Abstract
The shoulders with critical shoulder angle (CSA) of greater than 33-35° are associated with rotator cuff tears, whereas a CSA of less than 30° is likely to be osteoarthritic. However, anterior acromioplasty or lateral acromioplasty could not reduce high CSAs to the desired range (30-33°), with satisfactory accuracy and efficacy. Thus, we introduce a computer image-guided precise acromioplasty (CIG-PAP) technique, an individualized treatment based on three-dimensional planning. We believe that the introduction of this technique will provide an alternative approach to reduce a large CSA to the desired range (30-33°).
Technique Video
This video demonstrates the preoperative three-dimensional (3-D) planning and the intraoperative procedures of the computer image-guided precise acromioplasty (CIG-PAP) for reducing the critical shoulder angle.
Introduction
The critical shoulder angle (CSA) describes the lateral extension of the acromion in relation to the inclination of the glenoid and has been demonstrated to be an effective predictor for the development of shoulder pathology.1, 2, 3, 4 Numerous studies have documented that shoulders with a CSA of less than 30° were likely to be osteoarthritic, whereas a CSA of greater than 33-35° was associated with rotator cuff tears (RCTs).5, 6, 7, 8, 9, 10 Gerber et al. demonstrated that patients with a CSA reduced to 33° or less had superior abduction strength and lower retear rate after arthroscopic rotator cuff repair (RCR).11 Therefore, accurately reducing the large CSA to the desired range (30-33°) seems to become one of the important goals in the clinical treatment of RCTs.
Several studies have shown that anterior acromioplasty reduced the CSA by a mean of 1-3.2°.12, 13, 14, 15 In comparison, lateral acromioplasty could significantly decrease the CSA by a mean of 3.6-6.5°.11,16,17 However, whether anterior or lateral, 20-52% of patients still had postoperative CSA > 35° after acromioplasty, while CSA were over-reduced to below 30° in some cases.11, 12, 13, 14,16, 17, 18, 19 Currently, avoiding insufficient or over-reduction of the CSA is still a challenging problem.
In this article, we present a computer image-guided precise acromioplasty (CIG-PAP) technique, which is an individualized treatment based on three-dimensional (3-D) planning to reduce a large CSA to the desired range (30-33°). CIG-PAP is especially indicated for patients with RCTs combined with preoperative CSA greater than 35°. We hope that using this technique concomitant to arthroscopic RCR would provide clinical benefits to patients. Conversely, contraindication for CIG-PAP would include the following: irreparable RCTs, inflammatory arthritis, and concomitant fracture or dislocation of the shoulder.
