Abstract
Background:
Reverse total shoulder replacement (RTSR) is becoming a popular and reliable treatment for rotator cuff arthropathy. However, little is known about the ability to participate in sports after surgery.
Purpose:
To determine to what extent RTSR will allow patients to participate in sporting activities and identify the associated factors that could affect postoperative sports participation.
Study Design:
Case series; Level of evidence, 4.
Methods:
Data were collected prospectively from patients who underwent RTSR over a 10-year period from April 2009 to May 2019. Patients were assessed before surgery, at 6 months after surgery, and at the final follow-up. Patients were asked within a validated shoulder questionnaire to rank their current highest level of sports participation, overall shoulder status, frequency of pain, level of pain, and functional levels. Their shoulder range of motion and strength were assessed before surgery and at 6 months after surgery.
Results:
The study included 108 shoulders (106 patients). The mean age was 74 years (range, 51-88 years), with 44 men and 64 women. The mean follow-up was 4 years. Overall shoulder satisfaction, frequency and levels of pain, and shoulder function improved significantly at 6 months and 4 years (P < .0001). External rotation, abduction, and forward flexion range of motion improved significantly at 6 months (P < .05 for all). The strength of internal rotation, external rotation, abduction, and adduction improved significantly at 6 months (P < .001 for all). The rate of return to sports was 67% at 6 months and 48% at 4 years. Multiple significantly associated factors were identified with return to sports at 6 months, including sex and age.
Conclusion:
The rate of return to sports after RTSR is high. Around two-thirds of patients can return to sports at 6 months postoperatively, although the results slightly deteriorate over time (48% at 4 years).
Keywords: shoulder, reverse replacement, arthroplasty, sport
In 1987, Grammont et al 9 introduced the concept and design of a reverse total shoulder replacement (RTSR) to treat rotator cuff tear arthropathy. After it was initiated in Europe in the 1990s, RTSR was approved by the US Food and Drug Administration in 2004. The number of RTSRs performed annually has increased dramatically around the world. In Australia, RTSR became available in the early 2000s and has continued to increase in popularity. According to the Australian National Joint Registry 2020 annual report, 1 the number of RTSRs performed in 2019 continued to increase to reach 30,330 reported to the registry. Primary RTSR increased from 43% of all total shoulder replacements in 2008 to 80% in 2019.
The RTSR was proven to be a reliable treatment option for rotator cuff arthropathy. 2,3,5 It provides significant improvement in shoulder function, pain relief, and subsequently quality of life. 6,8,16
The indications for the RTSR have been expanded recently. Although the primary indication for RTSR was cuff arthropathy, other difficult shoulder problems have been managed with RTSR and showed favorable outcomes. 10,12,18 These indications include glenohumeral arthritis, acute proximal humerus fracture, revision of failed standard total shoulder replacement and hemiarthroplasty, and others. The 2020 annual report of the Australian National Joint Replacement Registry showed that the most common diagnosis for which RTSR was performed is osteoarthritis (44%), followed by rotator cuff arthropathy (35%) and fracture (15%). 1
Sporting activities in the long term have been linked to good mental and physical health and as well as social well-being. We have observed a number of patients asking about their expected return to sports or the ability to participate in sports in general after RTSR. An understanding of how effectively this surgical procedure facilitates return to sports may assist patients and surgeons in more accurately managing expectations and planning for the future. While RTSR has been shown to improve functional outcomes and achieve significant pain relief, 4,14,15 return to sports has not been well studied. We hypothesize that RTSR will enable patients to return to sports. The few studies that have studied this particular outcome 7,11,17 have shown variable results. The percentage of patients returning to sports after RTSR ranged from 60% to 85%. Simovitch et al 17 reported 60% return to sports in a series of 67 patients. Kolling et al 11 showed 77% return to sporting activities after RTSR in a screening of the Swiss shoulder arthroplasty registry. In a case series of 76 patients, Garcia et al 7 showed an 85% return to sports.
