| Preparedness | 0.08*** | 0.02 | 0.19*** | 0.05* | 0.02 | 0.11* | 0.04* | 0.02 | 0.10* | 0.02 | 0.02 | 0.05 | 0.00 | 0.02 | 0.00 |
| Information Sources | |||||||||||||||
| Infor_Authorities | 0.13* | 0.06 | 0.13* | 0.15* | 0.06 | 0.14* | 0.09 | 0.05 | 0.09 | 0.09 | 0.05 | 0.09 | |||
| Infor_Public | 0.07 | 0.05 | 0.07 | ||||||||||||
| Infor_Private | 0.15** | 0.06 | 0.16** | 0.17** | 0.06 | 0.17** | 0.10 | 0.05 | 0.10 | 0.04 | 0.05 | 0.04 | |||
| Social Cues | 0.00 | 0.00 | 0.02 | ||||||||||||
| Emotional Variables | |||||||||||||||
| Positive Emotion | 0.01 | 0.04 | 0.01 | ||||||||||||
| Negative Emotion | 0.04 | 0.05 | 0.04 | ||||||||||||
| Alert Emotion | 0.05 | 0.04 | 0.07 | 0.04 | 0.03 | 0.06 | 0.02 | 0.03 | 0.02 | ||||||
| Experiences | |||||||||||||||
| NPIs | 0.00 | 0.05 | 0.00 | ||||||||||||
| FluShot Confidence | 0.54*** | 0.05 | 0.41*** | 0.15* | 0.06 | 0.11* | |||||||||
| Vaccine Attributes | |||||||||||||||
| Health | 0.28*** | 0.05 | 0.24*** | ||||||||||||
| RemResource | 0.44*** | 0.05 | 0.38*** | ||||||||||||
| Expense | -0.03 | 0.03 | -0.02 | ||||||||||||
| (Constant) | 2.57 | 0.44 | 2.22 | 0.19 | 2.11 | 0.20 | 0.82 | 0.24 | 0.02 | 0.21 | |||||
| R2 | 0.08 | 0.15 | 0.15 | 0.30 | 0.46 | ||||||||||
| Adj R2 | 0.06 | 0.14 | 0.14 | 0.29 | 0.45 | ||||||||||
| df | (9,482) | (6,485) | (7,484) | (7,484) | (11,480) | ||||||||||
| F | 4.46*** | 14.20*** | 12.71*** | 29.57*** | 37.89*** | ||||||||||
* p <.05; ** p <.01; *** p <.001.
Note: Age = Age; Female = Female; Married = Married; Majority = Han Ethnicity Identification; Household Size = Household Size; Homeownership = Homeownership; Education Years = Years of Education; Income = Income in $1,000 RMB; Preparedness = Level of Preparedness; Infor_Authority = Information Reliance on Authorities; Infor_Public = Information Reliance on Public Intermediate Sources; Infor_Private = Information Reliance on Private Intermediate Sources; Social Cues = Seeing People Wearing Mask; Positive Emotion = Positive Emotion; Negative Emotion = Negative Emotion; Alert Emotion = Alert Emotion; NPIs = Previous Adoptions of Non-Pharmaceutical Interventions; Flushot Confidence = Confidence in Influenza Vaccine; Health = Health-Related Attributes; RemResource = Remaining Resource-Related Attributes; Expense = Expense-Related Attributes; Willingness = Willingness to Get Vaccinated.
4.3. Influenza vaccine effects on COVID-19 vaccination intention
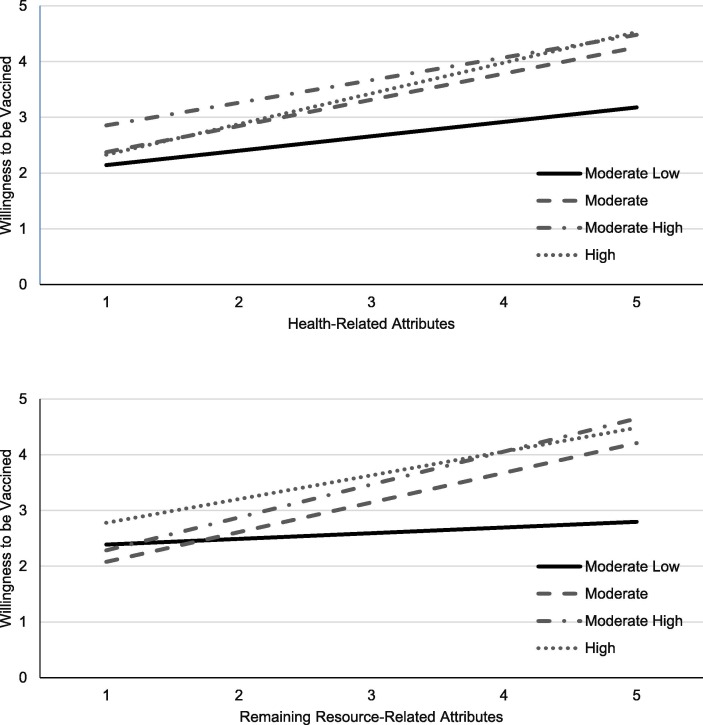
RQ1 (Does respondents’ confidence in the influenza vaccine moderate the effects of perceived COVID-19 vaccine attributes on COVID-19 vaccination willingness?) was tested by one MANOVA that assessed the interaction effects of Flu shot confidence and Health on COVID-19 vaccination willingness and another MANOVA that assessed the interaction effects of Flu shot confidence and Rem-Resource on COVID-19 vaccination willingness. As indicated in Table 3 , both tests produced significant interactions (F69 = 1.65, p <.01; F55 = 1.59, p <.01, respectively). Specifically, Fig. 3 shows that both Health and Rem-Resource have moderately strong positive effects when respondents’ Flu shot confidence is higher than the moderate level but negligible effects when Flu shot confidence is lower than that.
Table 3.
