Abstract
Background:
Most of the research data of arthroscopic treatment for femoroacetabular impingement syndrome (FAIS) have been generated from Western populations.
Purpose:
To report the minimum 2-year follow-up results after hip arthroscopy for FAIS in Chinese patients.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 434 hips that underwent primary hip arthroscopy for FAIS between 2016 and 2018 were included. Excluded were patients with previous ipsilateral hip surgery, ipsilateral surgery during the follow-up time, preoperative lateral center-edge angle <25°, Tönnis grade ≥2, sacroiliac joint disease, or incomplete preoperative radiographs or medical records. Preoperative and postoperative patient-reported outcomes (PROs; modified Harris Hip Score [mHHS], Hip Outcome Score–Activities of Daily Living [HOS-ADL], international Hip Outcome Tool, 12-component form [iHOT-12], and visual analog scale [VAS] for pain) were compared with the 2-tailed paired Student t test. Radiographic measures, intraoperative findings, performed procedures, complications, and revision surgery were also reported. The Spearman rank correlation was used to determine the association between patient characteristics and improvement in PRO scores.
Results:
Included were 272 hips with a mean follow-up of 39.4 ± 8.1 months. Overall, 243 hips (89.3%) underwent labral repair. The PROs from baseline to final follow-up were 64.7 to 90.0 for HOS-ADL, 41.1 to 73.4 for iHOT-12, 62.8 to 89.6 for mHHS, and 6.1 to 1.7 for VAS (P < .001 for all). Younger age was correlated significantly with improved iHOT-12 scores (r = -0.230; P < .001), and shorter symptom duration was significantly correlated with improved HOS-ADL (r = -0.190; P = .003), iHOT-12 (r = -0.146; P = .024), and VAS pain (r = -0.143; P = .027) scores. The overall complication and revision hip arthroscopy rates were 4.0% and 3.3% respectively. At the final follow-up, no patient required conversion to total hip arthroplasty (THA).
Conclusion:
At 2 years after hip arthroscopy for FAIS, Chinese patients demonstrated statistically significant improvement in PROs, with a low rate of revision surgery or conversion to THA. Shorter symptom duration and younger age were significantly positively correlated with improvement in PROs.
Keywords: Chinese population, femoroacetabular impingement syndrome, hip arthroscopy, patient-reported outcome
Femoroacetabular impingement syndrome (FAIS) is a notable cause of hip joint pain and limited range of motion of the hip joint, and it is increasingly recognized as a strong risk factor for hip osteoarthritis. 40,42 Hip arthroscopy is recommended to treat this disorder. 26 It is reported that surgical intervention for FAIS has shown a 25-fold increase between 2006 and 2013, and studies published on surgical outcomes increased 2600% between 2004 and 2016. 38 In accordance with this trend, the volume of hip arthroscopy had made significant progress at our center in the past decade.
Favorable outcomes have been reported regarding the surgical treatment of FAIS, 12,25,27,39,43 not only regarding pain and function scores, but also regarding the rate of return to sport, including professional athletes. 8,28,32,42 The majority of these studies concern populations in Western countries, and outcomes in the Asian population have been limited to small sample sizes. 13,16,27 Moon et al 27 reported good outcomes in 73 patients with concomitant labral tears in Korea. Choi et al 5 studied 109 Korean patients with cam impingement and reported improvement in range of motion and symptoms. Lee et al 19 reported good clinical outcomes in 41 Korean patients with FAIS.
We speculated that differences in body size, physical activities, and genetic factors in the Chinese population might affect the results of PROs, complication rates, and secondary surgery rates after hip arthroscopy compared with Western populations. The purpose of this study was to report the minimum 2-year follow-up outcomes of hip arthroscopy for FAIS in Chinese patients.
Methods
Approval for the study was granted by our institutional review board and we obtained informed consent exemptions approved by the ethics committee. A retrospective analysis of patients who underwent primary hip arthroscopy for FAIS between November 2016 and December 2018 was conducted. Patients meeting inclusion criteria had a history of hip pain, physical examination (positive FADIR [flexion adduction internal rotation] or FABER [flexion abduction external rotation] tests), radiographic evidence of FAIS, and a minimum 2 years of follow-up data. Indication for surgery was persistent pain, dysfunction, and failed nonoperative treatment of ≥3 months (physical therapy, oral anti-inflammatory drugs, and/or intra-articular injection). All procedures were performed by 3 senior authors(Y.X., X.Z., J.-Q.W.), whose surgical volume exceeded 50 hips per year. Exclusion criteria included history of previous ipsilateral hip surgery, contralateral hip surgery during the follow-up time, preoperative lateral center-edge angle (LCEA) <25°, moderate to advanced osteoarthritis (Tönnis grade ≥2), sacroiliac joint disease, and incomplete preoperative radiographs and medical record. A total of 434 hips underwent arthroscopic procedures. The inclusion criteria were met in 338 hips, of which 272 hips (80.4%) had a minimum 2-year follow-up and were enrolled in the study (Figure 1).
