Abstract
Purpose
To assess the diagnostic accuracy of contrast-enhanced ultrasound (CEUS) and computed tomography (CT) within Bosniak IIF/III categories.
Methods
After cystic renal mass diagnosis by contrast-enhanced CT, all patients with Bosniak score ≥ II also underwent CEUS between March 2017 and March 2019. Their exams were retrospectively analyzed. One experienced uro-radiologist performed every CEUS and reviewed the exams according to the EFSUMB 2020 Position Statement, while blinded to clinical data. CT Bosniak scores were retrospectively given blindly by two uro-radiologists (CT 1 and CT 2). We compared CEUS, CT 1 and CT 2 scores to clinical findings and histological tests. Clinical performance characteristics and area under the receiver operating characteristic (ROC) curves (AUCs) were determined separately for CEUS and CT, and then compared.
Results
101 cystic masses were analyzed. In Bosniak categories IIF and III, the AUCs were 0.854 for CT 1, 0.779 for CT 2, and 0.746 for CEUS.
Conclusion
Despite some statistical limitations, this study confirms that among cystic renal masses, those classified as Bosniak IIF and III are the most difficult to assess. The diagnostic performances of CEUS and CT are similar within this group. However, in experienced hands, CEUS could be valuable in further evaluation of ambiguous cystic masses, and in more ductile, safer, and cost-effective surveillance of those classified as Bosniak IIF and III. When challenging cystic renal masses occur, CEUS is a useful tool for clinical management and for the follow-up of non-surgical lesions.
Keywords: Cystic renal masses, Kidney, Renal cysts, CEUS, CT, Comparison, Diagnostic accuracy
Introduction
Renal cysts are frequently encountered in clinical practice, with an incidence rate of approximately 50% in patients aged > 50 years [1], and 8–15% of them may have a complex appearance [2, 3]. The Bosniak classification system categorizes renal cysts into five categories (I, II, IIF, III, and IV) [4, 5] according to their computed tomography (CT) features. It has consistently demonstrated the ability to predict the proportion of these cysts that will be renal cell carcinoma (RCC) [6].
Renal cysts can also be evaluated with magnetic resonance imaging (MRI) and contrast-enhanced ultrasound (CEUS), which achieve good concordance rates compared to contrast CT [7]. CEUS could be more sensitive compared to contrast CT in detecting blood flow in renal vessels [8] in hypovascular lesions [9], very thin septa, cystic walls, and solid components [10]. Furthermore, CEUS has some potential advantages compared to other contrast-enhanced imaging techniques: it can be safely used without the risk of contrast-induced nephropathy [11], hyperthyroidism, nephrogenic systemic fibrosis [12], or contrast accumulation in organs [13]. CEUS does not expose patients to ionizing radiation, it can be used in patients with metal implants, it can also be performed at the bedside even in non-cooperative patients prone to motion artifacts [9] and it reduces costs for the health care system [14].
In the Bosniak classification, IIF/III scores cause challenges in making the right diagnosis [5, 15]. The malignancy prevalence rates for Bosniak IIF and III are 0.18 [0.13, 0.25] and 0.51 [0.44, 0.58], respectively. For this reason, some patients may receive unnecessary surgical treatments; cancer may be missed as well [16]. Often, multiple CT scans expose patients to a high dose of ionizing radiation [7]. We hypothesized that CEUS could give some advantages compared to CT in terms of diagnostic performance, especially in the difficult group of Bosniak IIF/III cystic masses. The aim of this study was to assess the diagnostic accuracy of CEUS and CT within Bosniak IIF/III categories.
Methods
Patient selection
We retrospectively collected data of all patients who underwent CEUS at a single institution between March 2017 and March 2019 after a three-phase CT scan diagnosis of cystic renal masses (i.e., those with a Bosniak score of II or higher).
Ethical approval for this study was obtained from the local ethics committee (approval number: 0090337). The study was conducted in accordance with current legislation, in compliance with the rules of good clinical practice (GCP) and the principles of the Declaration of Helsinki. Patients in the study were provided with information pursuant to and for the purposes of a national regulation relating to the protection of individuals with regard to the processing of personal data. A specific authorization from the local committee was applied for patients who were deceased or non-contactable at the time of enrollment in the study.
Study inclusion criteria were: age over 18 years; contrast-enhanced CT scan diagnosis of cystic masses according to Bosniak category II or higher; normal kidney function (estimated creatinine clearance > 60 ml/min/1.74 m2); and CEUS performed after the CT scan by the same radiologist.
Exclusion criteria were: age under 18 years; contrast allergy and contraindications to contrast medium CT scan or CEUS; pregnancy or breastfeeding; previous renal surgery or biopsy; CEUS performed by a different radiologist than E.G.; CT diagnosis of simple benign cysts; and necrotic masses.