Surgical Technique (With Video Illustration)
3-D Reconstruction and Coordinate System Establishment
Digital Imaging and Communications in Medicine (DICOM) data of shoulder are obtained. Three-dimensional reconstruction is made using Mimics 20.0 (Materialise, Leuven, Belgium). Subsequently, 3-D shoulder model is imported into Blender 2.81 (Amsterdam, Netherlands) to establish a Cartesian coordinate system for position alignment, according to previous studies.20,21
Preoperative Planning and Measurement
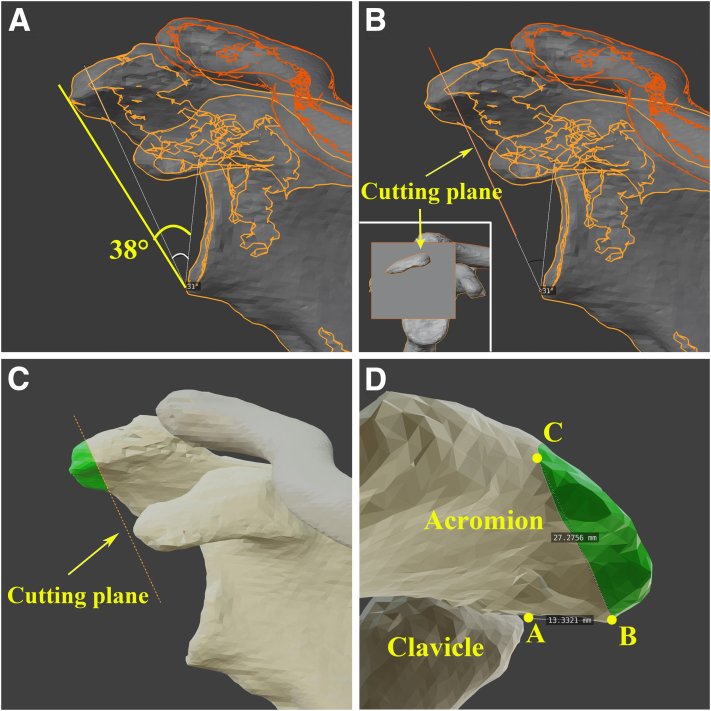
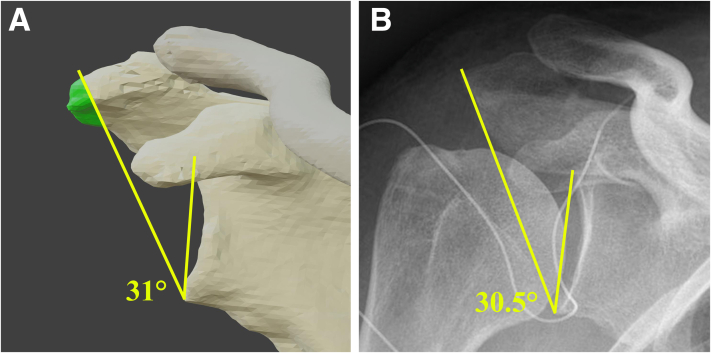
Preoperative planning is performed on 3-D shoulder model using Blender 2.81. First, preoperative CSA is measured on the standard anterior view to confirm the value of CSA greater than 35° (38° in this article). The CSA is measured between a line connecting the superior and inferior borders of the glenoid and another line from the inferior borders of the glenoid to the most inferolateral point of the acromion.1 And then, the postoperative target CSA is set at 31°, which is in the middle of the desired range of 30-33° (Fig 1A). Next, a cutting plane is established and positioned at the measuring line of 31° (Fig 1B). Hence, the external acromion of the cutting plane (green region) is the part of the bone to be removed (Fig 1C). Lastly, the resected bone borders are identified and measured on the computer, including the anterior acromial edge of acromioclavicular joint (Point A), anteromedial resection margin (Point B), posterolateral resection margin (Point C), and the distance of AB (approximately 13 mm) and BC (approximately 27 mm) (Fig 1D).
Fig 1.
Demonstration of preoperative planning and measurement (right shoulder). (A) Preoperative CSA (yellow line, 38°) is measured on the standard anterior view of 3-D shoulder. And the postoperative target CSA is set at 31° (white line). (B) The cutting plane is created and positioned at the measuring line of 31°. (C) The green region outside the cutting plane is the part of the acromion to be resected. (D) The measurement of resected bone borders, including the distance of AB (approximately 13 mm) and BC (approximately 27 mm). “A” denotes anterior acromial edge of acromioclavicular joint, “B” denotes anteromedial resection margin, and “C” denotes posterolateral resection margin; CSA, critical shoulder angle.
Arthroscopic CIG-PAP
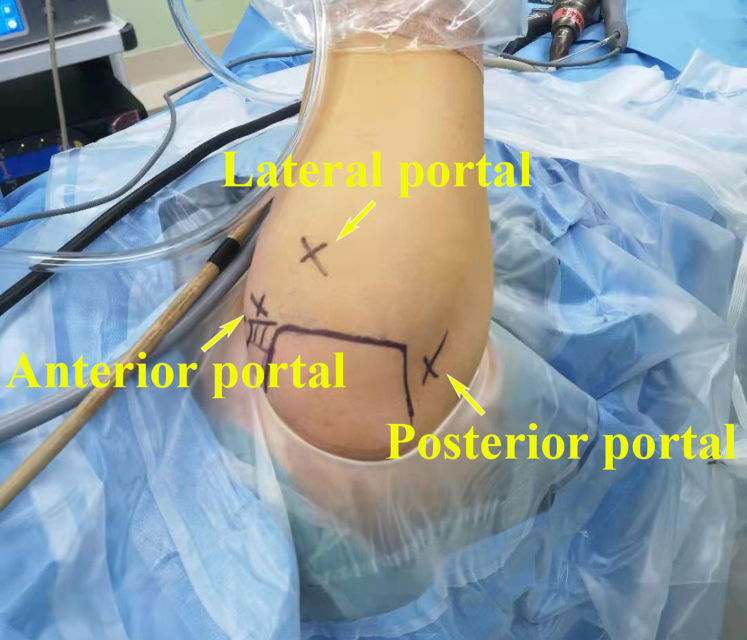
After general anesthesia combined with brachial plexus block, the patient is placed in the lateral decubitus position with the arm in 30° abduction and with 10 pounds of traction. The bony landmarks are identified and marked, together with anterior, posterior, and lateral portals (Fig 2).
