Summary
Background
No nosocomial infection was recorded in our healthcare workers (HCWs) during the early phase of the coronavirus disease 2019 (COVID-19) pandemic. With the emergence of the Omicron variant of increased transmissibility, infection in HCWs occurred as expected. We aimed to study the epidemiology of infection in HCWs and to describe the infection control measures during the outbreak of the Omicron variant.
Methods
With daily rapid antigen testing and molecular confirmation test for COVID-19, infected HCWs were interviewed by infection control nurses (ICNs) to investigate the potential source of infection. The epidemiology of COVID-19 in Hong Kong served as reference.
Results
During the fifth wave of COVID-19 (31 December 2021 to 31 May 2022), 1,200,068 cases were reported (incidence 95 times higher than in preceding waves in Hong Kong; 162,103 vs 1,707 per million population respectively, P<0.001). The proportion of infected HCWs was significantly higher than that of the general population (24.9%, 1,607/6,452 vs 16.2%, 1,200,068/7,403,100 respectively; P<0.01). The proportion of infected non-clinical staff was significantly higher than that of clinical staff (31.8%, 536/1,687 vs 22.5%, 1,071/4,765 respectively; P<0.001). Of 82.8% (1,330/1,607) infected HCWs interviewed by ICNs, 99.5% (1,324/1,330) had been fully vaccinated; 49.5% (659/1,330) had no identifiable source; 40.7% (541/1,330) were probably infected from household members; 9.8% (130/1,330) had possible exposure to confirmed patients or HCWs, but no lapse in infection control measures or inappropriate use of personal protective equipment was recalled.
Conclusion
Omicron variant is highly transmissible such that breakthrough infection occurred despite high level of vaccination.
Keywords: Healthcare workers, Vaccination, COVID-19, SARS-CoV-2, Omicron, Hong Kong
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was described as the first Disease X on the World Health Organization list of priority diseases requiring urgent research and development attention [1,2]. As of 18 September 2022, over 609 million confirmed cases and over 6.5 million deaths have been reported globally [3]. Infection and death among healthcare workers (HCWs) were not unusual, especially during the early phase of the pandemic [4]. In a systemic review of COVID-19 infection among HCWs, 152,888 infections and 1,413 deaths were reported globally as of 8 May 2020. Deaths among HCWs constituted 0.52% of total population of COVID-19 deaths [5].
In Hong Kong, infection control and public health response was immediately activated following the official announcement of the community-acquired pneumonia outbreak in Wuhan, Hubei Province by the National Health Commission of the People's Republic of China on 31 December 2019 [6,7]. Protection of HCWs from nosocomial acquisition of SARS-CoV-2 was considered paramount because 8 HCWs died during the outbreak of severe acute respiratory syndrome (SARS) in 2003. With stringent infection control measures, there was no nosocomial infection with SARS-CoV-2 among HCWs up till the pre-Omicron phase [[8], [9], [10]].
The emergence of Omicron sublineages (BA.1, BA.2 to BA.4 and BA.5) of increasing transmissibility [11] has resulted in explosive outbreaks in the community [[12], [13], [14], [15]]. Models simulating the household setting underscored the contribution of airborne transmission of the Omicron variant, especially during asymptomatic or pre-symptomatic infection, as compared with the ancestral strain [16]. HCWs could also be infected with SARS-CoV-2 in the community, especially during the Omicron wave. Here, we reported the epidemiology of COVID-19 infection among our HCWs and described our infection control measures during the outbreak of the SARS-CoV-2 Omicron variant.
Material and methods
Epidemiology of the fifth wave of COVID-19 Hong Kong
From the outset, the daily number of laboratory-confirmed COVID-19 cases was reported in the public domain of the Centre for Health Protection (CHP), Department of Health, the Government of Hong Kong Special Administrative Region, China [17]. The evolution of the COVID-19 epidemic from the first to the fourth wave in Hong Kong has been summarized previously [14]. The epidemic curve and public health responses were described.
Control of COVID-19 and burden of COVID-19 patients in the hospital
Infection control measures have evolved to minimize the risk of nosocomial outbreaks during the COVID-19 pandemic [[8], [9], [10]]. Briefly, the measures included staff training, directly observed donning and doffing of personal protective equipment (PPE), enforcement of hand hygiene and environmental disinfection, as well as proactive screening and isolation of COVID-19 patients in airborne infection isolation rooms (AIIRs). In the fifth wave, some of the general wards were temporarily converted into negative pressure wards (NPWs) for COVID-19 patients in view of the high occupancy of the AIIRs in Queen Mary Hospital (QMH), a 1,700-bed university-affiliated hospital. COVID-19 patients with clinical improvement were transferred to four extended-care hospitals in our healthcare network. For hospitalized patients, universal admission screening by real-time reverse transcription polymerase chain reaction (RT-PCR) using deep throat saliva (DTS) or nasopharyngeal swab (NPS) specimens was performed. While awaiting RT-PCR results upon admission, patients were managed in designated cubicles, namely surveillance cubicles, in general wards with 6 air changes per hour. Portable air purifiers were placed inside the surveillance cubicles to improve air dilution. Patients with positive RT-PCR results for SARS-CoV-2 were immediately transferred to AIIRs or NPWs which were designated for COVID-19 patients. Patients with negative SARS-CoV-2 results were transferred to other cubicles in general wards. In general wards, repeated testing was undertaken if the patient had clinical features suggestive of COVID-19. The extent of contact tracing for potential secondary cases would depend on risk assessment by the infection control team. For the purpose of the current study, patients with positive SARS-CoV-2 RNA detection 3 or more days after hospitalization were defined as nosocomial cases, so as to include as many nosocomial cases as possible for analysis. For nosocomial COVID-19 cases, sporadic cases referred to isolated cases, whereas clusters referred to ≥ 2 cases. The number of COVID-19 patient admissions and bed occupancy in our network during the fifth wave were recorded.
