Abstract
Idiopathic granulomatous mastitis (IGM) is a rare inflammatory condition of the breast. IGM is a benign condition, and is more typical in women of child-bearing age, with a recent history of pregnancy and breast feeding. Its clinical presentation can mimic inflammatory breast cancer or breast abscess. The etiology of IGM is not well defined, but proposed to be a localized immune reaction to the breast tissue without the presence of an underlying infectious condition.
Here we report a case of a healthy 35-year-old female, with no story of pregnancy and lactation, who presented with sudden left breast lump, swelling and pain. She underwent first diagnostic ultrasound of the affected breast, then breast MR imaging was performed. A biopsy of the lesion was obtained, which revealed chronic granulomatous inflammation, confirming the diagnosis of GM. Furthermore, the patient was found to have had hyperprolactinemia secondary to a prolactinoma of the pituitary gland (PitNET) many years before, during her 20s, for which she had been treated with surgery.
Keywords: Idiopathic granulomatous mastitis, Breast cancer, Breast abscess, Breast lump, Hyperprolactinemia, Prolactinoma
Abbreviations: IGM,, idiopathic granulomatous mastitis; IBC,, inflammatory breast cancer; MRI,, magnetic resonance imaging; MDAIDS,, mammary duct-associated inflammatory disease sequence; PitNET,, pituitary neuroendocrine tumor
Introduction
Idiopathic granulomatous mastitis (IGM), also known as granulomatous lobular mastitis, is an uncommon, benign and chronic inflammatory condition of the breast. In 1972, Kessler and Wolloch first defined granulomatous mastitis (GM) [1,2]. GM can be idiopathic (primary, IGM) or specific (secondary) [2,3]. Secondary GM is distinguished by caseous necrosis and usually emerges with a variety of infectious conditions such as vasculitis, sarcoidosis, tuberculosis, actinomycosis, and blastomycosis filariasis [2,3]. Entities with similar clinical manifestations also include inflammatory breast cancer (IBC), infective mastitis, foreign body injection granulomas, mammary duct ectasia, diabetic fibrous mastopathy, and systemic granulomatous processes.
IGM is detected in less than 1% of breast biopsies [1,3]. It is also called idiopathic granulomatous lobular mastitis, often seen in women between the second and fourth decade of life, especially pregnant or breast feeding patients. It is definitely rare in men [1]. Gold standard for diagnosis is always histopathology.
This case report involved a 35-year-old woman in good health who received histological diagnosis of GM, with no previous story of child-bearing or breast feeding.
Case presentation
A 35-year-old female in good health presented with sudden left breast redness and pain of about 2 weeks duration. It was not associated with a purulent discharge; the patient had no fever. She denied any current or previous pregnancies, lactation or trauma of the breast. On examination, left breast exam revealed a firm lump of about 1 cm, which was palpable underneath the nipple region. No abnormal findings were noted on the right breast. Axillary examination did not reveal palpable lymph nodes in the left axilla. The patient underwent bilateral breast ultrasound on the same day, and a small hypoechoic, regular limited, solid, and heterogeneous mass of 7 × 4 mm in diameter was found. There were not enlarged lymph nodes in the left axilla at the ultrasound examination (Fig. 1, Fig. 2). The findings were classified under Breast Imaging Reporting and Data System (BI-RADS, fifth edition) assessment category 4 A (abnormality with low suspicion for malignancy, <10%). Biopsy was recommended for differential diagnosis of inflammatory breast cancer.
