Abstract
The advent of arthroscopy in shoulder surgery has allowed for the development of minimally invasive techniques for the treatment of shoulder pathology. Further developments in needle arthroscopy have continued this trend toward less invasive shoulder surgery, allowing for decreased pain using smaller portals and decreased fluid irrigation through the shoulder joint during surgery. This technique describes a minimally invasive rotator cuff repair using a dual-lumen cannula that provides both direct visualization and direct instrument access to the pathology. This new cannula has the potential to further refine and to simplify needle arthroscopic techniques about the shoulder. With judicious patient selection, needle arthroscopy is a viable option for the treatment of common shoulder pathology.
Technique Video
A spinal needle is used to create a location for the standard lateral portal, and using a hemostat, the Passport Dual Lumen Cannula (Arthrex) is then inserted to be a working and viewing portal. A spinal needle is seen from superior, and lateral to the acromion, the placement for the medial 2 knotless anchors is located. A small stab incision is made and the punch is brought in, and while viewing from lateral, the medial anchors are placed. The medial swivel lock (Arthrex) anchors loaded with sutures are then placed in standard fashion. While viewing through the lateral portal with the NanoScope in the axillary lumen, a suture retriever is used to retrieve the suture tape coming out of the anterior-most anchor, and it is loaded into a Scorpion (Arthrex) suture passer. This passer is then used through the main lumen from the lateral portal to pass the anterior and posterior respective sutures through the rotator cuff. Those are then retrieved superiorly and cut to give 4 separate sutures. One anterior suture and 1 posterior suture are retrieved from lateral while still viewing with the NanoScope through the axillary lumen. These are placed through a knotless swivel lock, and the lateral row anchors are punched for from laterally in standard fashion. The anchors are then tensioned and placed into the bone while directly visualizing from the lateral portal. Final views of the repair and the shoulder are then seen.
Rotator cuff injuries and tears are common causes of pain and disability. The presence of rotator cuff tears increases as patients age, with full-thickness tears estimated to present in 25% of patients over the age of 60 years.1 Multiple risk factors have been associated with rotator cuff tears. Greater patient age is likely the most significant risk factor, but smoking, hyperlipidemia, and family history have also correlated with higher prevalence of rotator cuff tears.
Codman2 was the first to describe repairing the rotator cuff in an article back in 1911. Over time, the standard of care for surgical repair of rotator cuff tears has progressed from the larger open approach, to the mini open approach, to the arthroscopic approach. With the continued improvement in equipment and technique, the arthroscopic approach to rotator cuff repair has been shown to produce equivalent or superior results.3 These advancements in arthroscopy have allowed for shoulder surgery with less invasive approaches intended to improve patient outcomes and decrease pain. Developments and advancements in arthroscopy have allowed for shoulder surgery with less invasive approaches in hopes to improve patient outcomes and decrease pain. Various needle arthroscopic techniques have been described. A surgical technique for repairing the rotator cuff with the NanoScope (Arthrex) and a single incision have previously been described by Lavender et al.4 Using the NanoScope allows for smaller incisions, less fluid use and swelling, and in theory less pain in the early postoperative period. This article describes rotator cuff repair using the NanoScope with a new dual-lumen cannula designed to improve direct visualization. This allows the surgeon to visualize and work through the same cannula simultaneously.
Technique
Positioning
The patient is placed in the lateral position with the operative extremity placed in traction and an axillary roll placed appropriately. All bony prominences are well padded and an extremity drape placed.
Posterior Portal Creation
A spinal needle is placed into the subacromial space from posterior and medial and inferior to the lateral acromion. A nitinol wire is then placed through that spinal needle, and a curved high-flow sheath is then placed over that wire. A small incision may need to be made for passage of the sheath. The nitinol wire is then removed from the sheath. At this point, the NanoScope can be placed into that cannula after flow is established (Video 1).