Imaging evaluation modalities and techniques
The same CT scanner, same ultrasound scanning system and same CT/CEUS contrast agents were used in all patients analyzed. CEUS were performed by a radiologist (E.G.) with over 20 years of experience in urological imaging and CEUS. He performed a preliminary review of the CT imaging and performed each CEUS. Potential limitations of CEUS analysis, such as difficult-to-image patients, deep cyst positions, calcification hampering evaluation of the intracystic content, large cysts that were incompletely examined or poor acoustic windows, were recorded at the time of examination. CT Bosniak scores and CEUS Bosniak scores were assigned by evaluation of the number of septa, thickness of walls and septa, presence of a solid component, and calcification, according to Bosniak classification [4, 5] and modified Bosniak classification [15, 17]. For CT Bosniak score evaluation, the enhancement was considered only if measurable [17] (Figs. 1, 2). All data were stored in the local Picture Archive Communication System (PACS).
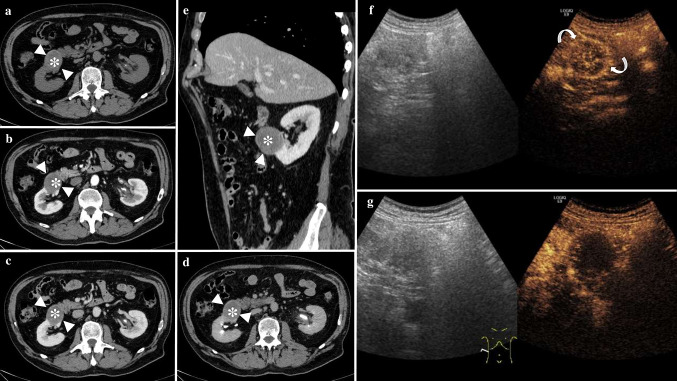
Fig. 1.
CT: unenhanced (a), corticomedullary (b), nephrographic (c), urographic (d), sagittal reconstruction (e). An exophytic mass of 4 cm in diameter arose from the anterior lip of the right kidney. The unenhanced phase showed a slightly thickened and hyperdense capsule (arrowheads). After iodine contrast media injection, a mild enhancement of the capsule appeared. The core of the lesion (asterisks) showed nonenhancing content (< 20 Hounsfield units) [17] after contrast injection. CEUS: arterial (f) and late phase (g). The arterial phase showed a capsular enhancement (curved arrows) and intralesional vascularized areas. In the late phase, the washout was noticeable both for the capsule and the intralesional area. The reviewed CT Bosniak scores were IV for CT1 and III for CT2. The CEUS Bosniak score was IV. The pathologic specimen was consistent with a type 2 papillary RCC
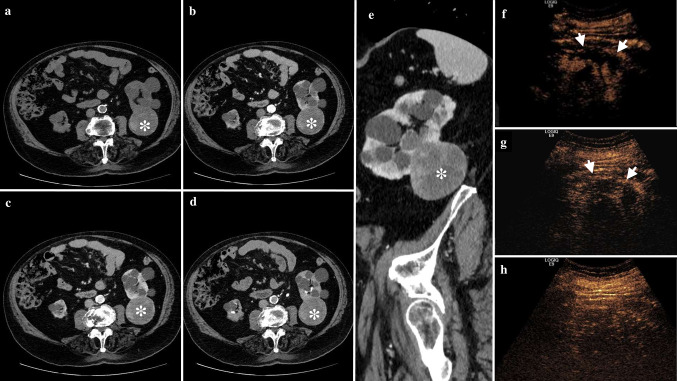
Fig. 2.
CT: unenhanced (a), corticomedullary (b), nephrographic (c), urographic (d) and coronal reconstruction (e). An exophytic 5 cm mass originated from the inferior pole of the left kidney. The center of the mass (asterisks) was characterized by weakly hyperintense areas. After iodine contrast media injection, some weakly vascularized sepimentations surrounding multiple chambers were highlighted. CEUS: arterial (f), venous (g) and late phase (h). In the arterial and venous phases, some focal vascularized thickenings of the wall appeared (arrowheads), and some mildly enhanced thickened septa were highlighted. In late phase scans, walls and septa presented partial washout. The reviewed CT Bosniak scores were III (CT1) and IV (CT2). The CEUS Bosniak score was III. The pathologic specimen was consistent with a xanthogranulomatous cyst
CT scan
The CT protocol used in this study was obtained on a 64-channel CT (Philips Diamond Select Brilliance CT 64-slice. Philips, The Netherlands). The scanning range was from the diaphragm to the perineum, and the field of view (FoV) was at skin level. An unenhanced scanning phase was performed before contrast media injection. A bolus of 120 ml iodine contrast media (Ioexole 350 mg/ml) was injected intravenously, followed by a 40 ml of 0.9% NaCl solution flush with injection rate at 3 ml/s for both contrast media and saline. The arterial contrast concentration was monitored with ROI in the diaphragm and abdominal aorta, with a trigger level of 115 Hounsfield Units (HU). Corticomedullary, nephrographic and urographic phase images were taken 10 s, 90 s and 10 min after the trigger. The scan parameters for all three phases were kept the same for all the CT exams. Slice thickness was 0.625 mm, with rotation speed at 0.5 s/rotation. All images were reconstructed with three-dimensional algorithm in 1 mm slice thickness.
