Abstract
Diagnostic needle arthroscopy performed in office is a safe and cost-effective method for accurate evaluation of intra-articular pathology, improving clinical decision making. This minimally invasive approach is an effective alternative to traditional diagnostic techniques of diagnostic surgical arthroscopy and magnetic resonance imaging (MRI). Needle arthroscopy is considered low-risk, with an extremely low complication rate when performed with appropriate technique and indications. The purpose of this article is to describe an approach to an in-office diagnostic procedure using a needle arthroscopy system.
Technique Video
Standard arthroscopic approach to the left knee via anterolateral and anteromedial portals. Place the patient in a supine or sitting position, with the left knee at ∼90°, and sterilely prep the left knee. Anesthetize the anterolateral and anteromedial standard portal sites with ∼15 cc of local anesthetic (1% lidocaine with epinephrine and 0.5% Marcaine without epinephrine) on a 25-gauge needle, creating a wheel. Next, insufflate the joint via the anterolateral portal using 20 cc of .25% Marcaine without epinephrine on a 20-gauge needle. After an additional re-prep of the knee with chlorohexidine, wait about 5 minutes, and then place sterile blue drapes at the proximal tibia and distal femur to create a sterile field. Introduce the 2.2-mm inflow NanoScope™ (Arthrex) sheath with the sharp trocar into the anterolateral portal, which is the primary viewing portal, and withdraw the trocar, and then attach the one-way stop valve to the sheath. Insert the 1.9-mm NanoScope™ (Arthrex) needle arthroscopy system, which is approximately one-third of the size of a standard arthroscopy camera. Connect a 30-cc syringe of sterile 0.9% normal saline to the NanoScope™ (Arthrex) via the one-way stop valve, open the valve, and use all 30 cc to insufflate the joint. This is followed by connecting another 30 cc of sterile saline to the one-way stop valve to inject as needed, while performing a standard diagnostic left knee arthroscopy to identify and assess any intraarticular pathology. In this particular patient, a medial femoral condyle defect is identified. If needed, a 2.0-mm NanoProbe (Arthrex) or other NanoSope™ (Arthrex) instrumentation can be used for both diagnostic and therapeutic treatment. This is inserted into the anteromedial portal, which is the accessory portal. If possible, have an assistant available to provide valgus stress or assist in patient knee positioning, as the arthroscopy is being performed. At the conclusion of the standard diagnostic needle arthroscopy, aspirate as much fluid off the knee as possible through the NanoSope™ (Arthrex), while it remains inserted in the anterolateral portal. Remove the scope and resolve any bleeding by applying pressure with sterile gauze. Apply Steri-Strips to the percutaneous portal sites, followed by gauze and an ACE wrap. The patient may ambulate immediately afterward. Post-procedure antibiotics may be considered
Introduction
In-office diagnostic needle arthroscopy has become increasingly popular as a feasible technique to accurately diagnose and treat intra-articular pathology, improving clinical and surgical decision-making and patient satisfaction.1,2 Notably, in-office needle arthroscopy has been shown to be a safe procedure with multiple studies documenting a 0% infection rate in both the shoulder and the knee.1 Further, in some settings, this procedure has been found to be statistically equivalent in both efficiency and accuracy when compared to diagnostic surgical arthroscopy, and more accurate than MRI, without increased complications.3, 4, 5 Real-time visualization of intra-articular pathology in an office setting can lead to reduced duration of time between diagnosis and ultimate management (whether surgical or nonsurgical), therefore, reducing time between injury and recovery.6,7 Indications for an in-office diagnostic needle arthroscopy of the knee include patients who are unable to obtain an MRI (i.e., due to a pacemaker, claustrophobia, etc.), patients with suspected intra-articular pathologies, including meniscal tears, chondral lesions, ligament tears, and loose bodies; and further, can be used for second-look arthroscopy following a variety of procedures, including meniscus and/or cartilage repair/restoration when MRI may not provide clear results.5,6 The purpose of this Technical Note is to describe a standard in-office needle arthroscopy technique using the NanoScope™ (Arthrex Inc., Naples, FL) arthroscopy system.