Fig 2.
The patient is placed in the lateral decubitus position with continuous extremity traction (right shoulder). The bony landmarks are outlined, and the anterior, posterior, and lateral portals are marked.
After the posterior and anterior portals are created, a routine diagnostic arthroscopy is performed in the articular cavity. Any intra-articular pathology is assessed and addressed appropriately if necessary, including articular cartilage, glenoid labrum, glenohumeral ligament, biceps, and subscapularis.
The 30° arthroscope is then inserted into the subacromial space, and a lateral portal is established to assess the reparability of the RCT based on tear location, size, degree of retraction, tension, tissue quality, and other variables. Once the RCT is determined to be reparable, the following procedures will be performed.
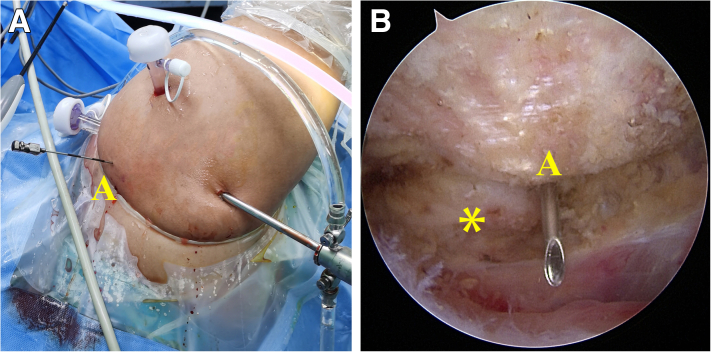
First, all soft tissue undersurface of the acromion and acromioclavicular joint is cleaned using radiofrequency electrocautery (Arthrex, Naples, FL). After fully revealing the acromioclavicular joint, anterior and lateral borders of the acromion, the anterior acromial edge of acromioclavicular joint (point A) is identified and marked with a spinal needle (Fig 3; Video 1).
Fig 3.
Identifying and marking the point A with a spinal needle (right shoulder in lateral decubitus position). (A) Gross view after inserting the spinal needle. (B) Arthroscopic view using 30° arthroscope from the posterior portal. A denotes anterior acromial edge of acromioclavicular joint. The asterisk (∗) denotes the clavicle.
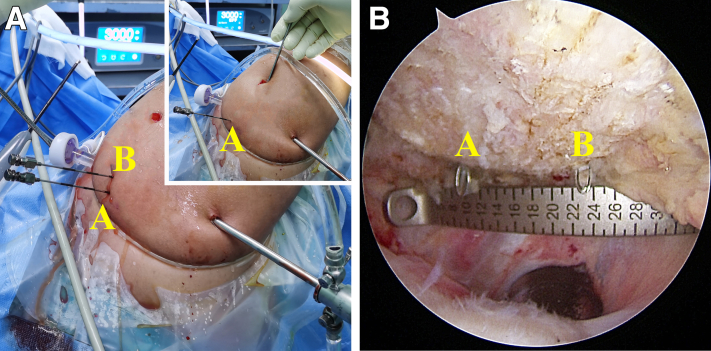
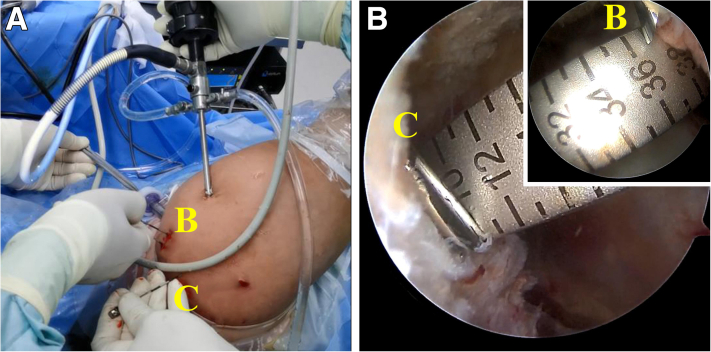
Second, the posterior portal is used as the viewing portal, and the lateral portal is used as the working portal for measurement. According to the preoperative planning, the anteromedial resection margin (point B) is identified by measuring the distance of AB (approximately 13 mm in this article), and marked with a spinal needle (Fig 4; Video 1).
