Abstract
Purpose
Because of the inaccuracy of the biparietal diameter in cases with an engaged fetal head in the pelvis, measuring the estimated fetal weigh (EFW) using Hadlock’s formula could be compromised in these cases. The aim of this prospective study is to determine the accuracy of using only two thigh parameters, the femur length (FL) and the cross-sectional area of the thigh (CSAT) (Isobe’s formula), in detecting the fetal weight of both engaged pelvis fetuses and non-engaged head fetuses and to compare this method with Hadlock’s formula in both groups using the actual birth weight as a gold standard.
Methods
The study included 51 cases with an engaged fetal head and 51 cases with a non-engaged fetal head that came in active labour. 2D ultrasonography examination was performed to determine the EFW using both Hadlock’s formula and Isobe’s formula. The EFW was then compared with the actual birth weight after delivery.
Results
There was a strong positive correlation between Isobe’s formula and the actual birth weight in the engaged fetal head group (r = 0.993, p < 0.01), but there was a strong positive correlation between Hadlock’s formula and the actual birth weight in the non-engaged fetal head group (r = 0.994, p < 0.01).
Conclusion
We concluded that Isobe’s formula is convenient in predicting the fetal weight, especially when head measurements are difficult to assess (in the engaged fetal head group). It can be used with 2D ultrasonography as an alternative to Hadlock’s formula in cases with an engaged fetal head in the pelvis.
Keywords: Hadlock’s formula, Isobe’s formula, Fetal weight, Ultrasonography, Engaged fetal head
Background
In the process of antenatal care, ultrasonographic assessment of fetal weight is mandatory for detecting fetuses that are appropriately grown, small and large for gestational age (AGA, SGA, and LGA, respectively). The estimation of fetal weight is important for the management of labour and for the determination of a suitable mode of delivery. The estimated fetal weight (EFW) is measured by four parameters: the fetal head circumference (HC), biparietal diameter (BPD), femur length (FL), and abdominal circumference (AC) [1].
Hadlock’s formula is one of the commonly used formulas for estimating fetal weight, including measurements of the HC, AC, FL, and BPD alone and in combination [2].
The accuracy of the fetal biparital diameter is uncertain in conditions such as an engaged fetal head and breech presentation and for fetuses in direct occipito-anterior or occipito-posterior position. The estimation of fetal weight using only two fetal thigh dimensions, as in Isobe’s formula, could be used to avoid these situations [2, 3].
In this comparative study, we aimed to determine the accuracy of using only two thigh parameters, the femur length and the cross-sectional area of the thigh (CSAT) (Isobe’s formula), in detecting the fetal weight of both engaged pelvis fetuses and non-engaged head fetuses and to compare this method with Hadlock's formula in both groups using the actual birth weight as a gold standard.
Methods
The current study has been approved by the Research and Ethical Committee of Kasr El-Aini Hospital.
The study population included 102 mothers with singleton term pregnancy in cephalic presentation at term (37–40 weeks of gestation) and who came in active labour to the labour room between February 2020 and May 2021 and delivered within the next 24 h.
In total, 82 patients had a vaginal delivery, and only 20 patients underwent a caesarean section due to an obstetric cause.
Two groups of patients were included in this study:
-
The first group included 51 cases with an engaged fetal head in the pelvis.
The fetal head is considered “engaged” when the largest part of the head (BPD) has entered the pelvis (at the level of the ischial spines – station zero). If the presenting part lies above the ischial spines, the station is reported as a negative number (not considered to be engaged).
The second group included 51 cases with a non-engaged fetal head in the pelvis.
All the patients were examined by an expert obstetrician to determine the engagement of the head and to decide the mode of delivery.
The patients were then subjected to two-dimensional ultrasonography examinations to estimate the fetal weight using the well-established Hadlock and Isobe formulas.
After delivery, the actual birth weight was then measured to compare it with the EFW detected by the two formulas.
The cases included in this study were only those with an average fetal weight for gestational age (2.5–4 kg).
Patients with fetal malpresentation, multiple pregnancies, and oligohydramnios were excluded from the study because the exact fetal thigh circumference is difficult to obtain in these patients owing to the blurring of the echographs and the deformation of the fetal thigh circumference under compression. Preterm babies and fetuses with growth abnormalities were also excluded from the study.