COVID-19 testing among HCWs
HCWs were encouraged to refrain from work if they had fever or respiratory symptoms. Self-collected DTS specimens were sent to the hospital microbiology laboratory for SARS-CoV-2 RNA detection by RT-PCR if HCWs had symptoms or any epidemiological exposure to COVID-19. Since 21 February 2022, all HCWs were required to perform a rapid antigen test (GLINE-2019-nCoV Ag, BGI, China) by self-collected nasal swabs before work. If the rapid antigen test result was positive, HCWs were required to perform another rapid antigen test to ensure a consistent positive result. HCWs with immediately repeated positive rapid antigen test results were required to refrain from work and to proceed with a confirmatory test by RT-PCR using DTS. Infected HCWs would be interviewed by an infection control nurse (ICN) to assess the potential source of infection. Possible exposure to COVID-19 was defined as HCWs having contacted a COVID-19 case in either hospital or community setting, regardless of appropriateness of PPE, in the past 5 days. Nosocomial COVID-19 infection among HCWs was defined as staff who had inappropriate PPE when caring for a COVID-19 patient in the past 5 days. Appropriate PPE included the use of a surgical respirator, cap, face shield, gown, and gloves.
COVID-19 vaccination among HCWs
Two formulations of COVID-19 vaccines were available for HCWs since March 2021: CoronaVac, inactivated whole cell vaccine, Sinovac Biotech (Hong Kong) Limited, and BNT162b2 mRNA vaccine, BioNTech, Fosun Pharma in collaboration with the German drug manufacturer. HCWs with direct patient care were required to complete the second dose of COVID-19 vaccination by 16 February 2022. All uninfected HCWs were required to complete the second dose by 1 April 2022. The deadline of receiving the third dose was 16 May 2022, or within 150 calendar days from the second dose, whichever later. HCWs who recovered from COVID-19 were required to complete 2 doses of COVID-19 vaccination unless they had already completed the second or third dose of vaccination before infection. Exemption of vaccination was provided to staff with medical contraindication.
Viral load assessment of respiratory specimens
For clinical specimens, total nucleic acid extraction was performed using 250 μL of the specimen by the eMAG extraction system (bioMérieux, Marcy-l'Etoile, France) following the manufacturer's instructions. Quantification of SARS-CoV-2 RNA was performed by RT-PCR as previously described [18].
This study was approved by the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong West Hospital Cluster.
Statistical analysis
The Chi-Square test was used to compare independent categorical variables between groups. All reported P values were two-sided. A P value of <0.05 was considered statistically significant. Computation was performed using the SPSS Version 15.0 for Windows.
Results
Epidemiology of the fifth wave of COVID-19 in Hong Kong
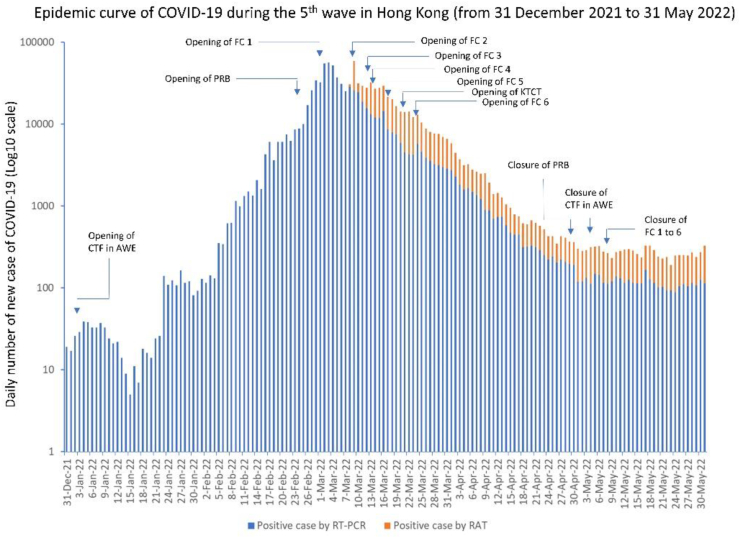
Soon after the importation of the SARS-CoV-2 Omicron variant [19], the fifth wave of COVID-19 in Hong Kong commenced on 31 December 2021, which was the second anniversary of the official announcement of community-acquired pneumonia of unknown etiology in Wuhan, Hubei Province [6]. During the fifth wave (defined as 31 December 2021 to 31 May 2022 in the current study), a total of 1,200,068 COVID-19 cases were reported to CHP. The incidence of COVID-19 during the fifth wave was 95 times higher than the total from the first to fourth wave (n=12,636) in Hong Kong (162,103 vs 1,707 per million population respectively, P<0.001). The daily number of new cases exceeded 10,000 on 25 February 2022 and reached a peak of >50,000 on 3 March 2022, amounting to 1,352 and >7,676 per million population respectively. As of 31 May 2022, there were 9,165 deaths within the fifth wave (1,238 per million population), of which 6,507 (71.0%) and 1,534 (16.7%) were aged ≥ 80 and 70–79 years respectively. Among the fatal cases, 6,923 out of 9,165 (75.5.%) had not received any COVID-19 vaccine, while the vaccination coverage of the first, second, and third dose in the Hong Kong population was 6,700,406 (90.5%), 6,332,041 (85.5%), and 3,876,310 (52.4%) respectively [20]. The epidemic curve and public health responses by managing cases in community isolation facilities in the Asia World-Expo (∼1,000 beds), public rental buildings (∼3,000 residential flats), fangcang shelters (∼20,000 beds), and Kai Tak cruise terminal (∼1,000 beds) are shown in Figure 1.