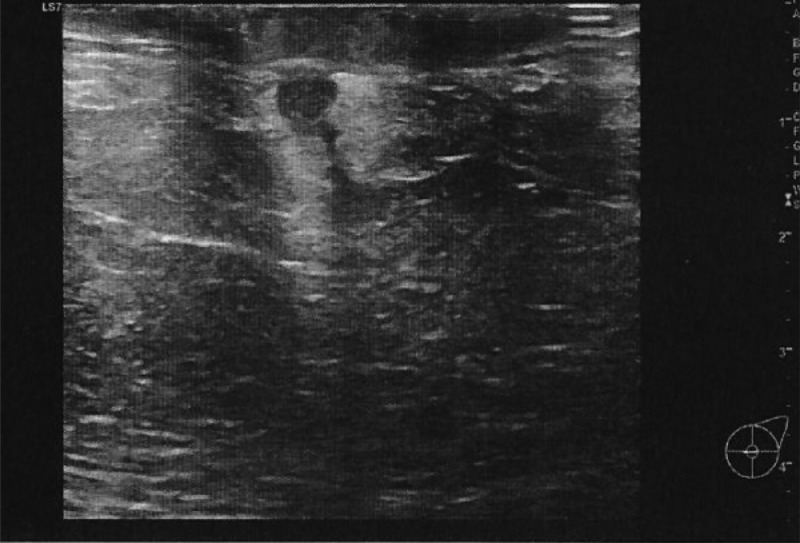
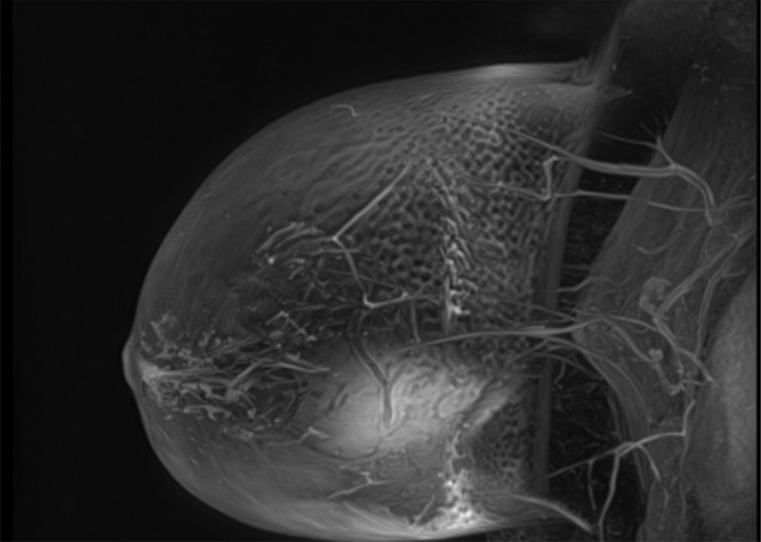
Fig. 1.
A small hypoechoic, regular limited, solid and heterogeneous mass of 7 × 4 mm in diameter was found in the retroareolar region of the left breast at the ultrasound exam. The mass showed a thin linear tract.
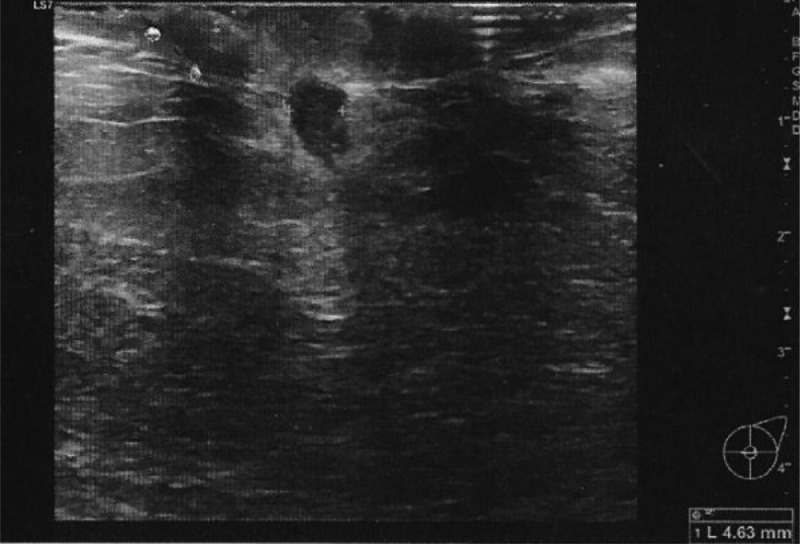
Fig. 2.
The mass had a faint hyperechoic halo, and did not show signs of vascularity at Power Doppler.
She was soon referred to a breast surgeon, in order to do ultrasound-guided core biopsy of the breast, which was performed 5 days after her first presentation. The hystopathologic examination revealed a benign breast tissue with acute and chronic inflammation, and micro abscess formation. Breast magnetic resonance imaging (MRI) was performed 25 days after the breast biopsy, and it demonstrated the presence of a small round “mass-type” lesion with homogeneous enhancement of 8 mm in diameter in the left retroareolar region (Fig. 3, Fig. 4, Fig. 5). The MRI finding was given BI-RADS category 4 B (moderate suspicion for malignancy, >10% to 50%), because of the enhancement time-intensity kinetic curve (type II: progressive contrast enhancement with initial uptake of gadolinium, followed by the plateau phase - plateau pattern). In the case that we report here, medical treatment was not considered for our patient because despite the histological outcome, MRI was still quite concerning. Breast surgeon by agreement with the radiologist decided for surgical excision of the lump, and the hystopatological result was a fibrous tissue-producing subacute-chronic inflammatory process, with aspects of a foreign body-associated giant cell granulomatousis, showing a prevalent periductal disposition (Fig. 6).