CEUS
All performed ultrasound examinations were made by GE LOGIQ E9 scanner (GE Healthcare, Milwaukee, WI, US) at a low acoustic mechanical index. We used an aqueous suspension of stabilized sulfur hexafluoride microbubbles with a phospholipidic shall (SonoVue®, Bracco, Milan, Italy) as contrast media. Before CEUS, all suspected lesions were studied in B mode, and then color Doppler was performed to evaluate the intratumoral vascularity. Examinations were performed with 1 dose of 2.4 ml contrast medium, and a second dose was administered if needed. Contrast medium was injected rapidly through an antecubital vein, immediately followed by a flush of 5 ml 0.9% NaCl solution. Each single 2.4 ml dose examination lasted approximately 6 min, during which video clips and single images were stored.
Outcome and follow-up
CT and CEUS images were discussed in multidisciplinary meetings to decide the subsequent treatment (discharge, follow-up, surgical treatment). Patients with CT Bosniak II and subsequent CEUS Bosniak I had their follow-up ended. We decided to follow-up CT Bosniak IIF or superior and every CEUS Bosniak II and Bosniak IIF. CEUS and CT were alternately used for follow-up, with the same scanner, technique and contrast agents adopted for the initial CT/CEUS. The timing of follow-up and the imaging technique were decided according to the characteristics of the cystic masses (CT/CEUS Bosniak score, dimensional stability, appearance of new septa or solid components, thickening of previous ones, increasing contrast enhancement) and patient (comorbidities, suitability for surgical procedures, life expectancy). In patients with Bosniak III and IV scores, a radical/partial nephrectomy was the first choice performed by two surgeons, while in patients with severe comorbidities and reduced lifespan, surveillance or cryoablation was the best choice. When surgery was performed, a histologic diagnosis was obtained for each surgical specimen.
Data recording
We collected radiological, clinical, pathological and follow-up data, along with clinical discussion recordings. The same radiologist who had performed CEUS re-evaluated the CEUS images stored in the PACS according to EFSUMB 2020 Position Statement [15] and blinded from other clinical data (CEUS Bosniak score). Two dedicated uro-radiologists (E.G, N.C.), with over 20 and over 10 years of experience in urologic imaging, retrospectively reviewed CT imaging, blinded to clinical/laboratory/imaging findings, and gave their Bosniak score to every cystic mass (CT 1 and CT 2) according to the 2019 Silverman classification [17].
All pathologic specimens were reviewed by two trained genitourinary pathologists (P.M, F.C.), with over 15 years of experience each, who were blinded to clinical/laboratory/imaging findings. CT Bosniak scores reviewed (CT 1 and CT 2) and CEUS Bosniak scores were compared to clinical and histological outcomes. Every benign histology and Bosniak ≤ IIF during the follow-up was considered benign, while every malignant histology and Bosniak score ≥ III during the follow-up was considered malignant.
Statistical analysis
Diagnostic performance, defined by sensitivity, specificity, positive predictive value, negative predictive value, area under the receiver operating characteristic (ROC) curve (AUC), accuracy and Youden Index, was determined separately for CEUS, reviewed CT 1 and CT 2. Areas under CEUS and CT 1/CT 2 ROC curves were compared. A p-value of less than 0.05 was considered to indicate a statistically significant difference. Statistical analyses were performed using MedCalc for Windows, version 14.8.1 (MedCalc Software, Ostend, Belgium).
Results
Of the 104 cystic masses evaluated with contrast CT and CEUS, 3 were lost during follow-up and 101 were considered for the study (Table 1). Of these, 8 were CT Bosniak II and CEUS Bosniak I, and therefore considered benign; 71 required repeated CT or CEUS for follow-up and 22 were addressed with surgery (Table 2).
Table 1.