Figure 1.
Epidemic curve of COVID-19 during the fifth wave in Hong Kong (31 December 2021 to 31 May 2022). Note. CTF in AWE, community treatment facility of around 1,000 beds in Asia World-Expo which was re-opened on 2 January 2022; FC, fangcang shelter for the purpose of community isolation facility. FC1 denotes fangcang shelter located in Tsing Yi which was opened on 1 March 2022; FC2 denotes fangcang shelter located in San Tin which was opened on 9 March 2022; FC3 denotes fangcang shelter located in Hong Kong-Zhuhai-Macao Bridge which was opened on 12 March 2022; FC4 denotes fangcang shelter located in Fanling which was opened on 13 March 2022; FC5 denotes fangcang shelter located in Hung Shui Kiu which was opened on 17 March 2022; FC6 denotes fangcang shelter located in Tam Mi which was opened on 24 March 2022. All six fangcang shelters were purposely built as community isolation facilities to provide a total of 20,000 beds; KTCT denotes Kai Tak cruise terminal which was converted into community isolation facility and opened on 21 March 2022 to provide around 1,000 beds; PRB denotes public rental buildings, Queens Hill Estate, located in Fanling, and Heng King House of Lai King Estate, located in Kwai Chung, which were converted into community isolation facility and opened on 24 February 2022 to provide around 3,000 residential flats; RAT, rapid antigen test; RT-PCR, reverse transcription polymerase chain reaction.
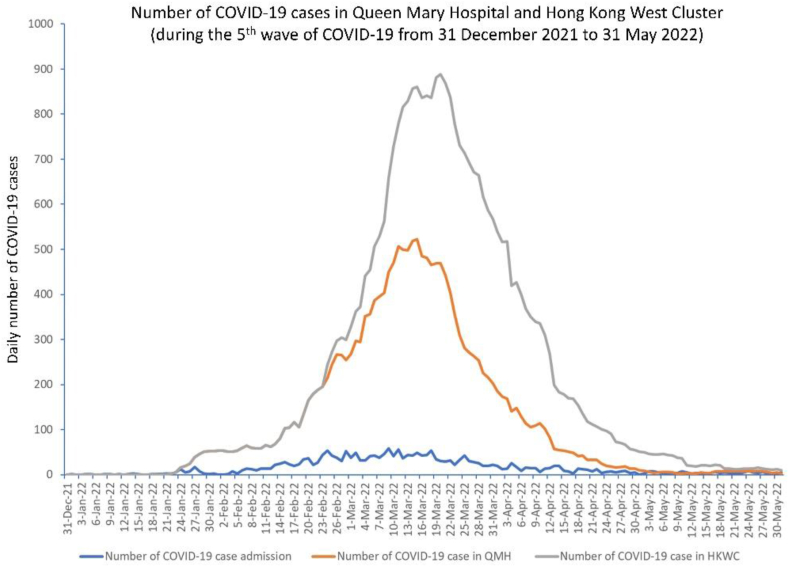
Control of COVID-19 and burden of COVID-19 in the hospital
With increasing COVID-19 patient admissions during the fifth wave, up to 50% of beds in the general wards were temporarily converted into NPWs caring for COVID-19 patients. Mobile Modular High Efficiency Particulate Arrestance Filter Units (MMHUs) and exhaust fans were installed in each cubicle to increase air changes per hour from 6 to 10. Negative pressure was established with airflow from the corridor to the cubicles. Of 2,320 COVID-19 patients admitted to QMH, 1,284 were male and 1,036 female, with a median age of 73 years (range: 8 days to 107 years). The daily numbers of COVID-19 patient admissions and bed occupancy during the fifth wave are shown in Figure 2.
Figure 2.
Number of COVID-19 cases in Queen Mary Hospital and Hong Kong West Cluster during the fifth wave of COVID-19. Note. HKWC, Hong Kong West Cluster; QMH, Queen Mary Hospital. Hong Kong West Cluster is a healthcare network comprising Queen Mary Hospital, a 1,700-bed university-affiliated tertiary referral center, and another 5 extended-care hospitals with a total of 1,700 beds. During the fifth wave of COVID-19, four out of 5 extended-care hospitals received clinically stable COVID-19 from Queen Mary Hospital.