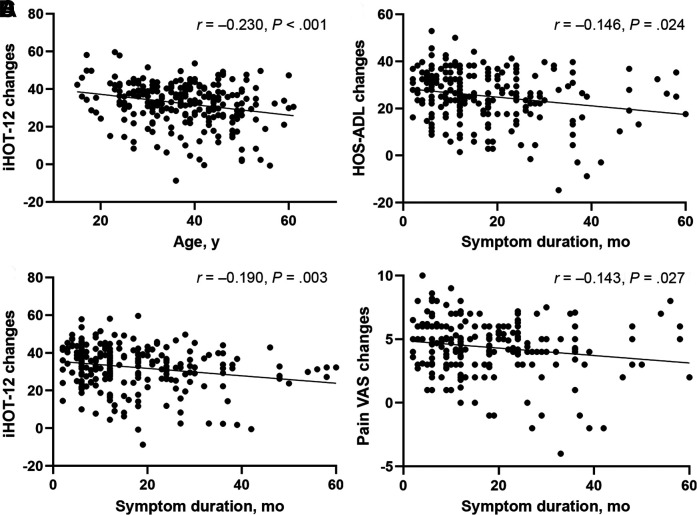
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) diagram indicating the total patient population that met the inclusion criteria and did not meet any of the exclusion criteria.
Surgical Technique
The patient was placed in the modified supine position on a standard hip traction table and the perineum was protected while performing operated limb traction. 36 An anterolateral portal was established under fluoroscopic guidance using a spinal needle. Next, anterior and midanterior portals were made under direct visualization with a 70° arthroscope. 17 An interportal capsulotomy was performed between these portals to allow for improved visualization and a detailed inspection of the central compartment. Most pathologies in the central compartment could be addressed with these portals, including pincer deformity, labral injury, and chondrolabral injury. Labral debridement, repair, or reconstruction were selected depending on the condition of the labrum.
Labral tears were repaired with suture anchor fixation (Smith & Nephew) when possible. According to preoperative imaging and intraoperative fluoroscopy, acetabuloplasty was performed with a motorized bur and involved minimally burred to produce a bleeding bone bed for labral healing. Then the suture anchors were placed to reattach the labrum. Extensive labral calcification, insufficient viable labral tissue (<6 mm), and iatrogenic labral insufficiency was considered irreparable. 6 Labral reconstruction with iliotibial band or gracilis autograft from the operative side was considered in the case of an irreparable labral tear. 4,24
Chondroplasty was performed for partial-thickness cartilage lesions and chondral flaps with an arthroscopic shaver and/or electrocautery device (Smith & Nephew). 9 Subspine impingement was diagnosed using preoperative imaging and confirmed by preoperative subspine blocking test guided by ultrasound. Generally, the subspine deformity is resected back to the level of the acetabular sourcil. After fully addressing the pathologies in the central compartment, the arthroscope was moved into the peripheral compartment for decompression of the cam deformity using a high-speed bur (Smith & Nephew). Dynamic examination and fluoroscopic imaging were used to confirm adequate resection of the cam deformity. The capsule was routinely repaired at the end of the procedure with a nonabsorbable Orthocord suture (DePuy Mitek).
Postoperative Rehabilitation
All patients followed a standardized prescribed rehabilitation protocol under the direct supervision of our physical therapy team. Rehabilitation took an average of 4 to 5 months. Briefly, the first phase comprised isometric contractions (the ankle pump, quadriceps, and hip joint muscle isometric contraction exercises) and passive range of motion exercises at 1 to 2 days postoperatively. Partial weightbearing was allowed 3 to 7 days postoperatively. The second phase focused on maintaining a regular gait and restoring a full range of motion, including adduction, abduction, and pronation at 2 to 6 weeks postoperatively. The third phase was about regaining lower extremity strength as well as normal functional activities at 8 to 12 weeks postoperatively. The final phase focused on resuming preinjury higher-level activities.