All of these studies are retrospective in nature. Furthermore, these previous studies have not reported correlations with other outcomes or asserted any predictive factors to return to sports. Hence, the aim of this study was to determine what proportion of our patients could return to sports after RTSR and what factors were associated with return to sports.
Methods
Study Design
This study was a retrospective analysis of prospectively collected data of patients who had RTSRs over a 10-year period, from April 2009 to May 2019. Ethical approval for the study protocol was obtained, and all included patients provided informed consent. All surgical procedures were performed by a single surgeon using 2 implant systems. The inclusion criteria were that patients had to have a primary RTSR and a minimum 1-year follow-up. Patients were excluded if they had revision surgery (revised from hemiarthroplasty or standard shoulder arthroplasty), were unwilling to participate in the study, had passed away, or could not be reached for the final follow-up.
The primary outcome of the study was to assess patients’ ability to participate in sports after reverse total shoulder arthroplasty (RTSA). The secondary outcomes included the overall shoulder condition, functional outcomes, and the type and level of sporting activities. The data were retrieved from the medical record system and the preoperative and initial follow-up information. Further follow-up through telephone interviews was done at the time of conducting the study.
Surgical Technique
All RTSAs were performed using a deltopectoral approach. The subscapularis tendon was detached from the lesser tuberosity and later reattached with Mersilene tape (Ethicon). Inferior osteophytes of the humeral head were removed to expose the anatomic neck, followed by an anatomic neck cut to achieve 30° of retroversion. Glenoid preparation consisted of extensive ligament and capsular release and labral excision to achieve optical glenoid exposure. The glenoid surface was reamed eccentrically to remove more bone inferiorly to create a 10° inferior tilt of the baseplate. All RTSAs were performed using either the Grammont-style Aequalis Reversed Shoulder System (Tornier) or lateralized Encore Reverse Shoulder Prosthesis (DJO Surgical).
Postoperatively, all patients had their arms immobilized in a sling for 2 days. Patients were instructed to follow a home-based rehabilitation program composed of 3 phases: phase 1 focused on passive range of motion (ROM), pendulum exercises, and isometric strengthening; phase 2 incorporated active external rotation and flexion stretches; and phase 3 was supplemented with active-resistant band exercises and incremental light weightlifting. Patients were advised not to engage in overhead work for >15 minutes. At 6-month follow-up, most patients were encouraged to return to full duties.
Outcome Measures
Patients received a modified L’Insalata questionnaire 13 before surgery, 6 months after surgery, and at the final follow-up. Patients were asked within the 14-question L’Insalata questionnaire to rank their current highest level of sports participation, overall shoulder status, frequency of pain, level of pain, and functional level using a Likert scale. Responses were converted to ordinal numerical values for statistical analysis. For example, for our primary outcome question (“What is your highest level of sport now?”), there were 4 possible responses on a Likert scale (none, hobby, club, and national), which were assigned the numbers 0, 1, 2, and 3, respectively. Secondary outcomes for this study were patient-reported overall shoulder status (graded from very bad to good), frequency of pain (daily to none), level of pain (very severe to none), and difficulty with activities (very severe to none).
Secondary outcomes included passive shoulder ROM and muscle strength. Visual estimation was utilized as a measure for ROM. Abduction, forward flexion, and external and internal rotation ROM were assessed and recorded preoperatively and at 6 months postoperatively. Similarly, supraspinatus, internal rotation, external rotation, adduction, and liftoff strength were recorded preoperatively and at 6 months postoperatively. A handheld dynamometer (Mecmesin) was utilized to measure muscle strength.