Clinical characteristics of patients and cystic masses evaluated
| No | % | |
|---|---|---|
| Patients | ||
| Tot | 87 | |
| Males | 64 | 73.5% |
| Females | 23 | 26.5% |
| Mean age ± SD | 69.1 ± 10.6 years | |
| Number of cystic masses evaluated | ||
| Tot | 101 | |
| Number of cystic masses per patient | ||
| 1 | 75 patients | 86.2% |
| 2 | 10 patients | 11.5% |
| 3 | 2 patients | 2.3% |
| Mean size of the cyst at diagnosis ± SD | 3.2 ± 2.7 cm | |
| Cystic mass location | ||
| Left kidney | 60 | 59.4% |
| Right kidney | 41 | 40.6% |
| Cystic mass position | ||
| Superficial | 78 | 77.2% |
| Deep | 23 | 22.8% |
| Number of cystic masses per Bosniak category at CT diagnosis | ||
| II | 44 | 43.6% |
| IIF | 25 | 24.7% |
| III | 21 | 20.8% |
| IV | 11 | 10.9% |
Table 2.
Clinical and pathological results
| Number of cystic masses | % related to the masses | |
|---|---|---|
| Patients lost during follow-up | 3/104 | 2.9% |
| Multidisciplinary meeting decision (101 cystic masses) | ||
| End of follow-up | ||
| CT Bosniak II and CEUS Bosniak I | 8 | 7.9% |
| Follow-up (71 cystic masses) | ||
| Last CT imaging | 17 | 16.8% |
| Last CEUS imaging | 54 | 53.5% |
| Surgeries (22 cystic masses) | ||
| Radical nephrectomy | 7 | 6.9% |
| Partial nephrectomy | 14 | 13.9% |
| Renal biopsy and cryoablation | 1 | 1% |
| Cystic mass histology (22 cystic masses) | ||
| Clear cell RCC | 9 | 42.8% |
| Type 1 papillary RCC | 2 | 9.5% |
| Type 2 papillary RCC | 3 | 14.3% |
| Multilocular cystic renal neoplasm of low malignant potential (MCRNLMP) | 1 | 4.8% |
| Oncocytoma | 1 | 4.8% |
| Simple Cyst | 4 | 19% |
| Xanthogranulomatous cyst (renal biopsy) | 1 | 4.8% |
| Pathological T stage (15 surgeries for malignant tumors) | ||
| pT1a | 11 | 73.3% |
| pT1b | 3 | 20% |
| pT2b | 1 | 6.7% |
| ISUP grade (15 surgeries for malignant tumors) | ||
| 1 | 3 | 20% |
| 2 | 7 | 46.7% |
| 3 | 3 | 20% |
| 4 | 2 | 13.3% |
Due to severe comorbidities, a conservative regime was chosen in 10 patients (11 cystic masses) with CEUS Bosniak III and in 9 patients (9 cystic masses) with Bosniak IV cystic masses, and one patient was treated with renal biopsy before cryoablation. In this case, the histology was consistent with a xanthogranulomatous cyst. Overall, the pathologic specimens and follow-up imaging were consistent with 72 benign and 29 malignant cystic masses (Table 2). The median follow-up was 32 months (range 12–56).
We recorded difficult examinations in eight out of 101 cysts: in 4, the patient's body habitus was unfavorable, in 2 the acoustic window was poor, and in 2, there were relevant artifacts. We found no difficulty in fully examining large cysts, and no masses were so calcified as to prevent proper examination. However, at the time of the CEUS exam, these difficulties were not considered severe enough to undermine the reliability of the exam. We found 78 cystic masses in superficial position and 23 in deep position. The comparisons between the diagnostic performances of CT and CEUS in these groups are summarized in Table 3.
Table 3.