Radiographic Measurements
All included patients had undergone preoperative anteroposterior (AP) pelvis and 45° Dunn lateral radiography and unilateral hip computed tomography (CT) and magnetic resonance imaging (MRI). Radiographic measurements were performed using a picture archiving and communication system (GE Healthcare). The LCEA angle and joint space were measured on AP pelvis radiographs. The alpha angle was measured on 45° Dunn lateral radiographs, with an alpha angle >55° indicating cam impingement. 29 The LCEA angle was measured on AP pelvis radiographs, with an LCEA angle >40° indicating pincer impingement. 44 Three-dimensional CT was used for preoperative and postoperative cam deformity evaluation. Plain MRI was used to evaluate the status of labral and articular cartilage. All radiographic data were evaluated by a single musculoskeletal radiologist with >15 years of radiological diagnosis experience.
Outcome Measures
The following patient-reported outcomes (PROs) were used to evaluate function: the modified Harris Hip Score (mHHS), 3 the Hip Outcome Score–Activities of Daily Living (HOS-ADL), 21 international Hip Outcome Tool, 12-component form (iHOT-12), 23 and the visual analog scale (VAS) for pain. 22 The minimal clinically important difference (MCID) and Patient Acceptable Symptom State (PASS) were also calculated to determine meaningful outcome improvement. 20 HOS–Sports Subscale was not included in this study because nearly half of the patients reported that they did not have regular exercise routines. The following published PASS cutoffs were used: 1.91 for VAS pain, 83.3 for mHHS, 88.2 for HOS-ADL, and 72.2 for iHOT-12. The MCID thresholds were 1.5 points for VAS pain, 8.7 points for mHHS, 8.3 points for HOS-ADL, and 13.0 points for iHOT-12. 2,23,31 Complications included chondrolabral injury, traction-related neurapraxia and perineal numbness, extravasation of fluid into the intra-abdominal compartments, infection, thromboembolic disease, and heterotopic ossification. 11
Statistical Analysis
All data were inspected to determine whether all parametric statistical assumptions were met. In cases of violation of parametric statistical assumptions, nonparametric testing was used for analysis. The 2-tailed paired Student t test was used to compare pre- and postoperative PRO scores. The Spearman rank correlation was used to determine the associations between patient characteristics and change in PRO score. SPSS Version 26 (IBM) was used for all statistical analyses. Differences with a P value <.05 were considered statistically significant.
An a priori power analysis using G*Power (Version 3.1, Franz Faul, University of Kiel, Kiel, Germany) was performed to determine sample size. Based on the assumption that a mean difference of 8.3 points in follow-up mHHS is clinically important according to Jimenez et al, 15 an adequate sample size was determined to be 34 patients, using alpha at .05 and beta at 0.2 (80% power).
Results
Patient Characteristics and Radiographic Findings
Of the 272 included hips, 123 (45.2%) were from female patients. The mean follow-up was 39.4 ± 8.1 months. The mean age and body mass index (BMI) were 37.2 ± 10.0 years and 23.4 ± 3.1, respectively. Combined cam- and pincer-type FAIS was found in 211 hips (77.6%), 52 hips (19.1%) had isolated cam-type FAIS, and only 9 hips (3.3%) had isolated pincer-type FAIS. Patient demographics and radiographic data are summarized in Table 1.
Table 1.
Characteristics of the Study Cohort (N = 272 hips) a
| Variable | Value |
|---|---|
| Age, years | 37.2 ± 10.0 |
| BMI | 23.4 ± 3.1 |
| Sex, female | 123 (45.2) |
| Laterality, right side | 140 (51.5) |
| Follow-up time, months | 39.4 ± 8.1 |
| Symptom duration, months | 18.0 ± 15.5 |
| Tönnis grade | |
| Grade 0 | 169 (62.1) |
| Grade 1 | 103 (37.9) |
| Alpha angle, deg, preoperative | 65.5 ± 8.0 |
| Alpha angle, deg, postoperative | 44.0 ± 5.3 |
| LCEA, deg, preoperative | 32.7 ± 6.5 |
| LCEA, deg, postoperative | 30.8 ± 5.4 |
| Joint space, mm | 4.6 ± 0.8 |
| Revision surgery | 9 (3.3) |
a Values are presented as mean ± SD or No. of hips (%). BMI, body mass index; LCEA, lateral center-edge angle.