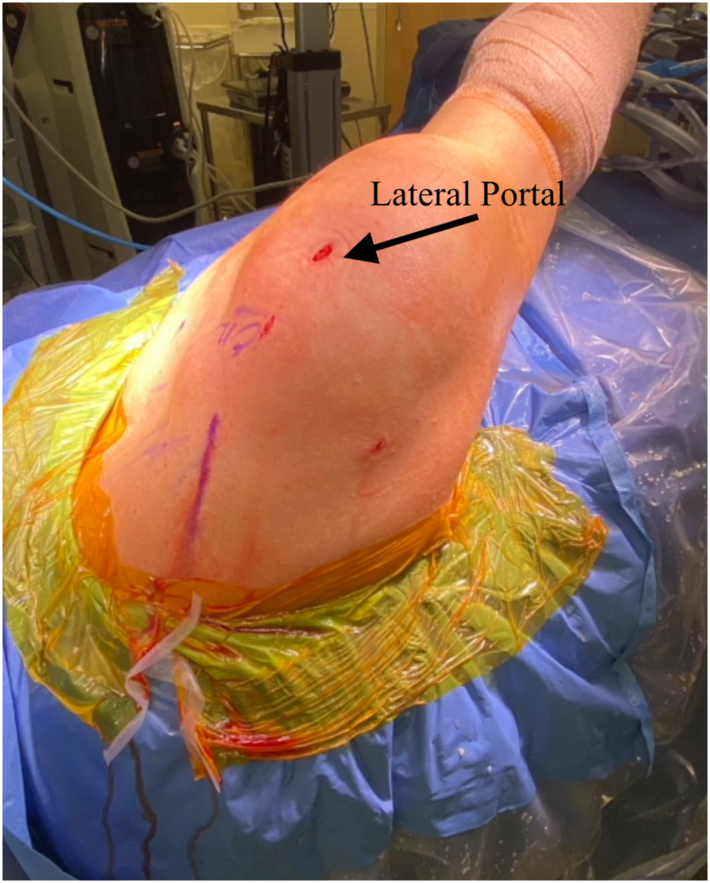
Lateral Portal Creation
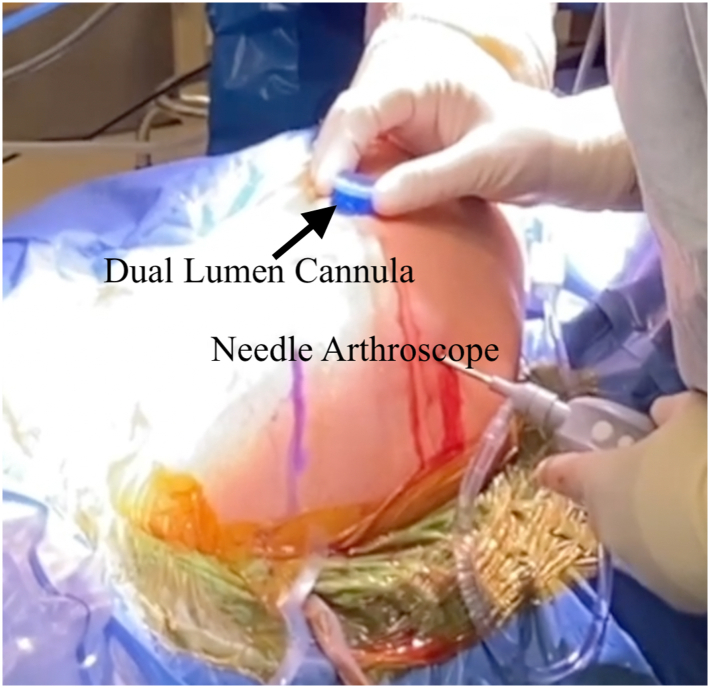
A spinal needle is used to create a location for the standard lateral portal. A slightly curved hemostat is clamped around a Passport Dual Lumen Cannula (Arthrex), and this cannula is inserted using the hemostat. This portal will be used during the case as both the working and viewing portal (Fig 1).
Fig 1.
A view from outside of the right shoulder with the arm in the lateral position showing the NanoScope placed into the lateral portal and a Passport dual-lumen cannula placed laterally.
