Abstract
Background
Online health data collection has gained a reputation over the last years to record and process information about health issues for implementing digital health.
Objective
The research aim was to appraise two online methods (open and rewarded) to collect information about HRQoL and nutritional well-being and to compare the results between both surveyed populations.
Methods
This cross-sectional study is framed on the NUTRiMDEA project. Online data through two different web-based methods (open survey and rewarded survey) were retrieved to assemble data related to sociodemographic, lifestyle (diet, physical activity and sleep patterns) and general health aspects, as well as HRQoL by an evidence-based form such as the SF-12 questionnaire, the IPAQ survey, and MEDAS-14, participants were adults (>18 years old).
Results
Overall, 17,332 participants responded to the open survey (OS, n = 11,883) or the rewarded survey (RS, n = 5449). About 65.1% of the participants were female, while the mean age was in the range of 40–70 years. There were significant differences (p < 0.05) between surveyed populations in sociodemographic, lifestyle (diet and physical activity), health and HRQoL data.
Conclusions
This investigation implemented an evidence-based online questionnaire that collected demographic, lifestyle factors, phenotypic and health-related aspects as well as compared differential outcomes in HRQoL and nutritional/lifestyle well-being depending on the online mode data collection. Findings demonstrated dissimilarities in most aspects of health, HRQoL, dietary intake and physical activity records between both populations. Overall, OS sample was characterized as a healthier population with superior lifestyle habits than RS participants.
Keywords: Online data collection, health-related quality of life, nutritional well-being, web-based health, eHealth, digital health
Introduction
Individual and population health and well-being are not only determined by the absence of disease but also by socioeconomic, environmental, educational and cultural factors, as well as daily habits.1,2 Furthermore, lifestyle could be considered as the most relevant and modifiable factor, with an impact on health.3 In this context, health-related quality of life (HRQoL) has been described as a subjective perception about the influence of health and personal features on human well-being.4 Quality of life (QoL) has been defined as “A conscious cognitive judgment of satisfaction with one's life” and also as “An individuals” perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns; therefore, focusing on aspects not only related to one's own health.5 Interestingly, a pioneer categorization of nutritional well-being and health status into qualitative (proto)nutritypes allowed to develop a pilot quantitative nutrimeter to objectively integrate nutritional information, which evidenced the association with quality of life6 for precision public health actions. Also, validated tools are available to assess diet quality and physical activity.7,8
Prevention of non-communicable diseases (NCDs) will increase the number and proportion of people who age healthily and avoid health surplus care costs.9 Strategies for NCDs prevention are a priority worldwide that include the adoption of a healthy lifestyle through a balanced diet quality and physical activity, also avoid harmful habits such as smoking and an excessive alcohol intake,9 whose precision knowledge at individual level and community may contribute to develop health care services and to implement well-being programs.3 In this context, the use of eHealth for patient monitoring and follow-up is a growing sector.10,11
Available data reveal that the use of information and communication technologies (ICTs) is increasing; broadband internet access was used by 88% of the households in the European Union in 2019, 33% points higher than in 2009 (55%).12 Therefore, the use of digital technologies for the implementation of health strategies and interventions could offer additional advantages to conventional approaches and tools.13 Indeed, online data collection has gained popularity compared to traditional paper-based surveys.14 Internet methods allow contact with larger groups and populations and are less costly and more scalable.15,16 Any person through a link or an app can respond to health surveys easily and immediately.14 There are questionnaires that evaluate from alcohol dependence disorders, gambling addiction, anxiety symptoms, and depression symptoms to eating or physical activity behaviors; as the 14-item Questionnaire of Mediterranean diet adherence or the International Physical Activity Questionnaire.
Diet and health counseling can be provided through a number of different ways, including face-to-face or online: through group or individual sessions in physical or virtual consultation (over the phone or video call, by e-mails or text messages), and can therefore be offered verbally and/or in written form.15,17,18 Although a consumer preference for face-to-face dietary counseling has been classically described,19 interest in web-based dietary counseling and personalized nutrition (PN), in particular, is rising.15 Thus, a European endeavor showed a positive attitude of consumers toward personalized advice on nutrition based on their genetic profile.20
Different intervention studies have already been carried out through eHealth, for example, in a meta-analysis, the effectiveness of eHealth interventions to prevent or treat childhood overweight and obesity is analyzed, with discrete results in the improvement of diet or physical activity.21 The effectiveness of eHealth interventions to improve adherence to treatment in adults with obstructive sleep apnea has also been assessed in a meta-analysis, with positive short-term results, but no long-term data.22 The promotion of physical activity in older people in the context of the COVID-19 pandemic has even been studied using eHeatlh, concluding that there is low to moderate evidence that interventions delivered via mHealth or eHealth approaches may be effective in increasing physical activity in older adults in the short term.23 Also, modest evidence was found in a systematic review about digital-only interventions having a positive impact on employee health for a broad range of outcomes such as sleep, mental health, sedentary behaviors and physical activity levels.24 Therefore, it is recommended to carry out longer and quality eHealth studies, which transform successful components from face-to-face interventions into an eHealth format.25,26
Given the differences between the distinct populations that can be reached through different ways, it is important to know how to achieve the target population, to study or in which to carry out the intervention. This knowledge will certainly contribute to decision-making approaches by increasing the health of the participants and reducing the risk of developing future chronic diseases as well as to facilitate the implementation of precision medicine and public health strategies and policies. As it has been exposed, there are many tracks to reach and interact with the public, from physical formats (magazines, newspapers, visits), as well as online methods (e-mail, web pages, online newspapers or paid survey platforms), being online methods where the system is booming. Therefore, in summary, the main objective of this study is firstly to value and compare two online survey methods (open and rewarded access) and secondly to analyze differential information about HRQoL and nutritional/lifestyle well-being in both population samples.
Methods
This study is framed on the NUTRiMDEA project, which aims to analyze online information about HRQoL and nutritional/lifestyle well-being, oriented to precision nutrition and public health advice.
The questionnaire(s)
The survey was based on previously validated questionnaires including HRQoL27 and well-being features.6 Correlations and reliability of web-based self-reported sociodemographic and anthropometric data have already been validated in Food4Me project28 and SUN Cohort.29
The survey consisted of different types of questionnaires, distributed into several sections: health/disease, dietary data, physical activity, HRQoL and lifestyle perceptions. One of the sections collected information on sociodemographic variables (sex, age range, educational level, smoking, hours and sleep routine among others), anthropometric (measurements of weight and height, t-shirt and pants size) and variables related to health and disease (medical diagnosis of chronic diseases: obesity, diabetes, dyslipidemia, high blood pressure, and family diseases). Another section encompassed the 14-item Mediterranean Diet Adherence Screener (MEDAS-14) from the project Prevention with Mediterranean Diet (PREDIMED), which collects the consumption of olive oil, vegetables, fruits, legumes, poultry, red and processed meats, butter, beverages, red wine, fish, pastries and nuts; final score ranges from 0 to 14 points.30–32 This FFQ surrogate is commonly used in epidemiological studies as it allows to report habitual food consumption with limited resources.33 A high reproducibility of a validated FFQ has been demonstrated for Spanish participants who answered the questionnaire twice in a period of less than 1 year.33 Physical activity and sitting time were collected by the International Physical Activity Questionnaire (IPAQ) validated for Spanish population,8,34 which allowed to estimate light, moderate and intense activity minutes per week. Total METs per week (METs-h/wk) were also calculated with such a questionnaire. Another section was the Spanish version of the Short Form-12 Health Survey (SF-12),27 which is a validated subset of the Short Form 36 (SF-36) that measures the same eight domains (physical functioning, physical role limitation, pain, general health, vitality, social functioning, emotional role limitations and general perception of health), with reduced length and yields two different global scores: Physical Component Summary (PCS12) and Mental Component Summary (MCS12) scaled from 0 to 100 (high score indicates good health).35 Traditionally, HRQoL has been assessed through self-administered questionnaires, which have been adapted and validated for different populations.27,35–39 All dimensions are hypothetically influenced by nutrition and lifestyle, whose measurement estimated the role of these factors in HRQoL.6
Adiposity was calculated through the body mass index (BMI), to categorize individuals according to the WHO classification as follows: underweight <18.5 kg/m2, normal weight 18.5 to <25 kg/m2, overweight 25 to <30 kg/m2 and obesity 30 kg/m2.40 Also, shirt and pants sizes as indirect proxies of complexion were recorded.