Technique of the examination
The patients were examined using a LOGIQ P6, GE (General Electric) ultrasound machine equipped with a 5-MHz transducer. Examinations were performed by two consultant radiologists experienced in fetal ultrasound (more than 10 years’ experience).
Each fetus was examined on a single occasion. Gestational age was determined from the last menstrual period and confirmed by ultrasound; it was given in exact number of weeks (37–40 weeks). The patient lied in a flat position, and after good exposure a conducting gel was applied. First, a rapid overview was performed to confirm positive fetal life and longitudinal lie. Cephalic presentation head parameters, such as bi parital diameter and HC, were measured, as well as abdominal circumference, femur length and cross sectional area of the thigh. Amniotic fluid was assessed using the amniotic fluid index method by dividing the abdomen into four quadrants and then measuring amniotic fluid pockets in each quadrant.
BPD is measured from the outer edge of the proximal parietal bone to the inner edge of the distal parietal bone (outer to inner) at the level of the widest part of the fetal skull [4].
FL measurement includes the ossified portion of the diaphysis and metaphysis. Although the proximal and distal epiphyseal cartilages should not be measured, they should be visualized to ensure that the entire osseous femur is measured without shortening or elongation [4].
AC is measured at the level of the stomach bubble and a short segment of the umbilical vein at the level of the portal sinus using the ellipse facility of the ultrasound imaging [4].
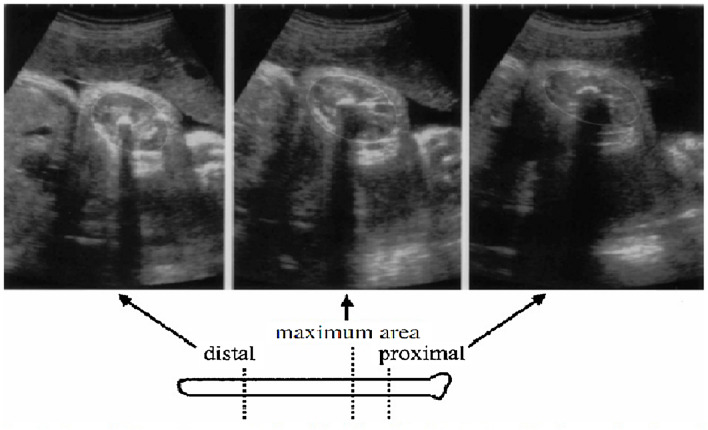
The CSAT is defined as the cross-sectional area of the muscles and bones of the thigh on the plane at a right angle to the long axis of the femur, where the area is the largest. The CSAT was measured as follows. The fetal thigh circumference was recorded at a transverse plane at the junction of the upper and middle thirds of the thigh, at the level of the proximal nutrient foramen of the femur (Fig. 1) [5]. Measurements made within 1–2 cm of the transition plane were quite similar, demonstrating that exact positioning of the plane is not necessary. At the point where the cross-sectional area of the thigh reached its maximum, the probe motion was stopped. The area was then measured using the HC and AC ellipse function.
Fig. 1.
Sonographic views of the cross sectional area of the thigh at right angles to the long axis in the proximal, maximum and distal portions. Isobe [5]
Then the estimated fetal body weight was calculated as follows:
Using Hadlock's formula: calculated by the machine software using the BPD, HC, AC, and FL parameters.
Using Isobe's formula: calculated using FL and CSAT:
where FL is in millimeters and CSAT is in centimetres. The actual birth weight (ABW) of the infant was measured immediately after delivery and after clamping the umbilical cord at an equal distance (7 cm) in every baby.
Statistical methods
Data were coded and entered using the Statistical Package for the Social Sciences (SPSS) version 26 (IBM Corp., Armonk, NY, USA). The data were summarized using the mean, standard deviation, median, minimum, and maximum for quantitative variables and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between groups were made using an unpaired t-test. Comparisons with the actual weight in each group were carried out using a paired t-test. For comparing categorical data, a chi-square test was performed. An exact test was used instead when the expected frequency was less than 5. Correlations between quantitative variables were calculated using Pearson’s correlation coefficient; p values less than 0.05 were considered statistically significant.