Surgical Technique
A demonstration of a diagnostic knee arthroscopy performed in an office setting using the NanoScope™ (Arthrex Inc.) arthroscopy system is presented in Video 1.
Preprocedure Evaluation and Processes
A thorough evaluation is performed on the patient, including medical history and physical examination. The patient undergoes standard weight-bearing radiographs of the knee, including anterior-posterior, lateral, merchant, and posterior-anterior flexion (Rosenberg) views, as well as bilateral long-leg weight-bearing alignment radiographs when indicated. MRI may be performed in addition to the needle arthroscopy when pathology of the bone (i.e., bone marrow edema-like reactions and/or bone involvement in osteochondral defects) and/or extra-articular anatomy, requires evaluation. Risks, benefits, and alternatives to the procedure are discussed with the patient, informed consent is obtained, and a procedural time-out is performed.
Procedural Steps
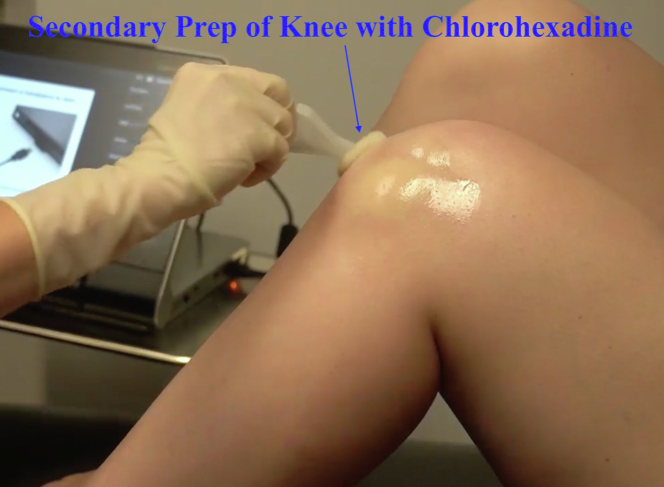
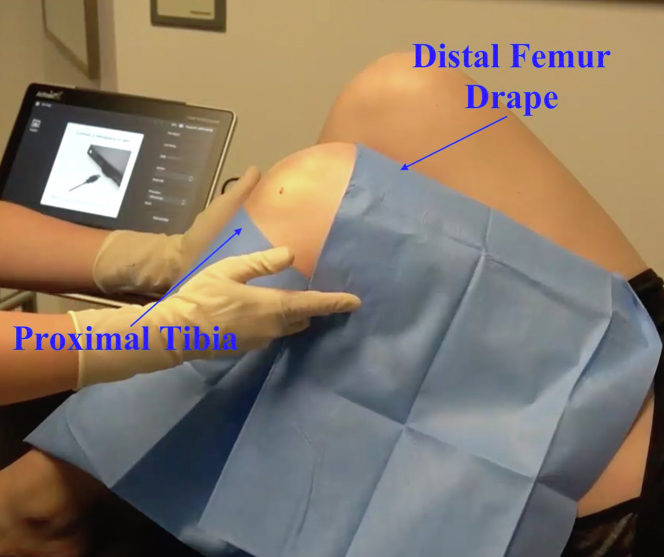
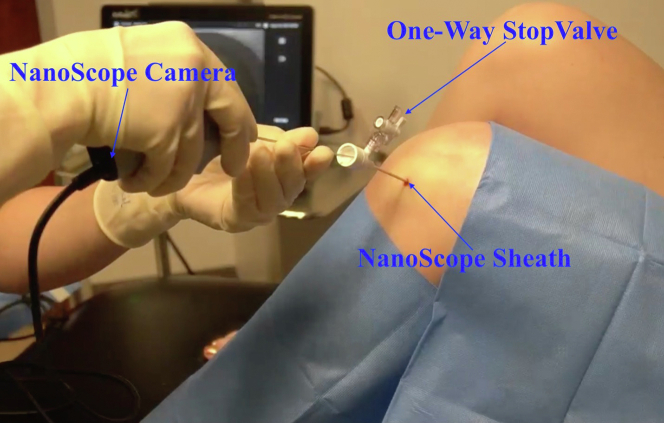
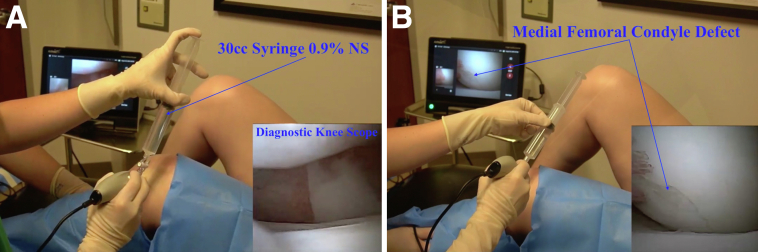
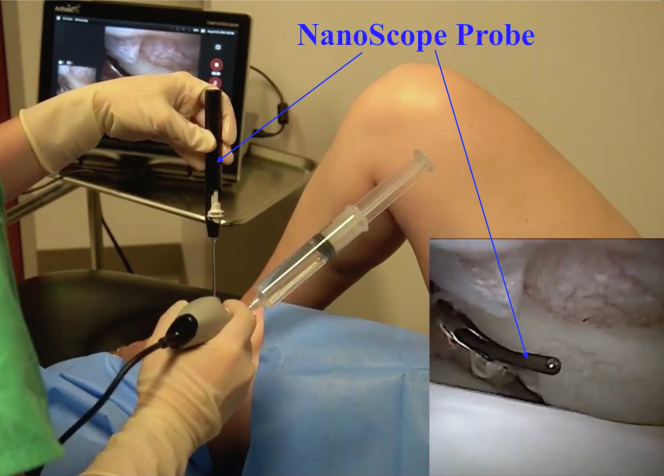
The patient is positioned supine on the examination table, and can either lie down on the table or sit up leaning against the back of the table or wall if they wish to observe the procedure. The NanoScope™ (Arthrex Inc.) console is placed in proximity to the patient area and facing the surgeon outside of the sterile field. The affected knee is preliminarily prepped with alcohol and chlorhexidine. The desired portal site (standard anterolateral or anteromedial portal) is identified, and a 25-gauge needle is used to inject approximately 7.5 cc of a mixture of local anesthetic, including 1% lidocaine with epinephrine and 0.5% Marcaine without epinephrine at the capsule only, creating a wheel (Fig 1). The epinephrine is helpful to improve hemostasis at the portal site(s). Both portal sites can be anesthetized if the surgeon anticipates using both portals during the procedure (i.e., one for viewing and one for probing), although for diagnostic purposes alone, the authors prefer to only anesthetize a single. Next, a sterile field adjacent to the examination table with either a mayo stand or side table is prepared with sterile, disposable drapes. The NanoScope™ (Arthrex Inc.) handpiece kit is