All these questionnaires were administered for both samples of the population in two different settings but the questions and sequence were same. The first scenario, an open survey (OS) through a web-based platform tailored to online surveys (QuestionPro), freely accessible through the website of NUTRiMDEA study,41 publicly deferred by different communication channels (radio, digital newspapers, social media…). The second scenario involved that audiences purchased from different online survey tools (Survey Planet, QuestionPro panel, Zoho Survey, Netquest). In the latter scenario, respondents are rewarded by the chosen platforms (RS). Upon questionnaire completion, participants of the OS obtained an automatic result of their health parameters, such as their BMI, total diet score, level of physical activity and learned some brief recommendations based on their results to improve it.
Participants
The inclusion criteria of the study were based on the acceptance of participation in the survey, being over 18 years of age, Spanish speaker and consenting to the use of the data provided for scientific purposes. Interested participants were directed to the study website to complete the online questionnaire.
All information collected is completely anonymous, only the IP addresses were administered to avoid survey completion more than once from the same IP address. However, this did not guarantee that the questionnaire could be completed more than once from different IP addresses by the same person in the case of the open survey, neither a small overlying among both surveys, but could be estimated as negligible. The completed questionnaires are finally encrypted and stored in local servers for exclusive access by the study researchers.
The NUTRiMDEA survey included a disclaimer informing the participants about this information and acquiescent that submitting the questionnaire constitutes acceptance of the use of their anonymity data for scientific purposes. This statement was positively accepted by the IMDEA CEI and the companies in charge of the rewarded surveys.
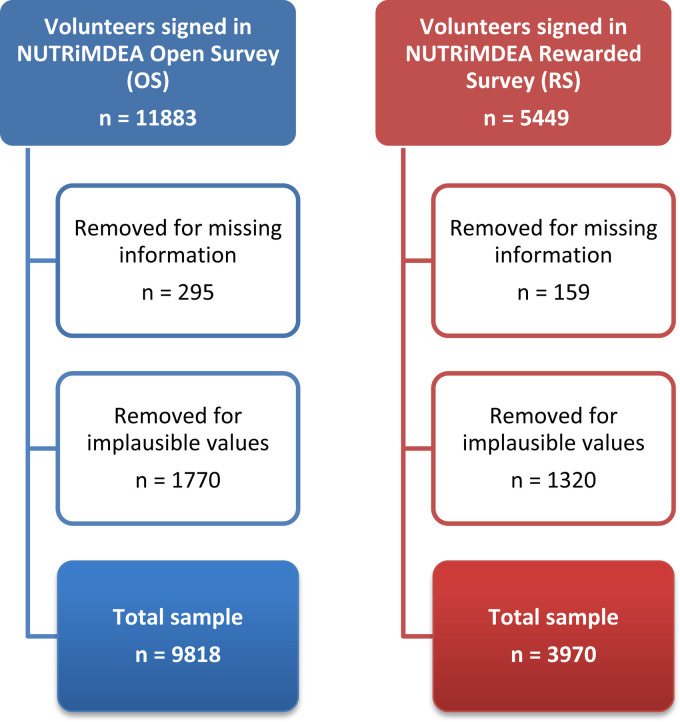
A total of 17,332 participants were screened online from May 2020 to November 2020. Online ads such as internet websites, online newspapers and radio ads were used to enroll volunteers. A total of 11,883 people completed the OS, while the number of participants who encompassed the RS was 5449. The final population of the study after data cleaning was 13,788 volunteers, of which 9818 volunteers responded to the OS and 3970 completed the RW as illustrated in a flowchart (Figure 1).
Figure 1.
Flowchart for the NUTRiMDEA study.
Statistical analyses
Mean values and standard deviations (SD) for continuous variables and percentages for categorical variables were used as descriptive statistics. Data normality was assumed due to the sample size, while distributions were inspected using graphical means, where statistical outliers were removed. Either T-student or analysis of variance (ANOVA) tests was used to compare parametric continuous variables of the participants according to their survey or characteristics of the analyses. Categorical variables were described as proportions, and statistical analyses were performed using chi-square (χ2) test. PCS12 and MCS12 scores were stratified as follows: low or high adherence to Mediterranean diet, low or high level of Physical Activity (using the median of each variable as the cutoff value and divided by type of survey). All the performed statistical tests were two-tailed; p-values <0.05 were considered as statistically significant. Statistical analyses were performed using RStudio version 4.0.1.
For Spanish population, the survey produced a margin of error of 0.9% with a confidence level of 95% (46,940,000 population size and a 10,169 sample).
The propensity score matching was estimated by running a logit model where the outcome variable was a binary variable indicating treatment status (type of survey), to establish the directions of the associations.42 The independent variables that were included were sex, age, ethnicity, education, work and the presence of any disease, since they are the main variables that showed differences between both surveys (Table 1). The rest of the comparison analyzes were adjusted with the estimated propensity score, thus verifying that the differences between both groups were due to data collection and not to their sociodemographic characteristics.
Table 1.
Sociodemographic participant characteristics categorized by type of survey: open survey and rewarded survey.
| Overall | Open surveya | Rewarded surveyb | p c | |
|---|---|---|---|---|
| N | 13,788 | 9818 | 3970 | |
| Age, n (%) | <0.001 | |||
| 18–40 years | 5378 (39.0) | 3420 (34.8) | 1958 (49.3) | |
| 40–70 years | 7873 (57.1) | 6279 (64.0) | 1594 (40.2) | |
| >70 years | 537 (3.9) | 119 (1.2) | 418 (10.5) | |
| Sex, n (%) | <0.001 | |||
| Male | 4700 (34.1) | 2918 (29.7) | 1782 (44.9) | |
| Female | 9043 (65.6) | 6861 (69.9) | 2182 (55.0) | |
| BMId categories, n (%) | <0.001 | |||
| Underweight (BMI < 18.5) | 499 (3.6) | 370 (3.8) | 129 (3.2) | |
| Normalweight (18.5 ≤ BMI < 25) | 8309 (60.3) | 6346 (64.6) | 1963 (49.4) | |
| Overweight (25 ≤ BMI < 30) | 3994 (29.0) | 2571 (26.2) | 1423 (35.8) | |
| Obesity (30 ≤ BMI) | 986 (7.2) | 531 (5.4) | 455 (11.5) | |
| Shirt size, n (%) | <0.001 | |||
| XS/S | 3309 (24.0) | 2613 (26.6) | 696 (17.5) | |
| M | 5177 (37.5) | 3919 (39.9) | 1258 (31.7) | |
| L | 3344 (24.3) | 2257 (23.0) | 1087 (27.4) | |
| XL/XXL | 1958 (14.2) | 1029 (10.5) | 929 (23.4) | |
| Trousers size, mean (SD) | 40.5 (4.0) | 40.1 (3.8) | 41.4 (4.3) | <0.001 |
| Ethnicity, n (%) | <0.001 | |||
| Caucasian/European | 9078 (65.9) | 6720 (68.4) | 2358 (59.7) | |
| Hispanic/Latino/a | 4149 (30.1) | 2793 (28.4) | 1356 (34.4) | |
| Othere | 538 (3.9) | 305 (3.1) | 233 (5.9) | |
| Education, n (%) | <0.001 | |||
| Compulsory education | 1549 (11.2) | 483 (4.9) | 1066 (26.9) | |
| Higher education | 12,051 (87.4) | 9221 (93.9) | 2830 (71.3) | |
| Other | 188 (1.4) | 114 (1.2) | 74 (1.9) | |
| Home situation, n (%) | ||||
| Alone | 2705 (19.6) | 2091 (21.3) | 614 (15.5) | <0.001 |
| Couple | 7904 (57.3) | 5597 (57.0) | 2307 (58.1) | 0.243 |
| Children | 4943 (35.9) | 3561 (36.3) | 1382 (34.8) | 0.110 |
| Older | 633 (4.6) | 369 (3.8) | 264 (6.6) | <0.001 |
| Other | 1193 (8.7) | 680 (6.9) | 513 (12.9) | <0.001 |
| Occupation and work, n (%) | <0.001 | |||
| Employee | 10,238 (74.3) | 8010 (81.6) | 2228 (56.1) | |
| Unemployed/Retired | 2583 (18.7) | 1322 (13.5) | 1261 (31.8) | |
| Student | 967 (7.0) | 486 (5.0) | 481 (12.1) | |
| Smoking status, n (%) | <0.001 | |||
| Current | 2513 (18.2) | 1228 (12.5) | 1285 (32.4) | |
| Former | 2600 (18.9) | 2120 (21.6) | 480 (12.1) |
Open Survey refers to a sample of users who completed the survey online for open.