Statistical Analysis
For nonparametric data such as pain scores and internal rotation (vertebrate levels), the Mann-Whitney rank-sum test was used to assess differences between groups. The Kruskal-Wallis test was used to assess nonparametric data at different time points within a group, with significant level set at 0.05. For parametric data such as shoulder strength and ROM, an unpaired Student t test was used to compare results between groups at different time points. Chi-square analysis was used to evaluate dichotomous data, such as patient demographics and percentage change in sports participation. The threshold for significance was set at P < .05
The Spearman rho (r) correlation coefficient was used to assess the relationship of sports participation with demographic data, patient-reported pain, function, and examiner-assessed shoulder ROM and strength. Statistical analysis was performed using Prism Version 9.2.0 (GraphPad Software) and SPSS Version 26 (IBM).
Results
During the study period, 169 RTSAs were performed. Of the 169 shoulders, 61 were excluded, leaving 108 shoulders (106 patients) for the study (Figure 1). The mean age was 74 years (range, 51-88 years). Forty-four patients were men, and 64 were women; 59 were right side, and 49 were left. The mean final follow-up was 4 years postoperatively (Table 1).
Figure 1.
CONSORT flowchart of included and excluded patients in this study. RTSA, reverse total shoulder arthroplasty.
Table 1.
Characteristics of the Study Patients (n = 106 Patients, 108 Shoulders) a
| Preoperative Sports Participation | |||
|---|---|---|---|
| Yes | No | P Value | |
| Sex | .08 | ||
| Male | 13 (62) | 30 (38) | |
| Female | 8 (38) | 48 (62) | |
| Age, y | 72.1 (54-84) | 74.2 (51-88) | .27 |
| Side | .99 | ||
| Right | 11 (52) | 43 (55) | |
| Left | 10 (48) | 35 (45) | |
| Prosthesis | .99 | ||
| DJO | 16 (76) | 57 (73) | |
| Tornier | 5 (24) | 21 (27) | |
| Follow-up duration, y | 4.4 (1-9) | 3.9 (1-10) | .42 |
a Data are reported as No. (%) or mean (range).
Patient overall satisfaction improved significantly at 6 months post- vs preoperatively and was maintained at the final follow-up (Figure 2A). Pain and functional outcomes also improved after RTSR. As compared with preoperative values, frequency of pain during sleep and during activities had significantly improved at 6 months and 4 years (P < .0001 for both). Likewise, the frequency of patient-ranked extreme shoulder pain at 6 months and 4 years had significantly reduced as compared with preoperative levels (P < .0001 for both) (Figure 2B).
Figure 2.
Mean patient-reported responses for (A) overall shoulder satisfaction (B) frequency of pain, (C) level of pain, and (D) shoulder function after reverse total shoulder replacement. Error bars indicate SEM. Statistically significant difference (Kruskal-Wallis test): ****P < .0001. RTSA, reverse total shoulder arthroplasty.
The level of pain was significantly better after surgery; the level of pain at rest improved significantly at 6 months and 4 years (P < .0001 for both); and the levels of pain during sleep and overhead activities significantly improved as well (P < .0001 for both) (Figure 2C). Patients also demonstrated significant improvement in subjective stiffness at 6 months and 4 years (P < .0001 for both); similarly, patients had significantly less difficulty performing overhead activities and reaching behind their backs (P < .0001 for both) (Figure 2D).
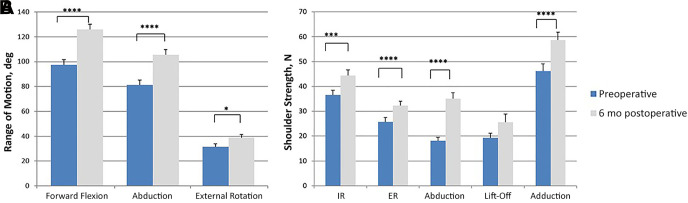
Regarding improvement in ROM, at 6 months postoperatively, there was a significant increase in abduction and forward flexion (P < .0001) and a less pronounced but still significant increase in external rotation (P = .04) when compared with preoperative values (Figure 3A). The increase in internal rotation was not statistically significant. Shoulder strength improved significantly pre- to postoperatively (Figure 3B).