Intraoperative Findings and Performed Procedures
The findings and procedures performed during arthroscopic surgery are summarized in Table 2. Overall, the majority of the study population underwent labral repair (89.3%), femoroplasty (96.7%), and acetabular rim trimming (80.9%).
Table 2.
Intraoperative Findings and Procedures a
| No. of Hips (%) | |
|---|---|
| Femoral head chondral lesion: Outerbridge classification | 35 (12.9) |
| Grade 1 | 4 (1.5) |
| Grade 2 | 18 (6.6) |
| Grade 3 | 10 (3.7) |
| Grade 4 | 3 (1.1) |
| Acetabulum chondral lesion: ALAD classification | 248 (91.2) |
| Grade 1 | 31 (11.4) |
| Grade 2 | 95 (34.9) |
| Grade 3 | 90 (33.1) |
| Grade 4 | 56 (20.6) |
| Labral | |
| Debridement | 18 (6.6) |
| Repair | 243 (89.3) |
| Reconstruction | 11 (4.0) |
| Femoroplasty | 263 (96.7) |
| Acetabuloplasty | 220 (80.9) |
| LT partial debridement | 18 (6.6) |
| Subspine decompression | 17 (6.3) |
a ALAD, acetabular labral articular disruption; LT, ligamentum teres.
Patient-Reported Outcomes
In patients who underwent labral repair (243 hips), most demonstrated significant improvement in PROs at the final follow-up compared with preoperative levels. The score improvement from baseline to final follow-up was 64.7 to 90.0 for HOS-ADL (P < .001), 41.1 to 73.4 for iHOT-12 (P < .001), 62.8 to 89.6 for mHHS (P < .001), and 6.1 to 1.7 for VAS (P < .001). The probabilities of achieving MCID and PASS are summarized in Table 3. The mHHS showed the highest probability for capturing MCID and PASS improvement, with 95.0% achieving MCID and 79.0% achieving PASS.
Table 3.
Patient-Reported Outcomes After Hip Arthroscopy in Patients With Labral Repair (n = 243 hips) a
| Preoperative | Postoperative | P | MCID | PASS | |
|---|---|---|---|---|---|
| mHHS | 62.8 ± 7.6 | 89.6 ± 9.2 | <.001 | 95.0 | 79.0 |
| iHOT-12 | 41.1 ± 6.7 | 73.4 ± 11.0 | <.001 | 93.0 | 58.0 |
| HOS-ADL | 64.7 ± 8.6 | 90.0 ± 8.9 | <.001 | 93.0 | 71.0 |
| VAS pain | 6.1 ± 1.4 | 1.7 ± 1.5 | <.001 | 93.0 | 55.0 |
a Values are presented as mean ± SD or %. HOS-ADL, Hip Outcome Score–Activities of Daily Living; iHOT-12, international Hip Outcome Tool, 12-component form; MCID, minimum clinically important difference; mHHS, modified Harris Hip Score; PASS, Patient Acceptable Symptom State; VAS, visual analog scale.
Factors Associated With PRO Improvement
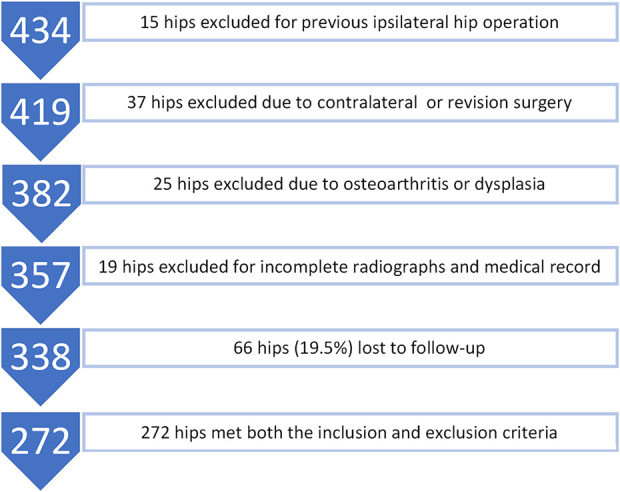
Younger age was significantly correlated with improvement in iHOT-12 scores (P < .001), and shorter symptom duration was significantly correlated with the improvement in HOS-ADL, iHOT-12, and VAS pain scores (P = .024, .003, and .027, respectively) (Table 4 and Figure 2). BMI and sex were not significantly correlated with changes in PROs.
Table 4.