opened and placed onto this field in preparation for the procedure. The skin over the anterior aspect of the knee, from the superior pole of the patella to the region of the distal patellar tendon prepped with chlorhexidine, and drapes are placed along the superior and inferior borders of this sterile field, creating a working space centered over the patella. Next, using an 18- or 20-gauge needle, ∼20 cc of 0.25% Marcaine without epinephrine is injected into the joint (Fig 2, Fig 3). After a few minutes, the 2.2-mm inflow NanoScope™ (Arthrex Inc.) sheath with sharp trocar is inserted through the anterolateral (or anteromedial) portal into the knee joint, the trocar is withdrawn, the one way stop valve is attached, and the 1.9-mm NanoScope™ (Arthrex Inc.) is inserted (Fig 4). A 30-cc syringe of sterile 0.9% normal saline is then connected to the NanoScope™ (Arthrex Inc.) via the one-way stop valve, the valve is opened, and the saline is used to insufflate the knee. This is followed by the injection of additional saline, up to 90-100 mL total, injected as needed to insufflate the joint and improve visualization. The diagnostic arthroscopy of the knee is then performed on the basis of the patient’s clinical history, physical examination, and any previously obtained diagnostic imaging (Fig 5, A and B). Using the opposite portal, a NanoProbe™ (Arthrex Inc.) may be used to evaluate the pathology, particularly useful for sizing chondral defects and/or probing the meniscus (Fig 6). If necessary, the scope may be alternated between the anterolateral and anteromedial portal sites, depending on required visualization, although the authors preference is to maintain efficiency of the procedure by avoiding unnecessary withdrawal and subsequent reintroduction of the scope. At the conclusion of the procedure, all previously insufflated saline is aspirated via the stop valve, and the NanoScope™ (Arthrex Inc.) is removed (Fig 7). A sterile dressing with Steri-Strips, 4×4" gauzes, and an ace-wrap is then applied. The post-procedural plan includes permitted weight-bearing and range of motion, as tolerated, and the use of acetaminophen and/or NSAIDs for pain control. No narcotics are prescribed post-procedure, and no sedatives are used before or during the procedure.
Fig 1.
