A 40-year old male presented to his GP with a red spot on the tip of his nose which was initially classified as a sunburn. Within three days, the nasal area progressed to necrosis (Fig. 1). In parallel, typical MPXV lesions (confirmed by PCR) appeared on the whole body with serious infection of the penis and oral mucosa. The patient was transferred to a tertiary care hospital for tecovirimat treatment. Diagnostic work-up revealed a concomitant syphilis of longer duration (TPPA 1:2560, VDRL 1:8) and an advanced HIV infection with a CD4 T cell count of 127/uL. The patient had never been tested for sexually transmitted diseases (STD) before. The patient was treated with oral tecovirimat 600 mg bid for 7 days in addition to antiretroviral therapy (bictegravir/emtricitabine/tenofoviralafenamide single tablet p.o. qd) for the HIV infection and ceftriaxone 2 g i.v. for 10 days for the syphilis. The monkeypox lesions on the skin dried out and the nose partially improved with less swelling. Most cases of MPXV infection so far have been reported as mild and controlled HIV infection does not appear to be a risk factor for severe courses [1–4]. However, this case illustrates the potential severity of MPXV infection in the setting of severe immunosuppression and untreated HIV infection.
Fig. 1.
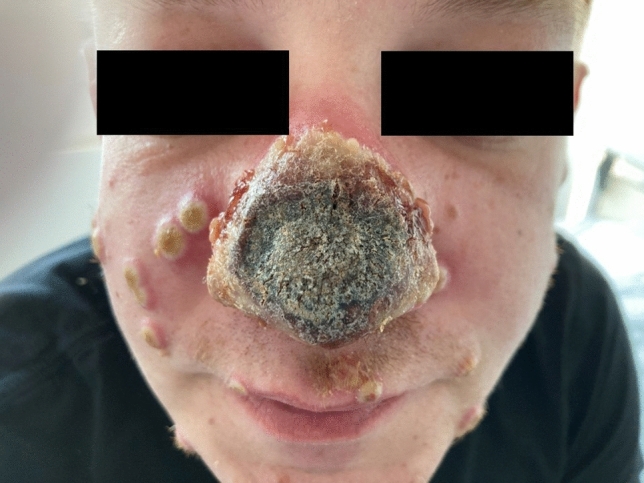
Nasal necrosis and skin lesions due to MPXV infection in a patient with advanced undiagnosed HIV infection
Author contributions
CB wrote the manuscript draft. All authors have reviewed the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. None.
Data availability
Upon request from corresponding author.
Declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
Patient gave written consent to participate and be published.
Consent to participate and consent to publish
Patient gave written consent to participate and be published.
References
- 1.Noe S, Zange S, Seilmaier M, Antwerpen MH, Fenzl T, Schneider J, Spinner CD, Bugert JJ, Wendtner CM, Wölfel R. Clinical and virological features of first human monkeypox cases in Germany. Infection. 2022 doi: 10.1007/s15010-022-01874-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thornhill JP, Barkati S, Walmsley S, Rockstroh J, Antinori A, Harrison LB, Palich R, Nori A, Reeves I, Habibi MS, Apea V, Boesecke C, Vandekerckhove L, Yakubovsky M, Sendagorta E, Blanco JL, Florence E, Moschese D, Maltez FM, Goorhuis A, Pourcher V, Migaud P, Noe S, Pintado C, Maggi F, Hansen AE, Hoffmann C, Lezama JI, Mussini C, Cattelan A, Makofane K, Tan D, Nozza S, Nemeth J, Klein MB, Orkin CM. SHARE-net clinical group. N Engl J Med. 2022 doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 3.Hoffmann C, Jessen H, Teichmann J, Wyen C, Noe S, Kreckel P, Köppe S, Krauss AS, Schuler C, Bickel M, Lenz J, Scholten S, Klausen G, Lindhof HH, Jensen B, Glaunsinger T, Pauli R, Härter G, Radke B, Unger S, Marquardt S, Masuhr A, Esser S, Flettner TO, Schäfer G, Schneider J, Spinner CD, Boesecke C. Monkeypox in Germany—initial clinical observations. Dtsch Arztebl Int. 2022 doi: 10.3238/arztebl.m2022.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlabe S, Isselstein J, Boesecke C. Ulcer at corner of mouth as first sign of infection with monkeypox virus. Dtsch Arztebl Int. 2022;119:511. doi: 10.3238/arztebl.m2022.0274. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Upon request from corresponding author.