Correlation Between Change in PROs and Patient Characteristics a
| BMI | Sex | Age | Symptom Duration | |||||
|---|---|---|---|---|---|---|---|---|
| r | P | r | P | r | P | r | P | |
| mHHS | −0.080 | NS | 0.065 | NS | −0.019 | NS | −0.124 | NS |
| iHOT-12 | −0.097 | NS | −0.108 | NS | −0.230 | <.001 | −0.190 | .003 |
| HOS-ADL | 0.124 | NS | −0.009 | NS | −0.051 | NS | −0.146 | .024 |
| VAS pain | −0.003 | NS | −0.028 | NS | −0.154 | NS | −0.143 | .027 |
a BMI, body mass index; HOS-ADL, Hip Outcome Score–Activities of Daily Living; iHOT-12, international Hip Outcome Tool, 12-component form; mHHS, modified Harris Hip Score; NS, not significant; VAS, visual analog scale. Bold P values indicate a statistically significant difference between groups compared.
Figure 2.
Significant associations were seen between (A) patient age and changes in iHOT-12 and (B) symptom duration and changes in HOS-ADL, iHOT-12, and pain VAS. iHOT-12, International Hip Outcome Tool, 12-component form; HOS-ADL, Hip Outcome Score–Activities of Daily Living; VAS, visual analog scale.
Complications and Secondary Surgery
The overall complication rate was 4.0%; 3 patients had transient femoral cutaneous nerve palsy and 2 patients had lower limb venous thrombosis. Six patients had imaging evidence of heterotopic ossification 37 : 3 hips were classified as Brooker stage 1, 2 hips as Brooker stage 2, and 1 hip as Brooker stage 3. There were no infections at the final follow-up.
At the final follow-up, 9 hips (3.3%) had undergone revision hip arthroscopy. Five of these patients had residual cam deformity and gradual onset of symptoms. These patients required revision cam osteochondroplasty. Three patients underwent revision arthroscopy due to subspine impingement, and 1 patient underwent revision surgery due to heterotopic ossification. No patient required conversion to total hip arthroplasty (THA) at the final follow-up.
Discussion
The study results showed that all PRO scores improved significantly from baseline to final follow-up (P < .001 for all). Younger age was significantly correlated with the improvement of iHOT-12 (r = -0.230; P < .001), and shorter symptom duration was significantly correlated with the improvement of HOS-ADL (r = -0.190; P = .003), iHOT-12 (r = -0.146; P = .024;), and VAS score (r = -0.143; P = .027). A majority of Chinese patients with FAIS were able to attain clinically significant outcomes at 2 years after arthroscopic surgery, with a low rate of revision surgery and no conversions to THA.
Moon et al 27 reported the 2-year follow-up of 73 patients in Korea, and no revision surgery or THA was required after hip arthroscopy for FAIS. These results differ from studies conducted in Western populations, where the incidence of conversion to THA was 4% to 7.7%. 12,27,39 Increased age, high BMI, and revision procedures were suggested as risk factors for conversion to THA in previous studies. 12,33,35 The mean BMI of the patients in the present study was 23.3, which is less than previous studies conducted in Western populations. 33 The mean age in this study was 37.2, similar to in Western countries. 25 Moreover, Nevitt et al 30 reported that hip osteoarthritis in Chinese patients was 80% to 90% less frequent than in White patients in the United States. All the above factors might result in a low rate of revision and conversion to THA in the present study.
A population-based study in Japan reported that the prevalence of cam-type and pincer type FAIS were 4.2% and 20.3%, respectively. Pincer type was more common than cam type. 13 However, only 9 hips (3.3%) had isolated pincer-type and 52 hips (18.4%) had cam-type FAIS in our study. Part of the explanation for the disparity in cam-type FAIS is that alpha angle was measured on AP pelvic radiographs in their study. Alpha angle was measured on 45° Dunn lateral radiographs in the present study, as the 1:30 and 2:00 clockface positions are the common locations for cam deformity. 41 The reason for the disparity in pincer-type FAIS might be that pincer deformity was more common in asymptomatic hips. A systematic review of the imaging prevalence of FAIS found that pincer deformity was 67% and cam deformity was 37% in asymptomatic volunteers. 10
In the analysis of the factors related to the increase of the PROs, BMI was not significantly correlated with the improvement in PROs. BMI has been considered a risk factor for the poor prognosis after hip arthroscopy. Parvaresh et al 33 reported the normal-weight patients demonstrated universal improvement in all PROs and a significantly greater likelihood of achieving the PASS and the substantial clinical benefit level compared with obese patients. The prevalence of obesity in China was much lower than that in Western countries. It is inconclusive whether high BMI is a poor prognostic indicator in Chinese patients, since the prevalence in the overall general population is low, which was reflected in this study.