Rewarded Survey refers to a sample of users of different payment platforms who completed the survey.
Propensity score analysis was made to balance the distribution of the initial observed covariates so that they are similar among subjects in the different groups.
BMI: body mass index (kg/m2), categorized by World Health Organization (WHO) criteria.
Other includes Africans, Asians, mestizos, and other ethnicities. Statistical analyses were performed using chi-square (χ2) test to compare categorical variables.
Results
Sociodemographic participant characteristics were collected and categorized by type of survey (Table 1). In summary, 65.6% of the participants were female, mean age was in the range of 40–70 years, 29% were overweight and 7.2% were obese. Most of them lived in couple were employees and had higher education levels. When comparing populations, there is a higher percentage of middle-aged, female, workers, more educated, Caucasian/European and less smokers’ participants in OS population, than in the RS population (p < 0.05).
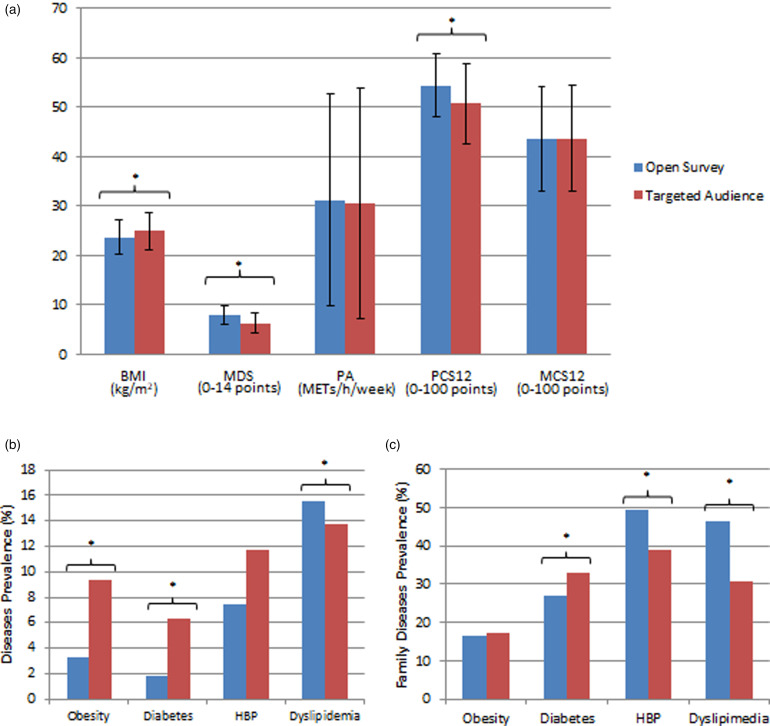
The HRQoL profile was analyzed using the SF-12 questionnaire (Table 2). In general, the OS population reported a better HRQoL compared to RS population, with significant differences in most of the questions (p < 0.05). About 59.2% of participants auto-declared that their heath was good, compared to 25.9% who declared an excellent or very good health, with a higher percentage in the OS than RS (27.0% vs. 21.0% p < 0.05, respectively), while 14.9% declared a fair/poor health, higher percentage from the RS than OS (21.8% vs. 13.3% p < 0.05, respectively). Around 90% declared no limitations in their work or activities due to their physical health, with remarkable differences between OS and RS (92.9% vs. 82.7% p < 0.05, respectively) and about 70% had no limitations relating to their emotional health, with no differences between surveys. The OS had a better PCS12 than RS (54.4 vs. 50.7 p < 0.05), while there were no differences in MCS12 between surveys (Figure 2).
Table 2.
Frequency of response for the short-form 12-item health survey (SF-12) categorized by type of survey: open survey and rewarded survey.a
| Overall | Open survey | Rewarded survey | p b | |
|---|---|---|---|---|
| N | 11,799 | 9595 | 2204 | |
| 1. In general, would you say your health is, n (%) | <0.001 | |||
| Excellent/very good | 3057 (25.9) | 2595 (27.0) | 462 (21.0) | |
| Good | 6987 (59.2) | 5725 (59.7) | 1262 (57.3) | |
| Fair/Poor | 1755 (14.9) | 1275 (13.3) | 480 (21.8) | |
| 2. Does your health now limit you in moderate activities, such as moving a table, or pushing a vacuum cleaner, n (%) | <0.001 | |||
| Yes, limited a lot/little | 1009 (8.6) | 627 (6.5) | 382 (17.3) | |
| No, not limited me at all | 10,790 (91.4) | 8968 (93.5) | 1822 (82.7) | |
| 3. Does your health now limit you in climbing several flights of stairs, n (%) | <0.001 | |||
| Yes, limited a lot/little | 2190 (18.6) | 1570 (16.4) | 620 (28.1) | |
| No, not limited me at all | 9609 (81.4) | 8025 (83.6) | 1584 (71.9) | |
| During the past 4 weeks, have you had any of the following problems as a result of your physical health? | ||||
| 4. Accomplished less than you would like, n (%) | <0.001 | |||
| Yes | 1421 (12.0) | 956 (10.0) | 465 (21.1) | |
| No | 10,378 (88.0) | 8639 (90.0) | 1739 (78.9) | |
| 5. Were limited in the kind of work or other activities, n (%) | <0.001 | |||
| Yes | 1059 (9.0) | 678 (7.1) | 381 (17.3) | |
| No | 10,740 (91.0) | 8917 (92.9) | 1823 (82.7) | |
| During the past 4 weeks, have you had any of the following problems as a result of any emotional problems? | ||||
| 6. Accomplished less than you would like, n (%) | 0.003 | |||
| Yes | 3405 (28.9) | 2803 (29.2) | 602 (27.3) | |
| No | 8394 (71.1) | 6792 (70.8) | 1602 (72.7) | |
| 7. Didn't do work or other activities as carefully as usual, n (%) | 0.037 | |||
| Yes | 3233 (27.4) | 2651 (27.6) | 582 (26.4) | |
| No | 8566 (72.6) | 6944 (72.4) | 1622 (73.6) | |
| 8. During the past 4 weeks, how much did pain interfere with your normal work?, n (%) | <0.001 | |||
| Not at all | 7275 (61.7) | 6268 (65.3) | 1007 (45.7) | |
| A little bit/Moderately | 4051 (34.3) | 3031 (31.6) | 1020 (46.3) | |
| Quite a bit/Extremely | 473 (4.0) | 296 (3.1) | 177 (8.0) | |
| 9. How much of the time during the past 4 weeks, have you felt calm and peaceful?, n (%) | <0.001 | |||
| All of the time/ Most of the time | 4470 (37.9) | 3695 (38.5) | 775 (35.2) | |
| A good bit of the time/ Some of the time | 6731 (57.0) | 5476 (57.1) | 1255 (56.9) | |
| A little of the time/ None of the time | 598 (5.1) | 424 (4.4) | 174 (7.9) | |
| 10. How much of the time during the past 4 weeks, did you have a lot of energy?, n (%) | 0.179 | |||
| All of the time/ Most of the time | 2730 (23.1) | 2219 (23.1) | 511 (23.2) | |
| A good bit of the time/ Some of the time | 7886 (66.8) | 6437 (67.1) | 1449 (65.7) | |
| A little of the time/ None of the time | 1183 (10.0) | 939 (9.8) | 244 (11.1) | |
| 11. How much of the time during the past 4 weeks, have you felt downhearted and blue?, n (%) | <0.001 | |||
| All of the time/ Most of the time | 323 (2.7) | 221 (2.3) | 102 (4.6) | |
| A good bit of the time/ Some of the time | 5994 (50.8) | 4780 (49.8) | 1214 (55.1) | |
| A little of the time/ None of the time | 5482 (46.5) | 4594 (47.9) | 888 (40.3) | |
| 12. How much of the time has your physical health or emotional problems interfered with your social activities?, n (%) | <0.001 | |||
| All of the time/ Most of the time | 373 (3.2) | 247 (2.6) | 126 (5.7) | |
| Some of the time | 2198 (18.6) | 1643 (17.1) | 555 (25.2) | |
| A little of the time/ None of the time | 9228 (78.2) | 7705 (80.3) | 1523 (69.1) | |
Statistical analyses were performed using chi-square (χ2) test to compare categorical variables.
Propensity score analysis was made to balance the distribution of the initial observed covariates so that they are similar among subjects in the different groups.
Figure 2.
