Abstract
Patellar tendon grafts have long been considered the gold standard for anterior cruciate ligament reconstruction (ACLR). This Technical Note describes ACLR using bone-patella tendon-bone (BPTB) autograft with press-fit femoral fixation using an outside-in drilling technique.
Technique Video
This technical note describes the original technique which is an anterior cruciate ligament reconstruction using bone-patella tendon-bone autograft with press-fit femoral fixation using an outside-in drilling technique.
Introduction
Anterior cruciate ligament reconstruction (ACLR) has evolved over recent decades.1 Historically, bone-patella tendon-bone (BPTB) autograft was considered the gold standard for ACLR, as it allowed bone-to-bone tunnel healing, providing excellent biomechanical strength.2 However, BPTB autografts are frequently associated with donor site morbidity, including anterior knee pain, pain when kneeling, and extensor mechanism complications, such as patella fractures and patellar tendon ruptures.3 This has led to hamstring autografts gaining increasing popularity.4
Additionally, debate still exists regarding the different femoral tunnel drilling techniques. Femoral guides have been developed that enable the femoral tunnel to be drilled from outside to inside under arthroscopic control. This aims to reproduce the anterior portion of the ACL, namely, the anteromedial bundle. This establishes a favorable nonisometry, relaxed in flexion and tight in extension, which addresses the parameters in which the ACL-deficient knee produces greatest instability.1,5
Surgical Technique
This technical note describes an arthroscopic reconstruction of the ACL using BPTB autograft with outside-in drilling and press-fit femoral fixation (Video 1). Pearls and pitfalls plus advantages and disadvantages are described in Tables 1 and 2.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
|
|
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
Patient Positioning and Landmarks
The patient is placed in the supine position on the operating table with a lateral support at the level of a padded tourniquet and a foot roll positioned to stabilize the leg at 90° of knee flexion. The injured leg is prepared and draped using the surgeons preferred method, and then appropriate landmarks are palpated and marked (Fig 1).
Fig 1.

Patient positioning and landmarks. Right knee, frontal view. Positioned at 90° of knee flexion. Appropriate landmarks are palpated and marked. P, patella; PT, patellar tendon; TT, tibial tuberosity.
Graft Harvest
Traditionally, a single incision extending from the inferior pole of the patella to the tibial tuberosity is performed. However, this technique has evolved, and we now use two incisions to reduce the risk of damage to the infrapatellar branch of the saphenous nerve. The first incision extends proximally from the distal pole of the patella, as the key step is harvesting the patella bone block. The second incision is located more medially at the level of the tibial tuberosity. This incision has several advantages, including being enable to drill the tibial tunnel through the same incision, incorporating previous hamstring harvesting incisions in revision cases and similarly being able to use the incision if future revision surgery is required using hamstring autograft (Fig 2).
Fig 2.

Incisions for graft harvest. Right knee, frontal view. The first incision extends proximally from the distal pole of the patella. The second incision is located more medially at the level of the tibial tubercule. P, patella; PT, patellar tendon; TT, tibial tuberosity.
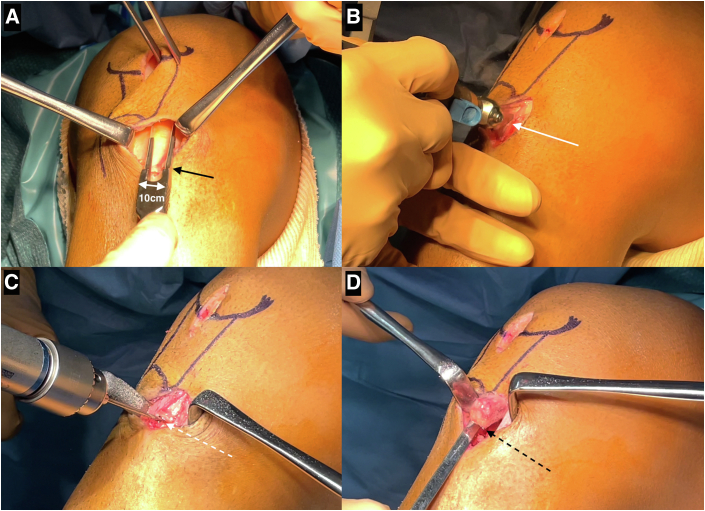
The paratenon is identified and divided longitudinally. The middle third of the patellar tendon is then incised longitudinally using a double-bladed scalpel with a width of 10 mm. The bone blocks are harvested using an oscillating saw. Two 2-mm drill holes are placed on the patella bone block for a figure-of-8 traction suture, and a further drill hole is made 5 mm from the end of the tibial bone block. Drill holes are then made around the bone blocks to prevent fractures when they are removed with a chisel. First, the tibial bone block is removed, and then it is delivered to the proximal incision after releasing adhesions from the patellar tendon; then finally, the patella bone block is removed (Fig 3).