We used the following terms:
Error: the difference between the EFW (by either formula) and the actual birth weight.
Absolute error: the absolute value of the error.
Absolute error percentage: the absolute error divided by the actual birth weight as percentage. The accepted range was 10% of the actual birth weight.
The actual birth weight was considered the gold standard in our study.
Results
This study was carried out on 102 patients referred to us from the emergency department between February 2020 and May 2021; their age ranged from 22 to 42 years (mean age 31). The gestational age of the women was from 37 to 40 weeks (mean gestational age 38.5).
All patients were subjected to relevant history taking, ultrasonographic examination, and estimation of the actual birth weight after delivery.
Correlation in each group
The correlation between the actual birth weight and the EFW (using both Hadlock’s formula and Isobe’s formula) was calculated in each group.
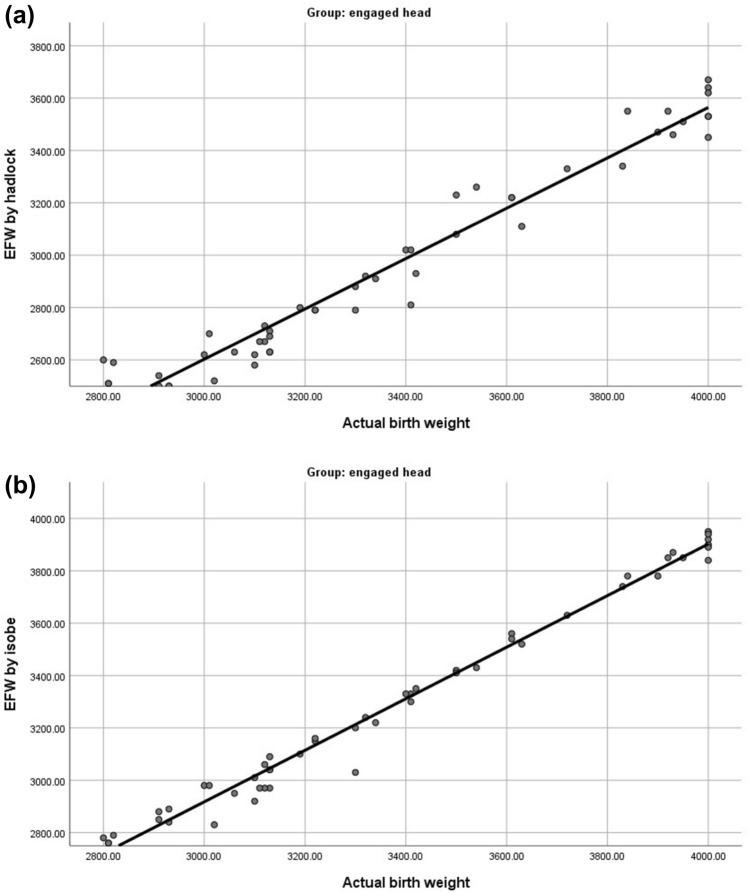
Engaged group
There was a strong positive correlation between the EFW (obtained by either Hadlock’s formula or Isobe’s formula) and the actual birth weight in the engaged fetal head group, with a higher correlation coefficient with Isobe’s formula (r = 0.993, p < 0.01) (Table 1, Figs. 2 and 3).
Table 1.
Correlation between EFW by both formulae and actual birth weight
| EFW by Hadlock | EFW by Isobe | |
|---|---|---|
| Engaged head | ||
| Actual birth weight | ||
| r | 0.978 | 0.993 |
| P value | < 0.001 | < 0.001 |
| N | 51 | 51 |
| Non engaged head | ||
| Actual birth weight | ||
| r | 0.994 | 0.975 |
| P value | < 0.001 | < 0.001 |
| N | 51 | 51 |
Significant P values are given in bold (P < 0.005)
Fig. 2.