Tests of Interaction Effects.
| DV = COVID-19 Vaccination Willingness | Model I | Model II | ||||
|---|---|---|---|---|---|---|
| Predictors | df | Mean Square | F | df | Mean Square | F |
| Corrected Model | 97 | 2.35 | 5.06*** | 81 | 2.86 | 6.52*** |
| Intercept | 1 | 90.55 | 194.79*** | 1 | 97.65 | 222.78*** |
| Covariance Variables | ||||||
| Income | 1 | 3.14 | 6.76** | 1 | 1.12 | 2.55 |
| Preparedness | 1 | 0.42 | 0.90 | 1 | 0.62 | 1.42 |
| Infor_Authorities | 1 | 0.25 | 0.54 | 1 | 1.05 | 2.38 |
| Infor_Private | 1 | 0.78 | 1.69 | 1 | 0.14 | 0.32 |
| Alert Emotion | 1 | 0.86 | 1.85 | 1 | 0.04 | 0.08 |
| Fixed Factors | ||||||
| FluShot Confidence | 13 | 1.16 | 2.50** | 13 | 1.34 | 3.07*** |
| Health | 10 | 3.24 | 6.98*** | |||
| RemResource | 8 | 4.59 | 10.48*** | |||
| FluShot Confidence* Health | 69 | 0.77 | 1.65** | |||
| FluShot Confidence* RemResource | 55 | 0.70 | 1.59** | |||
| Error | 394 | 0.46 | 410 | 0.44 | ||
| Total | 492 | 492 | ||||
| Corrected Total | 491 | 491 | ||||
| R2 | 0.56 | 0.56 | ||||
| Adj R2 | 0.46 | 0.48 | ||||
Fig. 3.
Interactions of influenza vaccination confidence with COVID-19 vaccination health-related and resource-related attributes on COVID-19 vaccination willingness, Note: Income, Preparedness, Infor_Authorities, Infor_Private, and Alert emotion are controlled as covariates.
5. Discussion
This study investigated rural households’ perceptions of the already-known influenza vaccine and the unknown COVID-19 vaccine and also explored factors affecting people’s willingness to get the COVID-19 vaccine. While other scholars have studied the general Chinese population’s COVID-19 vaccine willingness, they relied on online surveys for data collection, given the movement restrictions due to pandemic containment protocols [21], [51], [90]. Similar survey methods were also used by researchers in the US [46], Australia [12], and Qatar [3] or an extensive bibliographic review in India [71], as COVID-19 containment measures prevented face-to-face interviews. Moreover, the respondents of these prior studies were younger, with higher education, and higher income than their national populations [46], [51], possibly producing variance restriction in the predictor variables that would cause downward bias in the correlation and regression coefficients [67]. This study used face-to-face interviews with a mix of young and elderly, literate and illiterate, male and female members in rural populations adding to its uniqueness.
This study’s findings suggest that rural populations require additional knowledge for both types of vaccines, with more of them requiring additional information about the COVID-19 vaccine. Data on the Expanded Program of Immunization (EPI) in China suggests that vaccine coverage for children has been consistently over 90 %, but the coverage of non-EPI vaccines such as influenza vaccines for adults is much lower [24]. For instance, the coverage of influenza vaccine achieved no more than 0.4 % in 2019 in China, which was much lower than that in the US (48.4 %) (Y. [90]. In addition, there was a higher mortality burden of influenza in the west of China than in the center of China, due to a low influenza vaccination coverage and a shortage of access to health-care services, especially in rural areas [52]. One reason for the influenza vaccine’s low coverage may be people’s underestimates of the vaccine’s health-related attributes and overestimates of its resource-related attributes. During the face-to-face survey, some of the elderly respondents expressed beliefs that if they took the influenza vaccine once, they had beaten the influenza virus forever. Additionally, people in rural China who live a poor life with hardships do not believe the common cold/influenza as something to worry about. Oftentimes the illiterate tend to consider the influenza virus the same as a common cold and simply follow traditional Chinese medicinal practices, drinking more boiled hot water with ginger and brown sugar as remedies. During the time this study was conducted in November 2020, information on vaccine research and development, clinical trials, and manufacturing were being released extensively through multiple media channels like the TV, and social media including TikTok videos [21], [89]. However, most of the information sources were difficult for rural populations to access and the content was difficult to understand.
The fact that amongst the health-related attributes, the safety of influenza vaccine received higher ratings than the COVID-19 vaccine was not surprising. People are usually much more cautious about any new pharmaceutical in the market, especially rural populations who are unfamiliar with new innovations. For instance, during the early stages of the COVID-19 pandemic, due to the fear of the virus, people in rural regions destroyed main roads leading to their communities in order to prevent outsiders from entering their village [85].
The lack of knowledge surrounding the COVID-19 vaccine arose mainly from doctors’, pharmaceutical research and development agencies’, and manufacturers’ very abstract discourse during the pandemic’s initial days about the coronavirus and mitigation measures. These perspectives could be quite different from those of the majority of the population in the Ya’an region, who have little or no education. Due to the limited understanding of COVID-19 vaccines, rural people believed that only the inactivated COVID-19 vaccine is the best for preventing the virus [51]. Moreover concerns about the expense related to this new vaccine was high amongst rural households, whose annual income is very low compared to their urban counterparts. During the survey, rural respondents expressed concerns of affordability because they had heard that the cost of one dose of the COVID-19 vaccine would be higher than that of the influenza vaccine (100–150 RMB), due to limited manufacturing and distribution networks to rural areas.
The strong influence of flu shot confidence on COVID-19 vaccination intentions might be due to the perception of similar infection mechanisms on respiratory system between influenza and COVID-19 [34]; WHO, 2021). Previous studies have indicated that people would be more likely to use an availability heuristic—responding to an emerging threat by using a familiar protective action to a similar previous threat [36], [79]. Hence, given that the influenza vaccine is known to protect individuals from the threats of fever, cough, and throat pain [98], it is not surprising that respondents imagined and linked COVID-19 vaccine with influenza vaccine as they share some similar respiratory symptoms (WHO, 2021). Another reason might be an overconfidence in the influenza vaccine [34], as its production has not been fraught with scandal. Hence, despite the combined effects of low education, low income, and poor accessibility to health care, there could be a strong effect of flu shot experience/perceptions on COVID-19 vaccination intentions. However, further research is needed to assess the reasons for this finding.