Figure 3.
Improvement in (A) range of motion and (B) strength after reverse total shoulder arthroplasty. Statistically significant difference vs preoperative (paired sample t test): ****P < .0001. ***P < .001. *P < .05.
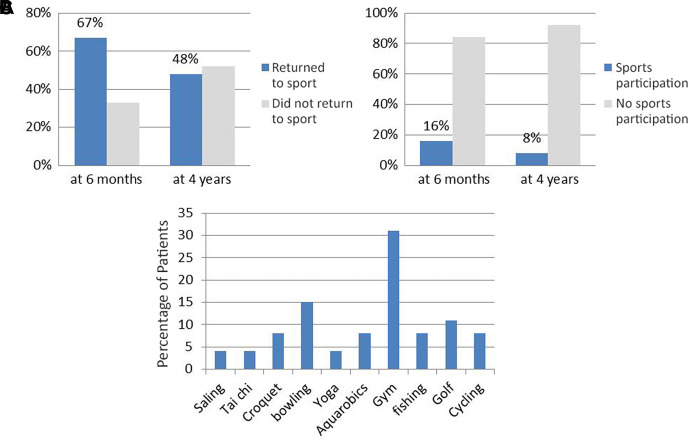
Preoperatively, 22% of patients indicated playing sports (15% hobby and 7% in a club). At 6 months postoperatively, 26% reported playing sports (19.5% hobby, 5.2% club, and 1.3% national). At the final follow-up, 17% were able to participate in sports (15% hobby and 2% club) (Figure 4).
Figure 4.
Levels of sports participation preoperatively, at 6 months postoperatively, and at a mean 4 years postoperatively.
For those who were involved in sporting activities preoperatively, the rate of return to sports was 67% at 6 months postoperatively and 48% at the final follow-up. The patients who indicated preoperatively that they did not play sports reported participating in sports postoperatively at a rate of 16% at 6 months and 8% at the final follow-up. The sports were mainly noncontact in nature. Some patients were involved in >1 sport. Gym/fitness, bowling, and golf were the most frequently mentioned sports (Figure 5).
Figure 5.
(A) Rates of return to sports at 6 months and 4 years after reverse total shoulder replacement. (B) Sports participation after surgery for those who could not participate before surgery. (C) Sports played as reported by patients at the most recent follow-up (4 years).
Results of the correlation analysis indicated that participation in sporting activities at 6 months after RTSR was significantly associated with younger age (r = –0.22, P = .049) and male sex (r = 0.24, P = .032). Overall, younger men had a higher chance of participating in sports. Participation in sports at 6 months also had a strong positive correlation with a preoperative ability to work (r = 0.39, P = .0005), sports participation (r = 0.41, P = .0002), and lift-off strength (r = 0.33, P = .008). The ability to perform sports at 6 months was positively correlated with 6-month overall satisfaction (r = 0.29, P = .01) and work (r = 0.38, P = .0004) as well as greater 6-month forward flexion (r = 0.30, P = .009) and abduction (r = 0.25, P = .036). With the exception of external rotation strength, muscle strength at 6 months was positively correlated with sports: internal rotation (r = 0.30, P = .01), abduction along scapular plane (r = 0.27, P = .02), liftoff (r = 0.27, P = .03), and adduction (r = 0.29, P = .01) (Table 2). Participation in sport at the most recent follow-up (4 years) was correlated only with sports participation preoperatively (r = 0.46, P = .0001) and sports participation at 6 months (r = 0.26, P = .02) (Table 3).
Table 2.