Clinical photograph demonstrating the authors’ preferred approach to in-office needle arthroscopy (left knee). Standard anterolateral and anteromedial portals are shown. With the patient seated and the knee flexed to approximately 90 degrees, a 25-gauge needle is used to inject local anesthetic at one or both portal sites, staying superficial at the skin, making a wheel.
Fig 2.
Clinical photograph (left knee) demonstrating the lateral side of the knee prior to introducing the needle-scope. After the local anesthetic has been injected superficially, the knee is re-prepped with chlorohexidine, after which, sterile drapes are placed.
Fig 3.
Clinical photograph (left knee) demonstrating the use of sterile drapes proximally (along the distal femur) and distally (along the proximal tibia), creating a sterile field prior to introduction of the needle scope.
Fig 4.
Clinical photograph (left knee) demonstrating introduction of the 2.2mm inflow NanoScope (Arthrex Inc.) sheath with sharp trocar through the anterolateral portal into the joint. After successful insertion into the joint, the trocar is removed, and the one-way stop valve is attached to the sheath. Next, the 1.9-mm NanoScope (Arthrex Inc.) is inserted through the sheath. A 30-cc syringe of sterile 0.9% normal saline is then connected to the one-way stop valve, and the saline is used to insufflate the joint.
Fig 5.
(A) View of the lateral side of the left knee. Inset is an arthroscopic view of the left knee through the anterolateral portal site. After insufflating the joint with 30 cc of sterile 0.9% normal saline, additional sterile saline can be injected via the one-way stop valve as needed during the diagnostic procedure to improve visualization. A standard diagnostic arthroscopy of the left knee is performed, as pictured in the inset. (B) View of the lateral side of the left knee. Inset is an arthroscopic view of the left knee through the anterolateral portal site. The medial femoral condyle full-thickness osteochondral defect is identified (pictured in the inset).
Fig 6.
Clinical photograph (left knee). Inset is an arthroscopic view of the left knee through the anterolateral portal site. The medial femoral condyle defect is being probed with a NanoProbe (Arthrex Inc.) through the anteromedial portal, which is the accessory portal, as pictured in the inset. This provides the ability to assess the pathology in question and further evaluate the entirety of the joint.
Fig 7.