Interestingly, perceptions of COVID-19 vaccine health-related and resource-related attributes have the strongest influence on COVID-19 vaccination willingness. These results indicate that it is essential for people to believe that the COVID-19 vaccine will be effective and safe, as well as that information about it and access to it will be readily available. During times of uncertainty, due to lack of understandable information from credible sources, individuals often engage in health information seeking before deciding whether to comply with protective action recommendations [81], [94]. Also, at the time of the survey, there were divergent views and reports about COVID-19 vaccines, such as that COVID-19 vaccine production would be very limited and, therefore, rural people would have to wait for a long time for vaccinations [27], [89]. Additionally, the National Health Commission of China [65] announced that the distribution of COVID-19 vaccine would be given first to people working for medical services, import–export industries, and domestic and international shipping industries. This message could have increased rural residents’ doubts about their timely access to COVID-19 vaccination.
6. Conclusions
6.1. Theoretical implications
Compared to previous COVID-19 studies on vaccine uptake, the current study makes a meaningful contribution by contributing data collected through face-to-face interviews with rural populations before the vaccinations were started. This provides a broader knowledge on how elderly, lower educated, and lower income population segments think about COVID-19 vaccinations. Findings on the significant associated factors with vaccination intentions such as vaccine knowledge and information source, will allow public health authorities to provide effective risk communication that encourages protective health behavior changes in future outbreaks. Specifically, by knowing the effective risk communication channels, societies could avoid the so called “Andrew Wakefield case” that misled people, especially those with lower education and income, to reject vaccines (Motta & Stecula, 2021). Furthermore, because our case study could roughly represent the rural regions in China from the perspective of COVID-19 control and infection, our findings on COVID-19 vaccination intention have strong empirical contributions to identify the general considerations about the COVID-19 vaccine in these places. This is important because at the time of our survey, nearly no information existed and little attention had been paid to rural regions in regard to COVID-19 vaccine in such a country with a large rural population.
The current study applied the PADM framework and related measures to investigate the factors influencing rural Chinese residents’ COVID-19 vaccination intentions. By examining people’s perceptions of the health-related and resource-related attributes of influenza and COVID-19 vaccines, this study utilized some new survey scales to measure these two types of attributes in a pandemic context. Although many previous studies have analyzed the effectiveness of protective action attributes of natural disasters and technological disasters [38], the current study extends previous PADM research on respiratory infectious diseases by Wang et al. [89], [90] and Wei et al. [91] to the COVID-19 pandemic context. Furthermore, based on the data analysis results, the current study statistically categorized the specific items for the health-related and resource-related attributes of COVID-19 vaccines. This method went beyond the simple categorical method of assigning certain items for attributes. For instance, these data show that the expense of COVID-19 vaccine, which the PADM categorizes theoretically as a resource-related attribute, is different from the other resource-related attributes and—contrary to economic theory—to have a low correlation with vaccination intention.
6.2. Practical implications
The current study has two major practical implications: one at the individual level and the other at the policy level. Getting vaccinated is considered to be the strongest mitigation tool to combat the COVID-19 pandemic. However, many previous studies have reported that overconfidence, inconvenience, and complacency cause vaccine hesitancy [8], [24]. As the vaccine expense was unclear at the time of the survey, one might presume that low-income populations would be hesitant about getting vaccinated but these data show that expense was not a major obstacle to vaccination intention. Instead, the influenza vaccine attributes show strong effect on COVID-19 vaccination intention, which suggests that these respondents tend to extrapolate from their former vaccination experience to the current pandemic. Specifically, those who had positive perceptions of the influenza vaccine also had more positive perceptions of a COVID-19 vaccine. This indicates that, to increase vaccination uptake, local health agencies should consider the geographical and social events that had influenced the local population.
Further, to improve food, nutrition, and livelihood security, these rural communities may be encouraged to grow fruits and vegetables in kitchen gardens as a cheap source of healthy nutritious foods [83] which in turn can make them resilient to future threats.
At the policy level, convenient access to recommended protective actions could affect people’s behavioral intentions. For the COVID-19 vaccine, access to vaccination clinics and the timely availability of the vaccine would ordinarily expected to be rural residents’ two biggest concerns. Nevertheless, the Ya’an data reveal that the COVID-19 vaccine’s resource-related attributes had just as strong an impact on vaccination intention as its health-related attributes. These results indicate that administrative agencies should emphasize new vaccines’ resource-related and health-related attributes through a diverse set of information channels. In addition, administrative agencies in rural regions should consider people’s literacy levels, especially those who cannot obtain information from sources other than TV and peers. Although people’s beliefs about COVID-19 and vaccinations have changed in the Ya’an region since this survey, this does not limit the significant contribution of our results. Because our findings focus on the internal mechanisms of risk communication and coping behaviors during the COVID-19 pandemic, they will be useful for local authorities in managing responses to a future public health emergencies.
One apparent limitation of the current study is the potential for bias due to the unavailability of a random sampling strategy. However, it is important to understand that the effect of geographic/demographic bias depends upon what statistic is being assessed (means and proportions vs correlation and regression coefficients) and the relationships between demographic characteristics and dependent variables of interest (psychological variables and behaviors). First, estimates of means and proportions are biased by geographic/demographic non-representativeness only to the degree that the relevant dependent variables are correlated with those geographic/demographic variables. However, the literatures on hurricane evacuation [7], [37] and household emergency preparedness [55], [56] indicate that the correlations of demographic variables with behavioral variables are small and inconsistent. Consequently, geographic/demographic non-representativeness appears to have little effect on estimates of mean level of behavioral variables (or the proportion of people engaging in a behavior). Even more important is that geographic/demographic non-representativeness will have little effect on correlation and regression coefficients unless it is so severe that there are “ceiling” or “floor” effects that cause these coefficients to be systematically underestimated (Lindell & Perry, 2000; [67]. Since Table 1 shows that the cluster sampling strategy provided a reasonable level of diversity in the sample’s demographic characteristics, it is unlikely that the correlation and regression coefficients were underestimated to any significant degree. Nonetheless, the study was conducted in only one region, so further studies should be conducted in rural communities in other provinces, regions, or even countries.