Fig 4.
Marking the point B with a spinal needle by measuring the distance of AB on the undersurface of the acromion (right shoulder in lateral decubitus position). (A) Gross view of the measurement and marking. (B) Arthroscopic view using 30° arthroscope from the posterior portal, and measuring the distance of AB from the lateral portal (scale from 10 mm to 23 mm, ∼13 mm). A denotes the anterior acromial edge of acromioclavicular joint; B denotes the anteromedial resection margin.
Third, the lateral portal is used as the viewing portal, and the anterior portal is used as the working portal for measurement. The posterolateral resection margin (point C) is identified by measuring the distance of BC (approximately 27 mm in this article), and also marked with a spinal needle (Fig 5; Video 1).
Fig 5.
Marking the point C with a spinal needle by measuring the distance of BC on the undersurface of the acromion (right shoulder in lateral decubitus position). (A) Gross view of the measurement and marking. (B) Arthroscopic view using 30° arthroscope from the lateral portal, and measuring the distance of BC from anterior portal (scale from 10 mm to 37 mm, ∼27 mm). B denotes the anteromedial resection margin; C denotes the posterolateral resection margin.
Then, a 0# PDS® (polydioxanone) suture (Ethicon, Somerville, NJ) is introduced under arthroscopy from point B to C through the inner core of the straight needles, and the blue resection line (BC) is made (Video 1).
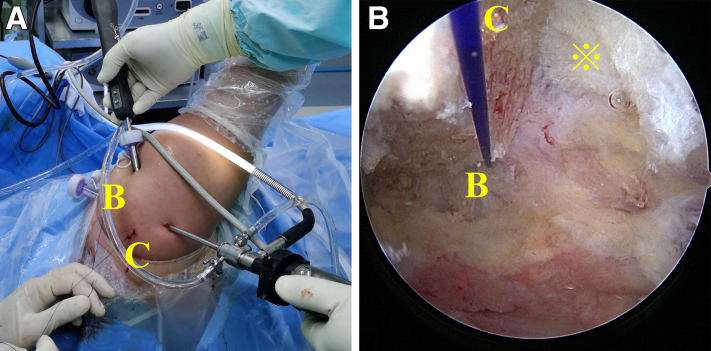
Next, the region of the acromion outside the blue resection line is gradually resected by a 5.5-mm shaver burr (Arthrex) via the lateral portal (Fig 6; Video 1). Finally, the cutting surface of the acromion is deactivated using radiofrequency electrocautery (Arthrex).
Fig 6.
Removing the acromial bone outside the resection line BC (right shoulder in lateral decubitus position). (A) Gross view after marking the resection line BC with a 0# PDS® (polydioxanone) suture (Ethicon, Somerville, NJ). (B) Arthroscopic view using 30° arthroscope from the posterior portal, and working from the lateral portal. B denotes the anteromedial resection margin; C denotes the posterolateral resection margin; ※ symbol denotes the deltoid fascia.
Arthroscopic RCR is then performed depending on the tear location and size. Standard anteroposterior (AP) radiograph (type A1 or C1 according to the Suter-Henninger classification20) (Fig 7) or CT scans of the shoulder is taken 3-5 days postoperation to assess the post-operative CSA.