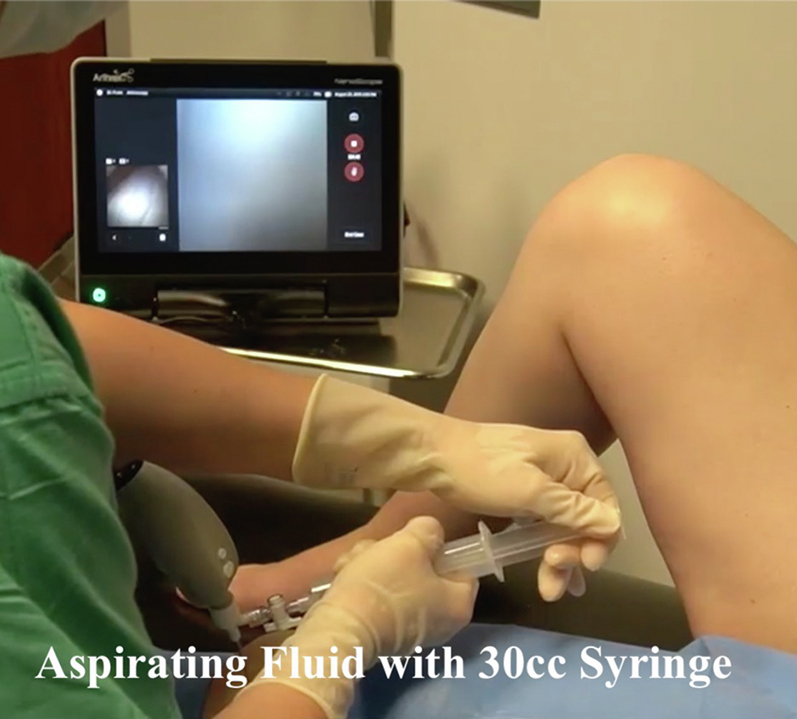
Clinical photograph (left knee), demonstrating the authors' preferred technique of aspirating as much fluid as possible through the scope at the conclusion of the procedure. The scope is removed and the portal sites are dressed with Steri-Strips, gauze, and an ACE wrap. The patient is allowed immediate weight-bearing as tolerated and range-of-motion as tolerated.
Discussion
Traditional diagnostic arthroscopy has historically been considered the optimal technique arriving at a definitive diagnosis of intra-articular knee pathology.8 However, traditional knee arthroscopy requires a surgical procedure typically performed under general (or spinal) anesthesia, with associated costs and risks of complications. MRI has also traditionally been considered the optimal noninvasive diagnostic tool for both intra-articular and extra-articular knee pathology, and although MRI certainly has value as a diagnostic tool, it can be costly, time-consuming, difficult for some patients to tolerate, and further, remains imprecise in comparison to arthroscopy, particularly for the identification and sizing of chondral lesions.1,8 Several studies have reported statistical equivalence, with respect to accuracy, sensitivity, and specificity, of diagnostic in-office needle arthroscopy compared to diagnostic surgical arthroscopy in detecting knee joint pathology.3,4 A minimally invasive needle-scope used in an office-based setting maintains the high level of accuracy of surgical arthroscopy, while reducing costs to the healthcare system, offloads the costs of regular use of MRIs, provides a point-of-care diagnosis, and reduces the time from injury to recovery.9 Further, McMillan and colleagues recently validated the safety of this procedure, reporting no major complications and a minimal risk of minor complications among 1,419 cases, which included shoulders and knees.1
Amin et al. recently performed a cost-analysis of in-office needle arthroscopy versus MRI and found that needle arthroscopy was the more cost-effective diagnostic tool.10 Further, patient-reported outcomes were evaluated over a 2-year period from baseline, and it was shown that needle arthroscopy resulted in similar outcomes compared with MRI. Combined with previously reported findings of MRI unreliability, the authors concluded that MRI resulted in more costly care compared to needle arthrorscopy.10 Additional research has shown that the use of in-office needle arthroscopy in place of MRI has several potential additional benefits in addition to saving the healthcare system money. These include shortening the diagnostic process for patients, allowing their active participation for improved understanding of their condition; high patient satisfaction rates; better preparing surgeons for definitive surgical procedure(s) when needed; and eliminating unnecessary, higher risk outpatient arthroscopy procedures simply to get a diagnosis.7,9
In-office needle arthroscopy is not without limitations. Most importantly, with a lack of continuous fluid flow during the procedure, visualization may be impacted, possibly decreasing the diagnostic accuracy. In addition, while not overly painful, some patients may not tolerate being awake for such a procedure. The pearls and pitfalls of this technique are outlined in Table 1, and the advantages and disadvantages are listed in Table 2. In summary, using in-office needle arthroscopy as a diagnostic tool is a safe and effective alternative to surgical arthroscopy or MRI for evaluation of intra-articular knee pathology. A standard technique has been described here using the NanoScope™ (Arthrex Inc.) arthroscopy system.