During the study period, 37 nosocomial COVID-19 patients were diagnosed at a median of 12 days (range, 3–158 days) after hospitalization in 16 general wards without conversion to NPWs. There were 10 sporadic cases in 10 different general wards. The remaining 27 patients comprised 6 clusters in 6 different general wards, including 12 cases in 1 cluster. ICNs coordinated infection control measures when a nosocomial COVID-19 patient was diagnosed. Nosocomial COVID-19 patients were immediately transferred to AIIRs to reduce the risk of further transmission in the general wards. Terminal disinfection of the general ward was performed. Hand hygiene among HCWs and patients were enforced based on our previous experience on outbreak prevention and control [[21], [22], [23], [24], [25]]. All exposed patients and HCWs in the general ward were tested for SARS-CoV-2 by RT-PCR daily for 7 days for early recognition of secondary cases.
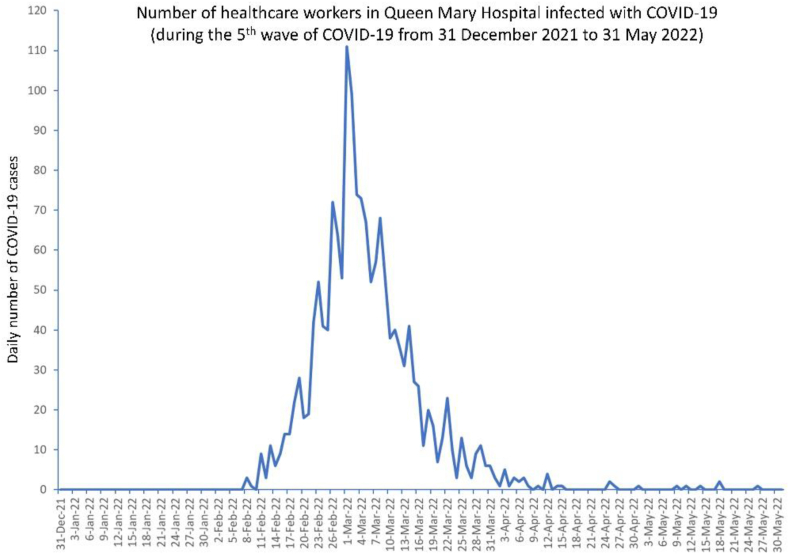
COVID-19 infection among HCWs
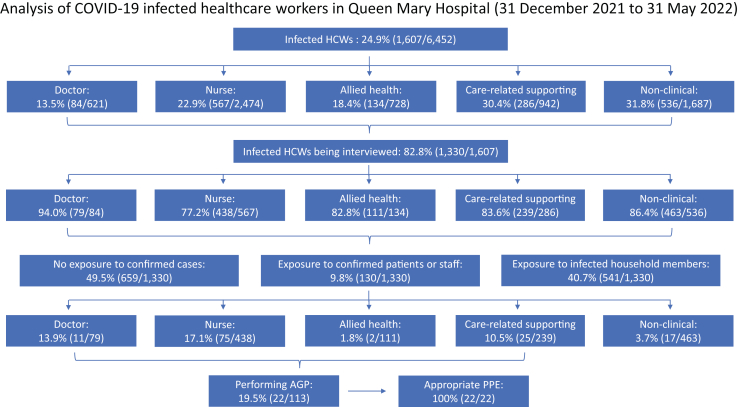
During the fifth wave, a total of 1,607 (24.9%) of 6,452 HCWs in QMH were tested positive for COVID-19 till 31 May 2022 (Figure 3). The proportion of infected HCWs was significantly higher than that of the general population in Hong Kong (24.9%, 1,607/6,452 vs 16.2%, 1,200,068/7,403,100 respectively; P<0.001). The proportion of infected non-clinical staff was significantly higher than that of clinical staff (31.8%, 536/1,687 vs 22.5%, 1,071/4,765 respectively; P<0.001). Among 1,607 infected HCWs, 1,330 (82.8%) were interviewed by an ICN by phone. None had history of past infection of COVID-19. Symptomatic infection was reported in 1,050 (78.9%) HCWs. Symptoms included sore throat (53.8%, 565), cough (27.1%, 285), fever (19.9%, 209), runny nose (12.8%, 134) and headache (7.0%, 74). Among the 1,330 interviewees, 659 (49.5%) did not report any exposure to cases in the household or hospital. Another 541 (40.7%) reported contact with infected household members. The remaining 130 (9.8%) recalled possible exposure in the past 5 days to patients or staff within or outside the hospital, who were subsequently diagnosed to have COVID-19. Among this group of 130 HCWs, 113 were clinical staff, with 22 (19.5%) having performed aerosol generating procedures (AGPs) for COVID-19 patients with full PPE (Figure 4). Six (0.5%) out of 1,330 infected HCWs had not received any COVID-19 vaccine. Only 1% of the staff was exempted from COVID-19 vaccination in our healthcare network as of 31 May 2022.
Figure 3.
Number of healthcare workers in Queen Mary Hospital infected with COVID-19. Note. The peak of healthcare worker infection occurred earlier than the peak of COVID-19 cases in the community and the hospital. It was the result of effort of infection control nurses to remind healthcare workers to avoid social gathering and obey social distancing when there was increasing HCW infection.
Figure 4.