Percutaneous Medial Anchor Placement
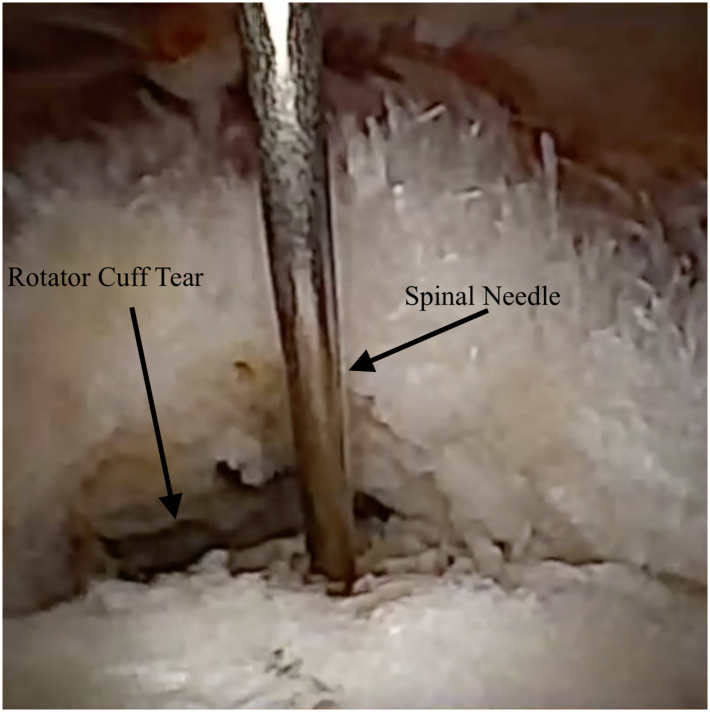
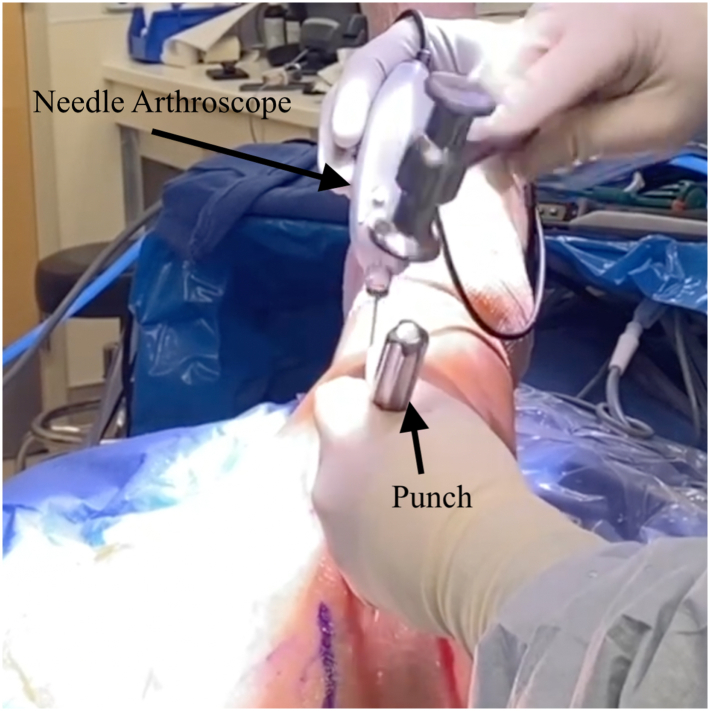
Using a spinal needle from superior and lateral to the acromion, the placement for the medial 2 knotless anchors is located. A small stab incision is made and the punch is brought in, and while viewing from lateral, the medial anchors are placed (Fig 2, Fig 3, Fig 4). The medial swivel lock (Arthrex) anchors loaded with sutures are then placed in standard fashion.
Fig 2.
Viewing from the lateral portal of the right shoulder with the arm in the lateral position with the 0° NanoScope, a spinal needle from superior localizes the location for the medial anchors.