Table 1.
Pearls and Pitfalls for Performing Diagnostic Arthroscopy Using In-Office Needle Arthroscopy
| Pearls |
| Additional saline beyond initial insufflation may be used to improve visualization by serially injecting saline through the NanoScope™ (Arthrex) cannula. |
| Give adequate time for incisional and intra-articular block to set up before proceeding. |
| Pitfalls |
| Patients with multiple knee surgeries have too much arthrofibrosis for appropriate visualization. |
| Patient compliance and motion may decrease diagnostic accuracy. |
| Utilizes clinic time and staff. |
Table 2.
Advantages and Disadvantages of Performing Diagnostic Arthroscopy Using In-Office Needle Arthroscopy
| Advantages |
| Shorter delay in definitive diagnosis. |
| Decreased operative burden and anesthesia for patients. |
| More accurate and real-time diagnosis for patients. |
| Disadvantages |
| Can interfere with clinic workflow, consume staff time, and clinic resources. |
| Learning curve for provider and staff in clinic. |
| Can cause patient pain and/or discomfort. |
| Increased risk compared to MRI alone. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.M.F. is a consultant and receives research support from Arthrex Inc.; publishing royalties from Elsevier; she is a board or committee member of AOSSM, AAOS, AANA, ICRS, and she also is on the editorial or governing board of JCJP and Orthopedics Today. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Standard arthroscopic approach to the left knee via anterolateral and anteromedial portals. Place the patient in a supine or sitting position, with the left knee at ∼90°, and sterilely prep the left knee. Anesthetize the anterolateral and anteromedial standard portal sites with ∼15 cc of local anesthetic (1% lidocaine with epinephrine and 0.5% Marcaine without epinephrine) on a 25-gauge needle, creating a wheel. Next, insufflate the joint via the anterolateral portal using 20 cc of .25% Marcaine without epinephrine on a 20-gauge needle. After an additional re-prep of the knee with chlorohexidine, wait about 5 minutes, and then place sterile blue drapes at the proximal tibia and distal femur to create a sterile field. Introduce the 2.2-mm inflow NanoScope™ (Arthrex) sheath with the sharp trocar into the anterolateral portal, which is the primary viewing portal, and withdraw the trocar, and then attach the one-way stop valve to the sheath. Insert the 1.9-mm NanoScope™ (Arthrex) needle arthroscopy system, which is approximately one-third of the size of a standard arthroscopy camera. Connect a 30-cc syringe of sterile 0.9% normal saline to the NanoScope™ (Arthrex) via the one-way stop valve, open the valve, and use all 30 cc to insufflate the joint. This is followed by connecting another 30 cc of sterile saline to the one-way stop valve to inject as needed, while performing a standard diagnostic left knee arthroscopy to identify and assess any intraarticular pathology. In this particular patient, a medial femoral condyle defect is identified. If needed, a 2.0-mm NanoProbe (Arthrex) or other NanoSope™ (Arthrex) instrumentation can be used for both diagnostic and therapeutic treatment. This is inserted into the anteromedial portal, which is the accessory portal. If possible, have an assistant available to provide valgus stress or assist in patient knee positioning, as the arthroscopy is being performed. At the conclusion of the standard diagnostic needle arthroscopy, aspirate as much fluid off the knee as possible through the NanoSope™ (Arthrex), while it remains inserted in the anterolateral portal. Remove the scope and resolve any bleeding by applying pressure with sterile gauze. Apply Steri-Strips to the percutaneous portal sites, followed by gauze and an ACE wrap. The patient may ambulate immediately afterward. Post-procedure antibiotics may be considered
References
