Abstract
Diabetic myonecrosis is a rare complication of poorly controlled diabetes mellitus which commonly affects the thigh and is managed conservatively. Spontaneous ischemic necrosis of muscle is noted without a reduction in vascular supply. Pyomyositis caused by Staphylococcus aureus infection is another rare complication. Atypical presentation of myonecrosis and pyomyositis can occur in the form of simultaneous or sequential involvement of multiple muscle groups. We present a rare case of myonecrosis with pyomyositis in a 39-year-old male patient with a background of type 2 diabetes mellitus who presented with a 5-day history of worsening pain of the right thigh radiating to the right ankle, associated with groin swelling and fever. It is important for clinicians to have a low threshold of suspicion of this rare condition due to the other diverse and similar diagnoses, as well as to prevent further complications and morbidity.
Keywords: Diabetes mellitus, Myonecrosis, Pyomyositis, Complications, Type 2
Introduction
Diabetes mellitus has a prevalence of 7% in the United Kingdom with type 2 diabetes accounting for 90% of them [1]. Acute or chronic complications are common for uncontrolled diabetes. Diabetic myonecrosis and pyomyositis are rare complications for which patients may present with atraumatic painful swollen limb, mostly affecting the thigh. Simultaneous and multiple involvement of muscle groups and sites is uncommon. We present an unusual case of diabetic myonecrosis with pyomyositis in a young male who was misdiagnosed initially as cellulitis.
Case report
A 39-year-old male attended a district general hospital with a 5-day history of worsening pain of the right thigh radiating to the right ankle without preceding trauma, associated with groin swelling and fever. His medical history included type 2 diabetes and hypertension. He was tachycardic with a normal blood pressure and pyrexic on admission. Atrial fibrillation was noted on electrocardiogram. The right lower limb was grossly swollen on examination, with tender lymph nodes in the right groin and erythema limited to the leg. Neurovascular status of lower limbs was intact bilaterally. No obvious skin ulcers or injury was found.
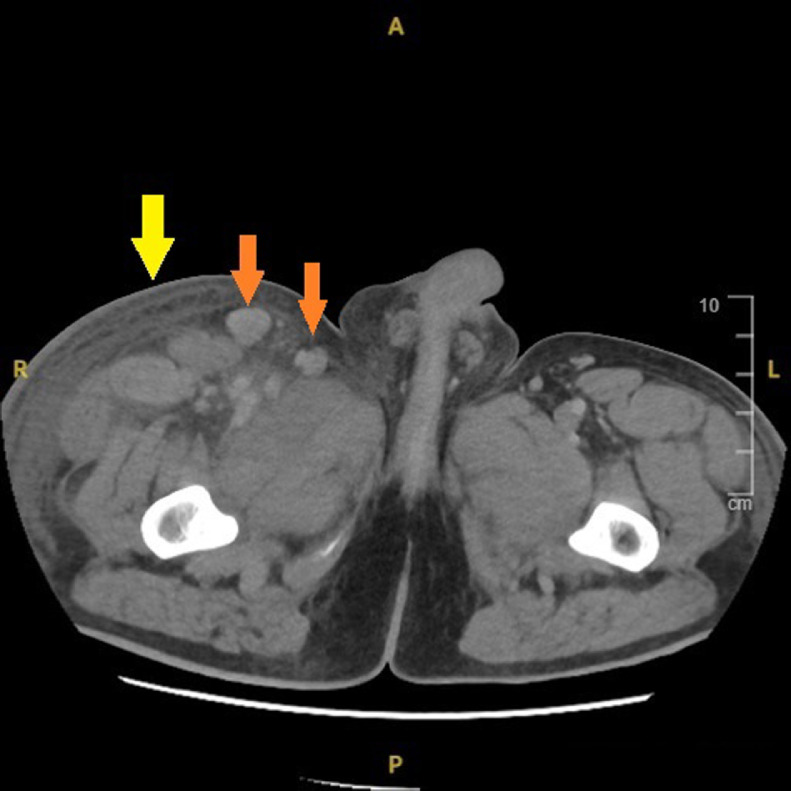
Initial hematology and biochemistry results revealed a normal leucocyte count of 9.5 × 109/L (normal range, 4.5-11 × 109/L), an elevated C-reactive protein of 595 (normal range, 0-5) and D-dimer of 604 (normal range, <243). Computerized tomography (CT) angiography of the lower limbs was performed. It showed no evidence of acute limb ischemia but right-sided subcutaneous edema with lymphadenopathy in the inguinal, external iliac and obturator regions and stranding around the inferior vena cava, suggesting cellulitis (Figs. 1 and 2). He was initially managed with antibiotics covering cellulitis. Ultrasonography of the right leg was later performed which excluded deep vein thrombosis.
