Abstract
Combined hip arthroscopy and periacetabular osteotomy are used for the treatment of concomitant intra-articular hip pathology and acetabular dysplasia or instability. Traditionally, the procedure has been achieved with the use of a traction table or table attachment for the arthroscopic portion and then subsequent transfer of the patient to a fully radiolucent flat bed. In this article, we highlight the technique of a combined hip arthroscopy and periacetabular osteotomy procedure using a single bed attachment system.
Technique Video
Step-by-step demonstration of a combined hip arthroscopy with labral repair and femoral acetabular osteochondroplasty with subsequent periacetabular osteotomy performed on a single radiolucent traction table without a perineal post in a patient with femooracetabular impingement in the setting of hip dysplasia of the patient's right hip. Standard arthroscopy portals are created and an interportal arthrotomy is created between the modified midanterior (MMA) portal and the anterolateral (AL) portal. While viewing through the AL portal, the labrum is debrided through the MMA portal and suture anchors are placed through the distal anterolateral accessory (DALA) portal. A capsular retention suture is then placed through the DALA to retract the inferior capsule to obtain better visualization of the femoral neck, and an osteochondroplasty is performed. The retention suture is removed, and the capsule is closed. Once the hip arthroscopy portion is complete, the periacetabular osteotomy is begun on the same operative table. A bikini-line incision is made along the inguinal crease of the hip. The superior pubic ramus cut is made with the use of an osteotome. An interval is created between the medial femoral neck and the iliopsoas tendon to gain access for the ischial osteotomy. Finally, the iliac osteotomy is performed parallel to the roof of the acetabulum and connected to the ischial osteotomy site with the use of a curved, tined osteotome, with care taken to preserve the posterior column. A Schanz pin is then placed in the osteotomized portion of the acetabulum and used to manipulate the free fragment with the assistance of additional manipulation and traction of the lower extremity from the traction table to provide adequate hip joint coverage. Once the dysplasia has been corrected, the periacetabular osteotomy is fixed into place with four solid 4.5-mm stainless steel screws.
Combined hip arthroscopy and periacetabular osteotomy (PAO) are used for the treatment of concomitant intra-articular hip pathology and acetabular dysplasia or instability. Traditionally, the procedure has been achieved with the use of either a proprietary traction table or a traction attachment to a standard table for the arthroscopic portion and then subsequent transfer of the patient to a radiolucent flat bed for the PAO.1 The use of multiple beds can contribute to increased time under anesthesia, intraoperative complications, increased room traffic, and increased chances for contamination of the sterile field. In an effort to prevent these complications, lessen anesthesia time, and allow more efficient and effective management of this condition, this article focuses on a technique using a single radiolucent, post-free traction bed system (Pivot Guardian Distraction System; Stryker, Kalamazoo, MI).
Surgical Technique
The following surgical technique is described in Video 1.