Diagnostic performances
| Sensitivity (%) |
Specificity (%) |
PPV (%) |
NPV (%) |
Accuracy (%) |
Youden’s index (%) |
AUC (Standard Error) |
|
|---|---|---|---|---|---|---|---|
| Bosniak IIF – III (number = 46) | |||||||
| CT 1 | 90 | 88.8 | 78.3 | 91.3 | 89.3 | 70.8 | 0.854 (0.052) |
| CT 2 | 75 | 80.8 | 75 | 80.8 | 78.3 | 55.8 | 0.779 (0.063) |
| CEUS | 80 | 69.2 | 66.6 | 81.8 | 73.9 | 49.2 | 0.746 (0.065) |
| Bosniak II – IV (number = 55) | |||||||
| CT 1 | 80 | 82.2 | 49.9 | 94.9 | 81.8 | 62.2 | 0.811 (0.073) |
| CT 2 | 100 | 77.8 | 49.9 | 100 | 84.3 | 77.8 | 0.889 (0.031) |
| CEUS | 100 | 86.7 | 62.6 | 100 | 88.5 | 86.7 | 0.933 (0.026) |
| Diameter ≤ 2 cm (number = 50) | |||||||
| CT 1 | 88.2 | 75.7 | 65.2 | 92.6 | 80 | 64 | 0.82 (0.055) |
| CT 2 | 76.5 | 75.8 | 61.9 | 86.2 | 76 | 52.3 | 0.761 (0.065) |
| CEUS | 76.5 | 81.8 | 68.4 | 87.1 | 80 | 58.3 | 0.791 (0.063) |
| Diameter > 2 cm (number = 51) | |||||||
| CT 1 | 84.6 | 86.8 | 68.7 | 94.3 | 86.2 | 71.5 | 0.857 (0.059) |
| CT 2 | 92.3 | 81.6 | 63.2 | 96.9 | 84.3 | 73.9 | 0.869 (0.05) |
| CEUS | 100 | 78.9 | 61.8 | 100 | 78.4 | 78.9 | 0.895 (0.033) |
| Superficial position (number = 78) | |||||||
| CT 1 | 85.7 | 82.5 | 64.3 | 94 | 83.4 | 68.2 | 0.841 (0.047) |
| CT 2 | 76.2 | 77.2 | 55.2 | 89.8 | 76.9 | 53.4 | 0.767 (0.055) |
| CEUS | 85.7 | 82.5 | 64.3 | 94 | 83.4 | 68.2 | 0.841 (0.047) |
| Deep position (number = 23) | |||||||
| CT 1 | 87.5 | 73.3 | 63.6 | 91.7 | 73.3 | 60.8 | 0.804 (0.086) |
| CT 2 | 87.5 | 80 | 70 | 92.3 | 80 | 67.5 | 0.838 (0.082) |
| CEUS | 87.5 | 66.7 | 58.3 | 91 | 66.8 | 54.2 | 0.771 (0.089) |
AUC Area Under the Curve, CT Computed Tomography, CEUS Contrast-Enhanced Ultrasound, NPV Negative Predictive Value, PPV Positive Predictive Value
Accuracy = (True positive + true negative)/(True positive + true negative + false positive + false negative)
Youden's index = Sensitivity + Specificity-1
AUC: Area Under Curve
Sensitivity, specificity, PPV, NPV, accuracy, and Youden’s index were calculated based on the number of positive cases and negative cases. PPV: Positive Predictive Value; NPV: Negative Predictive Value
In the group of 101 cystic masses evaluated, the probabilities of malignancy for CT1, CT2 and CEUS were 7.7%, 8.7% and 16.7%, respectively, for Bosniak IIF; 60%, 45.4%, and 43.7% for Bosniak III; and 73.7%, 83.3%, 76% for Bosniak IV.
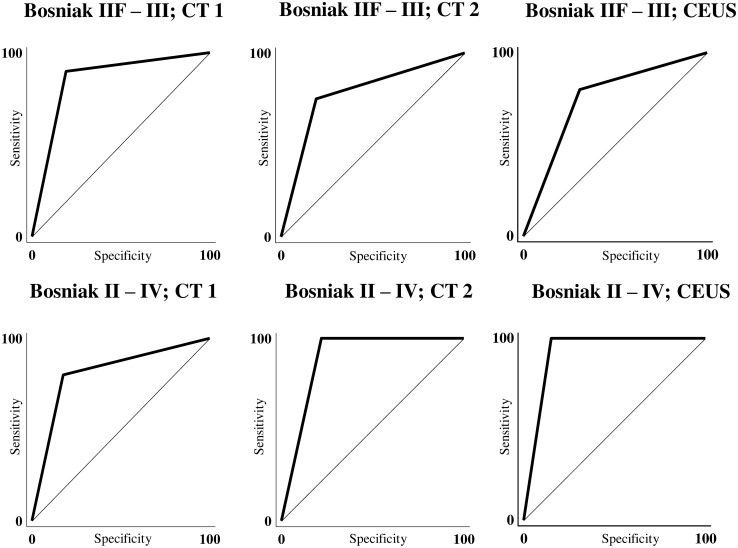
The result of ROC curves pairwise comparison (Fig. 3) within the Bosniak IIF/III category showed p-values (standard error, SE) of 0.19 (0.08) between CT 1 and CEUS, and of 0.7 (0.09) between CT 2 and CEUS. Within the Bosniak II/IV category, the p-value between CT 1 and CEUS was 0.11 (0.07), and between CT 2 and CEUS it was 0.28 (0.04). The p-value was more than 5% (p < 0.05) in both groups; therefore, no significant difference was observed between the AUCs of CT 1, CT 2 and CEUS. The ROC curves pairwise comparison of CT1, CT 2 and CEUS between Bosniak IIF/III and Bosniak II/IV groups showed p-values (standard error, SE) of respectively 0.63 (0.09), 0.12 (0.07) and 0.008 (0.07), respectively. The latter was statistically significant, with a p-value lower than 5% (p < 0.05). No side effects were recorded after CT or CEUS (Table 3).