Fig 7.
The pre-operative three-dimensional planning and postoperative measurement for CSA (right shoulder). (A) Target CSA of preoperative planning is set at 31°. (B) Postoperative CSA measured on the standard anteroposterior radiograph is 30.5°. CSA, critical shoulder angle.
Postoperative Management
As the CIG-PAP is concomitant with arthroscopic RCR, the patient should follow the rehabilitation protocol of RCR. The upper limb is placed into a shoulder and elbow brace for immobilization immediately after the operation. Active activity of the elbow and wrist should be started on the second day postoperatively. Passive or active-assisted shoulder range-of-motion exercises should begin 1-2 weeks after the operation. Active shoulder motion should be started after 8 weeks and gradually strengthened and reintegrated into normal activities at 12 weeks postoperatively.
Discussion
Since the reduction of CSA is difficult to predict intraoperatively, the favorable range of postoperative CSA is not always achieved after acromioplasty. Olmos et al. suggested using the approximation of “1 degree of CSA reduction for each 1 mm of resection” to quantify the amount of acromion to be resected by lateral acromioplasty; however, they found that 46.3% of patients still had a postoperative CSA > 35°.17 Similarly, to calculate the amount of acromion resection for reducing the CSA, Franceschetti et al. developed a formula by measuring the parameters on the AP radiographs.22 Although they reported using the complex formula could reduce the large CSAs to the range of 30-35°, how to accurately apply the preoperative planning to arthroscopic acromioplasty needs to be further clarified.22
The CIG-PAP provides a new potential strategy for accurate reduction of CSA without insufficient or over-resection of the acromion (Table 1). This all-arthroscopic personalized acromioplasty is concomitant with arthroscopic RCR. And it is recommended to perform this technique first to increase space for visualization and suture passage during RCR (Table 2). The most difficult manipulation of this technique is how to accurately locate the area of osteotomy during arthroscopy, according to the 3-D planning.
Table 1.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
|
|
|
|
|
|
|
CSA, critical shoulder angle; CT, computed tomography; 3-D, three dimensional.
Table 2.
Tips and Tricks
|
|
|
|
|
|
CIG-PAP, computer image-guided precise acromioplasty; RCR, rotator cuff repair.
In the early stage, we measured the resected bone borders on the patient’s skin after the bony landmarks were marked.23 This method was satisfactory for some thin patients. However, it was inaccurate for the patients with unclear bony landmarks. Moreover, the body surface marker points would shift after the shoulder was filled with water during the operation.
This article modified the procedure to locate the area of osteotomy with greater accuracy. We selected the anterior edge of the acromioclavicular joint (point A) as an initial marker point, because it was relatively stable and easy to identify under arthroscopy. And we directly measured and marked the resected bone border under the arthroscopy instead of marking it on the body skin. We hope these improvements would reduce the CSA with greater consistency between preoperative 3-D planning and intraoperative osteotomy. Our preliminary cohort results are promising.
The main disadvantage of this technique is that preoperative 3-D planning is necessary. Therefore, there are inevitable learning curves for the 3-D planning tools described in this article. However, any other similar application software can be chosen depending on the operator’s proficiency and preference. In fact, many other 3-D planning tools described in the literature can also realize the process.24, 25, 26 Maybe an automatic 3-D planning program will simplify the procedure in the future.
In general, the CIG-PAP provides a new individualized treatment for accurate correction of CSA. Further research and clinical trials need to be carried out to evaluate the clinical benefits.
Footnotes
This study was supported by the Fundamental Research Funds for the Central Universities, Sun Yat-sen University (no. 2020004). Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates the preoperative three-dimensional (3-D) planning and the intraoperative procedures of the computer image-guided precise acromioplasty (CIG-PAP) for reducing the critical shoulder angle.