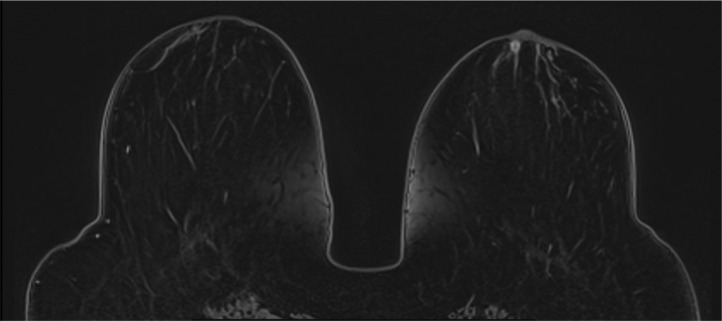
Fig. 3.
Breast MRI demonstrated in axial T1W fat suppressed contrast-enhanced (C–E) dynamic sequences the presence of a small round “mass-type” lesion with homogeneous enhancement of 8 mm in diameter in the left retro-areolar region.
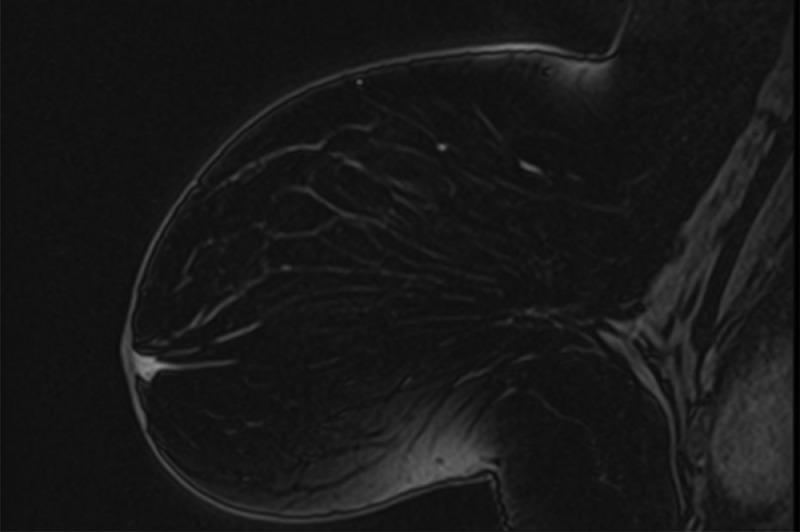
Fig. 4.
Sagittal T1W fat suppressed C-E sequence of the left breast, showing retroareolar enhancing lesion.
Fig. 5.
Sagittal MIP (Maximum Intensity Projection) dynamic sequence of the left breast.
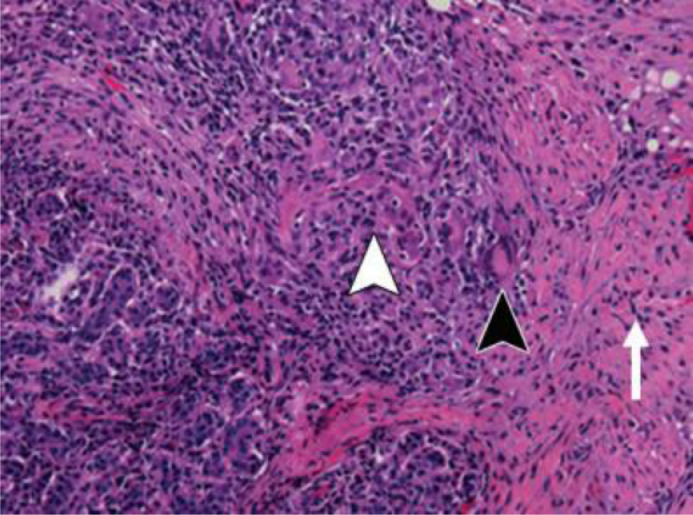
Fig. 6.
Photomicrograph shows the edge of a lobule, with lymphocytic and granulomatous inflammation. A lymphocyte-permeated damaged acinus (white arrowhead) and Langerhans giant cell (black arrowhead) are seen - surrounding fibrosis (arrow) is forming. (Hematoxylin-eosin stain; original magnification, 3400).