Positioning
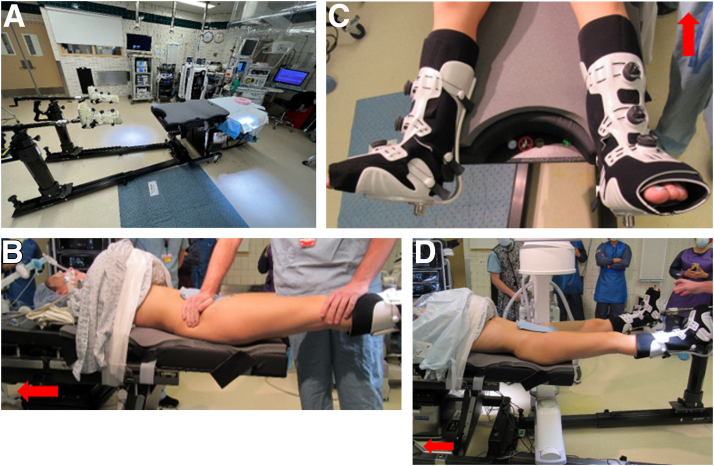
Surgery is performed by 2 fellowship-trained orthopaedic surgeons, one specializing in hip arthroscopy and the other in open hip preservation. This maximizes the outcomes of both procedures because they require quite different skill sets (Table 1). The arthroscopic portion is performed first to address intra-articular pathology such as femoroacetabular impingement, labral tears, and chondral injuries. An epidural catheter is placed prior to the start of the procedure to provide perioperative pain control and to minimize intraoperative blood loss by use of a hypotensive anesthesia technique. The surgical procedure is carried out using the Pivot Guardian Distraction System (Fig 1A). A standard operating room table with the bottom portion folded toward the floor is fitted with the Pivot Guardian Distraction System. The patient is placed supine on top of a friction pad made of dense foam that allows distraction of the operative hip without the need for a perineal post and obviates Trendelenburg positioning. The patient is placed with the iliac crest just distal to the radiopaque portion of the regular table (Video 1, Fig 1B). The patient’s feet are placed in well-padded boots designed to allow more uniform skeletal traction for the operative extremity and are secured in place (Fig 1C). The fluoroscope is positioned on the nonoperative side to provide intraoperative imaging as well as to confirm the appropriate amount of distraction, usually 8 to 10 mm, before entrance of the hip joint is attempted (Fig 1D). Traction is applied in a sequential manner with the operative leg held in slight abduction. The surgeon then applies gross inline traction and adduction to distract the hip. If more traction is needed, the fine adjustment lever is used until adequate space is obtained between the acetabulum and femoral head. This table also allows monitoring of the amount of force needed for appropriate hip distraction (Fig 2). A single preparation and drape are then used for both portions of the procedure.
Table 1.
Pearls and Pitfalls
| Pearls |
| Performing the hip arthroscopy prior to the PAO allows for preservation of the integrity of the hip capsule to maintain appropriate capsular pressure during hip arthroscopy and decrease the risk of fluid extravasation. |
| Performing the hip arthroscopy prior to the PAO allows for evaluation of articular cartilage quality; if there is significant cartilage injury, then the PAO can be disregarded because the benefits may not outweigh the risks. |
| A full-thickness capsulotomy is necessary to allow for appropriate visualization. |
| Creation of capsular flaps and placement of capsular retention sutures allow for improved visualization of the femoral neck during osteoplasty. |
| Capsular repair will limit fluid extravasation during the PAO. |
| The ASIS osteotomy allows for maintenance of the external oblique and flexor fascias and decreases the risk of iatrogenic injury to the LFCN. |
| Adequate anteversion of the acetabulum after PAO will provide appropriate posterior coverage to improve hip stability. |
| Pitfalls |
| Improper positioning during setup for the hip arthroscopy can lead to placement of the pelvis outside of the radiolucent zone of the operating table, which prohibits the use of fluoroscopy during the PAO. |
| The use of 2 lead surgeons who have are specialists in either hip arthroscopy or PAO is recommended. |
| Well-trained OR staff members who are comfortable in manipulating the leg holder are necessary throughout the peripheral portion of the hip arthroscopy to assess the osteoplasty. |
ASIS, anterior superior iliac spine; LFCN, lateral femoral cutaneous nerve; OR, operating room; PAO, periacetabular osteotomy.
Fig 1.
(A) Post-less distraction table (Pivot Guardian Distraction System). (B) Patient positioned supine on post-less distraction table preoperatively. The patient is positioned such that the iliac crest is just distal to the radiopaque portion of the regular table. (C) Boots associated with post-less distraction system. The boots are well padded and are designed to allow for uniform distraction of the operative extremity. (D) Preoperative imaging is obtained with the fluoroscope positioned appropriately patient positioning and hip joint distraction. The arrows point in the direction of the patient’s head.
Fig 2.
The tensiometer of the post-less distraction table allows for monitoring of the amount of force needed for appropriate hip joint distraction. The arrow points toward the head of the table.