Fig 3.
Graft harvest. (A) Right knee, frontal view. The middle third of the patellar tendon is incised longitudinally using a double-bladed scalpel (black arrow) with a width of 10 mm. (B) Right knee, medial view. The bone blocks are harvested using an oscillating saw (white arrow). (C) Right knee, medial view. Drill holes (white dotted arrow) are made around the blocks to prevent fractures when they are removed. (D) Right knee, medial view. The blocks are removed with a chisel (black dotted arrow).
Graft Preparation and Diagnostic Arthroscopy
The tibial bone block is cut in a trapezoidal fashion, and the patella bone block is cut in a triangular fashion. The intention is to create a 11 × 20 mm bone block from the tibial tuberosity and a 9 × 15mm bone block from the patella. A number-3 suture (Mersilene, Ethicon) is passed through the 2-mm drill hole in the tibial bone block. The patella bone block is prepared with a number-3 suture (Mersilene, Ethicon) and a number-2 suture (Polysorb, Covidien) in a figure-of-eight shape then a knot is positioned at the extremity. This configuration allows this bone block to be pulled during graft passage. The junctions between the tendon and bone are then marked with a sterile marker pen. Any excess bone from the graft preparation is kept for adding to the harvest sites at the end of the procedure (Fig 4).
Fig 4.
Graft preparation. A 11 × 20 mm bone block from the tibial tuberosity and a 9 × 15 mm bone block from the patella is created. A single suture is positioned through the drill hole in the tibial block (white arrow) and the patella block is prepared with 2 separate sutures in a figure-of-eight (black arrow) to allow the block to be pulled during graft passage.
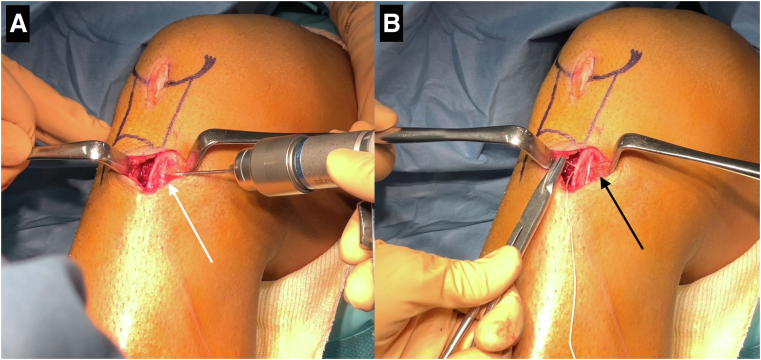
Two 2-mm drill holes are then made at the harvest site on the tibia, and number-1 sutures (Polysorb, Covidien) are looped through, to be used to facilitate secondary fixation later in the procedure. In addition, the patellar tendon defects are closed to help prevent leakage of fluid during the arthroscopy (Fig 5).
Fig 5.
Preparation for secondary fixation. Right knee, medial view. (A) 2-mm drill holes (white arrow) are made at the harvest site on the tibia. (B) Sutures are looped through the drill holes (black arrow) to be used to facilitate secondary fixation later in the procedure.
High anterolateral and anteromedial portals are established. A diagnostic arthroscopy is performed and any meniscal or chondral lesions are addressed before the ACLR.
