Abstract
Horizontal cleavage tears (HCTs) are challenging meniscal tear patterns, as they split the meniscus into inferior and superior leaflets, while also involving the central, less vascular portions of the meniscus. Circumferential compression sutures using an all-inside self-retrieving suture passing device like the Novostitch Pro (Smith & Nephew, Andover, MA) have demonstrated the ability to create stable repair constructs with uniform compression across both leaflets in the setting of HCTs. Additionally, biological augmentation of meniscal repairs using a marrow venting procedure (MVP) has demonstrated superior clinical outcomes relative to isolated meniscal repairs. Thus, the purpose of this technical note is to outline our procedure for implementing circumferential compression sutures and biologic augmentation using an MVP for repairing an HCT of the lateral meniscus.
Technique Video
In this technical note, we describe our procedure for implementing a right knee circumferential compression suture configuration and biologic augmentation using a marrow venting procedure for repairing a horizontal cleavage tear of the lateral meniscus.
Introduction
Horizontal cleavage tears (HCTs) split the meniscus into superior and inferior leaflets and disrupt both the vascular periphery and the avascular central portions of the meniscus.1,2 While nonoperative treatment may be a reasonable option for small HCTs with minimal symptoms, symptomatic HCT patterns have traditionally been treated with arthroscopic partial meniscectomy.3 Recent evidence has demonstrated that resection of meniscal tissue can directly impact joint biomechanics and longevity.4,5 For example, while a single leaflet resection can create a stable construct, relieve symptoms, and preserve meniscal tissue, it still leads to a decrease in contact area and an increase in contact pressures that can be equivalent to a dual leaflet resection.6,7 However, when a HCT undergoes repair, contact pressures within the affected compartment are restored to normal, physiological levels.7 As a result, there has been a growing trend to preserve the meniscus, whenever possible, given its critical role in preventing the progression of osteoarthritis and its role in maintaining knee stability, load distribution, and physiological kinematics.4
HCTs can be challenging to repair due to their orientation, intrameniscal location, and involvement of relatively avascular portions of the meniscus.8 Historically, tears involving the central zones of the meniscus had been treated with resection due to the belief that these regions have poor intrinsic healing potential. A recent study by Chahla et al. has demonstrated that the central white-white zone of the meniscus has intrinsic vascularization, as well as a resident mesenchymal progenitor cell population.5 A study by Cinque et al. translated these results to the clinical setting and demonstrated a significant subjective clinical improvement for meniscal repair of tears involving the white-white zone.9 The results of these studies would suggest that the central regions of the meniscus may have better healing potential than previously thought.
Healing of an HCT meniscal repair is highly dependent on stability of the repair, compression across the defect, and vascular supply to the repair site. Over time, this has led to the development and application of various anatomic reduction principles, biologic augmentation techniques, and optimized repair constructs for this complex injury pattern. Prominent examples of this include the implementation of circumferential compression sutures and biologic augmentation through marrow venting procedures (MVP). Circumferential compression suture configurations have demonstrated an ability to create stable HCT repairs with uniform compression across the torn leaflets, unlike conventional all-inside anchor-based devices, which fail to compress the leaflets together.4,10 Additionally, augmentation with marrow venting has demonstrated the ability to improve HCT repair clinical outcomes.11,12 Thus, the purpose of this article is to outline our technique for repair of a HCT of the lateral meniscus using an all-inside suture passing device to place circumferential compression sutures followed by subsequent biologic augmentation of the repair using an MVP (Video 1).
Surgical Technique
Patient Setup
After the induction of general anesthesia, the patient is positioned supine with padding posterolateral to the thigh. Alternatively, the operative limb can be placed in a leg holder. The post provides a fulcrum for valgus force applied when addressing the medial compartment. A pneumatic tourniquet is placed and secured on the proximal thigh, and draping is performed in standard sterile fashion.