Age was significantly negatively correlated with the improvement of iHOT-12 scores in our study. This result was consistent with previous studies in Western countries. 7 Although hip arthroscopy had demonstrated statistically significant PRO improvements in the elderly population in some studies, 14,34 surgeons should use rigorous selection criteria in the aged population.
Shorter symptom duration was significantly correlated with the improvement of HOS-ADL, iHOT-12, and VAS scores. Kunze et al 18 reported that surgical intervention early after the onset of symptoms was associated with superior postoperative outcomes when compared with patients who underwent surgical intervention beyond this time frame. Aprato et al 1 also reported significantly better outcomes for patients who underwent surgery within 6 months of symptom onset compared with those who waited longer. This information suggests a beneficial influence for early arthroscopic intervention and might help guide preoperative decision making regarding the delay of surgery.
Limitations
This study has certain limitations. First, it is a single-center case series study with no control group, so the result may not be generalizable to all Chinese patients. Second, because this was a retrospective study, there was an inherent bias. Third, there were no obese patients in this cohort, which may produce variations in the results if otherwise. Fourth, as this was a short-term follow-up study, revision cases may increase with longer follow-up, but the overall revision surgery rates might still be relatively low.
Conclusion
Hip arthroscopy for the FAIS in Chinese patients demonstrated statistically significant improvements on PROs at minimum 2-year follow-up, with a low rate of revision surgery. Moreover, shorter symptom duration before surgery and younger age were significantly positively correlated with the improved PRO scores after surgery.
Footnotes
Final revision submitted August 16, 2022; accepted August 30, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by funding from the National Natural Science Foundation of China (grants 82072403 and 81902205). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Peking University Third Hospital (ref No. M2019193).
References
- 1. Aprato A, Jayasekera N, Villar R. Timing in hip arthroscopy: does surgical timing change clinical results? Int Orthop. 2012;36(11):2231–2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Beck EC, Nwachukwu BU, Mehta N, et al. Defining meaningful functional improvement on the visual analog scale for satisfaction at 2 years after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2020;36(3):734–742.e732. [DOI] [PubMed] [Google Scholar]
- 3. Byrd JWT. Hip arthroscopy: patient assessment and indications. Instr Course Lect. 2003;52:711–719. [PubMed] [Google Scholar]
- 4. Chahla J, Soares E, Bhatia S, Mitchell JJ, Philippon MJ. Arthroscopic technique for acetabular labral reconstruction using iliotibial band autograft. Arthrosc Tech. 2016;5(3):e671–e677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Choi SM, Park MS, Ju BC, Yoon SJ. Alterations in range of motion and clinical outcomes after femoroplasty in Asians. J Am Acad Orthop Surg. 2018;26(8):e181–e190. [DOI] [PubMed] [Google Scholar]
- 6. Cooper JD, Dekker TJ, Ruzbarsky JJ, Pierpoint LA, Soares RW, Philippon MJ. Autograft versus allograft: the evidence in hip labral reconstruction and augmentation. Am J Sports Med. 2021;49(13):3575–3581. [DOI] [PubMed] [Google Scholar]
- 7. Domb BG, Chen SL, Go CC, et al. Predictors of clinical outcomes after hip arthroscopy: 5-year follow-up analysis of 1038 patients. Am J Sports Med. 2021;49(1):112–120. [DOI] [PubMed] [Google Scholar]
- 8. Domb BG, Martin TJ, Gui C, Chandrasekaran S, Suarez-Ahedo C, Lodhia P. Predictors of clinical outcomes after hip arthroscopy: a prospective analysis of 1038 patients with 2-year follow-up. Am J Sports Med. 2018;46(6):1324–1330. [DOI] [PubMed] [Google Scholar]
- 9. Ellis HB, Briggs KK, Philippon MJ. Innovation in hip arthroscopy: is hip arthritis preventable in the athlete? Br J Sports Med. 2011;45(4):253–258. [DOI] [PubMed] [Google Scholar]