Fig. 3.
ROC curves
Discussion
We analyzed the diagnostic accuracy of CT scan and CEUS in two cohorts of Bosniak IIF/III and Bosniak II/IV cystic masses, evaluated at the same institution. The results of our study show that diagnostic performances were better for both CT and CEUS in the Bosniak II/IV group compared to the Bosniak IIF/III group, confirming that in the former, cystic masses can be diagnosed with more confidence, as suggested by Israel et al. [18]. Although they were not significant, we found differences in CT 1 vs CEUS (p-value 0.19), CT 2 vs CEUS (p-value 0.7) within Bosniak IIF/III and CT 1 vs CEUS (p-value 0.11) and CT 2 vs CEUS (p-value 0.28) within the Bosniak II/IV category. We hypothesized that this difference was due to the interobserver variability between the two uroradiologists who reviewed CT exams. Notably, we found a greater difference in the diagnostic performances of CT and CEUS between the two cohorts than between CT and CEUS in the same cohort, as demonstrated by the significant difference between CEUS in the two groups (p-value 0.008). This can be explained by the high detection of contrast enhancement in CEUS. Accordingly, septa can appear thicker and wall/septa irregularities more evident [15], with the consequent risk of overestimating the Bosniak III category. For the management of the cystic masses with more nuanced features between categories IIF and III, we found useful to apply the EFSUMB 2020 Position Statement criteria [15] along with multidisciplinary discussion and closer follow-up.
Since the differentiation between benign and malignant tumors in category IIF/III is based mostly on CT [19], we believe that the clinical implications of our findings could be major. The distinction between these categories is essential, because their treatment is different [18]. Moreover, a surveillance approach for Bosniak III cystic masses has been considered recently as an alternative to surgical treatment in selected patients [19, 20], requiring less invasive imaging techniques in a short period of time. Therefore, in our opinion, these results suggest that CEUS could have a more important role in the evaluation and follow-up of Bosniak IIF and III cystic masses.
We found various reports suggesting equivalence between CT and CEUS [7, 21, 22], while others show better diagnostic performances for CEUS [23, 24]. Israel et al. speculated that CT may not reveal thin intracystic septations due to volume averaging [18], and thereby limit the assessment of small renal lesions. In order to reduce this effect, we adopted a CT scan protocol with 0.65 mm slices and multiplanar reconstructions, allowing a better view of millimetric septa. CT is also limited by the variable clearance of the contrast medium from the bloodstream and parenchyma from person to person. Therefore, the time at which the scan is performed may be suboptimal, especially in the nephrographic and urographic phases. Conversely, CEUS has two important characteristics. The first one is the exclusive blood pool without an excretory phase of microbubble contrast agent. Consequently, the renal cavity system is not enhanced [9]. The second one is the real-time observation of the contrast phase (a continuum from arterial phase, venous phase to late phase), which allows the radiologist to identify the best wash-in and wash-out imaging through a dynamic observation.
The value of MRI in the study of cystic renal masses is well recognized in the literature, where diagnostic performances comparable to CT are reported. Similarly to CEUS, MRI has a possible advantage in the study of vascularization and thin septa, but with the risk of higher false-positive rates [5, 7]. In our center, we have chosen to favor CEUS over MRI due to the presence of a radiologist who is an expert in CEUS, as well as due to the cost-effectiveness of CEUS compared to MRI. This preference also allows us to allocate as much MRI as possible where its use is irreplaceable. Furthermore, if CEUS is performed with dose fractions from 0.8 to 2.4 ml of ultrasound contrast, it is possible to perform two or more examinations with a single contrast pack, with a further cost reduction for the single exam.
CT (or MRI) is suggested at least once for evaluating incidental complex cystic masses, for three reasons. First, it gives a panoramic view of the kidney’s anatomy. In this way, cystic masses are discriminated from groups of adjacent simple cysts and from other anatomical anomalies. Second, the CEUS can be aimed directly on the cystic mass from the beginning of the contrast injection. Third, the operator can more easily orient the ultrasound probe in the most convenient fashion in order to sharpen the view of septa and solid components. In our experience, this standardized approach and the registration of CT and CEUS images helped the radiologist during the examinations and the multidisciplinary team during the case discussion. Above all, it assisted in the management of the follow-up.
This study had some limitations. First, it was a single-center and retrospective study. To reduce the discrepancies among examinations, one single radiologist performed each CEUS. In addition, CT and pathologic specimens were reviewed blindly twice. Second, we chose follow-up data besides the pathological outcome, but it would obviously be impossible to obtain a histology of all renal cystic masses, particularly of those for which surveillance is recommended. Third, one radiologist assessed CEUS, while two radiologists assessed for CT revision. Fourth, the analysis was not fully blinded, since one of the two radiologists who reviewed CT also performed CEUS. However, he was blinded to patient clinical data in both analyses.