A more significant limitation is that, the data were only collected once, and due to the vaccination policy changes, could not be repeated. Thus, the cross-sectional data cannot conclusively determine if the factors influencing vaccination intentions determined actual vaccinations when these became available. Following the recommendations of Bubeck et al. [14], Hudson et al. [39] and Siegrist [76], [77], longitudinal cohort studies should be conducted in these communities to determine if their perceptions and decisions about the vaccines have changed and, if so, why. Such studies could identify needed revisions to the survey items for explicating the factors affecting rural people’s vaccination intentions and actual vaccination adoption. Alternative, novel methods such as remote participatory research along with systems thinking design may be envisaged for the future [11].
Ethics approval
Ethics approval for conducting Human Subjects research was obtained from both the US University’s Institutional Review Board (Jacksonville State University), and the Chinese university’s ethics committee (Sichuan University).
Submission declaration
The current manuscript has not been published previous, that it is not under consideration for publication elsewhere, that its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work has carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
Funding.
National Natural Science Foundation of China (No. 72204253) and Sichuan Federation of Social Science Associations, China (No. SC20C012).
CRediT authorship contribution statement
Yingying Sun: Conceptualization, Project administration, Investigation, Funding acquisition. Shih-Kai Huang: Conceptualization, Methodology, Writing original draft. Sudha Arlikatti: Conceptualization, Methodology, Writing original draft, Review and editing, Visualization. Michael K. Lindell: Conceptualization, Methodology, Validation, Editing.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Yingying Sun reports financial support was provided by Sichuan Federation of Social Science Associations, China].
Appendix A. Measurements and calculations of survey items
| Item | Mean | SD |
|---|---|---|
| COVID-19 vaccination | ||
| Willingness | ||
| I will take a COVID-19 vaccination. | 3.86 | 0.92 |
| Health | α = 0.87, = 0.70 | |
| A COVID-19 vaccination protects against infection. | 3.87 | 0.83 |
| A COVID-19 vaccination improves body immunity. | 3.72 | 0.90 |
| A COVID-19 vaccination is safe. | 3.68 | 0.90 |
| RemResource | α = 0.62, = 0.45 | |
| I need more information about a COVID-19 vaccination. | 4.01 | 0.94 |
| I can get a COVID-19 vaccination within a year. | 3.70 | 0.87 |
| Expense | ||
| A COVID-19 vaccination may be expensive. | 3.51 | 0.97 |
| Influenza vaccination | ||
| FluShot Confidence | α = 0.84, = 0.57 | |
| Vaccination protects against infection. | 3.80 | 0.85 |
| Vaccination improves body immunity. | 3.71 | 0.88 |
| Vaccination is safe. | 3.77 | 0.81 |
| I will take an influenza vaccination | 3.83 | 0.90 |
|
Information seeking: To what extent have you accessed to information sources about the COVID-19 and protective actions? |
||
| Infor_Authorities | α = 0.93, = 0.63 | |
| Public health officials | 3.74 | 1.16 |
| Local government (i.e., town, county, district) | 3.82 | 1.01 |
| State government (i.e., city and province) | 3.69 | 1.05 |
| National government | 4.07 | 1.04 |
| Infor_Public | α = 0.96, = 0.54 | |
| Traditional media (i.e., TV, radio, newspapers) | 4.14 | 0.95 |
| Web-based media (i.e., mobile news, toutiao) | 3.78 | 1.30 |
| Social media (i.e., Weibo, Wechat, TikTok) | 3.67 | 1.32 |
| Infor_Private | α = 0.83, = 0.55 | |
| Community broadcasting (i.e., village, neighborhood, apartment) | 3.83 | 1.05 |
| Personal chat (i.e., relative, friend, colleague) | 3.75 | 1.06 |
| In the past week, what percentage of people you saw were wearing masks on the street? | ||
| Social Cues | 28.09 | 27.41 |
|
Emotional response How much does the possibility of being infected with COVID-19 make you feel… |
||
| Positive Emotion | α = 0.73, = 0.58 | |
| Optimistic | 2.87 | 1.24 |
| Energetic | 3.09 | 1.12 |
| Negative Emotion | α = 0.94, = 0.73 | |
| Depressed | 2.45 | 1.22 |
| Angry | 2.35 | 1.27 |
| Nervous | 2.86 | 1.23 |
| Annoyed | 2.59 | 1.22 |
| Fearful | 2.66 | 1.28 |
| Irritated | 2.48 | 1.25 |
| Alert Emotion | ||
| Alert | 3.17 | 1.21 |
|
NPIs performance To what extent have you taken each of the following actions to protect yourself and your loved ones from COVID-19? |
||
| NPIs | α = 0.86, = 0.46 | |
| Reducing outings | 4.29 | 1.01 |
| Social distancing | 4.19 | 0.98 |
| Sanitizing surfaces | 4.07 | 1.02 |
| Hand hygiene | 4.33 | 0.81 |
| Disinfecting hands | 4.03 | 1.08 |
| Taking body temperature | 3.48 | 1.38 |
| Reducng use of public transportation | 4.15 | 1.06 |
| Wearing goggles or disposable gloves | 3.06 | 1.52 |
|
Disaster preparedness Did your household have any of the following items before the pandemic? |
||
| Preparedness | α = 0.78, = 0.33 | |
| A working portable radio with spare batteries | 0.21 | 0.41 |
| At least 4 gallons of water per person in plastic containers | 0.48 | 0.50 |
| A two-week supply of non-perishable food for yourself and your family | 0.51 | 0.50 |
| At least a one-week supply of prescription medicines | 0.53 | 0.50 |
| A flashlight with extra batteries | 0.74 | 0.44 |
| Mobile phone charger | 0.69 | 0.46 |
| Face masks | 0.70 | 0.46 |
Data availability
Data will be made available on request.