The patient revealed that more than ten years earlier, during her 20s, she had undergone the surgical removal of a prolactin-secreting pituitary adenoma (PitNET), which did not relapse afterwards at neuroimaging. So it was decided to perform a new prolactin dosage in this lady, in order to check if some endocrinological imbalances were happening, but the result was negative.
Discussion
Breast lumps or abscesses are common findings in clinical practice. IGM, although rare, must be considered when evaluating an inflammatory condition of the breast, especially in women of child-bearing age (pregnant or breast feeding). An increased incidence in non-white persons has been proposed [15]. The most common clinical manifestation of IGM is a unilateral palpable tender breast mass; it often manifests with abscess formation and cutaneous mild erythema.
The etiology of IGM is not fully understood, but autoimmune and hormonal disorders are often mentioned [2,3]. IGM in fact may appear together with autoimmune disorders such as Sjogren's syndrome, erythema nodosum and arthritis [2,4,5]. Local infection with histoplasma and C. kroppenstedtii has been proposed, as well [6]. Breast trauma, breast feeding, and hyperprolactinemia with galactorrhea are also associated with increased risk of IGM. The most accepted theory is that an initial insult to the ductal epithelial cells in the breast causes a transition of luminal secretions to the lobular stroma. This may cause a local inflammatory response in the connective tissue, with macrophage and lymphocyte migration to the region affected and consequently a local granulomatous response [7]. Multiple inflammatory breast diseases that result from this cascade of events, including IGM, periductal mastitis and mammary duct ectasia, have been suggested to belong to a heterogeneous group of entities, referred to as the mammary duct-associated inflammatory disease sequence (MDAIDS) [8].
Patients with GM and IGM usually present with a painful breast mass which may cause nipple retraction or inversion and fistula formation. The chronicity and lack of response to antibiotics should raise the suspicion for GM. The strategy for radiological imaging of GM and IGM depends on patient's age, clinical manifestations and risk factors. Targeted ultrasonography, mammography, and when the doubt persists MRI, have proven to be mandatory [8,9]. Core-needle biopsy is usually required to exclude IBC and other benign inflammatory breast processes, so that it remains the gold standard in establishing the diagnosis. Due to the possible association between GM and hyperprolactinemia, screening prolactin is recommended, and if elevated can lead to diagnosis and management of pituitary adenoma (pitNET). Corticosteroids and immunosuppressive agents such as methotrexate are very effective in management of IGM, and in majority of cases avoid the need for surgery and potential complications [10]. In the case that we report here, medical treatment was not considered for our patient because despite the histological outcome, MRI was still quite suspicious for malignancy (type II curve - plateau pattern), thus surgical excision was preferred.
A close association between GM and hyperprolactinemia has been reported; also, prolactin levels are important in recurrent cases [11,12]. Prolactin plays a role in the inflammatory pathogenesis of the breast because it has an important place in the proliferation and differentiation of normal breast epithelial tissue and in stimulating lactation after pregnancy. Prolactin levels are thought to be relevant in breast fibrocystic changes, ductal ectasia, benign breast lesions, IGM, and even in the development of breast carcinoma [8]. It has been reported that prolactin antagonist therapies cure IGM successfully when used in the treatment of hyperprolactinemia [13,14]. In the case report that we present here, the patient underwent endocrinologic examination after the surgery, but no hyperprolactinemia was found.
Conclusions
Rare cases of biopsy-proven IGM in nulliparous and nonreproductive patients have been reported, and some of these cases have been attributed to increased levels of prolactin [15,16]. Some patients of course could develop hyperprolactinemia related to the use of antipsychotic agents (ie, risperidone), phenothiazine or metoclopramide. Blunt facial trauma with pituitary gland impairment and PitNETs are also common causes of secondary hyperprolactinemia.
Compared to published literature, unique attributes in our case report are diagnosis of symptomatic GM in a woman who was nulliparous and had a history of previous hyperprolactinemia which was actually very distant in time (more than ten years before the onset of breast symptoms). This is just a single case study, and the occurrence of benign GM in a patient with a story of prolactin-secreting pituitary adenoma treated with surgery many years before, and with normal prolactin dosage at the present time, could certainly represent coincidence somehow. An association between GM and high prolactin levels has been widely proven [15]. There is not much evidence in literature that benign inflammatory breast processes like GM may affect women after many years from the diagnosis and treatment of PitNET. This case study does identify the importance of a full medical history when evaluating sudden breast inflammatory conditions which could simulate breast cancer. Also, it suggests that GM with abscess formation mimicking IBC (inflammatory breast cancer) sometimes might occur even many years after surgical excision of PitNET; this fact prompts us to question if an association between GM and a previous existing prolactin imbalance is possible, although this will need further data and investigation to substantiate.