Descriptive lifestyle and health characteristics of a population categorized by type of survey. (a) Body Mass Index (BMI), Mediterranean Diet Score (MDS), Physical Activity (PA), Physical and Mental Component Summary of SF-12 Survey (PCS12 and MCS12). (b) Diseases prevalence (%). (c) Family diseases prevalence (%). *p < 0.05, propensity score analysis was made to balance the distribution of the initial observed covariates so that they are similar among subjects in the different groups. Statistical analyses were performed using chi-square (χ2) test to compare categorical variables. T-test was used to compare the mean of parametric continuous variables.
Adherence to Mediterranean diet was evaluated using the MEDAS-14 screener (Table 3). There were statistical differences between types of survey in all questions. On average, the OS population ate more meals per day, had less snacking habits, and added salt to meals less frequently than RS population (p < 0.05). There were no significant differences in water consumption. The OS population declared a higher adherence to Mediterranean diet (Figure 2) than RS population (7.95 points vs. 6.31 points, respectively, p < 0.05).
Table 3.
Adherence to Mediterranean diet (MEDAS-14) and other dietary factors categorized by type of survey: open survey and rewarded survey.a
| Overall | Open survey | Rewarded survey | p b | |
|---|---|---|---|---|
| Adherence to Mediterranean diet PREDIMED questionnaire, n (%): | ||||
| Use of olive oil as main culinary lipid (Yes) | 12,888 (93.6) | 9374 (95.5) | 3514 (89.0) | <0.001 |
| Olive oil (>4 tablespoons/day) | 6028 (43.8) | 4735 (48.2) | 1293 (32.8) | <0.001 |
| Vegetables (≥2 servings/day) | 9014 (65.5) | 6926 (70.5) | 2088 (52.9) | <0.001 |
| Fruits (≥3 servings/day) | 3559 (25.9) | 2872 (29.3) | 687 (17.4) | <0.001 |
| Red/processed meats (<1/day) | 7752 (56.2) | 6259 (63.8) | 1493 (37.6) | <0.001 |
| Butter, cream, margarine (<1/day) | 11,650 (84.5) | 8689 (88.5) | 2961 (74.6) | <0.001 |
| Soda drinks (<1/day) | 11,654 (84.5) | 9068 (92.4) | 2586 (65.1) | <0.001 |
| Wine glasses (≥7/week) | 512 (3.7) | 409 (4.2) | 103 (2.6) | <0.001 |
| Legumes (≥3/week) | 2156 (15.7) | 1570 (16.0) | 586 (14.8) | <0.001 |
| Fish/seafood (≥3/week) | 2687 (19.5) | 2122 (21.6) | 565 (14.3) | <0.001 |
| Commercial sweets and confectionery (<2/week) | 8786 (63.7) | 6749 (68.7) | 2037 (51.3) | <0.001 |
| Tree nuts (≥3/week) | 5839 (42.4) | 4741 (48.3) | 1098 (27.8) | <0.001 |
| Poultry more than red meats (Yes) | 11,180 (81.2) | 7947 (80.9) | 3233 (81.9) | 0.00671 |
| Use of sofrito sauce (≥2/week) | 9509 (69.1) | 6598 (67.2) | 2911 (73.7) | <0.001 |
| Other dietary habits, n (%): | ||||
| Meals per day | <0.001 | |||
| 1–2 meals per day | 1093 (7.9) | 616 (6.3) | 477 (12.0) | |
| 3 meals per day | 6259 (45.4) | 4357 (44.4) | 1902 (47.9) | |
| 4 meals per day | 4213 (30.6) | 3106 (31.7) | 1107 (27.9) | |
| 5 meals per day | 2122 (15.4) | 1672 (17.0) | 450 (11.3) | |
| 6 or more meals per day | 96 (0.7) | 62 (0.6) | 34 (0.9) | |
| Snacking habit | 6689 (48.5) | 4449 (45.3) | 2240 (56.4) | <0.001 |
| Water consumption | 0.277 | |||
| 1–2 glasses per day | 1486 (10.8) | 1068 (10.9) | 418 (10.5) | |
| 3–4 glasses per day | 3729 (27.1) | 2700 (27.5) | 1029 (25.9) | |
| 5–6 glasses per day | 4087 (29.7) | 2917 (29.7) | 1170 (29.5) | |
| 7–8 glasses per day | 2616 (19.0) | 1869 (19.0) | 747 (18.8) | |
| 9–10 glasses per day | 1047 (7.6) | 748 (7.6) | 299 (7.5) | |
| >10 glasses per day | 818 (5.9) | 511 (5.2) | 307 (7.7) | |
| Added salt | <0.001 | |||
| Never | 6051 (43.9) | 4747 (48.4) | 1304 (32.8) | |
| Rarely | 4402 (31.9) | 3097 (31.6) | 1305 (32.9) | |
| Sometimes | 2009 (14.6) | 1228 (12.5) | 781 (19.7) | |
| Often | 824 (6.0) | 479 (4.9) | 345 (8.7) | |
| Habitually | 497 (3.6) | 262 (2.7) | 235 (5.8) | |
Statistical analyses were performed using chi-square (χ2) test to compare categorical variables.
Propensity score analysis was made to balance the distribution of the initial observed covariates so that they are similar among subjects in the different groups.
Also, Physical Activity was recorded with the IPAQ questionnaire (Table 4). Analyses revealed significant differences in light, moderate and intense physical activity, OS population declared higher light and intense activity, while RS population revealed a higher moderate physical activity (p < 0.05). No significant differences were found in total physical activity calculated in METs-h/wk (Figure 2). The OS population was more sedentary, fewer people napped, spent less time napping both on weekdays and on weekends, and sleep more hours at night both on weekdays and on weekends than RS population (p < 0.05).
Table 4.
Physical activity and sleep routine categorized by type of survey: open survey and rewarded survey.a
| Overall | Open survey | Rewarded survey | P b | |
|---|---|---|---|---|
| Physical activity, mean (SD) | ||||
| Intense physical activity (min/week) | 107.0 (120.1) | 109.2 (120.8) | 101.3 (118.5) | <0.001 |
| Moderate physical activity (min/week) | 73.6 (89.6) | 70.6 (86.9) | 81.2 (95.7) | <0.001 |
| Light physical activity (min/week) | 215.8 (164.9) | 217.7 (165.4) | 211.3 (163.4) | 0.042 |
| In a typical week, how much time did you spend sitting during a business day? n (%) | <0.001 | |||
| 1–2 h | 785 (5.7) | 311 (3.2) | 474 (12.0) | |
| 2–4 h | 2707 (19.7) | 1483 (15.1) | 1224 (31.1) | |
| 5–7 h | 4523 (32.9) | 3262 (33.2) | 1261 (32.0) | |
| >8 h | 5743 (41.7) | 4762 (48.5) | 981 (24.9) | |
| Nap, n (%) | 4325 (31.4) | 2712 (27.6) | 1613 (40.6) | <0.001 |
| Nap weekdays, n (%) | <0.001 | |||
| <30 min/day | 2005 (46.4) | 1460 (53.8) | 545 (33.8) | |
| 30–60 min/day | 1938 (44.8) | 1091 (40.2) | 847 (52.5) | |
| >60 min/day | 381 (8.8) | 161 (5.9) | 220 (13.6) | |
| Nap weekends, n (%) | <0.001 | |||
| <30 min/day | 1354 (31.4) | 922 (34.0) | 432 (27.0) | |
| 30–60 min/day | 2129 (49.4) | 1345 (49.6) | 784 (49.0) | |
| >60 min/day | 828 (19.2) | 445 (16.4) | 383 (24.0) | |
| Sleep weekdays, n (%) | <0.001 | |||
| <5 h/day | 351 (2.5) | 143 (1.5) | 208 (5.2) | |
| 5–6 h/day | 4577 (33.2) | 3105 (31.6) | 1472 (37.1) | |
| 7–8 h/day | 8341 (60.5) | 6288 (64.0) | 2053 (51.7) | |
| >9 h/day | 519 (3.8) | 282 (2.9) | 237 (6.0) | |
| Sleep weekends, n (%) | <0.001 | |||
| <5 h/day | 247 (1.8) | 64 (0.7) | 183 (4.6) | |
| 5–6 h/day | 1791 (13.0) | 941 (9.6) | 850 (21.4) | |
| 7–8 h/day | 8409 (61.0) | 6287 (64.0) | 2122 (53.5) | |
| >9 h/day | 3341 (24.2) | 2526 (25.7) | 815 (20.5) | |
Statistical analyses were performed using chi-square (χ2) test to compare categorical variables. One way analysis of variance (ANOVA) test was used to compare parametric continuous variables.