Scatter-Plots showing. a Correlation between Actual Birth Weight and EFW using Hadlock’s Formula in engaged head group. b Correlation between Actual Birth Weight and EFW using Isobe’s Formula in engaged head group
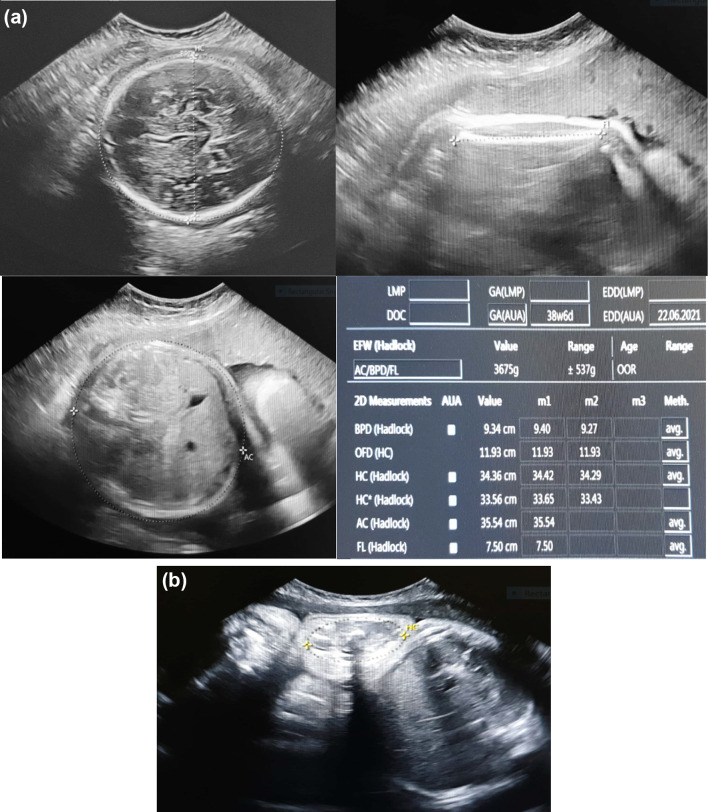
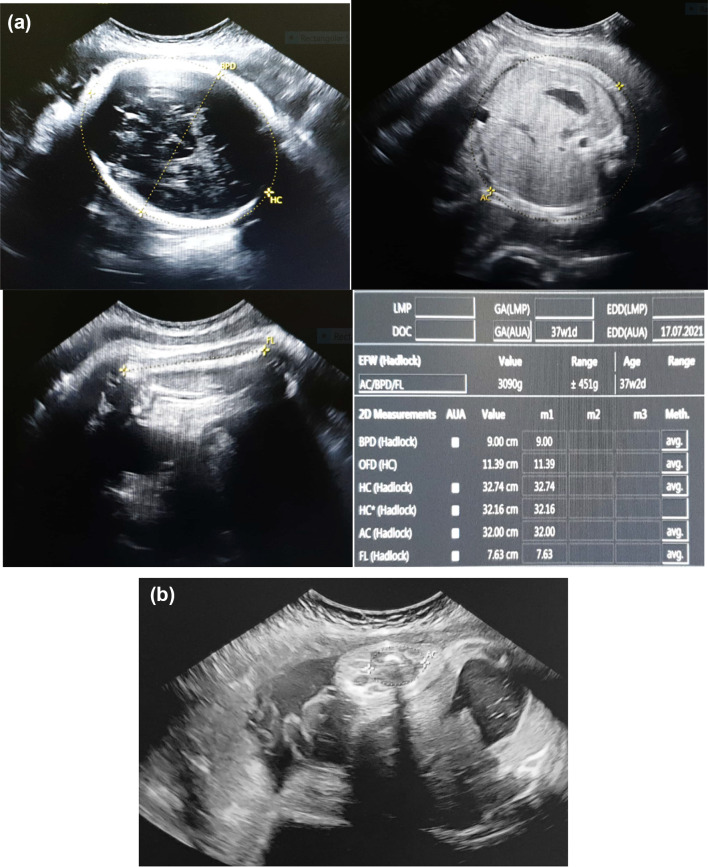
Fig. 3.