Arthroscopic Access
Arthroscopic access to the knee joint is obtained in a standard fashion. Optimized portal placement is essential to ensure adequate access without damaging the articular cartilage. The anterolateral portal is placed first, followed by the anteromedial portal under direct arthroscopic visualization. An anteromedial portal placed too proximally will prevent access to the posterior aspect of the joint due to obstruction of the instruments by the femoral condyle, while a low portal will direct the instruments upward as they collide with the tibial spines. Additionally, a low anteromedial portal puts the anterior medial meniscal root at risk.
An arthroscopic probe is used to identify tear configuration, extent, and stability. Because of the commonly degenerative nature of a HCT, there is frequently a complex tear pattern with associated fraying, a meniscal flap, or radial components (Fig 1).
Fig 1.
Tear of the lateral meniscus of the right knee. (A) Magnetic resonance imaging T2-coronal cut revealing a horizontal cleavage tear in the body of the lateral meniscus (white arrow) with associated meniscal parameniscal cyst (black arrow). (B) Initial arthroscopic visualization of the complex meniscal tear, with a small incomplete radial tear and an incomplete vertical tear on the upper surface of the meniscus. (C) Horizontal cleavage tear. (D) Tear site preparation with arthroscopic rasp (Smith & Nephew, Andover, MA), while viewing from the standard anterolateral portal and using the standard anteromedial portal as a working portal for instrumentation. For this lateral sided injury, the patient is placed in a figure-of-four position, paired with a slightly higher anteromedial portal in order to provide safe access to the posterior horn and midportion of the lateral meniscus.
Once the intra-articular pathology is initially verified, adequate space for thorough visualization and safe instrumentation must be ensured. For medial sided injuries, a medial cruciate ligament (MCL) “pie-crust” release is often necessary when approaching the posterior horn of the medial meniscus to ensure adequate visualization and access. For lateral sided injuries, a figure-of-four position, paired with a slightly higher anteromedial portal will provide safe access to the posterior horn and midportion of the lateral meniscus.
Tear Preparation
The frayed inner margins of the meniscus should be trimmed. Tear preparation is undertaken with an arthroscopic rasp (Smith & Nephew, Andover, MA) or shaver (DYONICS; Smith & Nephew). Care must be taken not to resect viable meniscal tissue so that the viability of the final construct is not compromised.
Meniscal Repair
Repair is performed with circumferential compression stitches, which allow for anatomic approximation and subsequent compression of the meniscal leaflets (Fig 2). This is done using the self-passing all-inside Novostitch Pro device (Smith & Nephew, Andover, MA). It is the senior author’s opinion that it is technically easier to maneuver the tip of the device without the constraint of an arthroscopic cannula. Conversely, at this point, a hemostat can be used to spread the capsular opening of the portal in order to minimize the risk of a soft tissue bridge during instrument passage and knot tying.
Fig 2.
Repair of a lateral meniscus tear of the right knee. The arthroscopic camera is inserted from the standard anterolateral portal, and the standard anteromedial portal is used as a working portal for instrumentation. For this lateral sided injury, the patient is placed in a figure-of-four position, in order to provide access to the posterior horn and midportion of the lateral meniscus. (A) The self-passing all-inside suture device is preloaded with 2-0 high-strength, nonabsorbable suture (Novostitch Pro; Smith & Nephew, Andover, MA) and is introduced into the joint with the lower jaw in the retracted position and the upper jaw in the horizontal, low-profile configuration. This is done for atraumatic insertion through the working anteromedial portal. The front, orange trigger is squeezed during introduction to maintain the upper jaw in this position. Upon accessing the site of the horizontal cleavage tear, the front trigger is released enough to elevate and place the upper jaw of the device on the femoral surface of the meniscus. The lower jaw is then protracted by activating the thumb lever on the side of the device, placing it between the tibial articular surface and the lower surface of the meniscus. (B) The suture is passed by pressing the posterior trigger of the all-inside suture device. The suture is passed using a minimally traumatic needle, through the meniscal tissue, and into the upper jaw, where it is self-captured. At the time of suture passage, the entire device should be gently driven toward the periphery of the meniscus as to prevent the meniscal tissue from extruding from the jaws of the device. (C) An arthroscopic knot is tied, followed by additional alternated half-stitches to complete the suture construct. Suture limbs are cut with a dedicated cutter. (D) Sequential stitching of the meniscus along the entire tear is performed until probing demonstrates adequate construct stability. Using a probe, knots should then be pushed toward the joint periphery to avoid knot placement in the meniscofemoral interface and prevent possible meniscal and/or cartilage injury.