References
- 1.Abedin M., Islam M.A., Rahman F.N., Reza H.M., Hossain M.Z., Hossain M.A., et al. Willingness to vaccinate against COVID-19 among Bangladeshi adults: Understanding the strategies to optimize vaccination coverage. PLoS One. 2021;16(4):e0250495. doi: 10.1371/journal.pone.0250495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adhikari B., Cheah P.Y. Vaccine Hesitancy in the COVID-19 Era. Lancet Infect Dis. 2021;21(8):1086. doi: 10.1016/S1473-3099(21)00390-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alabdulla M., Reagu S.M., Al‐Khal A., Elzain M., Jones R.M. COVID-19 vaccine hesitancy and attitudes in Qatar: A national cross-sectional survey of a migrant-majority population. Influenza Other Respi Viruses. 2021;15(3):361–370. doi: 10.1111/irv.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andrew S.A., Arlikatti S., Chatterjee V., Ismayilov O. Ebola crisis response in the USA: Communication management and SOPs. Int J Disaster Risk Reduct. 2018;31:243–250. doi: 10.1016/j.ijdrr.2018.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arlikatti S., Lindell M.K., Prater C.S., Zhang Y. Risk Area Accuracy and Hurricane Evacuation Expectations of Coastal Residents. Environ Behav. 2006;38(2):226–247. [Google Scholar]
- 6.Arlikatti S., Taibah H.A., Maghelal P., Andrew S.A., Alkhurayyif S.A. Hajj pilgrims’ perceptions of trust and Internet use for (emergency) information. International Journal of Religious Tourism and Pilgrimage. 2022;10(1) [Google Scholar]
- 7.Baker E.J. Hurricane evacuation behavior. Int J Mass Emerg Disasters. 1991;9(2):287–310. [Google Scholar]
- 8.Bedford H., Attwell K., Danchin M., Marshall H., Corben P., Leask J. Vaccine hesitancy, refusal and access barriers: The need for clarity in terminology. Vaccine. 2018;36(44):6556–6558. doi: 10.1016/j.vaccine.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Benjamini Y., Hochberg Y. Controlling the false discovery rate-A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B-Statistical Methodology. 1995;57(1):289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 10.Bergstrom C.T., West J.D. Randon House; New York, NY: 2021. Calling Bullshit: The Art of Skepticism in a Data-Driven World. [Google Scholar]
- 11.Bonin S., Singh W., Suresh V., Rashed T., Uppal K., Nair R., et al. A priority action roadmap for women’s economic empowerment (PARWEE) amid COVID-19: a co-creation approach. International Journal of Gender and Entrepreneurship. 2021;13(2):142–161. doi: 10.1108/IJGE-09-2020-0148. [DOI] [Google Scholar]
- 12.Borriello A., Master D., Pellegrini A., Rose J.M. Preferences for a COVID-19 vaccine in Australia. Vaccine. 2021;39(3):473–479. doi: 10.1016/j.vaccine.2020.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brandolini A. (2014). The bullshit asymmetry principle. Lecture delivered at XP2014 in Roma and at ALE2014 in Krakow 2014.
- 14.Bubeck P., Botzen W.J.W., Aerts J.C.J.H. A review of risk perceptions and other factors that influence flood mitigation behavior. Risk Anal. 2012;32(9):1481–1495. doi: 10.1111/j.1539-6924.2011.01783.x. [DOI] [PubMed] [Google Scholar]
- 15.Cao L., Zheng J.S., Cao L.S., Cui J., Xiao Q.Y. Evaluation of the impact of Shandong illegal vaccine sales incident on immunizations in China. Hum Vaccin Immunother. 2018;14(7):1672–1678. doi: 10.1080/21645515.2018.1473697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cao W.J., Fang Z.W., Hou G.Q., Han M., Xu X.R., Dong J.X., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:5. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cascio W.F., Aguinis H. (6th ed.). Pearson College Div; 2004. Applied psychology in human resource management. [Google Scholar]
- 18.Caserotti M., Girardi P., Rubaltelli E., Tasso A., Lotto L., Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021;272 doi: 10.1016/j.socscimed.2021.113688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CDC of China. (2021). The latest situation of the COVID-19 pandemic. (Accessed January 1, 2022) https://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11809/.