- 10. Frank JM, Harris JD, Erickson BJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015;31(6):1199–1204. [DOI] [PubMed] [Google Scholar]
- 11. Gupta A, Redmond JM, Hammarstedt JE, Schwindel L, Domb BG. Safety measures in hip arthroscopy and their efficacy in minimizing complications: a systematic review of the evidence. Arthroscopy. 2014;30(10):1342–1348. [DOI] [PubMed] [Google Scholar]
- 12. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? 2-year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44(1):74–82. [DOI] [PubMed] [Google Scholar]
- 13. Hasegawa M, Morikawa M, Seaman M, Cheng VK, Sudo A. Population-based prevalence of femoroacetabular impingement in Japan. Mod Rheumatol. 2021;31(4):899–903. [DOI] [PubMed] [Google Scholar]
- 14. Honda E, Utsunomiya H, Hatakeyama A, et al. Patients aged in their 70s do not have a high risk of progressive osteoarthritis following arthroscopic femoroacetabular impingement correction and labral preservation surgery. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1648–1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jimenez AE, Monahan PF, Miecznikowski KB, et al. Achieving successful outcomes in high-level athletes with borderline hip dysplasia undergoing hip arthroscopy with capsular plication and labral preservation: a propensity-matched controlled study. Am J Sports Med. 2021;49(9):2447–2456. [DOI] [PubMed] [Google Scholar]
- 16. Jo S, Lee SH, Jang SW, et al. Time taken to resume driving following hip arthroscopy. BMC Musculoskelet Disord. 2020;21(1):643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21(12):1496–1504. [DOI] [PubMed] [Google Scholar]
- 18. Kunze KN, Beck EC, Nwachukwu BU, Ahn J, Nho SJ. Early hip arthroscopy for femoroacetabular impingement syndrome provides superior outcomes when compared with delaying surgical treatment beyond 6 months. Am J Sports Med. 2019;47(9):2038–2044. [DOI] [PubMed] [Google Scholar]
- 19. Lee JW, Hwang DS, Kang C, Hwang JM, Chung HJ. Arthroscopic repair of acetabular labral tears associated with femoroacetabular impingement: 7-10 years of long-term follow-up results. Clin Orthop Surg. 2019;11(1):28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Levy DM, Kuhns BD, Chahal J, Philippon MJ, Kelly BT, Nho SJ. Hip arthroscopy outcomes with respect to patient acceptable symptomatic state and minimal clinically important difference. Arthroscopy. 2016;32(9):1877–1886. [DOI] [PubMed] [Google Scholar]
- 21. Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy. 2006;22(12):1304–1311. [DOI] [PubMed] [Google Scholar]
- 22. Martin RL, Kivlan BR, Christoforetti JJ, et al. Minimal clinically important difference and substantial clinical benefit values for a pain visual analog scale after hip arthroscopy. Arthroscopy. 2019;35(7):2064–2069. [DOI] [PubMed] [Google Scholar]
- 23. Martin RL, Kivlan BR, Christoforetti JJ, et al. Defining variations in outcomes of hip arthroscopy for femoroacetabular impingement using the 12-item International Hip Outcome Tool (iHOT-12). Am J Sports Med. 2020;48(5):1175–1180. [DOI] [PubMed] [Google Scholar]
- 24. Matsuda DK, Burchette RJ. Arthroscopic hip labral reconstruction with a gracilis autograft versus labral refixation: 2-year minimum outcomes. Am J Sports Med. 2013;41(5):980–987. [DOI] [PubMed] [Google Scholar]
- 25. Menge TJ, Briggs KK, Dornan GJ, McNamara SC, Philippon MJ. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: labral debridement compared with labral repair. J Bone Joint Surg Am. 2017;99(12):997–1004. [DOI] [PubMed] [Google Scholar]
- 26. Minkara AA, Westermann RW, Rosneck J, Lynch TS. Systematic review and meta-analysis of outcomes after hip arthroscopy in femoroacetabular impingement. Am J Sports Med. 2019;47(2):488–500. [DOI] [PubMed] [Google Scholar]
- 27. Moon JK, Yoon JY, Kim CH, Lee S, Kekatpure AL, Yoon PW. Hip arthroscopy for femoroacetabular impingement and concomitant labral tears: a minimum 2-year follow-up study. Arthroscopy. 2020;36(8):2186–2194. [DOI] [PubMed] [Google Scholar]