The device is preloaded with 2-0 high-strength, nonabsorbable suture and is introduced into the joint with the lower jaw in the retracted position and the upper jaw in the horizontal, low-profile configuration. This is done for atraumatic insertion through the working portal. The front, orange trigger is squeezed during introduction to maintain the upper jaw in this position. Upon accessing the site of the horizontal cleavage tear, the front trigger is released enough to elevate and place the upper jaw of the device on the femoral surface of the meniscus. The lower jaw is then protracted by activating the thumb lever on the side of the device, placing it between the tibial articular surface and the lower surface of the meniscus. Once the device is adequately placed with the aiming laser marking toward the periphery of the meniscus, the suture is passed by pressing the posterior trigger of the device. The Novostitch Pro (Smith & Nephew, Andover, MA) will pass the suture using a minimally traumatic needle, through the meniscal tissue, and into the upper jaw, where it is self-captured. At the time of suture passage, the entire device should be gently driven toward the periphery of the meniscus as to prevent the meniscal tissue from extruding from the jaws of the device. The device is retrieved from the joint and an arthroscopic knot is tied, followed by additional alternated half-stitches to complete the suture construct. Suture limbs are cut with a dedicated cutter. Sequential stitching of the meniscus along the entire tear is performed until probing demonstrates adequate construct stability. A single disposable device is used for placing additional circumferential stiches by merely reloading it with new high-strength suture cartridges. Using a probe, knots should then be pushed toward the joint periphery as to avoid knot placement in the meniscofemoral interface in order to prevent possible meniscal and/or cartilage injury.
When using the Novostitch Pro device (Smith & Nephew, Andover, MA), an HCT repair is carried out by deploying a single peripheral pass of suture, which is subsequently tied and cut for each circumferential stich. For other tear patterns, the technique must be modified. Vertical tears require that the second end of the suture be threaded back into the device, which is passed through the tissue once more to complete the desired suture configuration.13 Alternatively, a single suture or a double-locking loop suture can be threaded down a bone tunnel for transtibial repair of root or radial tears.14
Bone Marrow Venting Procedure
Once the meniscal repair is completed, biological augmentation can now be pursued. Attention is turned to the intercondylar notch. With the use of a microfracture awl, 4 to 5 holes in the lateral aspect of the intercondylar notch are created. These holes are anterior to the femoral origin of the anterior cruciate ligament (ACL) and allow for bone marrow elements to leak into the joint space. This marrow venting procedure provides a biologically enriched environment that promotes meniscal healing (Fig 3). Leakage of bone marrow products must be visually confirmed to ensure adequate marrow venting. If no leakage is initially observed, irrigation of the joint may be temporarily stopped to diminish the intra-articular pressure and confirm successful venting. Suction can also be used to provide negative pressure.
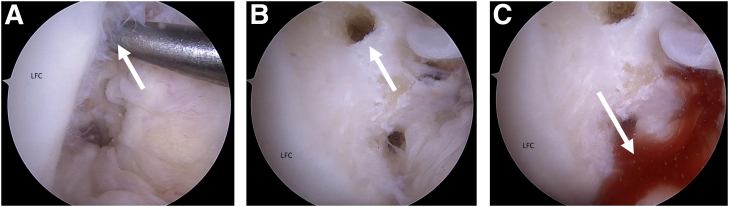
Fig 3.