- 1.McMillan S., Chhabra A., Hassebrock J.D., Ford E., Amin N.H. Risks and complications associated with intra-articular arthroscopy of the knee and shoulder in an office setting. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119869846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gauci M.-O., Monin B., Rudel A., Blasco L., Bige B., Boileau P. In-office biceps tenotomy with needle arthroscopy: A feasibility study. Arthrosc Tech. 2021;10:e1263–e1268. doi: 10.1016/j.eats.2021.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill T.J., Safran M., Mandelbaum B., Huber B., Gambardella R., Xerogeanes J. A prospective, blinded, multicenter clinical trial to compare the efficacy, accuracy, and safety of in-office diagnostic arthroscopy with magnetic resonance imaging and surgical diagnostic arthroscopy. Arthroscopy. 2018;34:2429–2435. doi: 10.1016/j.arthro.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Xerogeanes J.W., Safran M.R., Huber B., Mandelbaum B.R., Robertson W., Gambardella R.A. A prospective multi-center clinical trial to compare efficiency, accuracy and safety of the VisionScope Imaging System compared to MRI and diagnostic arthroscopy. Orthop J Sports Med. 2014;2 2325967114S2325960010. [Google Scholar]
- 5.Dibartola A.C., Rogers A., Kurzweil P., Knopp M.V., Flanigan D.C. In-office needle arthroscopy can evaluate meniscus tear repair healing as an alternative to magnetic resonance imaging. Arthroscopy. 2021;3:e1755–e1760. doi: 10.1016/j.asmr.2021.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMillan S., Saini S., Alyea E., Ford E. Office-based needle arthroscopy: A standardized diagnostic approach to the knee. Arthrosc Tech. 2017;6:e1119–e1124. doi: 10.1016/j.eats.2017.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colasanti C.A., Mercer N.P., Garcia J.V., Kerkhoffs G., Kennedy J.G. In-office needle arthroscopy for the treatment of anterior ankle impingement yields high patient satisfaction with high rates of return to work and sport. Arthrosc Tech. 2022;38:1302–1311. doi: 10.1016/j.arthro.2021.09.016. [DOI] [PubMed] [Google Scholar]
- 8.Patel K.A., Hartigan D.E., Makovicka J.L., Dulle D.L., Chhabra A. Diagnostic evaluation of the knee in the office setting using small-bore needle arthroscopy. Arthroscopy Tech. 2018;7:e17–e21. doi: 10.1016/j.eats.2017.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daggett M.C., Stepanovich B., Geraghty B., Meyers A., Whetstone J., Saithna A. Office-based needle arthroscopy: A standardized diagnostic approach to the shoulder. Arthrosc Tech. 2020;9:e521–e525. doi: 10.1016/j.eats.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amin N., McIntyre L., Carter T., Xerogeanes J., Voigt J. Cost-effectiveness analysis of needle arthroscopy versus magnetic resonance imaging in the diagnosis and treatment of meniscal tears of the knee. Arthroscopy. 2019;35:554–562. doi: 10.1016/j.arthro.2018.09.030. e513. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Standard arthroscopic approach to the left knee via anterolateral and anteromedial portals. Place the patient in a supine or sitting position, with the left knee at ∼90°, and sterilely prep the left knee. Anesthetize the anterolateral and anteromedial standard portal sites with ∼15 cc of local anesthetic (1% lidocaine with epinephrine and 0.5% Marcaine without epinephrine) on a 25-gauge needle, creating a wheel. Next, insufflate the joint via the anterolateral portal using 20 cc of .25% Marcaine without epinephrine on a 20-gauge needle. After an additional re-prep of the knee with chlorohexidine, wait about 5 minutes, and then place sterile blue drapes at the proximal tibia and distal femur to create a sterile field. Introduce the 2.2-mm inflow NanoScope™ (Arthrex) sheath with the sharp trocar into the anterolateral portal, which is the primary viewing portal, and withdraw the trocar, and then attach