- 28. Mullins K, Filan D, Carton P. Arthroscopic correction of sports-related femoroacetabular impingement in competitive athletes: 2-year clinical outcome and predictors for achieving minimal clinically important difference. Orthop J Sports Med. 2021;9(3):2325967121989675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Musielak BJ, Kubicka AM, Woźniak Ł, Jóźwiak M, Liu RW. Is cam morphology found in ancient and medieval populations in addition to modern populations? Clin Orthop Relat Res. 2021;479(8):1830–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nevitt MC, Xu L, Zhang Y, et al. Very low prevalence of hip osteoarthritis among Chinese elderly in Beijing, China, compared with whites in the United States: the Beijing osteoarthritis study. Arthritis Rheum. 2002;46(7):1773–1779. [DOI] [PubMed] [Google Scholar]
- 31. Nwachukwu BU, Beck EC, Kunze KN, et al. Defining the clinically meaningful outcomes for arthroscopic treatment of femoroacetabular impingement syndrome at minimum 5-year follow-up. Am J Sports Med. 2020;48(4):901–907. [DOI] [PubMed] [Google Scholar]
- 32. O’Connor M, Minkara AA, Westermann RW, Rosneck J, Lynch TS. Return to play after hip arthroscopy: a systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2780–2788. [DOI] [PubMed] [Google Scholar]
- 33. Parvaresh K, Rasio JP, Wichman D, Chahla J, Nho SJ. The influence of body mass index on outcomes after hip arthroscopy for femoroacetabular impingement syndrome: five-year results in 140 patients. Am J Sports Med. 2021;49(1):90–96. [DOI] [PubMed] [Google Scholar]
- 34. Perets I, Chaharbakhshi EO, Mu B, et al. Hip arthroscopy in patients ages 50 years or older: minimum 5-year outcomes, survivorship, and risk factors for conversion to total hip replacement. Arthroscopy. 2018;34(11):3001–3009. [DOI] [PubMed] [Google Scholar]
- 35. Perets I, Chaharbakhshi EO, Shapira J, Ashberg L, Mu BH, Domb BG. Hip arthroscopy for femoroacetabular impingement and labral tears in patients younger than 50 years: minimum five-year outcomes, survivorship, and risk factors for reoperations. J Am Acad Orthop Surg. 2019;27(4):e173–e183. [DOI] [PubMed] [Google Scholar]
- 36. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299–308. [DOI] [PubMed] [Google Scholar]
- 37. Rath E, Sherman H, Sampson TG, Ben Tov T, Maman E, Amar E. The incidence of heterotopic ossification in hip arthroscopy. Arthroscopy. 2013;29(3):427–433. [DOI] [PubMed] [Google Scholar]
- 38. Reiman MP, Peters S, Sylvain J, Hagymasi S, Ayeni OR. Prevalence and consistency in surgical outcome reporting for femoroacetabular impingement syndrome: a scoping review. Arthroscopy. 2018;34(4):1319–1328.e1319. [DOI] [PubMed] [Google Scholar]
- 39. Sansone M, Ahldén M, Jónasson P, et al. Outcome after hip arthroscopy for femoroacetabular impingement in 289 patients with minimum 2-year follow-up. Scand J Med Sci Sports. 2017;27(2):230–235. [DOI] [PubMed] [Google Scholar]
- 40. Thomas DD, Bernhardson AS, Bernstein E, Dewing CB. Hip arthroscopy for femoroacetabular impingement in a military population. Am J Sports Med. 2017;45(14):3298–3304. [DOI] [PubMed] [Google Scholar]
- 41. Uemura K, Atkins PR, Anderson AE, Aoki SK. Do your routine radiographs to diagnose cam femoroacetabular impingement visualize the region of the femoral head-neck junction you intended? Arthroscopy. 2019;35(6):1796–1806. [DOI] [PubMed] [Google Scholar]
- 42. Wolfson TS, Ryan MK, Begly JP, Youm T. Outcome trends after hip arthroscopy for femoroacetabular impingement: when do patients improve? Arthroscopy. 2019;35(12):3261–3270. [DOI] [PubMed] [Google Scholar]
- 43. Yang F, Mamtimin M, Duan Y-P, et al. Volume of gluteus maximus and minimus increases after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2021;37(3):862–870. [DOI] [PubMed] [Google Scholar]
- 44. Zhou J, Melugin HP, Hale RF, et al. The prevalence of radiographic findings of structural hip deformities for femoroacetabular impingement in patients with hip pain. Am J Sports Med. 2020;48(3):647–653. [DOI] [PubMed] [Google Scholar]