Femoral Tunnel
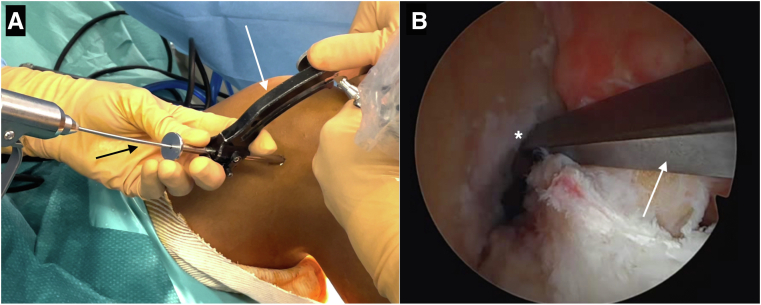
The femoral outside-in ACL guide (Arthrex) is positioned at the femoral origin of the ACL via the anteromedial portal. A lateral skin incision of around 2 cm is made for the guide to be positioned after it is set at an angle of 90°. A guidewire is inserted, and the correct position is confirmed arthroscopically. The femoral tunnel is established using outside-in drilling, starting with a 6-mm cannulated reamer. Initially, using a 6-mm reamer allows the position of the femoral tunnel to be rechecked and adjustments can be made in the direction of the subsequent 10-mm reamer, if necessary. The lateral aperture of the tunnel is then reamed to 11 mm for press-fit fixation (Fig 6).
Fig 6.
Femoral tunnel. (A) Right knee, lateral view. The bullet of the femoral outside-in ACL guide (white arrow) is positioned and a guidewire (black arrow) is inserted (B) Right knee, arthroscopic view. The guide (white arrow) is positioned at the femoral origin (∗) of the ACL.
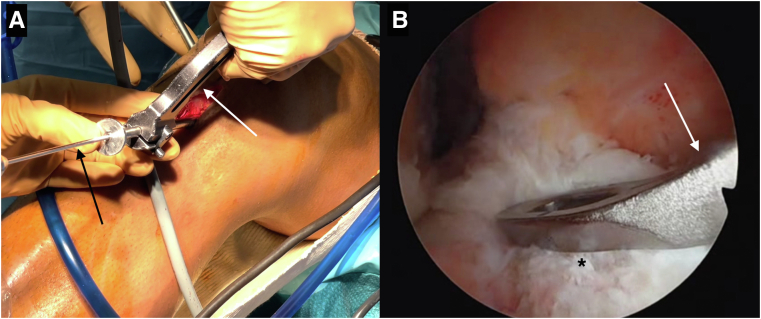
Tibial Tunnel
The tibial ACL guide (Arthrex) is set at 55° and then introduced through the anteromedial portal. It is positioned over the ACL footprint, and a guidewire is inserted. The tibial tunnel is established, starting with a 6-mm reamer and then upsizing to a 9-mm reamer once the position is confirmed. A shaver is then introduced into the tibial tunnel to debride the aperture of the tunnel. Reamings are collected to add to the harvest sites at the end of the procedure (Fig 7).
Fig 7.
Tibial tunnel. (A) Right knee, medial view. The tibial ACL guide (white arrow) is positioned and a guidewire (black arrow) is inserted. (B) Right knee, arthroscopic view. The guide (white arrow) is positioned over the ACL footprint (∗).
Graft Passage and Fixation
A number-2 passing suture (Polysorb, Covidien) is delivered from the tibial tunnel then through the femoral tunnel for antegrade passage of the graft. The sutures from the patella bone block are then inserted into the loop created by the passing suture. Using a clamp, the surgeon guides the patella bone block through the femoral tunnel and then the traction sutures are pulled to allow passage of the graft. A probe is sometimes required to assist the graft passage, particularly at the intra-articular entrance of the femoral tunnel. The tibial bone block is inserted in the femoral tunnel with the cortex face posteriorly. While the surgical assistant performs gentle traction distally, the surgeon lightly hammers the bone block using an impactor until press fit fixation is achieved. The previously marked junction is seen arthroscopically arriving at the intra-articular entrance of the femoral tunnel. Moreover, the marked junction is important on the tibial side to ensure that the whole bone block is in the tunnel and that there is no risk of impingement (Fig 8).
Fig 8.
Graft passage. Right knee, lateral view. (A) A passing suture (white dotted arrow) is delivered from the tibial tunnel then through the femoral tunnel and the sutures from the patella bone block (∗) are then inserted into the loop (white arrow) created by the passing suture. (B) Using a clamp (black arrow), the surgeon guides the patella bone block (∗) through the femoral tunnel then the traction sutures are pulled (white dotted arrow) to allow passage of the graft. (C) While the surgical assistant performs gentle traction distally (white dotted arrow), the surgeon lightly hammers the bone block (black dotted arrow) using an impactor until press fit fixation is achieved.