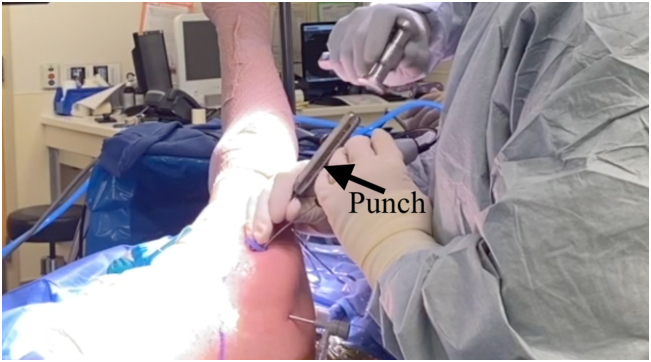
Fig 3.
A view of the right shoulder with the arm in the lateral position from outside of the joint showing the punch being used from superior and the NanoScope viewing from laterally.
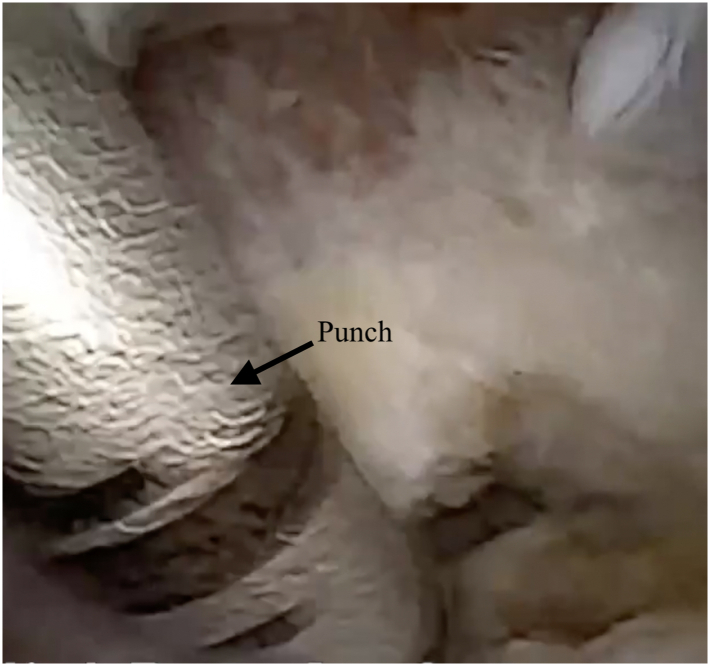
Fig 4.
Viewing right shoulder with the arm in the lateral position from the lateral portal with the 0° NanoScope, the punch is being used from the superior portal to punch for the medial anchors.
Suture Passage
While viewing through the lateral portal with the NanoScope in the axillary lumen, a suture retriever is used to retrieve the suture tape coming out of the anterior-most anchor, and it is loaded into a scorpion (Arthrex) suture passer. This passer is then used through the main lumen from the lateral portal to pass the anterior and posterior respective sutures through the rotator cuff (Figs 5 and 6). Those are then retrieved superiorly and cut to give 4 separate sutures. It is important to retrieve those sutures superiorly before pulling the entire suture out the lateral portal to prevent knots.