Bone marrow-venting procedure of the right knee. The arthroscopic camera is inserted from the standard anterolateral portal, and the standard anteromedial portal is used as a working portal for instrumentation. (A) Anterolateral portal view of microfracture awl position on the lateral aspect of the intercondylar notch. (B) Anteromedial portal view of three perforations, which are anterior to the femoral origin of the anterior cruciate ligament (ACL) and allow for bone marrow elements to leak into the joint space. This marrow venting procedure provides a biologically enriched environment that promotes meniscal healing; (C) leakage of bone marrow products must be visually confirmed to ensure adequate marrow venting. If no leakage is initially observed, irrigation of the joint may be temporarily stopped to diminish the intra-articular pressure and confirm successful venting. LFC, lateral femoral condyle.
Rehabilitation
Physical therapy is initiated on postoperative day 1 with an early emphasis on quadriceps activation and assisted range of motion exercises in the range of 0° to 90°. Patients who undergo HCT repair will be partial weight-bearing with the use of crutches for 2 weeks, at which point they progress to weight-bearing, as tolerated with incremental progression. Deep squatting and heavy lifting should be avoided until 4 months postoperatively. Rehabilitation protocols can vary depending on meniscal tear patterns and associated procedures, such as ligament reconstruction, cartilage repair, or osteotomy.
Indications and Contraindications
Candidates for HCT repair are young adults with persistently symptomatic tears that did not improve with conservative treatment; these patients should not have significant instability or osteoarthritis.3,4 Contraindications to HCT repair include diffuse cartilage lesions, advanced osteoarthritis, and a patient unwilling to comply with the rehabilitation protocol. Although there is not a defined threshold precluding repair, increasing age generally leads to inferior outcomes as do degenerative tears when compared to acute, traumatic tears.15,16
Discussion
HCTs of the lateral meniscus have historically been treated surgically via leaflet resection; however, it has been demonstrated that these interventions resulted in increased mean and peak pressures within the joint.6,17,18 As a result, more consideration has been placed on repair for this injury pattern. Although there has been well documented evidence supporting repair of this tear pattern, there are historic concerns due to the technical difficulty of the operation in conjunction with presumed poor healing rates. Nevertheless, a systematic review performed by Kurzweil et al. indicated that not only did HCT repair have satisfactory clinical outcomes, but repair of HCT had comparable success rates relative to other commonly repaired meniscal tear patterns.15 As there has been a growing interest to repair HCTs, recent efforts to optimize outcomes for HCT repair have revolved around creating a stable repair construct and implementing biologic adjuvants to augment healing.
Anatomic coaptation and uniform compression are essential for satisfactory meniscal healing. Circumferential compression stitches have been used to produce stable repair constructs that optimize healing for challenging injury patterns like HCTs. Circumferential compression using an all-inside self-retrieving suture-based device like the Novostitch Pro (Smith & Nephew, Andover, MA) allows for uniform compression between the superior and inferior leaflets and facilitates a stable, anatomic repair across the defect.4 When compared to inside-out repairs, circumferential compression stitches placed with the Novostitch device (Smith & Nephew, Andover, MA) demonstrated lower displacement (gap formation) at high cyclic loading.19 Moreover, circumferential compression stitches have demonstrated the highest load to failure of all meniscus repair patterns.19,20 Subsequent cadaveric testing has also demonstrated that circumferential compression stitches of HCTs return tibiofemoral contact pressures to near normal-normal levels.21 These biomechanical results have successfully translated to the clinical setting. A 2021 prospective, multicenter trial by Kurzweil et al. demonstrated the viability of using the Novostitch device (Smith & Nephew, Andover, MA) for HCTs.22 The authors concluded that circumferential compression sutures using the Novostitch device (Smith & Nephew, Andover, MA) is appropriately indicated for repairing HCTs.