References
- 1.Moor B.K., Bouaicha S., Rothenfluh D.A., Sukthankar A., Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint?: A radiological study of the critical shoulder angle. Bone Joint J. 2013:935–941. doi: 10.1302/0301-620X.95B7.31028. 95-B. [DOI] [PubMed] [Google Scholar]
- 2.Incesoy M.A., Yildiz K.I., Turk O.I., et al. The critical shoulder angle, the acromial index, the glenoid version angle and the acromial angulation are associated with rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2020;29:2257–2263. doi: 10.1007/s00167-020-06145-8. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham G., Cocor C., Smith M.M., Young A.A., Cass B., Moor B.K. Implication of bone morphology in degenerative rotator cuff lesions: A prospective comparative study between greater tuberosity angle and critical shoulder angle. Orthop Traumatol Surg Res. 2022;108:103046. doi: 10.1016/j.otsr.2021.103046. [DOI] [PubMed] [Google Scholar]
- 4.Lin C.L., Chen Y.W., Lin L.F., Chen C.P., Liou T.H., Huang S.W. Accuracy of the critical shoulder angle for predicting rotator cuff tears in patients with nontraumatic shoulder pain. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120918995. 2325967120918995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang Y., Hou J., Li Q., et al. The Effectiveness of using the critical shoulder angle and acromion index for predicting rotator cuff tears: Accurate diagnosis based on standard and nonstandard anteroposterior radiographs. Arthroscopy. 2019;35:2553–2561. doi: 10.1016/j.arthro.2019.03.050. [DOI] [PubMed] [Google Scholar]
- 6.Smith G.C.S., Liu V. High Critical shoulder angle values are associated with full-thickness posterosuperior cuff tears and low values with primary glenohumeral osteoarthritis. Arthroscopy. 2022;38:709–715. doi: 10.1016/j.arthro.2021.08.007. e701. [DOI] [PubMed] [Google Scholar]
- 7.Mantell M.T., Nelson R., Lowe J.T., Endrizzi D.P., Jawa A. Critical shoulder angle is associated with full-thickness rotator cuff tears in patients with glenohumeral osteoarthritis. J Shoulder Elbow Surg. 2017;26:e376–e381. doi: 10.1016/j.jse.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 8.Razmjou H., Palinkas V., Christakis M., Robarts S., Kennedy D. Reduced acromiohumeral distance and increased critical shoulder angle: implications for primary care clinicians. Phys Sportsmed. 2020;48:312–319. doi: 10.1080/00913847.2019.1703475. [DOI] [PubMed] [Google Scholar]
- 9.Hohmann E., Shea K., Scheiderer B., Millett P., Imhoff A. Indications for arthroscopic subacromial decompression. A level V evidence clinical guideline. Arthroscopy. 2020;36:913–922. doi: 10.1016/j.arthro.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 10.Tunali O., Ersen A., Kizilkurt T., Bayram S., Sivacioglu S., Atalar A.C. Are critical shoulder angle and acromion index correlated to the size of a rotator cuff tear. Orthop Traumatol Surg Res. 2022;108:103122. doi: 10.1016/j.otsr.2021.103122. [DOI] [PubMed] [Google Scholar]
- 11.Gerber C., Catanzaro S., Betz M., Ernstbrunner L. Arthroscopic correction of the critical shoulder angle through lateral acromioplasty: A safe adjunct to rotator cuff repair. Arthroscopy. 2018;34:771–780. doi: 10.1016/j.arthro.2017.08.255. [DOI] [PubMed] [Google Scholar]
- 12.Katthagen J.C., Marchetti D.C., Tahal D.S., Turnbull T.L., Millett P.J. The effects of arthroscopic lateral acromioplasty on the critical shoulder angle and the anterolateral deltoid origin: An anatomic cadaveric study. Arthroscopy. 2016;32:569–575. doi: 10.1016/j.arthro.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 13.Billaud A., Cruz-Ferreira E., Pesquer L., Abadie P., Carlier Y., Flurin P.H. Does the critical shoulder angle decrease after anterior acromioplasty? Arch Orthop Trauma Surg. 2019;139:1125–1132. doi: 10.1007/s00402-019-03163-1. [DOI] [PubMed] [Google Scholar]