Conclusions
Despite some statistical limitations, this study confirms that among cystic renal masses, those classified as Bosniak IIF and III are the most difficult to assess. Within this group, the diagnostic performances of CEUS and CT are similar. However, in experienced hands, CEUS could be valuable to further evaluate ambiguous cystic masses and for the more ductile, safer, and cost-effective surveillance of those classified as Bosniak IIF and III. When challenging cystic renal masses occur, CEUS is a useful tool for clinical management and for the follow-up of non-surgical lesions.
Author contributions
Conceptualization and methodology: LA, EG; formal analysis and investigation: EG, NC, PM, FC; writing—original draft preparation: LA; writing—review and editing: AG, CZ, YL; resources: AZ; supervision: AS, GP, SV.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Ethical approval for this study was obtained from AULSS 2 Marca Trevigiana Ethics Committee (approval number 0090337).
Informed consent
The study was conducted in accordance with current legislation, in compliance with the rules of good clinical practice (GCP) and the principles of the Declaration of Helsinki. Patients in the study were provided with the information pursuant to and for the purposes of the National Regulation relating to the protection of individuals with regard to the processing of personal data. For deceased or non-contactable patients at the time of enrollment in the study, a specific authorization of the local Committee was applied.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McGuire BB, Fitzpatrick JM. The diagnosis and management of complex renal cysts. Curr Opin Urol. 2010;20:349–354. doi: 10.1097/MOU.0b013e32833c7b04. [DOI] [PubMed] [Google Scholar]
- 2.Hitzeman N, Cotton E. Incidentalomas: Initial management. Am Fam Physician. 2014;90:784–789. [PubMed] [Google Scholar]
- 3.Harisinghani MG, Maher MM, Gervais DA, McGovern F, Hahn P, Jhaveri K, Varghese J, Mueller PR. Incidence of malignancy in complex cystic renal masses (Bosniak category III): should imaging-guided biopsy precede surgery? Am J Roentgenol. 2003;180:755–758. doi: 10.2214/ajr.180.3.1800755. [DOI] [PubMed] [Google Scholar]
- 4.Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986;158:1–10. doi: 10.1148/radiology.158.1.3510019. [DOI] [PubMed] [Google Scholar]
- 5.Bosniak MA. The Bosniak renal cyst classification: 25 years later. Radiology. 2012;262:781–785. doi: 10.1148/radiol.11111595. [DOI] [PubMed] [Google Scholar]
- 6.Donin NM, Mohan S, Pham H, Chandarana H, Doshi A, Deng FM, Stifelman MD, Taneja SS, Huang WC. Clinicopathologic outcomes of cystic renal cell carcinoma. Clin Genitourin Cancer. 2015;13:67–70. doi: 10.1016/j.clgc.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 7.Graumann O, Osther SS, Karstoft J, Hørlyck A, Osther PJS. Bosniak classification system: a prospective comparison of CT, contrast-enhanced US, and MR for categorizing complex renal cystic masses. Acta radiol. 2016;57:1409–1417. doi: 10.1177/0284185115588124. [DOI] [PubMed] [Google Scholar]
- 8.Correas JM, Claudon M, Tranquart F, Hélénon O. The kidney: imaging with microbubble contrast agents. Ultrasound Q. 2006;22:53–56. [PubMed] [Google Scholar]
- 9.Bertolotto M, Bucci S, Valentino M, Currò F, Sachs C, Cova MA. Contrast-enhanced ultrasound for characterizing renal masses. Eur J Radiol. 2018;105:41–48. doi: 10.1016/j.ejrad.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Chang EH, Chong WK, Kasoji SK, Fielding JR, Altun E, Mullin LB, Kim JI, Fine JP, Dayton PA, Rathmell WK. Diagnostic accuracy of contrast-enhanced ultrasound for characterization of kidney lesions in patients with and without chronic kidney disease. BMC Nephrol. 2017;18:1–13. doi: 10.1186/s12882-017-0681-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Granata A, Zanoli L, Insalaco M, Valentino M, Pavlica P, Di Nicolò PP, Scuderi M, Fiorini F, Fatuzzo P, Bertolotto M. Contrast-enhanced ultrasound (CEUS) in nephrology: Has the time come for its widespread use? Clin Exp Nephrol. 2015 doi: 10.1007/s10157-014-1040-8. [DOI] [PubMed] [Google Scholar]