38 weeks and 6 days pregnant primigravida with engaged fetal head (at + 1 station). a Estimation of fetal weight using Hadlock’s formula. b Measurement of CSAT in the same patient
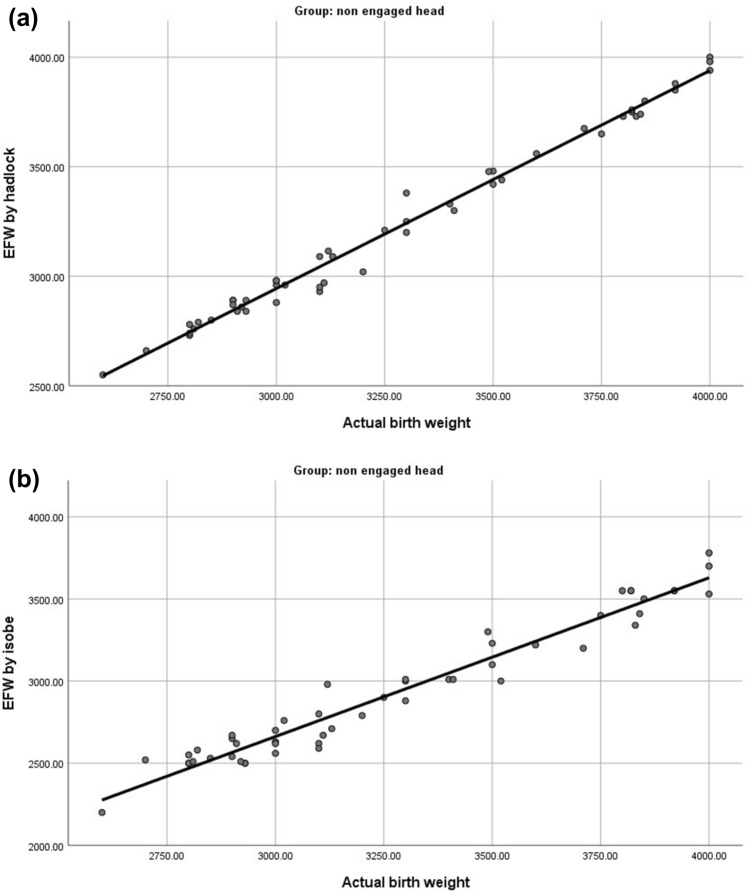
Non-engaged group
There was a strong positive correlation between the EFW (obtained by either Hadlock’s formula or Isobe’s formula) and the actual birth weight in the non-engaged fetal head group, with a higher correlation coefficient with Hadlock’s formula (r = 0.994, p < 0.01) (Table 1, Figs. 4 and 5).
Fig. 4.
Scatter-Plots showing. a Correlation between Actual Birth Weight and EFW using Hadlock’s Formula in non-engaged head group. b Correlation between Actual Birth Weight and EFW using Isobe’s Formula in non-engaged head group
Fig. 5.
37 weeks and 1 day pregnant primigravida with non-engaged fetal head. a Estimation of fetal weight using Hadlock’s formula. b Measurement of CSAT in the same patient
The paired difference between each method and the actual birth weight was measured in each group.
Engaged group
The paired difference between the EFW obtained by Hadlock’s formula and the actual birth weight was 411.96078 ± 81.09302, but the paired difference between the EFW obtained by Isobe’s formula and the actual birth weight was 88.23529 ± 46.93425.
The narrow 95% CI for Isobe’s formula compared to Hadlock’s formula shows that in the engaged head group, the EFW can be determined more accurately by Isobe’s formula (Table 2).
Table 2.
The paired difference between each method and actual birth weight in engaged and non-engaged fetal head groups
| Paired Differences | P value | |||||
|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | 95% confidence interval of the difference | |||
| Lower | Upper | |||||
| Engaged head | ||||||
| EFW by Hadlock - Actual birth weight | 411.96078 | 81.09302 | 11.35529 | 434.76856 | 389.15300 | <0.001 |
| EFW by Isobe - Actual birth weight | 88.23529 | 46.93425 | 6.57211 | 101.43576 | 75.03482 | <0.001 |
| Non engaged head | ||||||
| EFW by Hadlock - Actual birth weight | 57.49020 | 45.87652 | 6.42400 | 70.39317 | 44.58722 | <0.001 |
| EFW by Isobe - Actual birth weight | 347.05882 | 91.65793 | 12.83468 | 372.83803 | 321.27961 | <0.001 |
Significant P values are given in bold (P < 0.005)
Non-engaged group
The paired difference between the EFW obtained by Hadlock’s formula and the actual birth weight was 57.49020 ± 45.87652, but the paired difference between the EFW obtained by Isobe’s and the actual birth weight was 347.05882 ± 91.65793.