Beyond these biomechanical and clinical benefits, all-suture repair circumvents some of the shortcomings of traditional all-inside anchor-based devices. Overpenetration of the capsule during suture passage with traditional devices can lead to neurovascular damage or entrapment, while all-suture self-passing devices avoid this as they rely on knots instead of implants for fixation.13 Additionally, suture-based devices eliminate implant pull-through as a mode of failure for repairs and also eliminate implant-related complications.19,23,24 On the other hand, there is a distinct possibility of knot-slippage as a mode of failure. As a consequence, there is an increased importance of secure knot tying when using these devices.19 Suture-based repair also decreases the risk of possible iatrogenic meniscal extrusion and consequent intra-articular shrinkage of the functional meniscal surface inherent to repairs that rely on capsular stiches (inside-out, anchor-based all-inside).13 Furthermore, a recent study by Kinoshita et al. reported that circumferential repair results in lower formation of meniscal cysts postoperatively relative to anchor-based all-inside repair (5.56% versus 26.4%, respectively).25
In addition to optimizing stability of the repair and compression across the defect, there has also been a growing interest in the use of biologic augmentation tactics to drive chemotaxis, cellular proliferation, and matrix production in an attempt to improve healing at the site of the repair.5 The marrow venting procedure (MVP) is an adjunctive biological technique that aims to create a favorable healing environment through the intra-articular release of peptides, growth factors, and pluripotent cells from the bone marrow.11,26 Unlike other biologic augments like platelet-rich-plasma (PRP) or bone marrow aspirate concentrate (BMAC), marrow venting does not require a peripheral blood draw or harvest. Additionally, PRP and BMAC have been reported to have inconsistent preparation.27,28
Marrow venting was developed after superior outcomes were observed in meniscal repairs done concurrently with ACL reconstructions compared to isolated repair. The theoretical benefit was attributed to the release of biologic factors during tunnel drilling. In the setting of a surgically repaired HCT, an adjunct MVP has the potential to promote tissue repair and improve patient outcomes through similar mechanisms.11 A promising prospective clinical study by Dean et al. demonstrated that inside-out meniscal repair augmented with an MVP had comparable outcomes to meniscal repair with concomitant ACL reconstruction.11 A randomized controlled trial echoed these findings and reported that at 36-month follow up, MVP-augmented repair groups exhibited a 100% healing rate with superior patient-reported outcomes in comparison to isolated meniscal repair (76% healing rate).29 Finally, a retrospective case series specifically examining HCT repairs augmented with a MVP demonstrated a 91% healing rate in clinic.12
The present technique has several advantages relative to all-inside repair and inside-out repair of HCTs. The use of circumferential compression stitches allows for a uniform compression across both leaflets with a biomechanically stronger construct. Additionally, the technique is technically simple and uses a self-passing suture device to aid in passing of the sutures without placing the neurovascular structures at risk. Augmentation with an MVP allows for improved meniscal healing, as it creates a local environment that is similar to meniscus repair in the setting of ACL reconstruction (Tables 1 and 2).
Table 1.
Advantages and Disadvantages of Using an MVP for ACL Tears
| Advantages | Disadvantages |
|---|---|
| Provides uniform compression from top down across the torn leaflets (reduced gapping, higher load to failure) | Potential risk of suture loosening due to improper knot-tying |
| Eliminates the risk of neurovascular complications from overpenetration of implant-based devices or from inside-out repair | Suboptimal for repair of meniscocapsular vertical separation30 |
| Eliminates the risk of implant-related complications (e.g., pull-through, migration, loose body in the joint) | Increased cost in comparison to inside-out repair. |
| Decreased risk of iatrogenic meniscal extrusion (versus implant-based all-inside devices or inside-out repair) | |
| Decreased risk of postoperative meniscal cyst formation (versus implant-based all-inside devices) | |
| Versatility allows for repair of vertical, radial, root, horizontal, and complex tear patterns |
Table 2.
Pearls and Pitfalls of Using an MVP for ACL Tears
| Pearls | Pitfalls |
|---|---|
|
|
|
|
|
|
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C. reports being a paid consultant for Arthrex, CONMED Linvatec, Ossur, and Smith & Nephew; he is a board or committee member of the American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
In this technical note, we describe our procedure for implementing a right knee circumferential compression suture configuration and biologic augmentation using a marrow venting procedure for repairing a horizontal cleavage tear of the lateral meniscus.