Analysis of COVID-19 infected healthcare workers in Queen Mary Hospital (31 December 2021 to 31 May 2022). Non-clinical staff includes administrative, clerical, and non-care related supporting staff. AGP, aerosol generating procedures; PPE, personal protective equipment.
Discussion
During the fifth wave of COVID-19 predominantly caused by Omicron subvariant BA.2 in Hong Kong, an unprecedented number of COVID-19 infections was reported among our HCWs even though infection control practices in the healthcare setting remained stringently enforced throughout the COVID-19 pandemic. Our finding of HCWs infection was in contrast with the observation in the early phase of the COVID-19 pandemic in Hong Kong that nosocomial infection among HCWs was not recorded in hospitals [9,10], temporary test centers [26], and community isolation and treatment facilities [27]. Nosocomial infection of nine HCWs was only reported in a COVID-19 outbreak in late 2020 [18]. In this study, about one-fourth of HCWs were infected in our hospital and the proportion was comparable to a private hospital of 600-bed in Hong Kong [28]. It is important to explore if the infection control measures remained appropriate to protect our HCWs.
Before the onset of the fifth wave of COVID-19, we adopted a hospital-based approach that all suspected or confirmed COVID-19 patients were isolated in healthcare facilities, including AIIRs in the hospitals or community treatment facilities. This approach of institutionalization for containment could have minimized community transmission of COVID-19. In the healthcare facilities, HCWs were provided with full PPE including a surgical respirator, cap, face shield, gown, and gloves during patient care. Directly observed donning and doffing was enforced to maximize staff protection and minimize the risk of self-contamination upon removal of PPE. With the evolution of SARS-CoV-2, RNA of the virus has been increasingly detected in air samples collected in AIIRs with 12 air changes per hour [29,30]. However, the quantitation of viral RNA was as low as 0.005 genome copies per litre of air [30]. The provision of full PPE should be sufficient to protect HCWs from inhalation of SARS-CoV-2.
With the emergence of SARS-CoV-2 Omicron subvariant BA.2 in the fifth wave, there were explosive outbreaks in the community, especially during mask-off activities in restaurants [31] as well as vertical transmission in high-rise residential buildings [13,14]. Although the operation of community isolation facilities in the Asia World-Expo, public rental buildings, fangcang shelters, and Kai Tak cruise terminal had provided some 25,000 additional beds to manage patients with mild or asymptomatic COVID-19 infection, this was still insufficient to cope with the approach of institutionalization for containment during the peak of the fifth wave, with more than 10,000 confirmed cases per day. HCWs thus could also have acquired infection in the community. In fact, about 50% of HCWs had no identifiable source of infection in the household or the hospital setting based on our epidemiological analysis, suggesting widespread transmission of COVID-19 in the community.
The proportion of infected HCWs was significantly higher than that of our general population. It may be related to the policy of daily COVID-19 testing among the HCWs that the number of tests per HCW was significantly higher than that of the general population during the study period (unpublished data) according to the statistics on testing for COVID-19 in Hong Kong [32]. In fact, daily COVID-19 testing detected an additional 19% of asymptomatic cases among our HCWs in this study. In a systemic analysis of COVID-19 infection, frontline HCWs were more likely to report a positive COVID-19 test when compared with community individuals in the United Kingdom and the United States [33]. In our study, it is interesting to observe that the proportion of infected non-clinical staff was significantly higher than that of clinical staff. The alertness of clinical staff may be higher as a result of on-going infection control training. Hand hygiene among our clinical staff remained highly compliant during the COVID-19 pandemic [34].
Nosocomial acquisition of SARS-CoV-2 remains difficult to ascertain because our HCWs, especially clinical staff, were not under closed-loop management in the hospital as in mainland China [35]. Clinical staff who had performed AGP for COVID-19 patients reported having donned full PPE during patient care. None of our clinical staff fulfilled the case definition of nosocomial COVID-19 infection. However, about 10% of HCWs, including clinical and non-clinical staff, recalled possible exposure to patients in the general wards or infected HCWs. The possibility of COVID-19 transmission from patient to HCWs or HCWs to HCWs could not be excluded. In fact, 80% of air samples collected in NPWs caring for COVID-19 patients were positive for SARS-CoV-2 RNA [36]. Based on the results, air dispersal of SARS-CoV-2 in general wards with unrecognized COVID-19 patients would be possible. This may also explain the presence of 37 hospitalized patients with nosocomial acquisition of SARS-CoV-2 in general wards during our study period.
Universal masking has been adopted in our community and healthcare settings even before the announcement of the COVID-19 pandemic [37,38]. Universal masking was also recommended by the Centers for Disease Control and Prevention of the United States [39], and maximizing the fitness of the mask was further emphasized [40]. Experimental studies demonstrated that surgical masks were effective at preventing virus spread under conditions of low virus load, whereas more advanced masks were required in potentially virus-rich indoor environments including medical centers and hospitals [41]. Recent studies showed that the universal use of surgical respirators as an additional infection preventive measure contributed to the rapid control of Omicron transmission in the hospital [42]. Use of the surgical respirator by an infected HCW may be one of the reasons for the lack of Omicron transmission in a cohort of immunosuppressed patients [43]. These preliminary findings may provide indirect epidemiological evidence of airborne transmission of the Omicron variant in the clinical areas. The use of surgical masks or surgical respirators to minimize the risk of Omicron transmission in the healthcare setting deserves further investigation.