- 20.Chen B., Zhang J.M., Jiang Z.G., Shao J., Jiang T., Wang Z.T., et al. Media and public reactions toward vaccination during the “hepatitis B vaccine crisis” in China. Vaccine. 2015;33(15):1780–1785. doi: 10.1016/j.vaccine.2015.02.046. [DOI] [PubMed] [Google Scholar]
- 21.Chen M., Li Y., Chen J., Wen Z., Feng F., Zou H., et al. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum Vaccin Immunother. 2021;17(7):2279–2288. doi: 10.1080/21645515.2020.1853449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Converse P.J. In: The quantitative analysis of social problems. Tufte E.R., editor. Addison-Wesley; 1970. Attitudes and non-attitudes: Continuation of a dialogue; pp. 168–189. [Google Scholar]
- 23.Dagan N., Barda N., Kepten E., Miron O., Perchik S., Katz M.A., et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384(15):1412–1423. doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Du F.X., Chantler T., Francis M.R., Sun F.Y., Zhang X., Han K.Y., et al. The determinants of vaccine hesitancy in China: A cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. 2020;38(47):7464–7471. doi: 10.1016/j.vaccine.2020.09.075. [DOI] [PubMed] [Google Scholar]
- 25.Dube E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J. Vaccine hesitancy An overview. Hum Vaccin Immunother. 2013;9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunlap W., Burke M., Smith-Crowe K. Accurate tests of statistical significance for r(WG) and average deviation interrater agreement indexes. J Appl Psychol. 2003;88(2):356–362. doi: 10.1037/0021-9010.88.2.356. [DOI] [PubMed] [Google Scholar]
- 27.Feng J., Li J., Hu W., Li G. Public interest, risk, trust, and personal protective equipment purchase and usage: Face masks amid the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(9) doi: 10.3390/ijerph19095502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frankel M. In: Handbook of Survey Research. Rossi P.H., Wright J.D., Anderson A.B., editors. Academic Press; San Diego: 1983. Sampling theory; pp. 21–67. [Google Scholar]
- 29.Fridman I., Lucas N., Henke D., Zigler C.K. Association between public knowledge about COVID-19, trust in information sources, and adherence to social distancing: Cross-sectional survey. JMIR Public Health Surveill. 2020;6(3):e22060. doi: 10.2196/22060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fu W.N., Yan S.J., Zong Q., Anderson-Luxford D., Song X.Y., Lv Z.Y., et al. Mental health of college students during the COVID-19 epidemic in China. J Affect Disord. 2021;280:7–10. doi: 10.1016/j.jad.2020.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fullman N., Yearwood J., Abay S.M., Abbafati C., Abd-Allah F., Abdela J., et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: A systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391(10136):2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gilboa M., Regev-Yochay G., Mandelboim M., Indenbaum V., Asraf K., Fluss R., et al. Durability of immune response after COVID-19 booster vaccination and association With COVID-19 Omicron infection. JAMA Netw Open. 2022;5(9):e2231778. doi: 10.1001/jamanetworkopen.2022.31778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Glickman C.D., Gordon S.P., Ross-Gordon J. (10th ed.). Pearson; 2017. Supervision and instructional leadership: A developmental approach. [Google Scholar]
- 34.Gong L., Zhang X., Qu Z., Francis M., Han K., Xu C., et al. Public interest in distribution and determinants of influenza and pneumonia vaccination during the COVID-19 pandemic: An infodemiology and cross-sectional study from China. Vaccines. 2021;9(11) doi: 10.3390/vaccines9111329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hogan C., Atta M., Anderson P., Stead T., Solomon M., Banerjee P., et al. Knowledge and attitudes of us adults regarding COVID-19. International. J Emerg Med. 2020;13(1) doi: 10.1186/s12245-020-00309-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hua C., Huang S.-K., Lindell M.K., Yu C.-H. Rural Households’ Perceptions and Behavior Expectations in Response to Seismic Hazard in Sichuan. China Safety Science. 2020;125 [Google Scholar]
- 37.Huang S.K., Lindell M.K., Prater C.S. Who leaves and who stays? A review and statistical meta-analysis of hurricane evacuation studies. Environ Behav. 2016;48(8):991–1029. [Google Scholar]
- 38.Huang S.-K., Lindell M.K., Prater C.S. Multistage model of hurricane evacuation decision: Empirical study of Hurricanes Katrina and Rita. nat Hazard Rev. 2017;18(3):15. doi: 10.1061/(asce)nh.1527-6996.0000237. [DOI] [Google Scholar]
- 39.Hudson P., Thieken A.H., Bubeck P. The challenges of longitudinal surveys in the flood risk domain. J Risk Res. 2019;23(4):1–22. [Google Scholar]
- 40.Hyman A., Arlikatti S., Huang S.-K., Lindell M.K., Mumpower J., Prater C.S., et al. How do perceptions of risk communicator attributes affect emergency response? An examination of a water contamination emergency in Boston, USA. Water Resour Res. 2022;58(1) doi: 10.1029/2021WR030669. [DOI] [Google Scholar]
- 41.Kasperson R.E., Renn O., Slovic P., Brown H.S., Emel J., Goble R., et al. The Social Amplification of Risk: A Conceptual Framework. Risk Anal. 1988;8:177–187. [Google Scholar]
- 42.Keech C., Albert G., Cho I., Robertson A., Reed P., Neal S., et al. Phase 1–2 trial of a SARS-CoV-2 recombinant spike protein nanoparticle vaccine. N Engl J Med. 2020;383(24):2320–2332. doi: 10.1056/NEJMoa2026920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kennedy J. Vaccine Hesitancy: A Growing Concern. Pediatr Drugs. 2020;22:105–111. doi: 10.1007/s40272-020-00385-4. [DOI] [PubMed] [Google Scholar]