the one-way stop valve to the sheath. Insert the 1.9-mm NanoScope™ (Arthrex) needle arthroscopy system, which is approximately one-third of the size of a standard arthroscopy camera. Connect a 30-cc syringe of sterile 0.9% normal saline to the NanoScope™ (Arthrex) via the one-way stop valve, open the valve, and use all 30 cc to insufflate the joint. This is followed by connecting another 30 cc of sterile saline to the one-way stop valve to inject as needed, while performing a standard diagnostic left knee arthroscopy to identify and assess any intraarticular pathology. In this particular patient, a medial femoral condyle defect is identified. If needed, a 2.0-mm NanoProbe (Arthrex) or other NanoSope™ (Arthrex) instrumentation can be used for both diagnostic and therapeutic treatment. This is inserted into the anteromedial portal, which is the accessory portal. If possible, have an assistant available to provide valgus stress or assist in patient knee positioning, as the arthroscopy is being performed. At the conclusion of the standard diagnostic needle arthroscopy, aspirate as much fluid off the knee as possible through the NanoSope™ (Arthrex), while it remains inserted in the anterolateral portal. Remove the scope and resolve any bleeding by applying pressure with sterile gauze. Apply Steri-Strips to the percutaneous portal sites, followed by gauze and an ACE wrap. The patient may ambulate immediately afterward. Post-procedure antibiotics may be considered
Standard arthroscopic approach to the left knee via anterolateral and anteromedial portals. Place the patient in a supine or sitting position, with the left knee at ∼90°, and sterilely prep the left knee. Anesthetize the anterolateral and anteromedial standard portal sites with ∼15 cc of local anesthetic (1% lidocaine with epinephrine and 0.5% Marcaine without epinephrine) on a 25-gauge needle, creating a wheel. Next, insufflate the joint via the anterolateral portal using 20 cc of .25% Marcaine without epinephrine on a 20-gauge needle. After an additional re-prep of the knee with chlorohexidine, wait about 5 minutes, and then place sterile blue drapes at the proximal tibia and distal femur to create a sterile field. Introduce the 2.2-mm inflow NanoScope™ (Arthrex) sheath with the sharp trocar into the anterolateral portal, which is the primary viewing portal, and withdraw the trocar, and then attach the one-way stop valve to the sheath. Insert the 1.9-mm NanoScope™ (Arthrex) needle arthroscopy system, which is approximately one-third of the size of a standard arthroscopy camera. Connect a 30-cc syringe of sterile 0.9% normal saline to the NanoScope™ (Arthrex) via the one-way stop valve, open the valve, and use all 30 cc to insufflate the joint. This is followed by connecting another 30 cc of sterile saline to the one-way stop valve to inject as needed, while performing a standard diagnostic left knee arthroscopy to identify and assess any intraarticular pathology. In this particular patient, a medial femoral condyle defect is identified. If needed, a 2.0-mm NanoProbe (Arthrex) or other NanoSope™ (Arthrex) instrumentation can be used for both diagnostic and therapeutic treatment. This is inserted into the anteromedial portal, which is the accessory portal. If possible, have an assistant available to provide valgus stress or assist in patient knee positioning, as the arthroscopy is being performed. At the conclusion of the standard diagnostic needle arthroscopy, aspirate as much fluid off the knee as possible through the NanoSope™ (Arthrex), while it remains inserted in the anterolateral portal. Remove the scope and resolve any bleeding by applying pressure with sterile gauze. Apply Steri-Strips to the percutaneous portal sites, followed by gauze and an ACE wrap. The patient may ambulate immediately afterward. Post-procedure antibiotics may be considered