- 12.Girometti R, Stocca T, Serena E, Granata A, Bertolotto M. Impact of contrast-enhanced ultrasound in patients with renal function impairment. World J Radiol. 2017;9:10. doi: 10.4329/wjr.v9.i1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turyanskaya A, Rauwolf M, Pichler V, Simon R, Burghammer M, Fox OJL, Sawhney K, Hofstaetter JG, Roschger A, Roschger P, Wobrauschek P, Streli C. Detection and imaging of gadolinium accumulation in human bone tissue by micro- and submicro-XRF. Sci Rep. 2020;10:1–9. doi: 10.1038/s41598-020-63325-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gulati M, King KG, Gill IS, Pham V, Grant E, Duddalwar VA. Contrast-enhanced ultrasound (CEUS) of cystic and solid renal lesions: a review. Abdom Imaging. 2015;40:1982–1996. doi: 10.1007/s00261-015-0348-5. [DOI] [PubMed] [Google Scholar]
- 15.Cantisani V, Bertolotto M, Clevert D-A, Correas J-M, Drudi FM, Fischer T, Gilja OH, Granata A, Graumann O, Harvey CJ, Ignee A, Jenssen C, Lerchbaumer MH, Ragel M, Saftoiu A, Serra AL, Stock KF, Webb J, Sidhu PS. EFSUMB 2020 proposal for a contrast-enhanced ultrasound-adapted bosniak cyst categorization—position statement. Ultraschall Med. 2021;42:154–166. doi: 10.1055/a-1300-1727. [DOI] [PubMed] [Google Scholar]
- 16.O’Malley RL, Godoy G, Hecht EM, Stifelman MD, Taneja SS. Bosniak Category IIF designation and surgery for complex renal cysts. J Urol. 2009;182:1091–1095. doi: 10.1016/j.juro.2009.05.046. [DOI] [PubMed] [Google Scholar]
- 17.Silverman SG, Pedrosa I, Ellis JH, Hindman NM, Schieda N, Smith AD, Remer EM, Shinagare AB, Curci NE, Raman SS, Wells SA, Kaffenberger SD, Wang ZJ, Chandarana H, Davenport MS. Bosniak classification of cystic renal masses, version 2019: an update proposal and needs assessment. Radiology. 2019;292:475–488. doi: 10.1148/radiol.2019182646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Israel GM, Bosniak M. Follow-up CT of moderately complex cystic lesions of the kidney (Bosniak Category IIF) Am J Roentgenol. 2003;181:627–633. doi: 10.2214/ajr.181.3.1810627. [DOI] [PubMed] [Google Scholar]
- 19.Schoots IG, Zaccai K, Hunink MG, Verhagen PCMS. Bosniak classification for complex renal cysts reevaluated: a systematic review. J Urol. 2017;198:12–21. doi: 10.1016/j.juro.2016.09.160. [DOI] [PubMed] [Google Scholar]
- 20.Nouhaud FX, Bernhard JC, Bigot P, Khene ZE, Audenet F, Lang H, Bergerat S, Fraisse G, Grenier N, Cornelis F, Nedelcu C, Béjar S, Fromont-Hankard G, Allory Y, Lindner V, Verkarre V, Daniel L, Yacoub M, Correas JM, Méjean A, Rioux-Leclercq N, Bensalah K. Contemporary assessment of the correlation between Bosniak classification and histological characteristics of surgically removed atypical renal cysts (UroCCR-12 study) World J Urol. 2018;36:1643–1649. doi: 10.1007/s00345-018-2307-6. [DOI] [PubMed] [Google Scholar]
- 21.Ascenti G, Mazziotti S, Zimbaro G, Settineri N, Magno C, Melloni D, Caruso R, Scribano E. Complex cystic renal masses: characterization with contrast-enhanced US. Radiology. 2007;243:158–165. doi: 10.1148/radiol.2431051924. [DOI] [PubMed] [Google Scholar]
- 22.Oon SF, Foley RW, Quinn D, Quinlan DM, Gibney RG. Contrast-enhanced ultrasound of the kidney: a single-institution experience. Ir J Med Sci. 2017;187(3):795–802. doi: 10.1007/s11845-017-1725-6. [DOI] [PubMed] [Google Scholar]
- 23.Park BK, Kim B, Kim SH, Ko K, Lee HM, Choi HY. Assessment of cystic renal masses based on Bosniak classification: comparison of CT and contrast-enhanced US. Eur J Radiol. 2007;61:310–314. doi: 10.1016/j.ejrad.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Quaia E, Bertolotto M, Cioffi V, Rossi A, Baratella E, Pizzolato R, Cova MA. Comparison of contrast-enhanced sonography with unenhanced sonography and contrast-enhanced CT in the diagnosis of malignancy in complex cystic renal masses. Am J Roentgenol. 2008;191:1239–1249. doi: 10.2214/AJR.07.3546. [DOI] [PubMed] [Google Scholar]