Fig. 1.
Coronal section of CT abdomen and pelvis showing subcutaneous edema throughout the abdomen and extending into the right upper thigh deep fascia (yellow arrow) with multiple enhancing right inguinal lymph nodes (red arrow).
Fig. 2.
Transverse section of CT abdomen and pelvis showing subcutaneous edema of the right upper thigh deep fascia (yellow arrow) with multiple enhancing right inguinal lymph nodes (red arrows).
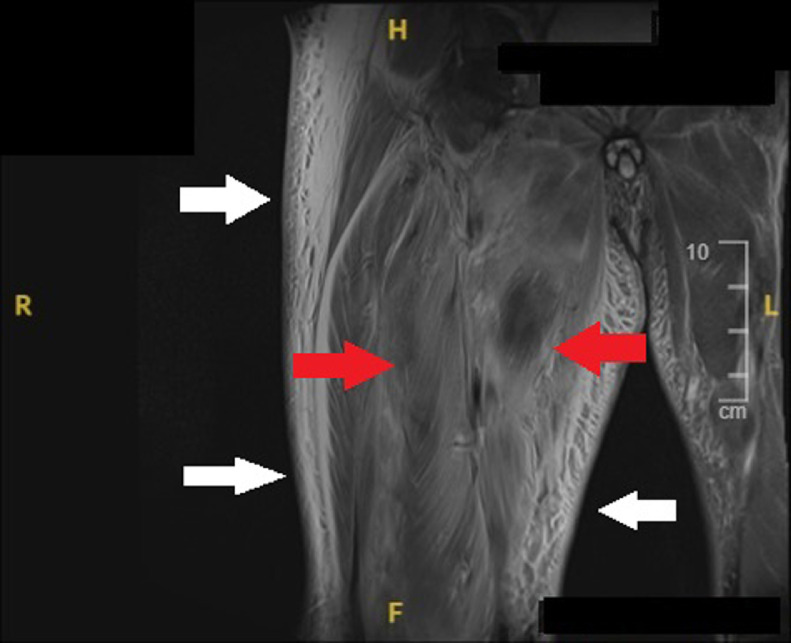
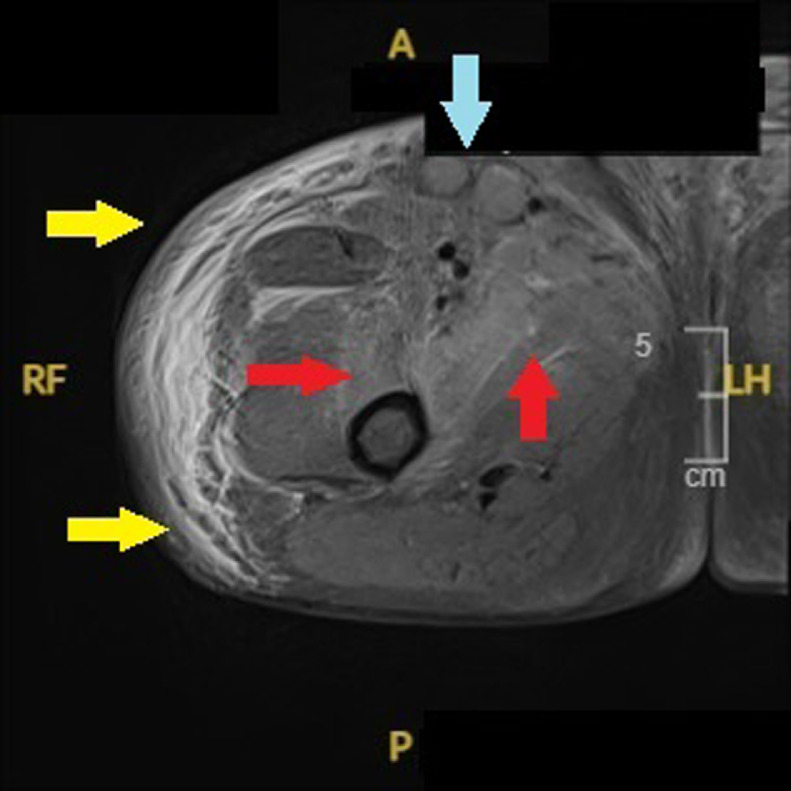
He continued to deteriorate clinically despite a change in antibiotics with worsening blood results and pain. CT abdomen and pelvis was subsequently performed which found no source of intraabdominal infection or gas gangrene (Figs. 1 and 2). No clinical improvement was made after Day 4 from admission, MRI was then performed to rule out pyomyositis due to raised Creatine Kinase of 1407 (normal range, 40-320). It showed extensive signal abnormality affecting the swollen musculature of the right adductor compartment, as well as the muscle fibers of the rectus femoris and both the vastus medialis and intermedius which was consistent with diabetic myonecrosis and pyomyositis (Figs. 3 and 4). He made an uneventful recovery with tight glycemic control, analgesics optimization, and targeted antibiotics.
Fig. 3.
Coronal section of MRI showing extensive and pronounced edema-like signal abnormality (yellow arrows) throughout the subcutaneous fat of the right thigh, groin, scrotum, and extensive signal abnormality affecting the swollen musculature of the right adductors, rectus femoris and vastus muscles (red arrows), consistent with pyomyositis and diabetic myonecrosis.