Hip Arthroscopy Technique
The boundaries of the greater trochanter are marked, as is the anterior superior iliac spine (ASIS), with a line drain distally to denote the “safe zone” to prevent iatrogenic injury to the neurovascular structures of the thigh. First, under fluoroscopic guidance, a 14-gauge spinal needle is placed over the anterior thigh in the trajectory and at the entry point of a standard anterolateral (AL) arthroscopy portal (at the tip and 1 cm medial to the anterior border of the greater trochanter). The modified midanterior (MMA) portal is marked 3 cm distal and medial to the AL portal, and the distal anterolateral accessory portal is marked 4 to 6 cm distal to the AL portal. The AL portal is then created under fluoroscopy, followed by the MMA portal under direct visualization. The portal placement is arthroscopically inspected to confirm that the cannula has not pierced the labrum. Next, an interportal capsulotomy is performed using a Samurai blade (Stryker). The medial boundary of this capsulotomy is just lateral to the psoas tendon. Care is taken to maintain a proximal flap capsule on the acetabular side for repair at the conclusion of the case. The acetabular rim is exposed using an arthroscopic shaver and radiofrequency ablation device, and decortication is performed. The labrum is repaired with suture anchors, and the sutures are shuttled in a trans-labral fashion and by a base refixation technique to avoid excessive eversion of the labrum, which can be detrimental to its suction-seal function. The acetabulum is inspected for chondral defects that may require treatment, and loose bodies are removed. Traction is then released, and the labral suction-seal function is tested and visualized, completing the central-compartment aspect of the hip arthroscopy.
The peripheral-compartment work is now initiated, which begins with the development of a capsular flap on the distal portion of the capsulotomy to release the fascial attachments to the iliocapsularis.2 This is performed to allow better capsule mobility, which aids in visualization for the planned osteoplasty. The hip is then flexed to 45°, and the C-arm x-ray machine image intensifier is tilted 10° to 15° in the caudal direction to provide the surgeon with a modified Dunn lateral view of the hip. Next, 2 retention sutures are placed through the distal anterolateral accessory portal in the lateral capsule to aid with visualization and by retracting the capsule. The femoral osteoplasty is then performed using a 2-tier technique, in which femoral head-neck offset is established first and head sphericity is then restored. This allows a more controlled resection of the cam lesion. The hip is externally rotated in flexion and internally rotated in extension to decompress the medial and lateral sides of the cam lesion, respectively. After completion of the osteoplasty with adequate resection, a dynamic examination is performed to confirm that impingement no longer occurs between the femoral neck and labrum. The capsule is closed using 2 simple suture stitches and tied arthroscopically through the MMA portal. The skin incisions are closed with nylon.
PAO Surgical Technique
Our preferred PAO incision is centered over the ASIS and is linear in nature. The superior aspect of the incision lies about 3 to 5 cm proximal to the ASIS along the iliac crest and runs as an oblique “bikini-line” incision within the inguinal-flexor crease of the hip (Video 1). The inferior aspect of the incision terminates about 3 to 5 cm along the same obliquity angling toward the symphysis pubis (Fig 3). The external oblique aponeurosis is released from the iliac crest, and the iliac fossa is entered bluntly in a subperiosteal fashion. The Hueter interval is opened over the midportion of the tensor fascia lata to protect the lateral femoral cutaneous nerve from iatrogenic injury. An ASIS osteotomy is performed using a small osteotome to take just a wafer of bone to maintain the fascial integrity of the external oblique and flexor fascias, as well as to protect the lateral femoral cutaneous nerve (Table 1). The superior pubic ramus is exposed subperiosteally with the hip in flexion to relax the iliopsoas. This is achieved with ease on the traction table system and reduces table clutter with use of a triangle or sterile bump. Dissection is carried medial to the iliopectineal eminence, and the iliopectineal fascia is released off the inner portion of the quadrilateral plate. A custom, sharp, pointed modified Hohmann retractor is used to expose the superior surface of the superior pubic ramus after identification of the superior border of the obturator foramen to ensure that the osteotomy does not violate the hip joint. Care should be taken not to plunge the osteotome, which could cause injury to the obturator neurovascular structures. The orientation of this osteotomy should be performed so as not to block mobility in the articular osteotomy fragment. The correct orientation of the osteotome has a medial to lateral obliquity so that the lateral portion can slide under the medial portion when unlocking the ramus (Fig 4).