The narrow 95% CI for Hadlock’s formula compared to Isobe’s formula shows that in the non-engaged head group, the EFW can be determined more accurately by Hadlock’s formula (Table 2).
Comparison between the two groups
In the engaged fetal head group, the mean EFW predicted by Hadlock’s formula was 2962.35 kg, and the mean EFW predicted by Isobe’s formula was 3286.08 kg. The mean actual birth weight was 3374.31 kg. This shows that the EFW obtained by Isobe’s formula is significantly higher in the engaged head group (Table 3).
Table 3.
Comparison between EFW and mean absolute error percentages by Hadlock’s and Isobe’s formula in both groups
| Engaged head | Non engaged head | P value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Minimum | Maximum | Mean | SD | Median | Minimum | Maximum | ||
| EFW by Hadlock | 2962.35 | 384.00 | 2810.00 | 2500.00 | 3670.00 | 3222.51 | 413.50 | 3090.00 | 2550.00 | 4000.00 | 0.001 |
| EFW by Isobe | 3286.08 | 387.52 | 3200.00 | 2760.00 | 3950.00 | 2932.94 | 409.21 | 2800.00 | 2200.00 | 3780.00 | < 0.001 |
| Actual birth weight | 3374.31 | 390.65 | 3300.00 | 2800.00 | 4000.00 | 3280.00 | 412.87 | 3130.00 | 2600.00 | 4000.00 | 0.239 |
| Absolute error of Hadlock | 411.96 | 81.09 | 420.00 | 200.00 | 600.00 | 60.63 | 41.55 | 50.00 | 0.00 | 180.00 | < 0.001 |
| Absolute error of Isobe | 88.24 | 46.93 | 80.00 | 20.00 | 270.00 | 347.06 | 91.66 | 350.00 | 140.00 | 520.00 | < 0.001 |
| Absolute error % of Hadlock | 12.31 | 2.57 | 12.50 | 7.14 | 17.60 | 1.86 | 1.30 | 1.75 | 0.00 | 5.63 | < 0.001 |
| Absolute error % of Isobe | 2.62 | 1.45 | 2.35 | 0.67 | 8.18 | 10.68 | 2.90 | 10.71 | 4.49 | 16.45 | < 0.001 |
Significant P values are given in bold (P < 0.005)
In the non-engaged fetal head group, the mean EFW predicted by Hadlock’s formula was 3222.51 kg, and the mean EFW predicted by Isobe’s formula was 2932.94 kg. The mean actual birth weight was 3280.00 kg. This shows that the EFW obtained by Hadlock’s formula is significantly higher in the non-engaged head group (Table 3).
In the engaged fetal head group, the mean absolute error percentage of the actual birth weight was 12.31% using Hadlock’s formula and 2.62% using Isobe’s formula. This indicates that the absolute error percentage of Hadlock’s formula is higher in the engaged group (Table 3).
In the non-engaged fetal head group, the mean absolute error percentage of the actual birth weight was 1.86% using Hadlock’s formula and 10.68% using Isobe’s formula. This indicates that the absolute error percentage of Isobe’s formula is higher in the non-engaged group (Table 3).
In the engaged fetal head group, of the included 51 cases, 9 (17.6%) had their absolute error in the EFW predicted by Hadlock’s formula within 10% of the actual birth weight, while 42 (82.4%) had their absolute error above 10% of the actual birth weight. However, all 51 cases (100%) had their absolute error in the EFW predicted by Isobe’s formula within 10% of the actual birth weight, with no cases with an error percentage above 10% of the actual birth weight (Table 4).
Table 4.
The absolute error of both formulae in the two studied groups
| Engaged head | Non engaged head | P value | |||
|---|---|---|---|---|---|
| Count | % | Count | % | ||
| Absolute error of hadlock | |||||
| Within 10% of actual birth weight | 9 | 17.6% | 51 | 100.0% | < 0.001 |
| > 10% of actual birth weight | 42 | 82.4% | 0 | 0.0% | |
| Absolute error of isobe | |||||
| Within 10% of actual birth weight | 51 | 100.0% | 23 | 45.1% | < 0.001 |
| > 10% of actual birth weight | 0 | 0.0% | 28 | 54.9% | |
Significant P values are given in bold (P < 0.005)
In the non-engaged fetal head group, of the included 51 cases, 23 (45.1%) had their absolute error in the EFW predicted by Isobe’s formula within 10% of the actual birth weight, while 28 (54.9%) had their absolute error above 10% of the actual birth weight. However, all 51 cases (100%) cases had their absolute error in the EFW predicted by Hadlock’s formula within 10% of the actual birth weight, with no cases with an error percentage above 10% of the actual birth weight (Table 4).