Propensity score analysis was made to balance the distribution of the initial observed covariates so that they are similar among subjects in the different groups.
Mean BMI was 24.1 kg/m2, which was higher in the RS population than OS population (25.0 kg/m2 vs. 23.7 kg/m2 p < 0.05, respectively). Percentage of obesity calculated by BMI is higher than when reported as diagnosed: 7.2% (5.4% and 11.5% OS and RS population, respectively) versus 5.1% diagnosed obesity cases (3.3% and 9.3% in open and OS and RS population, respectively). These data were paralleled by proxies related to shirt and pants sizes (Table 1).
Information about cardiometabolic diseases was also collected within both online questionnaires (Figure 2). Altogether, 31.9% reported the existence of a diagnosed disease: 5.1% obesity, 3.1% diabetes, 8.6% high blood pressure (HBP) and 15.1% dyslipidemia. In regard to diagnosed family diseases, 16.8% reported family obesity, 28.6% family diabetes, 46.5% family HBP and 41.8% family dyslipidemia. In general, OS population reported better health than RS population, except for dyslipidemia. Despite a higher prevalence of HBP in the RS population, for equal sociodemographic conditions, no significant differences were found in HBP between populations through the propensity score analysis. Nevertheless, family health seemed worse in OS population than in the RS population.
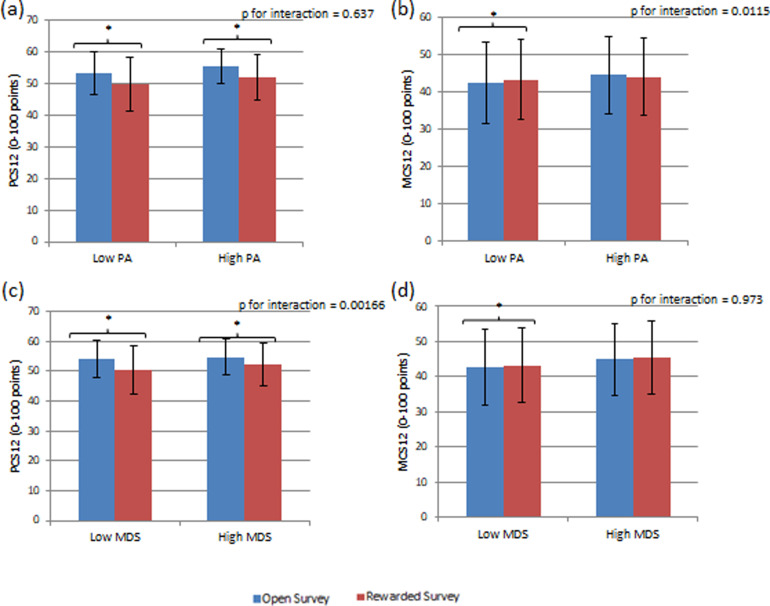
HRQoL items related to Physical Activity and Diet were recorded (Figure 3). Statistical differences (p < 0.05) were observed in the PCS12 between both online populations in both categories of physical activity (low and high), but there were no differences between physical activity categories. Regarding MCS12 there were significant differences between populations when physical activity was low, being lightly higher in the RS population (p < 0.05) but not when it was high; and there were also significant differences between activity categories.
Figure 3.
Physical and mental component summary of SF-12 survey (PCS12 and MCS12) score categorized by level of physical activity (low or high), Mediterranean diet score (low or high) and type of survey (open survey and rewarded survey), (a) PCS12 total score categorized by physical activity and type of survey, (b) MCS12 total score categorized by physical activity and type of survey, (c) PCS12 total score categorized by Mediterranean diet score and type of survey, (d) MCS12 total score categorized by Mediterranean diet score and type of survey. *p < 0.05, propensity score analysis was made to balance the distribution of the initial observed covariates so that they are similar among subjects in the different groups. P-values for two-way analysis of variance (ANOVA) and Sidak post-hoc test between groups.
Regarding HRQoL and diet, there were significant differences in PCS12 between populations (Figure 3), not only when adherence to MedDiet was low but also when adherence was high. Additionally, differences were described between high or low adherence to MedDiet, being higher in the OS population in all cases (p < 0.05). Dissimilarities in MCS12 were only observed between populations when adherence to MedDiet was low (p < 0.05), and it was slightly higher in RS population, as with physical activity and in contrast to the rest of the previous results in PCS12 (both for physical activity and for the Mediterranean diet).
Discussion
In this explanatory analysis, we compared two different methods of web-based survey for carrying out a cross-sectional study of a general population sample. The health, lifestyle and HRQoL characteristics varied depending on the online response platform.
Online enrollment studies have shown a general trend to recruit healthier and more educated participants with usually led by a greater proportion of women among these cohorts.43 However, when using the reward methodology through commercial companies, the selected sample of population more closely resembles the general population, with a higher frequency of diseases.44 Although it is expected that this rewarded sample is less likely to show a behavior modification due to the lack of intrinsic motivations,45,46 but both strategies were suitable for online-based epidemiologic studies and policies implementation.
This study has shown a higher percentage of women, a more educated, purported healthier population, and in general, with better habits and lifestyle than the population of the payment panels.
The study of HRQoL and nutritional well-being of a population is important in order to detect needs and develop tools that allow categorizing individuals according to accompanying health characteristics and thus improving well-being through precision medicine advices and nutrition epidemiological based evidence messages.6
The internet has been proofed to be a suitable platform to recruit participants and spread health information.14 Online surveys have the advantages of being a quick and economic response instrument, with a wide geographical reach, which may increase the feasibility of health-related studies.14,16,47,48 Thus, in a 10-year prospective cohort study, it has been found that the web-based version of data collection does not imply a loss in data quality.49 Furthermore, the web-based questionnaires were completed to a greater extent and with less missing data than paper-based ones.49 One of the largest PN dietary intervention trials to date, Food4Me, used a web-based model to assess the efficacy of different levels of PN compared to standard population-based dietary advice and found that PN improved dietary intake significantly more than conventional non-personalized advice (16).
Moreover, the Canadian Index of Well-being (CIW) designed to track country citizens’ general well-being and life quality from eight subdomains (personal wellness, life expectancy, physical conditions, functional and mental health, lifestyle factors plus behavior and public health care), from existing national databases, generated useful statistics for understanding and nursing the health of Canadians,50 which support the utility of the current survey that collected demography, anthropometrics, nutritional intake, physical activity, perceptions about meals and foods as well as life quality through validated questionnaires for precise public heath purposes. In the study, the same incidence of diabetes as that reported among participants in the rewarded survey of NUTRiMDEA study was found (6–7%). In contrast to obesity, the incidence of which was higher among the Canadian population (18%) than among the NUTRiMDEA population (5.1%). However, the familial obesity reported by NUTRiMDEA participants (17%) was almost identical to the Canadian population. Despite this, a higher percentage of the Canadian population reported an excellent or very good state of health in contrast to the NUTRiMDEA population (60% vs. 26%, respectively).
Noteworthy, a higher proportion of the NUTRiMDEA study participants were females. These results confirm findings from previous web-based nutritional or health studies,14,15,51–54 showing that females are more likely to volunteer for nutrition or health-related research studies and they may be the population group most interested in their health. The mean age coincides with other intervention studies,13,54,55 being the decade of 40 the one with the largest population. The percentage of current smoker in OS population was similar to other studies,56,57 but the RS population showed a much higher percentage. One of the major strengths of our study is that the RS population is more representative of younger and older people, conferring advantages to obtain a more representative population. Although OS participants are a middle age more specific population, subjects interested in their health and many of them used searching about their health through the Internet (apps or websites) platforms.
A higher percentage of workers were described on the OS, which could be explained because middle age participants are predominant in this population, a period of active working life. More volunteers of the RS were students (younger) or retired (older), and they may use these platforms as an opportunity for a small extra pay.58 Mean BMI was similar to other comparable settings.55,56 In addition, results suggest that not all cases of excess weight are diagnosed, since the BMI calculated, according to height and weight reported by the population, indicated a percentage of obesity higher than reported as diagnosed (7.2% vs. 5.1%, respectively), the percentage differences being equal in both cases, both in OS and RW. An integrated questionnaire accounting subjective, psychological and social dimensions showed that morbidities and disease duration are linked to more negative well-being outcomes among older outpatients and single individuals especially those with lower education level in a Chinese population59 as found in the current analyses.