Fig 3.
Incision for periacetabular osteotomy on the patients right. The incision is made along the iliac crest as an oblique bikini-line incision within the inguinal-flexor crease of the hip. The superior aspect of the incision lies roughly 3 to 5 cm proximal to the anterior superior iliac spine (ASIS) and runs in a line angled toward the pubic symphysis. Incisions in the inferior aspect of the image are from a prior hip arthroscopy procedure. The arrow points in the direction of the patient’s head.
Fig 4.
Pelvic models showing correct orientation of superior pubic ramus osteotomy (A) and incorrect orientation (B). The osteotomy should be performed from the superomedial to inferolateral aspect of the superior pubic ramus to allow for free motion of the articular block. The arrows are directed from inferior to superior.
Once the pubic osteotomy is complete, baseline fluoroscopic images are acquired. An anteroposterior (AP) pelvis image is taken and matched to the preoperative weight-bearing AP pelvis radiograph to account for lumbar lordosis. The tilt of the image intensifier is adjusted to match the patients’ pelvic tilt by use of the profiles of the obturator foramina. Baseline AP, obturator oblique, iliac oblique, and false-profile fluoroscopic images are then taken and saved for post-correction image comparison. The interval between the medial femoral neck and iliopsoas tendon is then developed. This is most safely achieved by running the surgeon’s finger first along the origin or the rectus femoris and following this medially around the femoral neck. A pair of curved Mayo dissection scissors is used to bluntly dissect through a thick connective tissue layer leading to the posterior aspect of the femoral neck and ischium. Opening the scissors in this space will dilate the tract and develop an interval between the iliopsoas tendon and the medial femoral neck. With the hip in extension, a small-offset, tined osteotome is carefully placed through this interval. The osteotome is then used to dissect the periosteal and capsular tissue from the anterior ischium so that the osteotome can comfortably rest in the infracotyloid groove. Alternating between iliac oblique and AP fluoroscopic images, the surgeon should then perform an ischial osteotomy in the medial, central, and lateral portions of the ischium (Fig 5). This is an incomplete osteotomy and should only travel about 50% through the ischium to ensure that the final osteotomy will not violate the integrity of the pelvic ring.
Fig 5.
Ischial osteotomy on intraoperative fluoroscopic iliac oblique (A) and anteroposterior (B) views. These images are of the patients left hip. The arrows point in the direction of the patient’s head.
Next, the position of the iliac osteotomy is marked with a metal guidewire parallel to the superior joint surface between the ASIS and anterior inferior iliac spine (Fig 6). A tip-oscillating saw is used to make the initial osteotomy under radiographic fluoroscopy to maintain an orientation perpendicular to the image intensifier. This blade minimizes soft-tissue damage to the musculature lateral to the outer table.3 The saw should be stopped before reaching the pelvic brim to maintain the integrity of the posterior column. The iliac and ischial osteotomies are connected using a curved, tined osteotome along the medial and lateral portions of the posterior column using an iliac oblique view on fluoroscopy (Fig 7).
Fig 6.
Prior to the iliac osteotomy, the osteotomy site is marked with a metal guidewire placed parallel to the superior aspect of the acetabular articular surface to ensure the osteotomy is parallel to the joint; this is confirmed on the iliac oblique fluoroscopic view. The arrow points in the direction of the patient’s head. The image is taken of the patients left hip.
Fig 7.