This shows that Hadlock’s formula is better in the non-engaged group, as 100% of the error is within 10% of the actual birth weight, but that Isobe’s formula is better in the engaged group, as 100% of the error is within 10% of the actual birth weight.
Discussion
Estimated fetal weight has been used in the routine antepartum evaluation of high-risk pregnancies and deliveries. The management of diabetic pregnancy, vaginal birth after a previous caesarean section, and breech presentations will be affected by estimated fetal weight. Hence, accurate estimation of fetal weight is important in the management of labour and delivery [6].
The two main methods for predicting birth weight are the clinical and the sonographic method. Although some investigators consider ultrasonography to be more accurate than clinical assessment, others found that both have the same level of accuracy [7].
The estimation of fetal weight commonly includes head circumference, abdomen circumference, and femur length, either separately or, more often, all together. Adding thigh measurements to these measurements have been studied to detect their role. Head measurements are inconvenient in certain conditions, such as when the fetal head is engaged deeply in the pelvis. In this situation, other methods for fetal weight estimation are needed to avoid head measurement [8].
This study showed that there was a strong positive correlation between the EFW (obtained by either Hadlock’s formula or Isobe’s formula) and the actual birth weight in the engaged fetal head group, with a higher correlation coefficient with Isobe’s formula (r = 0.993, p < 0.01). This agreed with a study by Rizwan et al., which found a high correlation coefficient of 0.910 with Isobe’s formula.
This present study found that there was a strong positive correlation between the EFW (obtained by either Hadlock’s formula or Isobe’s formula) and the actual birth weight in the non-engaged fetal head group, with a higher correlation coefficient with Hadlock’s formula (r = 0.994, p < 0.01).
In agreement with our results, Sonica et al. conducted a study that showed that the EFW obtained by Hadlock’s formula was not significantly different from the actual birth weight (p = 0.00001) [9].
When comparing the EFW in both groups with the actual birth weight, we found that the EFW obtained by Hadlock’s formula is significantly lower in the engaged head group and that the absolute error percentage of Hadlock’s formula is higher in the engaged head group, indicating that Hadlock’s formula is less accurate in measuring the EFW in the engaged fetal head group than in the non-engaged fetal head group. This agrees with a study by Joanna et al., which concluded that when head measurements are difficult to estimate by ultrasonography, Hadlock’s formula can be used without head measurements, indicating that Hadlock’s formula with head measurements is inaccurate in certain situations [10].
Our study is the first to indicate that the EFW obtained by Isobe’s formula is significantly higher in the engaged fetal head group and that the absolute error percentage of Isobe’s formula is lower in the engaged fetal head group, indicating that Isobe’s formula is more accurate in measuring the EFW in the engaged fetal head group than in the non-engaged fetal head group. Ayman et al. conducted a study that showed that using new algorithms, such as measuring fetal thigh soft tissue, is more important than using Hadlock’s formula in the estimation of fetal weight [11].
Conclusion
We concluded that the ultrasonographic estimation of fetal weight was statistically significant with both formulas, although Isobe’s formula was more accurate in detecting the fetal weight in cases with an engaged fetal head in the pelvis.
Hadlock’s formula was superior to Isobe’s formula in the non-engaged fetal head group, but Isobe’s formula was superior in the engaged fetal head group.
Isobe’s formula can be used as an accurate method for the estimation of fetal weight when head measurements are difficult to obtain because of an engaged fetal head in the pelvis.
Acknowledgements
The completion of this work couldn’t have been possible without the support and participation of Dr. Ahmed Adel Elagamy. His assistance is sincerely appreciated. We would like to express our gratitude to all the patients, staff members and colleagues.