Factors Associated With Sports Participation at 6 Months Postoperatively a
| No. | r | P Value | OR | |
|---|---|---|---|---|
| Age | 83 | –0.22 | .049 | — |
| Sex b | 83 | 0.24 | .032 | 3.167 |
| Preoperative | ||||
| Work | 79 | 0.39 | .0005 | 9.130 |
| Sport | 79 | 0.41 | .0002 | 9.533 |
| Liftoff strength | 65 | 0.33 | .008 | — |
| At 6 mo | ||||
| Overall satisfaction | 81 | 0.29 | .01 | — |
| Work | 83 | 0.38 | .0004 | 5.885 |
| Forward flexion | 73 | 0.30 | .009 | — |
| Abduction | 73 | 0.25 | .036 | — |
| Strength at 6 mo | ||||
| Internal rotation | 72 | 0.30 | .01 | — |
| Abduction along scapular plane | 72 | 0.27 | .02 | — |
| Liftoff | 62 | 0.27 | .03 | — |
| Adduction | 71 | 0.29 | .01 | — |
a All P values indicate statistical significance (P < .05). Dashes indicate odds ratios can only be calculated for binary responses. OR, odds ratio.
b Female = 0, male = 1.
Table 3.
Factors Associated With Sports Participation at Final Follow-up a
| No. | r | P Value | OR | |
|---|---|---|---|---|
| Age | 108 | 0.013 | .49 | — |
| Sex b | 108 | –0.066 | .89 | — |
| Sports | ||||
| Preoperative | 99 | 0.46 | .0001 | 10.909 |
| 6 mo postoperative | 83 | 0.26 | .02 | 5.610 |
a Bold P values indicate statistical significance (P < .05). Dashes indicate odds ratios can only be calculated for binary responses. OR, odds ratio.
b Female = 0, male = 1.
Discussion
Patients in this study showed significant improvement in shoulder strength and ROM after RTSR, with 67% of patients who played sports preoperatively returning by 6 months and with 48% continuing participation at 4 years after surgery. In addition, 16% of the patients who were unable to play sports before surgery could do so by 6 months postoperatively, and 8% of them continued to play sports at 4 years.
Return to sports after RTSR is variable. Simovitch et al 17 reported 60% return to sports in a series of 67 patients. In a case series of 76 patients, Garcia et al 7 showed a slightly higher rate of return to sports (85%). Kolling et al 11 showed 77% return to sports activities after RTSR in a screening of the Swiss shoulder arthroplasty registry.
It is worth mentioning that the majority (78%) of our patients undergoing RTSR did not participate in sports preoperatively. However, the overall percentage of patients playing sports slightly increased after surgery, from 22% to 26% at 6 months. In the Garcia et al 7 case series and the Swiss study, 11 74% and 61% of patients participated in sports before surgery, respectively.
It was not surprising to find out that younger patients with better strength and higher ROM had better chances to return to sports. Younger age, male sex, strength (internal rotation, liftoff, abduction, and adduction), and ROM (forward flexion and abduction) all positively correlated with return to sports at 6 months postoperatively. However, these correlations were not maintained over time (at 4 years postoperatively), despite maintained positive outcomes. Social and/or medical factors might come into play.
Limitations
Our study has some limitations, including the relatively small number of patients. However, all data were collected prospectively, and the mean follow-up was long. Furthermore, surgery was performed by a single surgeon in 1 campus, and all patients had the same rehabilitation protocol. Another limitation is the loss of follow-up. The follow-up percentage was 64% (108/169 shoulders). Moreover, we did not explore the reasons (medical or social) why patients discontinued sports.
Conclusion
We found that the rate of return to sports after reverse shoulder replacement was high. Men were 3 times more likely than women to return to sports. Around two-thirds of the patients could go back to sports by 6 months after surgery. Those patients who returned to sports at 6 months were 5 times more likely to continue sports in the long term (4 years).
Footnotes
Final revision submitted August 3, 2022; accepted August 12, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: G.A.C.M. has received research support and consulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for the study was obtained from the South Eastern Sydney Local Health District (HREC 12/310; LNR/13/POWH/186).