Fig. 4.
Transverse section of MRI showing extensive and pronounced edema-like signal abnormality (yellow arrows) throughout the subcutaneous fat of the right thigh, groin, scrotum, and extensive signal abnormality affecting the swollen musculature of the right adductors, rectus femoris and vastus muscles (red arrows)with bulky right inguinal lymphadenopathy (green arrow), consistent with pyomyositis and diabetic myonecrosis.
Discussion
Diabetic myonecrosis is a rare complication for patients with poor chronic glycemic control [2]. Other diabetic complications such as neuropathy, retinopathy, and nephropathy are often seen along with myonecrosis. Patients usually experience an acute onset of pain of the limb with edema and tenderness due to muscle ischemia and necrosis, although delay presentation may also be noted [3]. Diagnosis can be made by magnetic resonance imaging (MRI), absence in enhancement in the muscle following intravenous contrast is pathognomonic [4]. Non-contrast MRI may show edema of the muscle compartment on T2 and short tau inversion recovery images. Features such as the absence of a typical anechoic center in a typical abscess, hyperechoic lines within muscle fibers and lack of fluid-like motion when pressure applied may help differentiating between diabetic myonecrosis and abscess with the use of ultrasound [5]. Muscle biopsy may be performed if investigations are inconclusive. Good prognosis and recovery in weeks are seen in diabetic myonecrosis and patients are managed with muscle rest, optimization in glycemic level and pain control [6].