Abbreviations
- AC
Abdominal circumference
- BPD
Bi- parietal diameter
- CI
Confidence interval
- Cm
Centimeter
- CS
Cesarean section
- CSAT
Cross sectional area of the thigh
- EFBW
Estimated fetal body weight
- EFW
Estimated fetal weight
- FL
Femur length
- gm
Gram
- HC
Head circumference
- Kg
Kilogram
- MHz
Mega Hertz
- SD
Standard deviation
- SPSS
Statistical Package for the Social Science
- USA
United States of America
- 2D
Two dimensional
Author contributions
NK and AH analyzed and interpreted the patient data regarding the ultrasonographic results of both Hadlock’s and Isobe’s formula. AE examined the patients, analyzed and interpreted the data regarding the status of the fetal head during labour and the actual birth weight after delivery. MF revised all the data interpreted by other authors. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval and consent to participate
The current study had been approved by Kasr El-Aini Hospital, Research and Ethical committee. Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in the figures.
Contributor Information
Nour Mohamed Kandil, Email: dr.n.kandil@hotmail.com.
Mona Mohammed Fatouh, Email: monafatouh@yahoo.com.
Ahmed Adel Elagamy, Email: aaaaagami@gmail.com.
Aya Bassam Hashem, Email: Yummmy84@hotmail.com.
References
- 1.Hammami A, Mazer A, Syngelakir R, Akolekar K, Nicolaides H. Ultrasonographic estimation of fetal weight: development of new model and assessment of performance of previous models. Ultrasound Obstet Gynecol. 2018;52:35–43. doi: 10.1002/uog.19066. [DOI] [PubMed] [Google Scholar]
- 2.Saqib R, Tariq SS, Tahir SS, Fatima S. Estimation of fetal weight in third trimester using thigh measurements. J Ayub Med Coll Abbottabad. 2008;20(3):92–96. [PubMed] [Google Scholar]
- 3.Lokesh K, Bhawani S, Shikha S. Ultrasonographic fetal gestational age determination by biparietal diameter. Ann Int Med Dental Res. 2017;3:49–51. [Google Scholar]
- 4.Bronius Z, Daiva B, Gražina D, Algirdas U, Juozas K. Fetal biometry: relevance in obstetrical practice. Medicina. 2017;53:357–364. doi: 10.1016/j.medici.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Isobe T. Approach for estimating fetal body weight using two-dimensional ultrasound. J Maternal-Fetal Neonatal Med. 2004;15:225–231. doi: 10.1080/14767050410001668680. [DOI] [PubMed] [Google Scholar]
- 6.Ashwini I, Shweta A, Sneha S. Clinical versus ultrasonographic fetal weight estimation and its correlation with actual birth weight. Int J Reprod Contracept Obstet Gynecol. 2019;8:503–512. doi: 10.18203/2320-1770.ijrcog20190275. [DOI] [Google Scholar]
- 7.Avirupa G, Manasi H, Kathaley Comparison of estimation of fetal weight by clinical method, ultrasonography, and its correlation with actual birth weight in term pregnancy. MVP J Med Sci. 2018;5:75–81. doi: 10.18311/mvpjms/2018/v5/i1/10077. [DOI] [Google Scholar]
- 8.Rizwan S, Tariq S, Tahir S, Sughra F. Estimation of fetal weight in third trimester using thigh measurements. J Ayub Med Coll Abbottabad. 2008;20(3):92–96. [PubMed] [Google Scholar]
- 9.Sonica S, Indira G, PayalaV Ameen B, Suresh V. Comparative study between clinical methods and ultrasound examination in the estimation of fetal weight. Int J Health Sci Res. 2019;9(5):79–86. [Google Scholar]
- 10.Joanna D, Reli H, Salvatore A, et al. Estimation of fetal weight using Hadlock’s formulas: Is head circumference an essential parameter? Eur J Obstet Gynecol Reprod Biol. 2019;24:87–92. doi: 10.1016/j.ejogrb.2019.09.024. [DOI] [PubMed] [Google Scholar]
- 11.Ayman E, Sayed A, Waleed A, Mohammed FM, Alaa M. Antenatal ultrasound measurement of fetal-thigh soft-tissue thickness as a predictor of fetal birth weight. Menoufia Med J. 2021;34:724–728. doi: 10.4103/mmj.mmj_391_20. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.