References
- 1.Sallé de Chou E., Pujol N., Rochcongar G., et al. Analysis of short and long-term results of horizontal meniscal tears in young adults. Orthop Traumatol Surg Res. 2015;101:S317–S322. doi: 10.1016/j.otsr.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Mordecai S.C., Al-Hadithy N., Ware H.E., Gupte C.M. Treatment of meniscal tears: An evidence based approach. World J Orthop. 2014;5:233–241. doi: 10.5312/wjo.v5.i3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kurzweil P.R. Treatment of horizontal cleavage tears—Resection to repair. Oper Tech Sports Med. 2018;26:271–278. [Google Scholar]
- 4.Woodmass J.M., Johnson J.D., Wu I.T., Saris D.B.F., Stuart M.J., Krych A.J. Horizontal cleavage meniscus tear treated with all-inside circumferential compression stitches. Arthrosc Tech. 2017;6:e1329–e1333. doi: 10.1016/j.eats.2017.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chahla J., Papalamprou A., Chan V., et al. Assessing the resident progenitor cell population and the vascularity of the adult human meniscus. Arthroscopy. 2021;37:252–265. doi: 10.1016/j.arthro.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haemer J.M., Wang M.J., Carter D.R., Giori N.J. Benefit of single-leaf resection for horizontal meniscus tear. Clin Orthop Relat Res. 2007;457:194–202. doi: 10.1097/BLO.0b013e3180303b5c. [DOI] [PubMed] [Google Scholar]
- 7.Koh J.L., Yi S.J., Ren Y., Zimmerman T.A., Zhang L.Q. Tibiofemoral contact mechanics with horizontal cleavage tear and resection of the medial meniscus in the human knee. J Bone Joint Surg Am. 2016;98:1829–1836. doi: 10.2106/JBJS.16.00214. [DOI] [PubMed] [Google Scholar]
- 8.Beaufils P., Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017;103:S237–S244. doi: 10.1016/j.otsr.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Cinque M.E., Dephillipo N.N., Moatshe G., et al. Clinical outcomes of inside-out meniscal repair according to anatomic zone of the meniscal tear. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119860806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks K.R. Vertical lasso and horizontal lasso sutures for repair of horizontal cleavage and horizontal oblique meniscal tears: Surgical technique and indications. Arthroscopy Tech. 2017;6:e1767–e1773. doi: 10.1016/j.eats.2017.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dean C.S., Chahla J., Matheny L.M., Mitchell J.J., Laprade R.F. Outcomes after biologically augmented isolated meniscal repair with marrow venting are comparable with those after meniscal repair with concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:1341–1348. doi: 10.1177/0363546516686968. [DOI] [PubMed] [Google Scholar]
- 12.Ahn J-Hmdpd, Kwon O-Jmd, Nam T-Smdpd. Arthroscopic repair of horizontal meniscal cleavage tears with marrow-stimulating technique. Arthroscopy. 2015;31:92–98. doi: 10.1016/j.arthro.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 13.Saliman J.D. The circumferential compression stitch for meniscus repair. Arthroscopy Tech. 2013;2:e257–e264. doi: 10.1016/j.eats.2013.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blackman A.J., Stuart M.J., Levy B.A., McCarthy M.A., Krych A.J. Arthroscopic meniscal root repair using a Ceterix NovoStitch suture passer. Arthrosc Tech. 2014;3:e643–e646. doi: 10.1016/j.eats.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurzweil P.R., Lynch N.M., Coleman S., Kearney B. Repair of horizontal meniscus tears: A systematic review. Arthroscopy. 2014;30:1513–1519. doi: 10.1016/j.arthro.2014.05.038. [DOI] [PubMed] [Google Scholar]
- 16.Tengrootenhuysen M., Meermans G., Pittoors K., van Riet R., Victor J. Long-term outcome after meniscal repair. Knee Surg Sports Traumatol Arthrosc. 2011;19:236–241. doi: 10.1007/s00167-010-1286-y. [DOI] [PubMed] [Google Scholar]