Skeletal muscle is resistant to bacterial infection due to its sequestration of iron by myoglobin [7]. However, opportunistic infection and sepsis are common for immunocompromised patients including uncontrolled diabetes. Pyomyositis is another rare complication of DM and makes timely diagnosis challenging. Initial stage includes local symptoms and fever, when left untreated, it can progress into abscess formation with worsening symptoms. Delay in the diagnosis and management can result in severe sepsis with organ failure and shock at a late stage. MRI is the imaging modality of choice to accurate assess the extent of muscle involvement [8]. Muscle edema is typically present on T2 signal. Management should be directed by the stage of the disease with targeted antibiotics and drainage of abscess if required. Side effects and risks of prolonged antibiotics use should also be monitored.
Due to the rarity of the complications above, other, more common diagnoses should be initially considered. In this case, the patient was initially mismanaged, and treated as cellulitis. A wide range of differentials may also include osteomyelitis, septic arthritis, appendicitis, diverticulitis, hematoma, and muscle rupture. Life-threatening pathology such as necrotizing fasciitis may share some of the findings of myonecrosis, but often presents with localized pain out of proportion to examination findings [8]. Imaging is an essential tool in the differentiation between different diagnosis. Ultrasonography is readily accessible and able to show presence of abscess or effusion. Other cross-sectional imaging studies such as CT and MRI provide anatomic details and give a more definitive diagnosis. Delay in the diagnosis and management can lead to muscle fibrosis and functional disability [9].
Conclusion
Pyomyositis and myonecrosis are rare complications of uncontrolled diabetes. Appropriate and prompt use of imaging is essential in the evaluation of patients with local pain and swelling, associated with infection. Muscle biopsy may be considered for inconclusive cases. Good prognosis and recovery are seen in the patients after muscle rest, optimization in glycemic level and pain control, and targeted antibiotics for pyomyositis.
Patient consent
Written, informed consent for publication of case was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Diabetes UK - Know diabetes. Fight diabetes. | Diabetes UK [Internet]. Diabetes.org.uk. 2022 [cited 15 October 2022]. Available from: http://www.diabetes.org.uk/
- 2.Mukherjee S, Aggarwal A, Rastogi A, Bhansali A, Prakash M, Vaiphei K, et al. Spontaneous diabetic myonecrosis: report of four cases from a tertiary care institute. Endocrinol Diabetes Metab Case Rep. 2015;2015 doi: 10.1530/EDM-15-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trujillo-Santos A. Diabetic muscle infarction. Diabetes Care. 2003;26(1):211–215. doi: 10.2337/diacare.26.1.211. [DOI] [PubMed] [Google Scholar]
- 4.Naidoo P, Liu V, Mautone M, Bergin S. Lower limb complications of diabetes mellitus: a comprehensive review with clinicopathological insights from a dedicated high-risk diabetic foot multidisciplinary team. Br J Radiol. 2015;88(1053) doi: 10.1259/bjr.20150135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delaney-Sathy LO, Fessell DP, Jacobson JA, Hayes CW. Sonography of diabetic muscle infarction with MR imaging, CT, and pathologic correlation. Am J Roentgenol. 2000;174(1):165–169. doi: 10.2214/ajr.174.1.1740165. [DOI] [PubMed] [Google Scholar]
- 6.Kapur S, McKendry R. Treatment and outcomes of diabetic muscle infarction. JCR J Clin Rheumatol. 2005;11(1):8–12. doi: 10.1097/01.rhu.0000152142.33358.f1. [DOI] [PubMed] [Google Scholar]
- 7.Skaar E. The battle for iron between bacterial pathogens and their vertebrate hosts. PLoS Pathogens. 2010;6(8) doi: 10.1371/journal.ppat.1000949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wasserman P, Way A, Baig S, Gopireddy D. MRI of myositis and other urgent muscle-related disorders. Emerg Radiol. 2020;28(2):409–421. doi: 10.1007/s10140-020-01866-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pasternack M, Swartz M. Myositis and myonecrosis. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Elsevier Public Health Emergency Collection 2015;1:1216-1225.e2.