Intraoperative fluoroscopic iliac oblique images depicting use of curved, tined osteotome to connect ilium and ischium osteotomies. The arrows point in the direction of the patient’s head. These images are taken of the patients left hip.
Then, a threaded 5-mm Schanz pin is placed in the supra-acetabular bone to manipulate the osteotomized fragment. If the fragment is not mobile, it should be evaluated to confirm that it is adequately released at its corners. It should be able to be mobilized in a circular fashion without difficulty. A custom cannulated bone clamp is then used to firmly grasp and manipulate the osteotomy fragment. The pubic ramus is unlocked, the fragment is reoriented, and temporary fixation is performed with 2.8-mm terminally threaded wires (Fig 8A). Post-correction AP, obturator oblique, and/or iliac oblique views are obtained. If correction is appropriate, final internal fixation is performed with four 4.5-mm stainless steel solid screws (Fig 8B). After completion of the correction, the incision is irrigated and inspected for adequate hemostasis. The ASIS osteotomy is then repaired back to the ASIS through a bone tunnel using heavy nonabsorbable suture. A deep drain is placed if needed. Finally, the fascia of the external oblique and tensor fascia lata is repaired, and the dermis and/or epidermis is closed in a layered fashion.
Fig 8.
(A) Once the osteotomy is complete, it is provisionally held in place with 2.8-mm terminally threaded wires. The osteotomy is then fixed with the use of 4.5-mm stainless steel solid screws as seen on anteroposterior (B), obturator oblique (C), and iliac oblique (D) views of the pelvis. The arrows point in the direction of the patient’s head. The photograph in the top images is taken of a patients right hip intra-operatively. These fluoroscopic images are taken of a patients left hip intra-operatively.
Discussion
The prevalence of intra-articular hip pathology such as labral tears and chondral injuries is substantial in patients with dysplastic hips.4 Combined hip arthroscopy and PAO is an established treatment for concomitant intra-articular hip pathology and symptomatic hip dysplasia. Patients who undergo this procedure show improvement in function and pain relief.5 If left untreated, these conditions can cause continued pain and inferior patient outcomes.6 In addition, a known cause of failure after acetabular correction for hip dysplasia is residual or iatrogenic impingement from correction.7 Therefore, a combined procedure for the treatment of symptomatic hip dysplasia and intra-articular pathology (i.e., cam lesion and labral tear) should be performed in a safe and effective manner to help improve patients’ quality of life and minimize any potential complications.
Previously, the combined procedure was performed on 2 tables, with hip arthroscopy performed on a traction table and PAO performed on a flat radiolucent table.1 There is sparse literature on the use of a single table system, with previous techniques described using a fracture table that may not be available at ambulatory surgery centers.8 The single bed system also provides several benefits: less time spent under anesthesia, less risk of potential infection due to re-draping, less risk of accidental epidural catheter removal with patient transfer, less operating room time, and more efficient operating room use (Table 2). To help educate other providers on a safe and effective technique for combined hip arthroscopy and PAO, we present our technique, which can be performed with the addition of a simple post-less traction system to a regular operating room table.
Table 2.
Advantages, Risks, and Limitations
| Advantages |
| The use of a single operative table and a single preparation and drape leads to decreased OR time. |
| Removal of the perineal post decreases the risk of iatrogenic neurologic injury. |
| Our technique yields an overall reduced anesthetic time. |
| The presence of the tensiometer on the leg holder allows for objective measurement of the amount of traction used to limit the amount of traction required to obtain adequate distraction. |
| The combined approach allows for addressing both intra-articular and extra-articular pathology during a single anesthetic event. |
| Risks |
| Traction boots must be appropriately padded and applied; otherwise, the patient may end up with soft-tissue wounds. |
| The traction pad places increased friction on the epidural catheter, which is at risk of displacement during patient positioning. |
| The surgical bed is narrow and short, placing the patient at risk of falling if improperly positioned or secured. |
| Unknown potential complications may occur with our technique. |
| Limitations |
| PAO and hip arthroscopy are very specialized procedures with a steep learning curve, thus requiring the presence of either a single surgeon skilled in both procedures or 2 specialized surgeons. |
| Skilled OR staff is required to assist with manipulation of the leg holder to appropriately adjust leg traction and leg positioning throughout the case. |
| A skilled fluoroscopy technician is necessary to obtain the appropriate fluoroscopic views during the PAO. |
OR, operating room; PAO, periacetabular osteotomy.