References
- 1. Australian Orthopaedic Association National Joint Replacement Registry. Annual report 2020. Accessed November 22, 2020. https://aoanjrr.sahmri.com/annual-reports-2020 [DOI] [PubMed]
- 2. Boileau P, Gonzalez J-F, Chuinard C, Bicknell R, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg. 2009;18(4):600–606. [DOI] [PubMed] [Google Scholar]
- 3. Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15(5):527–540. doi:10.1016/j.jse.2006.01.003 [DOI] [PubMed] [Google Scholar]
- 4. Chelli M, Lo Cunsolo L, Gauci M-O, et al. Reverse shoulder arthroplasty in patients aged 65 years or younger: a systematic review of the literature. JSES Open Access. 2019;3(3):162–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ernstbrunner L, Andronic O, Grubhofer F, Camenzind RS, Wieser K, Gerber C. Long-term results of reverse total shoulder arthroplasty for rotator cuff dysfunction: a systematic review of longitudinal outcomes. J Shoulder Elbow Surg. 2019;28(4):774–781. doi:10.1016/j.jse.2018.10.005 [DOI] [PubMed] [Google Scholar]
- 6. Familiari F, Rojas J, Nedim Doral M, Huri G, McFarland EG. Reverse total shoulder arthroplasty. EFORT Open Rev. 2018;3(2):58–69. doi:10.1302/2058-5241.3.170044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Garcia GH, Taylor SA, DePalma BJ, et al. Patient activity levels after reverse total shoulder arthroplasty: what are patients doing? Am J Sports Med. 2015;43(11):2816–2821. [DOI] [PubMed] [Google Scholar]
- 8. Gerber C, Canonica S, Catanzaro S, Ernstbrunner L. Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: results after 15 years. J Shoulder Elbow Surg. 2018;27(5):831–838. [DOI] [PubMed] [Google Scholar]
- 9. Grammont P, Trouilloud P, Laffay JP, Deries X. Etude et réalisation d’une nouvelle prothèse d’épaule. Etude Réalis Une Nouv Prothèse Dépaule. 1987;39(10):407–418. [Google Scholar]
- 10. Hyun YS, Huri G, Garbis NG, McFarland EG. Uncommon indications for reverse total shoulder arthroplasty. Clin Orthop Surg. 2013;5(4):243–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kolling C, Borovac M, Audigé L, Mueller AM, Schwyzer H-K. Return to sports after reverse shoulder arthroplasty—the Swiss perspective. Int Orthop. 2018;42(5):1129–1135. [DOI] [PubMed] [Google Scholar]
- 12. Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007;89(2):292–300. [DOI] [PubMed] [Google Scholar]
- 13. L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79(5):738–748. [PubMed] [Google Scholar]
- 14. Petrillo S, Longo UG, Papalia R, Denaro V. Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: a systematic review. Musculoskelet Surg. 2017;101(2):105–112. [DOI] [PubMed] [Google Scholar]
- 15. Sevivas N, Ferreira N, Andrade R, et al. Reverse shoulder arthroplasty for irreparable massive rotator cuff tears: a systematic review with meta-analysis and meta-regression. J Shoulder Elbow Surg. 2017;26(9):e265–e277. [DOI] [PubMed] [Google Scholar]
- 16. Simovitch RW, Friedman RJ, Cheung EV, et al. Rate of improvement in clinical outcomes with anatomic and reverse total shoulder arthroplasty. JBJS. 2017;99(21):1801–1811. [DOI] [PubMed] [Google Scholar]
- 17. Simovitch RW, Gerard BK, Brees JA, Fullick R, Kearse JC. Outcomes of reverse total shoulder arthroplasty in a senior athletic population. J Shoulder Elbow Surg. 2015;24(9):1481–1485. [DOI] [PubMed] [Google Scholar]
- 18. Smith CD, Guyver P, Bunker TD. Indications for reverse shoulder replacement: a systematic review. J Bone Joint Surg Br. 2012;94(5):577–583. [DOI] [PubMed] [Google Scholar]