The relationship between well-being and healthy eating has been assessed with both online approaches as established in different settings.57,60,61 The results of these studies suggest that HRQoL is linked with dietary intake. According to our results, adherence to a Mediterranean dietary pattern was associated with better overall perceived quality of life.62 Also, positive association between adherence to Mediterranean diet, physical activity, sleep duration and HRQoL has already been described,61 whereas the female sex, age, BMI, less education and the presence of chronic diseases were associated with lower HRQoL scores.57,61
Nevertheless, no differences in MCS12 when comparing low and high adherence to Mediterranean diet were found. These results contrast to those obtained by Galilea-Zabalza et al., who showed a positive association between higher adherence to Mediterranean diet, emotional role and mental health.63 These disparities in results could be due to the use of different tools, Galilea-Zabalza et al. who used the 17-item questionnaire to evaluate the adherence to Mediterranean diet and SF-36 to assess HRQoL as well as different methods of data collection.
When adherence to Mediterranean diet and weight is compared, our results agree with prior published evidence,64 which described that a Mediterranean diet pattern, limiting the intake of known deleterious foods is linked to a lower risk of overweight or obesity. OS population showed a generalized higher adherence to Mediterranean diet, there were significant differences in all questions of MEDAS-14 between populations. Also, the data concerning red and processed meats consumption showed differences between samples where economic and cultural aspects may have a role.65
Another cross-sectional analysis to assess the influence of dietary, lifestyle, and demographic factors on HRQoL based on a subsample of the Seguimiento Universidad de Navarra (SUN) Mediterranean online cohort (n = 15,674) found relationships of HRQoL with dietary Mediterranean and provegetarian food pattern, lifestyles (sleeping hours, physical activity) thought multivariate linear and flexible regression models were used to estimate the pondered effect of personal factors on SF-36.61 Thus, BMI, females and preexisting diabetes, hypertension and hypercholesterolemia explained lower SF-36 scores, which are in agreement with our findings and validate both online approaches as estimators of dietary habits and physical activity patterns and associated relationships with life quality.
Apparently, the physical activity reported by both groups was quite high, compared to available indications,61 which could be explained by the different data collection methods. In any case, IPAQ may tend to overestimate physical activity66; however, these results agree with other studies.57 Although significant differences were found in all activity categories (OS indicated greater light and intense physical activity and RS showed greater moderate physical activity), no significant differences were found in total METs-h/wk. There were no differences between HRQoL and physical activity when PCS12 (low or high) was analyzed but there were differences when the MCS12 (low and high) was analyzed. These results are opposite to other studies that found that practice of physical activity was related to better health perception.57,61 In any case, work capacity, healthy lifestyles involving regular physical activity and overall well-being, in addition to reducing morbidity and mortality, also promote mental and social health and improve the quality of life,67 which is in agreement with reported findings.
Regarding the sleep pattern, the OS population declared more hours of sleep at night. This result may be one of the factors that explain a lower prevalence of obesity in this population as it has been reported in medical literature.68 Furthermore, an online self-administered survey exhibited that sleep patterns are associated with quality of life which appears to reflect general health, with important policy implications concerning the implementation of dietary and physical activity for disease management.69 OS population also declared a lower nap habit. This last result could contrast with another study that showed a positive association between napping and a lower risk of obesity.68 Concerning nap duration, those OS population who declared nap habit, dedicated a shorter period of time napping (<30 min/d) than RS population, who declared a higher mean of napping duration. These results coincide with the previous study, which describes that those who sleep a more adequate duration (30 min/d) had a 33% lower risk of becoming obese compared to those who did not take a nap or take it for more than 30 min/d.68
Another unexpected outcome was that despite the fact that the OS population seemed to have healthier habits and lifestyle; they showed a higher prevalence of dyslipidemia with significant differences compared to RS population. This finding may be related to a marked family connotation, since they also showed a higher prevalence of familiar dyslipidemia and also it could be taken into account that this population is quite more sedentary than RS population, which appears to be a determining factor.70,71 A higher prevalence of familiar HBP in the OS population was found. However, this result seemed not to translate to a higher prevalence in OS population, which may be offset by a better lifestyle compared to the RS population.72 A higher percentage of HBP was declared by the RS population. However, the propensity score showed that, with equal sociodemographic characteristics, the type of survey did not show significant differences in this disease between both populations when the selected confounders were included. Self-reported hypertension has been previously validated as a reliable tool to determine the hypertensive status among highly educated participants.73 Actually, a literature review has shown the scarcity of specific questionnaires to assess well-being within the community, but that measuring healthy lifestyle and mental health can estimate quality of life and well-being as well as chronic disease burdens.74
Limitations and strengths
One of the principal disadvantages of this cross-sectional study is that it cannot study cause-and-effect relationship between variables. On the other hand, the use of an online method for data collection can be criticized for not being representative of the whole population, because it excludes computer illiterate and those without access to internet.75 Nevertheless, the RS population may counteract this effect as it is more illustrative of younger and older people, conferring advantages to obtain a more representative population. Indeed, research has shown that rewarded platforms tend to be more diverse and thus recruit a wider range of the general population than other web-based and in-person recruitment methods.76
In our study, all data collected were self-reported, therefore, as with all studies utilizing online recruitment methods, there is the possibility that not all responses are completely accurate16 or the existence of measurement errors, although there is already available literature that validates this type of methods.28
The differences between OS and RS reveal that the collection method is useful but the results should be interpreted with care given that two different populations appear to respond to each online approach. Intrinsic differences in the platforms could have led to variation. But at the same time, this cross-platform variability seems to somehow alleviate the threats to external validity that come with gathering information solely through one platform. The influence of the COVID-19 pandemic cannot be ruled out, so there may be biases in the data. In the same way, when dealing with different populations (economically and educational less favored people…) it may also have influenced the biases.
The data validation is another question to examine with care since could be considered as a drawback of current data, but results from studies such as Nurses’, Health Professionals follow-up, and SUN or Food4me28,29,77 warrant the rationality of NUTRiMDEA analyses concerning representativeness, legitimacy and opportunity of the surveys despite the differences attributable to the collection mode. Furthermore, qualitative and quantitative investigations on component procedures, helpfulness, cost-effectiveness, fairness and suitability of different versions of health-related lifestyle guides in improving health have evidenced valuable benefits of online procedures despite the inherent questions about tool strength.78,79
Comparison with prior work
One of the biggest difficulties concerning these analyses was finding comparable studies. Most web-based studies available are based on dietary and physical activity interventions for weight loss primarily,80–82 Literature shows articles comparing web-based with non-web-based,13,47,49 physical,15 telephone, mailing83 or postal14 data collection. Other study compared the characteristics of a sample of pregnant smokers, recruited through four different online platforms (three crowdsourcing platforms and one social media site) and describes the differences and feasibility of each platform as well as the costs per completed survey.16 This article, to our knowledge, is newfangled to date by comparing two online modes of health-related data collection, one free, and other rewarded.
Conclusions
This study found dissimilarities in sociodemographic, health, diet, physical activity and HRQoL profile of a sample of people depending on whether they completed the online questionnaire in one or the other type of platform (open and free or rewarded access), despite being the same survey in both cases. OS participants seemed to be a healthier population with better health habits and HRQoL in general than RS sample. These observed differences are likely due to both different recruitment methods, possibly due to groups with different socioeconomic status and health interest, so it should be taken into account when interpreting results in future studies. This article contributes to the methodological literature on the impact of mode of data collection on measuring e-Health.
Acknowledgments
Thanks very much to our participants as well as NUTRiMDEA Research Group members for their invaluable support.
Footnotes
Contributorship: Conceptualization: R.S-C. and JA.M; Methodology: R.S-C, R.M. and JA.M.; Investigation: A.H., R.R., R.S-C, R.M. V.M., I.E., A.R.M. and JA.M.; Data Analysis: A.H., R.R., R.S-C, R.M.; Writing—Original Draft: A.H., R.S.C.; Visualization, A.H., R.R., R.S-C, R.M. V.M., I.E., A.R.M. and JA.M. All authors have read and agreed to the published version of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The NUTRiMDEA survey included a disclaimer informing the participants about this information and acquiescent that submitting the questionnaire constitutes acceptance of the use of their anonymity data for scientific purposes. This statement was positively accepted by the IMDEA CEI and the companies in charge of the rewarded surveys.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Centro de Investigación Biomédica en Red-Fisiopatología de la Obesidad y Nutrición, Consejería de Educación, Juventud y Deporte, Comunidad de Madrid, Ministerio de Ciencia e Innovación y Ministerio de Universidades (grant number P2013/ABI-2728, ALIBIRD-CM, FJC2018-038168-I).