Maximal manual tension is then applied to the sutures of the patella bone block, and the knee is cycled through full flexion and extension several times in order to assure the full passage of the graft. The knee is then placed in 30° of flexion, and tibial fixation is achieved using an interference screw (Biocomposite, Arthrex). Double fixation of the graft is then performed on the tibial side using the transosseous sutures positioned on the tibial tuberosity earlier in the procedure. Finally, bone graft is inserted into the graft harvest sites, and the wounds are closed (Fig 9).
Fig 9.
Graft fixation. Right knee, medial view. (A) The knee is placed in 30° of flexion, and tibial fixation is achieved using an interference screw (white arrow) (B) Double fixation of the graft is performed on the tibial side using the transosseous sutures positioned on the tibial tuberosity (black arrow) (C) Bone graft (∗) is inserted into the graft harvest sites.
Postoperative Rehabilitation
Postoperative rehabilitation begins with brace-free, full weight bearing and progressive range of motion exercises, with restriction of range of motion to 0-90° for 6 weeks in patients undergoing meniscal repair. Early rehabilitation focuses on maintaining full extension and quadriceps activation exercises. Return to sports is allowed at 4 months for nonpivoting sport, 6 months for pivoting noncontact sport, and 8 to 9 months for pivoting contact sports.
Discussion
This original ACLR technique using press-fit femoral fixation of the BPTB graft through an outside-in drilling technique was first described by Pierre Chambat in 1989. This technique has been associated with numerous studies and has evolved over the years.6, 7, 8 The rationale of this technique is based on two important technical aspects, press-fit fixation and outside-in drilling (Fig 10).
Fig 10.
The original technique. Illustration demonstrating the graft preparation, graft passage, and final construct following fixation.
Primary stability of the bone plug of the BPTB graft into the femoral tunnel is achieved through press-fit fixation leading to bone-to-bone healing. Therefore, additional screw fixation of the graft on the femoral side is not required. Indeed, Gobbi et al.9 has outlined the problems of interference screw fixation, such as screw misplacement, potential impingement, and abrasion. In addition, MRI interpretation postoperatively, especially when rerupture is suspected, can be difficult when metallic screws have been used. Revision ACLR is also made easier by the fact that no hardware requires removal. Additionally, recent studies have demonstrated that the implant-free press-fit fixation provides adequate primary stability with ultimate load to failure that is at least equal to the published results for interference screws.10,11 Furthermore, Biazzo et al.12 found better clinical results and better knee stability using press-fit femoral fixation in comparison to screw fixation in a 20-year follow-up study.
Outside-in drilling is a safe technique and leads to anatomic positioning of the ACL femoral tunnel at the center of the native ACL footprint. Moreover, outside-in drilling facilitates posterior wall preservation and adequate tunnel length, which is important for the stable fixation of the graft into the tunnel, whichever graft is used.7,13 This technique is also essential during revision ACLR (RACLR) as a result of its unconstrained nature, allowing the creation of RACLR tunnels that are divergent to the previous tunnels. Consequently, adequate graft fixation and positioning can be achieved regardless of the preoperative presence of tunnel widening or malposition.14
In summary, this original technique describes anterior cruciate ligament reconstruction using bone-patella tendon-bone autograft with press-fit femoral fixation using an outside-in drilling technique.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.S.-C. reports personal fees from Arthrex, outside the submitted work. G.H. reports a fellowship grant from Arthrex. J.-M.F. reports consulting fees from Arthrex and Newclip Technics, outside the submitted work. M.T. reports being a paid consultant for Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This technical note describes the original technique which is an anterior cruciate ligament reconstruction using bone-patella tendon-bone autograft with press-fit femoral fixation using an outside-in drilling technique.