- 17.Atsumi S., Hara K., Arai Y., et al. A novel arthroscopic all-inside suture technique using the Fast-Fix 360 system for repairing horizontal meniscal tears in young athletes: 3 case reports. Medicine (Baltimore) 2018;97:e9888. doi: 10.1097/MD.0000000000009888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baratz M.E., Fu F.H., Mengato R. Meniscal tears: The effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 19.Masoudi A., Beamer B.S., Harlow E.R., et al. Biomechanical evaluation of an all-inside suture-based device for repairing longitudinal meniscal tears. Arthroscopy. 2015;31:428–434. doi: 10.1016/j.arthro.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 20.Aşík M., Sener N. Failure strength of repair devices versus meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc. 2002;10:25–29. doi: 10.1007/s001670100247. [DOI] [PubMed] [Google Scholar]
- 21.Beamer B.S., Walley K.C., Okajima S., et al. Changes in contact area in meniscus horizontal cleavage tears subjected to repair and resection. Arthroscopy. 2017;33:617–624. doi: 10.1016/j.arthro.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Kurzweil P., Krych A.J., Anz A., et al. Favorable reoperation rate at 2 years following repair of horizontal cleavage tears using an all suture-based technique: A prospective, multicenter trial. Arthrosc Sports Med Rehabil. 2021;3:e773–e780. doi: 10.1016/j.asmr.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aros B.C., Pedroza A., Vasileff W.K., Litsky A.S., Flanigan D.C. Mechanical comparison of meniscal repair devices with mattress suture devices in vitro. Knee Surg Sports Traumatol Arthrosc. 2010;18:1594–1598. doi: 10.1007/s00167-010-1188-z. [DOI] [PubMed] [Google Scholar]
- 24.Malinowski K., Góralczyk A., Hermanowicz K., LaPrade R.F. Tips and pearls for all-inside medial meniscus repair. Arthrosc Tech. 2019;8:e131–e139. doi: 10.1016/j.eats.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kinoshita T., Hashimoto Y., Nishino K., Nishida Y., Takahashi S., Nakamura H. Comparison of new and old all-inside suture devices in meniscal cyst formation rates after meniscal repair. Int Orthop. 2022;46:1563–1571. doi: 10.1007/s00264-022-05375-4. [DOI] [PubMed] [Google Scholar]
- 26.LaPrade C.M., James E.W., LaPrade R.F., Engebretsen L. How should we evaluate outcomes for use of biologics in the knee? J Knee Surg. 2015;28:35–44. doi: 10.1055/s-0034-1390028. [DOI] [PubMed] [Google Scholar]
- 27.Chahla J., Cinque M.E., Piuzzi N.S., et al. A call for standardization in platelet-rich plasma preparation protocols and composition reporting: A systematic review of the clinical orthopaedic literature. J Bone Joint Surg Am. 2017;99:1769–1779. doi: 10.2106/JBJS.16.01374. [DOI] [PubMed] [Google Scholar]
- 28.LaPrade R.F., Chahla J. Elsevier; St. Louis, MO: 2021. Evidence-based management of complex knee injuries: Restoring the anatomy to achieve best outcomes. [Google Scholar]
- 29.Kaminski R., Kulinski K., Kozar-Kaminska K., Wasko M.K., Langner M., Pomianowski S. Repair augmentation of unstable, complete vertical meniscal tears with bone marrow venting procedure: A prospective, randomized, double-blind, parallel-group, placebo-controlled study. Arthroscopy. 2019;35:1500–1508. doi: 10.1016/j.arthro.2018.11.056. e1501. [DOI] [PubMed] [Google Scholar]
- 30.Foissey C., Thaunat M., Fayard J.-M. All-inside double-sided suture repair for longitudinal meniscal tears. Arthrosc Tech. 2021;10:e2043–e2048. doi: 10.1016/j.eats.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In this technical note, we describe our procedure for implementing a right knee circumferential compression suture configuration and biologic augmentation using a marrow venting procedure for repairing a horizontal cleavage tear of the lateral meniscus.
In this technical note, we describe our procedure for implementing a right knee circumferential compression suture configuration and biologic augmentation using a marrow venting procedure for repairing a horizontal cleavage tear of the lateral meniscus.