There are several limitations in this study. Firstly, we did not perform case-control analysis to investigate the risk factors for COVID-19 infection among HCWs, because 50% of them could not identify the source of infection during overwhelming transmission of COVID-19 in the community. Secondly, we were not able to perform detailed epidemiological analysis for HCWs who recalled possible exposure to infected patients or staff within or outside the hospital. The route of transmission thus could not be definitively ascertained. Thirdly, we did not perform whole genome sequencing analysis to establish the transmission relationships, as the predominant virus circulating in both the community and hospitals was already known to be subvariant BA.2 during the study period [13,36]. Fourthly, we defined nosocomial COVID-19 cases as patients with positive SARS-CoV-2 RNA detection 3 or more days after hospitalization. As the mean incubation period of COVID-19 was 3.42 days for the Omicron variant [44], misclassification of a small proportion of nosocomial cases might have occurred. Finally, we did not analyze the relationship between the regimen of COVID-19 vaccination and the risk of infection. The impact of COVID-19 vaccination on HCW infections during circulation of the SARS-CoV-2 Omicron variant has been reported previously. Using the two-dose BNT162b2 regimen as reference, two-dose CoronaVac recipients had a significantly higher risk of infection, whereas three-dose BNT162b2 and two-dose CoronaVac plus BNT162b2 booster regimens were associated with a lower risk of infection [28].
Conclusions
SARS-CoV-2 Omicron variant is highly transmissible such that breakthrough infection might occur despite a high level of vaccination coverage in the population. Although a significant proportion of HCWs were infected, none had severe infection, underpinned by a high vaccination rate. Nosocomial transmission of COVID-19 from patients to HCWs could not be ascertained by epidemiological analysis in view of the component of airborne transmission.
Acknowledgments
We are grateful to the contribution of our frontline staff and laboratory staff in enforcing the infection control measures and performing the laboratory work in the Queen Mary Hospital.
Funding statement
This study was partially supported by the Health and Medical Research Fund (HMRF) Commissioned Research on Control of Infectious Disease (Phase IV), CID-HKU1-16, Health Bureau, Hong Kong SAR Government.
Conflicts of interest statement
All authors report no conflicts of interest relevant to this article.
Credit Author Statement
Shuk-Ching Wong: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing - original draft, Writing - review and editing. Veronica Wing-Man Chan: Investigation. Lithia Lai-Ha Yuen: Investigation. Christine Ho-Yan AuYeung: Investigation. Jessica Oi-Yan Leung: Investigation. Chi-Kuen Li: Investigation. Monica Oi-Tung Kwok: Investigation. Simon Yung-Chun So: Data curation, Formal analysis. Jonathan Hon-Kwan Chen: Resources. Kelvin Hei-Yeung Chiu: Resources. Anthony Raymond Tam: Resources. Ivan Fan-Ngai Hung: Resources. Kelvin Kai-Wang To: Resources. Janice Yee-Chi Lo: Writing - review and editing. Kwok-Yung Yuen: Funding acquisition, Supervision. Vincent Chi-Chung Cheng: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing - original draft, Writing - review and editing. All authors have read and agreed to the published version of the manuscript.
References
- 1.Jiang S., Shi Z.L. The First Disease X is Caused by a Highly Transmissible Acute Respiratory Syndrome Coronavirus. Virol Sin. 2020;35:263–265. doi: 10.1007/s12250-020-00206-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bloom D.E., Cadarette D. Infectious Disease Threats in the Twenty-First Century: Strengthening the Global Response. Front Immunol. 2019;10:549. doi: 10.3389/fimmu.2019.00549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Covid-19 Weekly Epidemiological Update. Edition 109 published 14 September 2022. World Health Organization. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19-21-september-2022 (Accessed 24 September 2022).
- 4.COVID-19 has infected some 570,000 health workers and killed 2,500 in the Americas. Pan American health organization. World Health Organization. https://www.paho.org/en/news/2-9-2020-covid-19-has-infected-some-570000-health-workers-and-killed-2500-americas-paho (Accessed 19 September 2022).
- 5.Bandyopadhyay S., Baticulon R.E., Kadhum M., Alser M., Ojuka D.K., Badereddin Y., et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health. 2020;5:e003097. doi: 10.1136/bmjgh-2020–3097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Centre for Health Protection closely monitors cluster of pneumonia cases on Mainland. Press release of the Department of Health, Hong Kong Special Administrative Region. https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htm. (Accessed 19 September 2022).