References
- 1.Chambat P., Guier C., Sonnery-Cottet B., Fayard J.M., Thaunat M. The evolution of ACL reconstruction over the last fifty years. Int Orthop. 2013;37:181–186. doi: 10.1007/s00264-012-1759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delay B.S., Smolinski R.J., Wind W.M., Bowman D.S. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Knee Surg. 2001;14:85–91. [PubMed] [Google Scholar]
- 3.Webster K.E., Feller J.A., Hartnett N., Leigh W.B., Richmond A.K. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: A 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44:83–90. doi: 10.1177/0363546515611886. [DOI] [PubMed] [Google Scholar]
- 4.Mascarenhas R., Tranovich M.J., Kropf E.J., Fu F.H., Harner C.D. Bone-patellar tendon-bone autograft versus hamstring autograft anterior cruciate ligament reconstruction in the young athlete: a retrospective matched analysis with 2-10 year follow-up. Knee Surg Sports Traumatol Arthrosc. 2012;20:1520–1527. doi: 10.1007/s00167-011-1735-2. [DOI] [PubMed] [Google Scholar]
- 5.Chambat P., Verdot F. Arthroscopie. 2e ed. Elsevier; 2006. Reconstruction du ligament croisé antérieur avec un tunnel fémoral de dehors en dedans; pp. 139–142. [Google Scholar]
- 6.Garofalo R., Mouhsine E., Chambat P., Siegrist O. Anatomic anterior cruciate ligament reconstruction: the two-incision technique. Knee Surg Sports Traumatol Arthrosc. 2006;14:510–516. doi: 10.1007/s00167-005-0029-y. [DOI] [PubMed] [Google Scholar]
- 7.Gill T.J., Steadman J.R. Anterior cruciate ligament reconstruction the two-incision technique. Orthop Clin North Am. 2002;33:727–735. doi: 10.1016/s0030-5898(02)00030-5. vii. [DOI] [PubMed] [Google Scholar]
- 8.Gaudot F., Leymarie J.B., Drain O., Boisrenoult P., Charrois O., Beaufils P. Double-incision mini-invasive technique for BTB harvesting: its superiority in reducing anterior knee pain following ACL reconstruction. Orthop Traumatol Surg Res. 2009;95:28–35. doi: 10.1016/j.otsr.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Gobbi A., Diara A., Mahajan S., Zanazzo M., Tuy B. Patellar tendon anterior cruciate ligament reconstruction with conical press-fit femoral fixation: 5-year results in athletes population. Knee Surg Sports Traumatol Arthrosc. 2002;10:73–79. doi: 10.1007/s00167-001-0265-8. [DOI] [PubMed] [Google Scholar]
- 10.Pavlik A., Hidas P., Czigány T., Berkes I. Biomechanical evaluation of press-fit femoral fixation technique in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:528–533. doi: 10.1007/s00167-003-0452-x. [DOI] [PubMed] [Google Scholar]
- 11.Arnold M.P., Burger L.D., Wirz D., Goepfert B., Hirschmann M.T. The biomechanical strength of a hardware-free femoral press-fit method for ACL bone-tendon-bone graft fixation. Knee Surg Sports Traumatol Arthrosc. 2017;25:1234–1240. doi: 10.1007/s00167-015-3960-6. [DOI] [PubMed] [Google Scholar]
- 12.Biazzo A., Manzotti A., Motavalli K., Confalonieri N. Femoral press-fit fixation versus interference screw fixation in anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft: 20-year follow-up. J Clin Orthop Trauma. 2018;9:116–120. doi: 10.1016/j.jcot.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robin B.N., Jani S.S., Marvil S.C., Reid J.B., Schillhammer C.K., Lubowitz J.H. Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2015;31:1412–1417. doi: 10.1016/j.arthro.2015.01.018. [DOI] [PubMed] [Google Scholar]
- 14.Pioger C., Saithna A., Rayes J., et al. Influence of preoperative tunnel widening on the outcomes of a single stage-only approach to every revision anterior cruciate ligament reconstruction: An analysis of 409 consecutive patients from the SANTI Study Group. Am J Sports Med. 2021;49:1431–1440. doi: 10.1177/0363546521996389. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This technical note describes the original technique which is an anterior cruciate ligament reconstruction using bone-patella tendon-bone autograft with press-fit femoral fixation using an outside-in drilling technique.
This technical note describes the original technique which is an anterior cruciate ligament reconstruction using bone-patella tendon-bone autograft with press-fit femoral fixation using an outside-in drilling technique.