- 14.Girard M., Colombi R., Azoulay V., et al. Does anterior acromioplasty reduce critical shoulder angle? Orthop Traumatol Surg Res. 2020;106:1101–1106. doi: 10.1016/j.otsr.2020.04.013. [DOI] [PubMed] [Google Scholar]
- 15.MacLean I.S., Gowd A.K., Waterman B.R., et al. The effect of acromioplasty on the critical shoulder angle and acromial index. Arthroscopy. 2020;2:e623–e628. doi: 10.1016/j.asmr.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Altintas B., Kääb M., Greiner S. Arthroscopic lateral acromion resection (ALAR) optimizes rotator cuff tear relevant scapula parameters. Arch Orthop Trauma Surg. 2016;136:799–804. doi: 10.1007/s00402-016-2431-y. [DOI] [PubMed] [Google Scholar]
- 17.Olmos M.I., Boutsiadis A., Swan J., et al. Lateral acromioplasty cannot sufficiently reduce the critical shoulder angle if preoperatively measured over 40 degrees. Knee Surg Sports Traumatol Arthrosc. 2021;29:240–249. doi: 10.1007/s00167-020-05951-4. [DOI] [PubMed] [Google Scholar]
- 18.Gurpinar T., Polat B., Carkci E., Eren M., Polat A.E., Ozturkmen Y. The effect of critical shoulder angle on clinical scores and retear risk after rotator cuff tendon repair at short-term follow up. Sci Rep. 2019;9:12315. doi: 10.1038/s41598-019-48644-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardy V., Rony L., Bachler J., Favard L., Hubert L. Does anterior arthroscopic acromioplasty modify critical shoulder angle? Orthop Traumatol Surg Res. 2021;107:102936. doi: 10.1016/j.otsr.2021.102936. [DOI] [PubMed] [Google Scholar]
- 20.Suter T., Gerber Popp A., et al. The influence of radiographic viewing perspective and demographics on the critical shoulder angle. J Shoulder Elbow Surg. 2015;24:e149–158. doi: 10.1016/j.jse.2014.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suter T., Henninger H.B., Zhang Y., Wylie J.D., Tashjian R.Z. Comparison of measurements of the glenopolar angle in 3D CT reconstructions of the scapula and 2D plain radiographic views. Bone Joint J. 2016:1510–1516. doi: 10.1302/0301-620X.98B11.37800. 98-B. [DOI] [PubMed] [Google Scholar]
- 22.Franceschetti E., Giovannetti de Sanctis E., Palumbo A., et al. Lateral acromioplasty has a positive impact on rotator cuff repair in patients with a critical shoulder angle greater than 35 degrees. J Clin Med. 2020;9:3950. doi: 10.3390/jcm9123950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Long Y., Hou J., Tang Y., et al. Effect of arthroscopic acromioplasty on reducing critical shoulder angle: A protocol for a prospective randomized clinical trial. BMC Musculoskelet Disord. 2020;21:819. doi: 10.1186/s12891-020-03818-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghafurian S., Galdi B., Bastian S., Tan V., Li K. Computerized 3D morphological analysis of glenoid orientation. J Orthop Res. 2016;34:692–698. doi: 10.1002/jor.23053. [DOI] [PubMed] [Google Scholar]
- 25.Beeler S., Hasler A., Gotschi T., Meyer D.C., Gerber C. Different acromial roof morphology in concentric and eccentric osteoarthritis of the shoulder: A multiplane reconstruction analysis of 105 shoulder computed tomography scans. J Shoulder Elbow Surg. 2018;27:e357–e366. doi: 10.1016/j.jse.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 26.Billaud A., Lacroix P.M., Carlier Y., Pesquer L. How much acromial bone should be removed to decrease the critical shoulder angle? A 3D CT acromioplasty planning study. Arch Orthop Trauma Surg. 2022 doi: 10.1007/s00402-021-04292-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the preoperative three-dimensional (3-D) planning and the intraoperative procedures of the computer image-guided precise acromioplasty (CIG-PAP) for reducing the critical shoulder angle.
This video demonstrates the preoperative three-dimensional (3-D) planning and the intraoperative procedures of the computer image-guided precise acromioplasty (CIG-PAP) for reducing the critical shoulder angle.