Patient consent
This is to state that the Patient gives full permission for the publication of the case, and to declare that written informed consent for publication has been obtained from the Patient.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol. 1972;58(6):642–646. doi: 10.1093/ajcp/58.6.642. [DOI] [PubMed] [Google Scholar]
- 2.Fazzio R.T., Shah S.S., Sandhu N.P., Glazebrook K.N. Idiopathic granulomatous mastitis: imaging update and review. Insights into Imaging. 2016;7(4):531–539. doi: 10.1007/s13244-016-0499-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altintoprak F., Kivilcim T., Ozkan O.V. Aetiology of idiopathic granulomatous mastitis. World J Clin Cases. 2014;2(12):852–854. doi: 10.12998/wjcc.v2.i12.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diesing D., Axt-Fliedner R., Hornung D., Weiss J.M., Diedrich K., Friedrich M. Granulomatous mastitis. Arch Gynecol Obstet. 2004;269(4):233–236. doi: 10.1007/s00404-003-0561-2. [DOI] [PubMed] [Google Scholar]
- 5.Destek S., Gul V.O., Ahioglu S. A variety of gene polymorphisms associated with idiopathic granulomatous mastitis. J Surg Case Rep. 2016;2016(9) doi: 10.1093/jscr/rjw156. Article ID rjw156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor GB, Paviour SD, Musaad S, Jones WO, Holland DJ. A clinicopathological review of 34 cases of inflammatory breast disease showing an association between corynebacteria infection and granulomatous mastitis. Pathology. 2003;35(2):109–119. [PubMed] [Google Scholar]
- 7.Need E.F., Atashgaran V., Ingman W.V., Dasari P. Hormonal regulation of the immune microenvironment in 4 Case Reports in Endocrinology the mammary gland. J Mammary Gland Biol Neoplasia. 2014;19(2):229–239. doi: 10.1007/s10911-014-9324-x. [DOI] [PubMed] [Google Scholar]
- 8.Bland KI, Copeland EM. Saunders/Elsevier; Philadelphia, PA: 2009. The breast: comprehensive management of benign and malignant diseases. [Google Scholar]
- 9.Rowe P.H. Granulomatous mastitis associated with a pituitary prolactinoma. Br J Clin Pract. 1984;38(1):32–34. [PubMed] [Google Scholar]
- 10.Benson J.R., Dumitru D. Idiopathic granulomatous mastitis: presentation, investigation and management. Fut Oncol. 2016;12(11):1381–1394. doi: 10.2217/fon-2015-0038. [DOI] [PubMed] [Google Scholar]
- 11.Sakurai K., Fujisaki S., Enomoto K., Amano S., Sugitani M. Evaluation of follow-up strategies for corticosteroid therapy of idiopathic granulomatous mastitis. Surg Today. 2011;41(3):333–337. doi: 10.1007/s00595-009-4292-2. [DOI] [PubMed] [Google Scholar]
- 12.Agrawal A, Pabolu S. A rare case of idiopathic granulomatous mastitis in a nulliparous woman with hyperprolactinemia. Cureus. 2019;11(5):e4680. doi: 10.7759/cureus.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nikolaev A., Blake C.N., Carlson D.L. Association between hyperprolactinemia and granulomatous mastitis. Breast J. 2016;22(2):224–231. doi: 10.1111/tbj.12552. [DOI] [PubMed] [Google Scholar]
- 14.Azlina AF, Ariza Z, Arni T, Hisham AN. Chronic granulomatous mastitis: diagnostic and therapeutic considerations. World J Surg. 2003;27(5):515–518. doi: 10.1007/s00268-003-6806-1. [DOI] [PubMed] [Google Scholar]
- 15.Pluguez-Turull CW, Nanyes JE, Quintero CJ, Alizai H, Mais DD, Kist KA, et al. Idiopathic granulomatous mastitis: manifestations at multimodality imaging and pitfalls. Radiographics. 2018;38(2):330–356. doi: 10.1148/rg.2018170095. [DOI] [PubMed] [Google Scholar]
- 16.Aghajanzadeh M, Hassanzadeh R, Alizadeh Sefat S, Alavi A, Hemmati H, Esmaeili Delshad MS, et al. Granulomatous mastitis: presentations, diagnosis, treatment and outcome in 206 patients from the north of Iran. Breast. 2015;24(4):456–460. doi: 10.1016/j.breast.2015.04.003. [DOI] [PubMed] [Google Scholar]