- 7.Cheng V.C.C., Wong S.C., To K.K.W., Ho P.L., Yuen K.Y. Preparedness and proactive infection control measures against the emerging novel coronavirus in China. J Hosp Infect. 2020;104:254–255. doi: 10.1016/j.jhin.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y., et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng V.C.C., Wong S.C., Chuang V.W.M., So S.Y.C., Chen J.H.K., Sridhar S., et al. Absence of nosocomial transmission of coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in the prepandemic phase in Hong Kong. Am J Infect Control. 2020;48:890–896. doi: 10.1016/j.ajic.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng V.C., Wong S.C., Tong D.W., Chuang V.W., Chen J.H., Lee L.L., et al. Multipronged infection control strategy to achieve zero nosocomial coronavirus disease 2019 (COVID-19) cases among Hong Kong healthcare workers in the first 300 days of the pandemic. Infect Control Hosp Epidemiol. 2022;43:334–343. doi: 10.1017/ice.2021.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shrestha L.B., Foster C., Rawlinson W., Tedla N., Bull R.A. Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: Implications for immune escape and transmission. Rev Med Virol. 2022;32 doi: 10.1002/rmv.2381. e2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim E.Y., Choe Y.J., Park H., Jeong H., Chung J.H., Yu J., et al. Community Transmission of SARS-CoV-2 Omicron Variant, South Korea. Emerg Infect Dis. 2021;2022(28):898–900. doi: 10.3201/eid2804.220006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng V.C.C., Ip J.D., Chu A.W.H., Tam A.R., Chan W.M., Abdullah S.M.U., et al. Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Omicron Subvariant BA.2 in a Single-Source Community Outbreak. Clin Infect Dis. 2022;75:e44–e49. doi: 10.1093/cid/ciac203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng V.C., Wong S.C., Au A.K., Zhang C., Chen J.H., So S.Y., et al. Explosive outbreak of SARS-CoV-2 Omicron variant is associated with vertical transmission in high-rise residential buildings in Hong Kong. Build Environ. 2022;109323:221. doi: 10.1016/j.buildenv.2022.109323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Z., Deng X., Fang L., Sun K., Wu Y., Che T., et al. Epidemiological characteristics and transmission dynamics of the outbreak caused by the SARS-CoV-2 Omicron variant in Shanghai, China: A descriptive study. Lancet Reg Health West Pac. 2022;100592:29. doi: 10.1016/j.lanwpc.2022.100592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ji S., Xiao S., Wang H., Lei H. Increasing contributions of airborne route in SARS-CoV-2 omicron variant transmission compared with the ancestral strain. Build Environ. 2022;109328:221. doi: 10.1016/j.buildenv.2022.109328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Covid-19 Thematic Website. Centre for Health Protection. Department of Health. The Government of the Hong Kong Special Administrative Region. https://www.coronavirus.gov.hk/eng/index.html (Accessed 24 September 2022).
- 18.Cheng V.C., Fung K.S., Siu G.K., Wong S.C., Cheng L.S., Wong M.S., et al. Nosocomial Outbreak of Coronavirus Disease 2019 by Possible Airborne Transmission Leading to a Superspreading Event. Clin Infect Dis. 2021;73:e1356–e1364. doi: 10.1093/cid/ciab313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong S.C., Au A.K., Chen H., Yuen L.L., Li X., Lung D.C., et al. Transmission of Omicron (B.1.1.529) - SARS-CoV-2 Variant of Concern in a designated quarantine hotel for travelers: a challenge of elimination strategy of COVID-19. Lancet Reg Health West Pac. 2022;100360:18. doi: 10.1016/j.lanwpc.2021.100360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Statistics on 5th Wave of COVID-19. Centre for Health Protection. Department of Health. The Government of the Hong Kong Special Administrative Region. https://www.coronavirus.gov.hk/eng/5th-wave-statistics.html# (Accessed 24 September 2022).
- 21.Cheng V.C., Tai J.W., Li W.S., Chau P.H., So S.Y., Wong L.M., et al. Implementation of directly observed patient hand hygiene for hospitalized patients by hand hygiene ambassadors in Hong Kong. Am J Infect Control. 2016;44:621–624. doi: 10.1016/j.ajic.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 22.Cheng V.C., Tai J.W., Chau P.H., Lai C.K., Chuang V.W., So S.Y., et al. Successful control of emerging vancomycin-resistant enterococci by territory-wide implementation of directly observed hand hygiene in patients in Hong Kong. Am J Infect Control. 2016;44:1168–1171. doi: 10.1016/j.ajic.2016.03.050. [DOI] [PubMed] [Google Scholar]
- 23.Cheng V.C.C., Wong S.C., Wong I.W.Y., Chau P.H., So S.Y.C., Wong S.C.Y., et al. The challenge of patient empowerment in hand hygiene promotion in health care facilities in Hong Kong. Am J Infect Control. 2017;45:562–565. doi: 10.1016/j.ajic.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 24.Cheng V.C.C., Wong S.C., Wong S.C.Y., Yuen K.Y. Directly observed hand hygiene - from healthcare workers to patients. J Hosp Infect. 2019;101:380–382. doi: 10.1016/j.jhin.2018.11.016. [DOI] [PubMed] [Google Scholar]