Guarantor: JAM.
ORCID iD: Victor Mico https://orcid.org/0000-0003-0681-7962
References
- 1.Graham H, White PC. Social determinants and lifestyles: integrating environmental and public health perspectives. Public Health 2016; 141: 270–278. [DOI] [PubMed] [Google Scholar]
- 2.Estoque RC, Togawa T, Ooba M, et al. A review of quality of life (QOL) assessments and indicators: towards a “QOL-climate” assessment framework. Ambio 2019; 48: 619–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Budreviciute A, Damiati S, Sabir DK, et al. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health 2020; 8: 574111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics 2016; 34: 645–649. [DOI] [PubMed] [Google Scholar]
- 5.The world health organization quality of life assessment (WHOQOL): position paper from the world health organization. Soc Sci Med 1995; 41: 1403–1409. [DOI] [PubMed] [Google Scholar]
- 6.de Cuevillas B, Álvarez Álvarez I, Cuervo M, et al. Definition of nutritionally qualitative categorizing (proto)nutritypes and a pilot quantitative nutrimeter for mirroring nutritional well-being based on a quality of life health related questionnaire. Nutr Hosp 2019; 36: 862–874. [DOI] [PubMed] [Google Scholar]
- 7.Puchau B, Zulet MA, de Echávarri AG, et al. Dietary total antioxidant capacity: a novel indicator of diet quality in healthy young adults. J Am Coll Nutr 2009; 28: 648–656. [DOI] [PubMed] [Google Scholar]
- 8.Rodríguez-Muñoz S, Corella C, Abarca-Sos A, et al. Validation of three short physical activity questionnaires with accelerometers among university students in Spain. J Sports Med Phys Fitness 2017; 57: 1660–1668. [DOI] [PubMed] [Google Scholar]
- 9.Organization WH. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. WHO Global NCD Action Plan 2013-20202013.
- 10.Tennant B, Stellefson M, Dodd V, et al. Ehealth literacy and web 2.0 health information seeking behaviors among baby boomers and older adults. J Med Internet Res 2015; 17: e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Müller AM, Maher CA, Vandelanotte C, et al. Physical activity, sedentary behavior, and diet-related eHealth and mHealth research: bibliometric analysis. J Med Internet Res 2018; 20: e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eurostat. Digital economy and society statistics – households and individuals. 2021.
- 13.Wantland DJ, Portillo CJ, Holzemer WL, et al. The effectiveness of web-based vs. Non-web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res 2004; 6: e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rowen D, Carlton J, Elliott J. PROM Validation using paper-based or online surveys: data collection methods affect the sociodemographic and health profile of the sample. Value Health 2019; 22: 845–850. [DOI] [PubMed] [Google Scholar]
- 15.Al-Awadhi B, Fallaize R, Zenun Franco R, et al. Insights into the delivery of personalized nutrition: evidence from face-to-face and web-based dietary interventions. Front Nutr 2020; 7: 570531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibarra JL, Agas JM, Lee M, et al. Comparison of online survey recruitment platforms for hard-to-reach pregnant smoking populations: feasibility study. JMIR Res Protoc 2018; 7: e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Warner MM, Kelly JT, Reidlinger DP, et al. Reporting of telehealth-delivered dietary intervention trials in chronic disease: systematic review. J Med Internet Res 2017; 19: e410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Teasdale N, Elhussein A, Butcher F, et al. Systematic review and meta-analysis of remotely delivered interventions using self-monitoring or tailored feedback to change dietary behavior. Am J Clin Nutr 2018; 107: 247–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berezowska A, Fischer AR, Ronteltap A, et al. Understanding consumer evaluations of personalised nutrition services in terms of the privacy calculus: a qualitative study. Public Health Genomics 2014; 17: 127–140. [DOI] [PubMed] [Google Scholar]
- 20.San-Cristobal R, Milagro FI, Martínez JA. Future challenges and present ethical considerations in the use of personalized nutrition based on genetic advice. J Acad Nutr Diet 2013; 113: 1447–1454. [DOI] [PubMed] [Google Scholar]
- 21.Hammersley ML, Jones RA, Okely AD. Parent-focused childhood and adolescent overweight and obesity eHealth interventions: a systematic review and meta-analysis. J Med Internet Res 2016; 18: e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aardoom JJ, Loheide-Niesmann L, Ossebaard HC, et al. Effectiveness of eHealth interventions in improving treatment adherence for adults with obstructive sleep apnea: meta-analytic review. J Med Internet Res 2020; 22: e16972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGarrigle L, Todd C. Promotion of physical activity in older people using mHealth and eHealth technologies: rapid review of reviews. J Med Internet Res 2020; 22: e22201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howarth A, Quesada J, Silva J, et al. The impact of digital health interventions on health-related outcomes in the workplace: a systematic review. Digit Health 2018; 4: 2055207618770861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang S, Hong YA. Clinical trial participation in America: the roles of eHealth engagement and patient-provider communication. Digit Health 2021; 7: 20552076211067658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Granja C, Janssen W, Johansen MA. Factors determining the success and failure of eHealth interventions: systematic review of the literature. J Med Internet Res 2018; 20: e10235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmidt S, Vilagut G, Garin O, et al. [Reference guidelines for the 12-item short-form health survey version 2 based on the Catalan general population]. Med Clin (Barc) 2012; 139: 613–625. [DOI] [PubMed] [Google Scholar]
- 28.Celis-Morales C, Foster H, O’Donovan C, et al. Validation of web-based self-reported socio-demographic and anthropometric data collected in the Food4Me study. Proc Nutr Soc 2014; 73: E78. [Google Scholar]
- 29.Martínez-González MA, Sanchez-Villegas A, De Irala J, et al. Mediterranean diet and stroke: objectives and design of the SUN project. Seguimiento Universidad de Navarra. Nutr Neurosci 2002; 5: 65–73. [DOI] [PubMed] [Google Scholar]
- 30.Schröder H, Fitó M, Estruch R, et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 2011; 141: 1140–1145. [DOI] [PubMed] [Google Scholar]
- 31.Martínez-González MA, García-Arellano A, Toledo E, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One 2012; 7: e43134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martínez-González M, Corella D, Salas-Salvadó J, et al. Cohort profile: design and methods of the PREDIMED study. Int J Epidemiol 2012; 41: 377–385. [DOI] [PubMed] [Google Scholar]
- 33.de la Fuente-Arrillaga C, Ruiz ZV, Bes-Rastrollo M, et al. Reproducibility of an FFQ validated in Spain. Public Health Nutr 2010; 13: 1364–1372. [DOI] [PubMed] [Google Scholar]
- 34.Mantilla Toloza S, Gómez-Conesa A. International physical activity questionnaire. An adequate instrument in population physical activity monitoring. Rev Iberoam Fisioter Kinesiol 2007; 10: 48–52. [Google Scholar]
- 35.Vilagut G, Valderas JM, Ferrer M, et al. [Interpretation of SF-36 and SF-12 questionnaires in Spain: physical and mental components]. Med Clin (Barc) 2008; 130: 726–735. [DOI] [PubMed] [Google Scholar]
- 36.Vera-Villarroel P, Silva J, Celis-Atenas K, et al. [Evaluation of the SF-12: usefulness of the mental health scale]. Rev Med Chil 2014; 142: 1275–1283. [DOI] [PubMed] [Google Scholar]
- 37.Kontodimopoulos N, Pappa E, Niakas D, et al. Validity of SF-12 summary scores in a Greek general population. Health Qual Life Outcomes 2007; 5: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marinho MCP, Magalhaes TF, Fernandes LFC, et al. Quality of life in women with endometriosis: an integrative review. J Womens Health (Larchmt) 2018; 27: 399–408. [DOI] [PubMed] [Google Scholar]
- 39.Younsi M, Chakroun M. Measuring health-related quality of life: psychometric evaluation of the Tunisian version of the SF-12 health survey. Qual Life Res 2014; 23: 2047–2054. [DOI] [PubMed] [Google Scholar]
- 40.WHO. Body Mass Index (BMI). Available from: https://www.who.int/data/gho/data/themes/theme-details/GHO/body-mass-index-(bmi)2021.
- 41.NutrIMDEA study website, https://nutrimdea2020.questionpro.com/.