- 44.Kimhi S., Marciano H., Eshel Y., Adini B. Resilience and demographic characteristics predicting distress during the COVID-19 crisis. Soc Sci Med. 2020;265:113389. doi: 10.1016/j.socscimed.2020.113389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koslap-Petraco M. Vaccine Hesitancy: Not a New phenomenon, but a New Threat. J Am Assoc Nurse Pract. 2019;31(11):624–626. doi: 10.1097/JXX.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 46.Kreps S., Prasad S., Brownstein J.S., Hswen Y., Garibaldi B.T., Zhang B., et al. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020;3(10):e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lahijani A.Y., King A.R., Gullatte M.M., Hennink M., Bednarczyk R.A. HPV vaccine promotion: The church as an agent of change. Soc Sci Med. 2021;268:8. doi: 10.1016/j.socscimed.2020.113375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodram B. Trust in a COVID-19 vaccine in the US: A social-ecological perspective. Soc Sci Med. 2021;270:8. doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.LeBreton J., Senter J. Answers to 20 questions about interrater reliability and interrater agreement. Organ Res Methods. 2008;11(4):815–852. doi: 10.1177/1094428106296642. [DOI] [Google Scholar]
- 50.Lehberger M., Kleih A.-K., Sparke K. Panic buying in times of coronavirus (COVID-19): Extending the theory of planned behavior to understand the stockpiling of nonperishable food in Germany. Appetite. 2021;161:105118. doi: 10.1016/j.appet.2021.105118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leng A.L., Maitland E., Wang S.Y., Nicholas S., Liu R.G., Wang J. Individual preferences for COVID-19 vaccination in China. Vaccine. 2021;39(2):247–254. doi: 10.1016/j.vaccine.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li L.i., Liu Y., Wu P., Peng Z., Wang X., Chen T., et al. Influenza-associated excess respiratory mortality in China, 2010–15: A population-based study. Lancet Public Health. 2019;4(9):e473. doi: 10.1016/S2468-2667(19)30163-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lindell M.K. In: Handbook of Disaster Research. 2nd ed. Rodríguez H., Trainor J., Donner W., editors. Springer; New York: 2018. Communicating imminent risk; pp. 449–477. [Google Scholar]
- 54.Lindell M.K., Arlikatti S., Prater C.S. Why people do what they do to protect against earthquake risk: Perceptions of hazard adjustment attributes. Risk Anal. 2009;29(8):1072–1088. doi: 10.1111/j.1539-6924.2009.01243.x. [DOI] [PubMed] [Google Scholar]
- 55.Lindell M.K., Perry R.W. The Protective Action Decision Model: Theoretical modifications and additional evidence. Risk Anal. 2012;32(4):616–632. doi: 10.1111/j.1539-6924.2011.01647.x. [DOI] [PubMed] [Google Scholar]
- 56.Lindell M.K., Prater C.S., Gregg C.E., Apatu E., Huang S.-K., Wu H.-C. Households’ immediate responses to the 2009 Samoa earthquake and tsunami. Int J Disaster Risk Reduct. 2015;12:328–340. doi: 10.1016/j.ijdrr.2015.03.003. [DOI] [Google Scholar]
- 57.Liu Z., Yang J. In the wake of scandals: How media use and social trust influence risk perception and vaccination intention among Chinese parents. Health Commun. 2021;36(10):1188–1199. doi: 10.1080/10410236.2020.1748834. [DOI] [PubMed] [Google Scholar]
- 58.Luo R.F., Liu C.F., Gao J.J., Wang T.Y., Zhi H.Y., Shi P.F., et al. Impacts of the COVID-19 pandemic on rural poverty and policy responses in China. J Integr Agric. 2020;19(12):2946–2964. doi: 10.1016/s2095-3119(20)63426-8. [DOI] [Google Scholar]
- 59.MacPherson-Krutsky C.C., Brand B.D., Lindell M.K. From information to public preparedness in the Cascadia Subduction Zone: Examining risk communication outcomes in Metropolitan Portland. OREarthquake Spectra. 2022;38(2):1223–1253. doi: 10.1177/87552930211057582. [DOI] [Google Scholar]
- 60.Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5(7):947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 61.Motta M., Slyvester S., Callaghan T., Lunz-Trujillo K., et al. Encouraging COVID-19 vaccine uptake through effective health communication. Frontiers in Political Science. 2021;28(3):2. doi: 10.3389/fpos.2021.630133. [DOI] [Google Scholar]
- 62.Naeem S.B., Bhatti R. The Covid-19 ‘infodemic’: A new front for information professionals. Health Info Libr J. 2020;37(3):233–239. doi: 10.1111/hir.12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nakaya N., Nemoto H., Yi C., Sato A., Shingu K., Shoji T., et al. Effect of tsunami drill experience on evacuation behavior after the onset of the Great East Japan Earthquake. Int J Disaster Risk Reduct. 2018;28:206–213. [Google Scholar]
- 64.National Bureau of Statistics. (2021). Census data. http://www.stats.gov.cn/tjsj/pcsj/.
- 65.National Health Commission of China. (2022). The latest situation of the COVID-19 pandemic. (Accessed January 1, 2022) http://www.nhc.gov.cn/wjw/xwdt/list.shtml.
- 66.Nehal K.R., Steendam L.M., Campos Ponce M., van der Hoeven M., Smit G.S.A. Worldwide vaccination willingness for COVID-19: A systematic review and meta-analysis. Vaccines. 2021;9(10) doi: 10.3390/vaccines9101071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nunnally J.C., Bernstein I.H. 3rd ed. McGraw-Hill; New York: 1994. Psychometric Theory. [Google Scholar]
- 68.Our World in Data (2022). Coronavirus (COVID-19) vaccinations. Oct 22, 2022. https://ourworldindata.org/covid-vaccinations.
- 69.Ott R.L., Longnecker M.T. Cengage Learning; 2015. Introduction to statistical methods & data analysis. [Google Scholar]
- 70.Priyadarsini S.L., Suresh M., Huisingh D. What can we learn from previous pandemics to reduce the frequency of emerging infectious diseases like COVID-19? Global Transitions. 2020;2:202–220. doi: 10.1016/j.glt.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Raman R., Vinuesa R., Nedungadi P., et al. Bibliometric analysis of SARS, MERS, and COVID-19 studies from India and connection to sustainable development goals. Sustainability. 2021;13(4):755. doi: 10.3390/su13147555. [DOI] [Google Scholar]
- 72.Sapkota S., Priyadarshini M. Impact of the COVID-19 on cancer management at Birat Medical College and Teaching Hospital, Nepal. Asian Journal of Medical Sciences. 2021;12(5):21–24. doi: 10.3126/ajms.v12i5.34024. [DOI] [Google Scholar]
- 73.Schuman H., Kalton G. In: Lindzey G., Aronson E., editors. Vol. 1. Random House; 1985. Survey methods; pp. 635–697. (Handbook of social psychology). [Google Scholar]
- 74.Schutt R.K. Sage publications; Los Angeles: 2018. Investigating the Social World: The Process and Practice of Research. [Google Scholar]
- 75.Sichuan Provincial Bureau of Statistics. (2021). Statistical yearbook of 2021. (Accessed January 1, 2022) http://tjj.sc.gov.cn/scstjj/c105855/nj.shtml.