- 25.Wong S.C., Chau P.H., So S.Y., Lam G.K., Chan V.W., Yuen L.L., et al. Control of Healthcare-Associated Carbapenem-Resistant Acinetobacter baumannii by Enhancement of Infection Control Measures. Antibiotics (Basel) 2022;11:1076. doi: 10.3390/antibiotics11081076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong S.C., Leung M., Lee L.L., Chung K.L., Cheng V.C. Infection control challenge in setting up a temporary test centre at Hong Kong International Airport for rapid diagnosis of COVID-19 due to SARS-CoV-2. J Hosp Infect. 2020;105:571–573. doi: 10.1016/j.jhin.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong S.C., Leung M., Tong D.W., Lee L.L., Leung W.L., Chan F.W., et al. Infection control challenges in setting up community isolation and treatment facilities for patients with coronavirus disease 2019 (COVID-19): Implementation of directly observed environmental disinfection. Infect Control Hosp Epidemiol. 2021;42:1037–1045. doi: 10.1017/ice.2020.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zee S.T., Kwok L.F., Kee K.M., Fung L.H., Luk W.P., Chan T.L., et al. Impact of COVID-19 Vaccination on Healthcare Worker Infection Rate and Outcome during SARS-CoV-2 Omicron Variant Outbreak in Hong Kong. Vaccines (Basel) 2022;1322:10. doi: 10.3390/vaccines10081322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheng V.C., Wong S.C., Chan V.W., So S.Y., Chen J.H., Yip C.C., et al. Air and environmental sampling for SARS-CoV-2 around hospitalized patients with coronavirus disease 2019 (COVID-19) Infect Control Hosp Epidemiol. 2020;41:1258–1265. doi: 10.1017/ice.2020.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong S.C., Yuen L.L., Chan V.W., Chen J.H., To K.K., Yuen K.Y., et al. Airborne transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): What is the implication of hospital infection control? Infect Control Hosp Epidemiol. 2022;43:1522–1523. doi: 10.1017/ice.2021.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng V.C., Lung D.C., Wong S.C., Au A.K., Wang Q., Chen H., et al. Outbreak investigation of airborne transmission of Omicron (B.1.1.529) - SARS-CoV-2 variant of concern in a restaurant: Implication for enhancement of indoor air dilution. J Hazard Mater. 2022;128504:430. doi: 10.1016/j.jhazmat.2022.128504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Statistics on testing for COVID-19 in Hong Kong. https://www.chp.gov.hk/files/pdf/statistics_on_covid_19_testing.pdf (Accessed 10 November 2022).
- 33.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.G., Ma W., et al. Coronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong S.C., AuYeung C.H., Lam G.K., Leung E.Y., Chan V.W., Yuen K.Y., et al. Is it possible to achieve 100 percent hand hygiene compliance during the coronavirus disease 2019 (COVID-19) pandemic? J Hosp Infect. 2020;105:779–781. doi: 10.1016/j.jhin.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bai D.S., Geng P., Wang Z.D., Wang X.L., Xu G.R., Ye Q., et al. Practice and experience of regional medical center entrance linkage and closed-loop management under the wartime situation of the COVID-19 in China. Ann Transl Med. 2022;112:10. doi: 10.21037/atm-22-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wong S.C., Chan V.W., Yuen L.L., AuYeung C.H., Leung J.O., Li C.K., et al. Air dispersal of SARS-CoV-2 in general wards: implication on hospital infection control during the fifth wave of COVID-19 due to Omicron variant in Hong Kong. Infect Control Hosp Epidemiol. 2022 Oct 24:1–4. doi: 10.1017/ice.2022.258. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 37.Cheng V.C., Wong S.C., Chuang V.W., So S.Y., Chen J.H., Sridhar S., et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong S.C., Lam G.K., AuYeung C.H., Chan V.W., Wong N.L., So S.Y., et al. Absence of nosocomial influenza and respiratory syncytial virus infection in the coronavirus disease 2019 (COVID-19) era: Implication of universal masking in hospitals. Infect Control Hosp Epidemiol. 2021;42:218–221. doi: 10.1017/ice.2020.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Honein M.A., Christie A., Rose D.A., Brooks J.T., Meaney-Delman D., Cohn A., et al. CDC COVID-19 Response Team Summary of Guidance for Public Health Strategies to Address High Levels of Community Transmission of SARS-CoV-2 and Related Deaths. MMWR Morb Mortal Wkly Rep. December 2020;2020(69):1860–1867. doi: 10.15585/mmwr.mm6949e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brooks J.T., Beezhold D.H., Noti J.D., Coyle J.P., Derk R.C., Blachere F.M., et al. Maximizing Fit for Cloth and Medical Procedure Masks to Improve Performance and Reduce SARS-CoV-2 Transmission and Exposure. MMWR Morb Mortal Wkly Rep. 2021;2021(70):254–257. doi: 10.15585/mmwr.mm7007e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheng Y., Ma N., Witt C., Rapp S., Wild P.S., Andreae M.O., et al. Face masks effectively limit the probability of SARS-CoV-2 transmission. Science. 2021;372:1439–1443. doi: 10.1126/science.abg6296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baker M.A., Rhee C., Tucker R., Badwaik A., Coughlin C., Holtzman M.A., et al. Rapid Control of Hospital-Based Severe Acute Respiratory Syndrome Coronavirus 2 Omicron Clusters Through Daily Testing and Universal Use of N95 Respirators. Clin Infect Dis. 2022;75:e296–e299. doi: 10.1093/cid/ciac113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Karan A., Ferguson J., Salinas J.L. Lack of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) transmission from a healthcare worker to a cohort of immunosuppressed patients during the SARS-CoV-2 omicron variant surge, California. Infect Control Hosp Epidemiol 2022 Jul. 2022;7:1–2. doi: 10.1017/ice.2022.175. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu Y., Kang L., Guo Z., Liu J., Liu M., Liang W. Incubation Period of COVID-19 Caused by Unique SARS-CoV-2 Strains: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.28008. e2228008. [DOI] [PMC free article] [PubMed] [Google Scholar]