Acknowledgment
The authors thank Stryker for its assistance in the production of Video 1, as well as Nicholas Calabrese for his assistance with video editing.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.I. reports research grant support from Arthrex and education support from Rock Medical, outside the submitted work. M.S. is a consultant for Stryker. R.W. is a consultant for Stryker; is a consultant for Advanced Medical, Biocomposites, and Bone Solutions, outside the submitted work; and receives royalties from Innomed, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Step-by-step demonstration of a combined hip arthroscopy with labral repair and femoral acetabular osteochondroplasty with subsequent periacetabular osteotomy performed on a single radiolucent traction table without a perineal post in a patient with femooracetabular impingement in the setting of hip dysplasia of the patient's right hip. Standard arthroscopy portals are created and an interportal arthrotomy is created between the modified midanterior (MMA) portal and the anterolateral (AL) portal. While viewing through the AL portal, the labrum is debrided through the MMA portal and suture anchors are placed through the distal anterolateral accessory (DALA) portal. A capsular retention suture is then placed through the DALA to retract the inferior capsule to obtain better visualization of the femoral neck, and an osteochondroplasty is performed. The retention suture is removed, and the capsule is closed. Once the hip arthroscopy portion is complete, the periacetabular osteotomy is begun on the same operative table. A bikini-line incision is made along the inguinal crease of the hip. The superior pubic ramus cut is made with the use of an osteotome. An interval is created between the medial femoral neck and the iliopsoas tendon to gain access for the ischial osteotomy. Finally, the iliac osteotomy is performed parallel to the roof of the acetabulum and connected to the ischial osteotomy site with the use of a curved, tined osteotome, with care taken to preserve the posterior column. A Schanz pin is then placed in the osteotomized portion of the acetabulum and used to manipulate the free fragment with the assistance of additional manipulation and traction of the lower extremity from the traction table to provide adequate hip joint coverage. Once the dysplasia has been corrected, the periacetabular osteotomy is fixed into place with four solid 4.5-mm stainless steel screws.
References
- 1.Domb B., LaReau J., Redmond J.M. Combined hip arthroscopy and periacetabular osteotomy: Indications, advantages, technique, and complications. Arthrosc Tech. 2014;3:e95–e100. doi: 10.1016/j.eats.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spiker A.M., Turner E.H.G., Gans I., Sisel H.I., Wiseley B.R., Goodspeed D.C. Combined hip arthroscopy and periacetabular osteotomy (PAO): Technical focus on arthroscopically elevating the iliocapsularis and performing the open PAO. Arthrosc Tech. 2021;10:e2293–e2302. doi: 10.1016/j.eats.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wetzel R.J., Shah R.R., Puri L. Demonstration of saw blade accuracy and excursion: A cadaveric comparison study of blade types used in total knee arthroplasty. J Arthroplasty. 2013;28:985–987. doi: 10.1016/j.arth.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Redmond J.M., Gupta A., Stake C.E., Domb B.G. The prevalence of hip labral and chondral lesions identified by method of detection during periacetabular osteotomy: Arthroscopy versus arthrotomy. Arthroscopy. 2014;30:382–388. doi: 10.1016/j.arthro.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Domb B.G., LaReau J.M., Hammarstedt J.E., Gupta A., Stake C.E., Redmond J.M. Concomitant hip arthroscopy and periacetabular osteotomy. Arthroscopy. 2015;31:2199–2206. doi: 10.1016/j.arthro.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Ginnetti J.G., Pelt C.E., Erickson J.A., Van Dine C., Peters C.L. Prevalence and treatment of intraarticular pathology recognized at the time of periacetabular osteotomy for the dysplastic hip. Clin Orthop Relat Res. 2013;471:498–503. doi: 10.1007/s11999-012-2602-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albers C.E., Steppacher S.D., Ganz R., Tannast M., Siebenrock K.A. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614. doi: 10.1007/s11999-013-2799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woyski D., Olson S., Lewis B. Single table concomitant post-less hip arthroscopy combined with periacetabular osteotomy for hip dysplasia. Arthrosc Tech. 2019;8:e1569–e1578. doi: 10.1016/j.eats.2019.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step demonstration of a combined hip arthroscopy with labral repair and femoral acetabular osteochondroplasty with subsequent periacetabular osteotomy performed on a single radiolucent traction table without a perineal post in a patient with femooracetabular impingement in the setting of hip dysplasia of the patient's right hip. Standard arthroscopy portals are created and an interportal arthrotomy is created between the modified midanterior (MMA) portal and the anterolateral (AL) portal. While viewing through the AL portal, the labrum is debrided through the MMA portal and suture anchors are placed through the distal anterolateral accessory (DALA) portal. A capsular retention suture is then placed through the DALA to retract the inferior capsule to obtain better visualization of the femoral neck, and an osteochondroplasty is performed. The retention suture is removed, and the capsule is closed. Once the hip arthroscopy portion is complete, the periacetabular osteotomy is begun on the same operative table. A bikini-line incision is made along the inguinal crease of the hip. The superior pubic ramus cut is made with the use of an osteotome. An interval is created between the medial femoral neck and the iliopsoas tendon to gain access for the ischial osteotomy. Finally, the iliac osteotomy is performed parallel to the roof of the acetabulum and connected to the ischial osteotomy site with the use of a curved, tined osteotome, with care taken to preserve the posterior column. A Schanz pin is then placed in the osteotomized portion of the acetabulum and used to manipulate the free fragment with the assistance of additional manipulation and traction of the lower extremity from the traction table to provide adequate hip joint coverage. Once the dysplasia has been corrected, the periacetabular osteotomy is fixed into place with four solid 4.5-mm stainless steel screws.
Step-by-step demonstration of a combined hip arthroscopy with labral repair and femoral acetabular osteochondroplasty with subsequent periacetabular osteotomy performed on a single radiolucent traction table without a perineal post in a patient with femooracetabular impingement in the setting of hip dysplasia of the patient's right hip. Standard arthroscopy portals are created and an interportal arthrotomy is created between the modified midanterior (MMA) portal and the anterolateral (AL) portal. While viewing through the AL portal, the labrum is debrided through the MMA portal and suture anchors are placed through the distal anterolateral accessory (DALA) portal. A capsular retention suture is then placed through the DALA to retract the inferior capsule to obtain better visualization of the femoral neck, and an osteochondroplasty is performed. The retention suture is removed, and the capsule is closed. Once the hip arthroscopy portion is complete, the periacetabular osteotomy is begun on the same operative table. A bikini-line incision is made along the inguinal crease of the hip. The superior pubic ramus cut is made with the use of an osteotome. An interval is created between the medial femoral neck and the iliopsoas tendon to gain access for the ischial osteotomy. Finally, the iliac osteotomy is performed parallel to the roof of the acetabulum and connected to the ischial osteotomy site with the use of a curved, tined osteotome, with care taken to preserve the posterior column. A Schanz pin is then placed in the osteotomized portion of the acetabulum and used to manipulate the free fragment with the assistance of additional manipulation and traction of the lower extremity from the traction table to provide adequate hip joint coverage. Once the dysplasia has been corrected, the periacetabular osteotomy is fixed into place with four solid 4.5-mm stainless steel screws.