- 76.Siegrist M. The necessity for longitudinal studies in risk perception research. Risk Anal. 2013;33(1):50–51. doi: 10.1111/j.1539-6924.2012.01941.x. [DOI] [PubMed] [Google Scholar]
- 77.Siegrist M. Longitudinal studies on risk research. Risk Anal. 2014;34(8):1376–1377. doi: 10.1111/risa.12249. [DOI] [PubMed] [Google Scholar]
- 78.Siegrist M., Gutscher H. Natural hazards and motivation for mitigation behavior: People cannot predict the affect evoked by a severe flood. Risk Anal. 2008;28(3):771–778. doi: 10.1111/j.1539-6924.2008.01049.x. [DOI] [PubMed] [Google Scholar]
- 79.Sjoberg L., Engelberg E. Risk perception and movies: a study of availability as a factor in risk perception. Risk Anal. 2010;30(1):95–106. doi: 10.1111/j.1539-6924.2009.01335.x. [DOI] [PubMed] [Google Scholar]
- 80.Soroya S.H., Farooq A., Mahmood K., Isoaho J., Zara S.E. From information seeking to information avoidance: Understanding the health information behavior during a global health crisis. Inf Process Manag. 2021;58(2):16. doi: 10.1016/j.ipm.2020.102440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sun Y., Hu Q., Grossman S., Basnyat I., Wang P. Comparison of COVID-19 information seeking, trust of information sources, and protective behaviors in China and the US. J Health Commun. 2021;26(9):657–666. doi: 10.1080/10810730.2021.1987590. [DOI] [PubMed] [Google Scholar]
- 82.Sun Y., Monnat S.M. Rural-urban and within-rural differences in COVID-19 vaccination rates. J Rural Health. 2022;38(4):916–922. doi: 10.1111/jrh.12625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Suresh V., Fishman R., von Lieres J.S., Rao B.R., et al. Impact of the COVID-19 lockdown on the economic situation and food security of rural households in India. Journal of Agribusiness in Developing and Emerging Economies. Journal of Agribusiness in Developing and Emerging Economies. 2022;12(3):491–509. doi: 10.1108/JADEE-07-2021-0177. [DOI] [Google Scholar]
- 84.Szmyd B., Karuga F.F., Bartoszek A., Staniecka K., Siwecka N., Bartoszek A., et al. Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: A cross-sectional study from Poland. Vaccines. 2021;9(3) doi: 10.3390/vaccines9030218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tang L., Zou W. Health information consumption under COVID-19 lockdown: An interview study of residents of Hubei Province. China Health Communication. 2021;36(1):74–80. doi: 10.1080/10410236.2020.1847447. [DOI] [PubMed] [Google Scholar]
- 86.Terpstra T., Lindell M.K. Citizens’ perceptions of flood hazard adjustments: An application of the Protective Action Decision Model. Environ Behav. 2013;45:993–1018. doi: 10.1177/0013916512452427. [DOI] [Google Scholar]
- 87.Wake A. The willingness to receive COVID-19 vaccine and its associated factors: “Vaccination refusal could prolong the war of this pandemic” A systematic review. Risk Management And Healthcare Policy. 2021;14:2609–2623. doi: 10.2147/RMHP.S311074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang F., Wei J., Huang S.-K., Lindell M., Ge Y., Wei H. Public reactions to the 2013 Chinese H7N9 Influenza outbreak: Perceptions of risk, stakeholders, and protective actions. J Risk Res. 2018;21(7):809–833. doi: 10.1080/13669877.2016.1247377. [DOI] [Google Scholar]
- 89.Wang J., Yuan B., Lu X., Liu X., Li L., Geng S., et al. Willingness to accept COVID-19 vaccine among the elderly and the chronic disease population in China. Hum Vaccin Immunother. 2021;17(12):4873–4888. doi: 10.1080/21645515.2021.2009290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang Y., Cheng M., Wang S., Wu F., Yan Q., Yang Q., et al. Vaccination coverage with the pneumococcal and influenza vaccine among persons with chronic diseases in Shanghai, China, 2017. BMC Public Health. 2020;20(1) doi: 10.1186/s12889-020-8388-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wei H.-L., Lindell M.K., Prater C.S., Wei J., Wang F. Texas households’ expected responses to seasonal influenza. J Risk Res. 2021;24(11):1405–1425. [Google Scholar]
- 92.World Health Organization (WHO). (2021). Coronavirus disease (COVID-19): Similarities and differences between COVID-19 and Influenza. Available at https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-similarities-and-differences-with-influenza.
- 93.Wyte-Lake T., Der-Martirosian C., Chu K.R., Johnson-Koenke R., Dobalian A. Preparedness and response activities of the US Department of Veterans Affairs (VA) home-based primary care program around the fall 2017 hurricane season. BMC Public Health. 2020;20(1):9. doi: 10.1186/s12889-020-09888-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ye M., Lyu Z. Trust, risk perception, and COVID-19 infections: Evidence from multilevel analyses of combined original dataset in China. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yin F.L., Wu Z.L., Xia X.Y., Ji M.Q., Wang Y.Y., Hu Z.W. Unfolding the determinants of COVID-19 vaccine acceptance in China. J Med Internet Res. 2021;23(1):17. doi: 10.2196/26089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yue L., Sun L., Yang K., Li Z. Research on the status quo and strategy of China’s medical and health system reform (in Chinese) China Health Industry. 2019;16(19):185–188. doi: 10.16659/j.cnki.1672-5654.2019.19.185. [DOI] [Google Scholar]
- 97.Zheng J., Morstead T., Sin N., Klaiber P., Umberson D., Kamble S., et al. Psychological distress in North America during COVID-19: The role of pandemic-related stressors. Soc Sci Med. 2021;270 doi: 10.1016/j.socscimed.2021.113687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhu F.C., Li Y.H., Guan X.H., Hou L.H., Wang W.J., Li J.X., et al. Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: A dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020;395(10240):1845–1854. doi: 10.1016/s0140-6736(20)31208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.