- 42.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 2015; 34: 3661–3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Battineni G, Baldoni S, Chintalapudi N, et al. Factors affecting the quality and reliability of online health information. Digit Health 2020; 6: 2055207620948996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ribot-Rodriguez R, Higuera-Gomez A, San-Cristobal R, et al. Cardiometabolic health status, ethnicity and health-related quality of life (HRQoL) disparities in an adult population: NutrIMDEA observational web-based study. Int J Environ Res Public Health 2022; 19: 2948. DOI: 10.3390/ijerph19052948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kahlert D, Unyi-Reicherz A, Stratton G, et al. PREVIEW behavior modification intervention toolbox (PREMIT): A study protocol for a psychological element of a multicenter project. Front Psychol 2016; 7: 1136. Protocols. DOI: 10.3389/fpsyg.2016.01136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psychol 2008; 49: 182–185. [Google Scholar]
- 47.Taber N, Mehmood A, Vedagiri P, et al. Paper versus digital data collection methods for road safety observations: comparative efficiency analysis of cost, timeliness, reliability, and results. J Med Internet Res 2020; 22: e17129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Gelder MMHJ, Merkus PJFM, van Drongelen J, et al. The PRIDE study: evaluation of online methods of data collection. Paediatr Perinat Epidemiol 2020; 34: 484–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zazpe I, Santiago S, De la Fuente-Arrillaga C, et al. Paper-based versus web-based versions of self-administered questionnaires, including food-frequency questionnaires: prospective cohort study. JMIR Public Health Surveill 2019; 5: e11997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muhajarine N, Labonte R, Winquist BD. The Canadian index of wellbeing: key findings from the healthy populations domain. Can J Public Health 2012; 103: e342–e347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Celis-Morales C, Livingstone KM, Marsaux CF, et al. Design and baseline characteristics of the Food4Me study: a web-based randomised controlled trial of personalised nutrition in seven European countries. Genes Nutr 2015; 10: 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Livingstone KM, Celis-Morales C, Macready AL, et al. Characteristics of European adults who dropped out from the Food4Me internet-based personalised nutrition intervention. Public Health Nutr 2017; 20: 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Timon CM, Walton J, Flynn A, et al. Respondent characteristics and dietary intake data collected using web-based and traditional nutrition surveillance approaches: comparison and usability study. JMIR Public Health Surveill 2021; 7: e22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Oenema A, Brug J, Lechner L. Web-based tailored nutrition education: results of a randomized controlled trial. Health Educ Res 2001; 16: 647–660. [DOI] [PubMed] [Google Scholar]
- 55.Marshall AL, Leslie ER, Bauman AE, et al. Print versus website physical activity programs: a randomized trial. Am J Prev Med 2003; 25: 88–94. [DOI] [PubMed] [Google Scholar]
- 56.Celis-Morales C, Livingstone KM, Marsaux CFM, et al. Effect of personalized nutrition on healthrelated behaviour change: evidence from the Food4me European randomized controlled trial. Int J Epidemiol 2017; 46: 578–588. [DOI] [PubMed] [Google Scholar]
- 57.Sayón-Orea C, Santiago S, Bes-Rastrollo M, et al. Determinants of self-rated health perception in a sample of a physically active population: PLENUFAR VI study. Int J Environ Res Public Health 2018; 15: 2104. DOI: 10.3390/ijerph15102104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Baker R, Blumberg SJ, Brick MJ, et al. Research synthesis. AAPOR report on online panel. Public Opin Q 2010; 74: 711–781. [Google Scholar]
- 59.Huang F, Li H. Factors influencing integrated wellbeing in older Chinese outpatients with chronic diseases. Aust J Prim Health 2018; 24: 189–195. [DOI] [PubMed] [Google Scholar]
- 60.San-Cristobal R, Navas-Carretero S, Celis-Morales C, et al. Capturing health and eating status through a nutritional perception screening questionnaire (NPSQ9) in a randomised internet-based personalised nutrition intervention: the Food4Me study. Int J Behav Nutr Phys Act 2017; 14: 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pano O, Sayón-Orea C, Gea A, et al. Nutritional determinants of quality of life in a Mediterranean cohort: The SUN study. Int J Environ Res Public Health 2020; 17: 3897. DOI: 10.3390/ijerph17113897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Godos J, Castellano S, Marranzano M. Adherence to a Mediterranean dietary pattern is associated with higher quality of life in a cohort of Italian adults. Nutrients 2019; 11: 981. DOI: 10.3390/nu11050981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Galilea-Zabalza I, Buil-Cosiales P, Salas-Salvadó J, et al. Mediterranean diet and quality of life: baseline cross-sectional analysis of the PREDIMED-PLUS trial. PLoS One 2018; 13: e0198974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.San-Cristobal R, Navas-Carretero S, Celis-Morales C, et al. Analysis of dietary pattern impact on weight status for personalised nutrition through on-line advice: the Food4Me Spanish cohort. Nutrients 2015; 7: 9523–9537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim OY, Kwak SY, Kim B, et al. Selected food consumption mediates the association between education level and metabolic syndrome in Korean adults. Ann Nutr Metab 2017; 70: 122–131. [DOI] [PubMed] [Google Scholar]
- 66.Lee PH, Macfarlane DJ, Lam TH, et al. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act 2011; 8: 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Karvonen MJ. Physical activity for a healthy life. Res Q Exerc Sport 1996; 67: 213–215. [DOI] [PubMed] [Google Scholar]
- 68.Sayón-Orea C, Bes-Rastrollo M, Carlos S, et al. Association between sleeping hours and siesta and the risk of obesity: the SUN Mediterranean cohort. Obes Facts 2013; 6: 337–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Canaway R, Manderson L. Quality of life, perceptions of health and illness, and complementary therapy use among people with type 2 diabetes and cardiovascular disease. J Altern Complement Med 2013; 19: 882–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016; 388: 1302–1310. [DOI] [PubMed] [Google Scholar]
- 71.Wang Y, Xu D. Effects of aerobic exercise on lipids and lipoproteins. Lipids Health Dis 2017; 16: 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rust P, Ekmekcioglu C. Impact of salt intake on the pathogenesis and treatment of hypertension. Adv Exp Med Biol 2017; 956: 61–84. [DOI] [PubMed] [Google Scholar]
- 73.Alonso A, Beunza JJ, Delgado-Rodríguez M, et al. Validation of self reported diagnosis of hypertension in a cohort of university graduates in Spain. BMC Public Health 2005; 5: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ahmed N, Ahmed S, Carmichael Z, et al. Measuring healthy lifestyle and mental health indicators in south Asian women using the “your health: quality of life and well-being” questionnaire. Ann Glob Health 2017; 83: 463–470. [DOI] [PubMed] [Google Scholar]
- 75.Heponiemi T, Kaihlanen AM, Kouvonen A, et al. The role of age and digital competence on the use of online health and social care services: a cross-sectional population-based survey. Digit Health 2022; 8: 20552076221074485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Berinsky A, Huber G, Lenz G. Evaluating online labor markets for experimental research: Amazon.com’s MechanicalTurk. Polit Anal 2012; 20: 351–368. [Google Scholar]
- 77.Yuan C, Spiegelman D, Rimm EB, et al. Validity of a dietary questionnaire assessed by comparison with multiple weighed dietary records or 24-h recalls. Am J Epidemiol 2017; 185: 570–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Carr SM, Lhussier M, Forster N, et al. An evidence synthesis of qualitative and quantitative research on component intervention techniques, effectiveness, cost-effectiveness, equity and acceptability of different versions of health-related lifestyle advisor role in improving health. Health Technol Assess 2011; 15: iii–iv, 1-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jandoo T. WHO Guidance for digital health: what it means for researchers. Digit Health 2020; 6: 2055207619898984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lynch SM, Stricker CT, Brown JC, et al. Evaluation of a web-based weight loss intervention in overweight cancer survivors aged 50 years and younger. Obes Sci Pract 2017; 3: 83–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Héroux M, Watt M, McGuire KA, et al. A personalized, multi-platform nutrition, exercise, and lifestyle coaching program: a pilot in women. Internet Interv 2017; 7: 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Saslow LR, Mason AE, Kim S, et al. An online intervention comparing a very low-carbohydrate ketogenic diet and lifestyle recommendations versus a plate method diet in overweight individuals with type 2 diabetes: a randomized controlled trial. J Med Internet Res 2017; 19: e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lallukka T, Pietiläinen O, Jäppinen S, et al. Factors associated with health survey response among young employees: a register-based study using online, mailed and telephone interview data collection methods. BMC Public Health 2020; 20: 184. [DOI] [PMC free article] [PubMed] [Google Scholar]