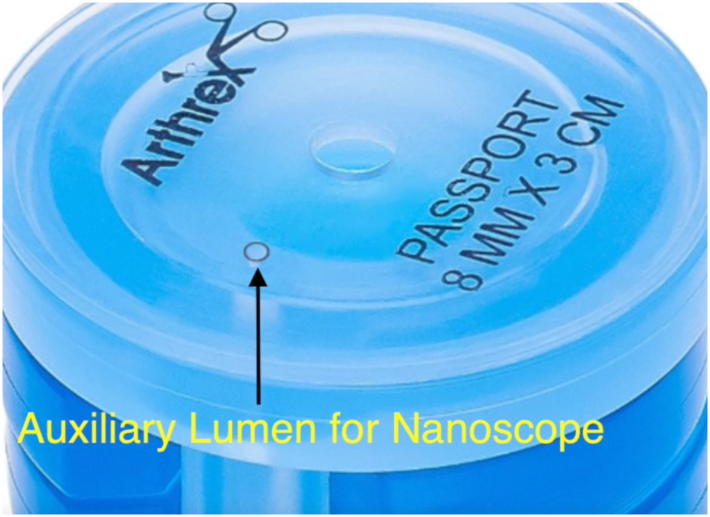
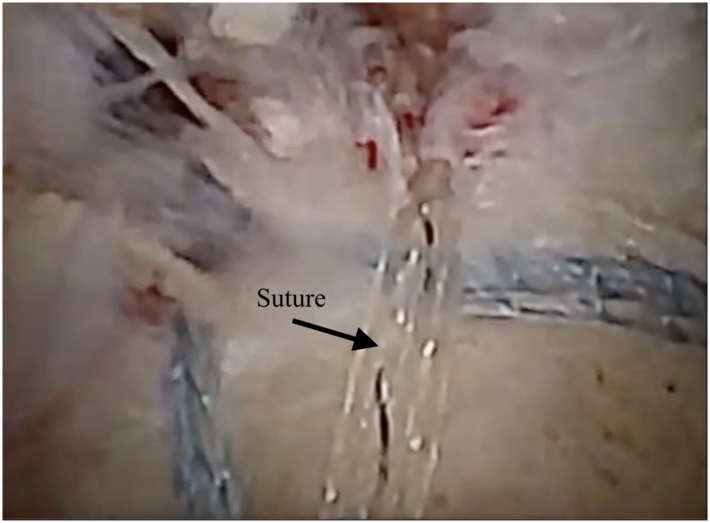
Fig 5.
An image of the right shoulder with the arm in the lateral position with the Passport cannula with an axillary lumen for the NanoScope.
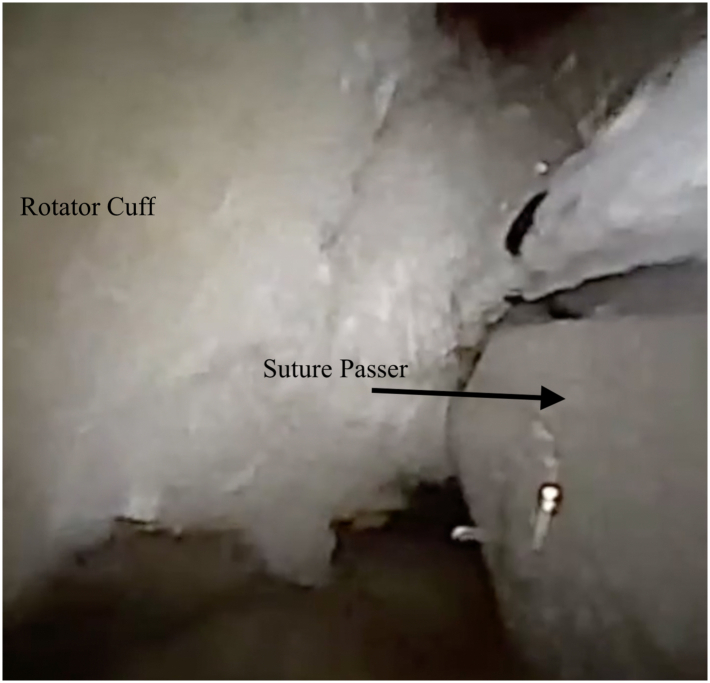
Fig 6.
Viewing the right shoulder with the arm in the lateral position from the lateral portal with the 0° NanoScope while the Scorpion is used to pass the anterior sutures into the rotator cuff from the same portal.
Lateral Row
One anterior suture and 1 posterior suture are retrieved from lateral while still viewing with the NanoScope through the axillary lumen. These are placed through a knotless swivel lock, and the lateral row anchors are punched for from laterally in standard fashion (Fig 7, Fig 8, Fig 9, Fig 10). The anchors are then tensioned and placed into the bone while directly visualizing from the lateral portal.
Fig 7.
A view of the right shoulder with the arm in the lateral position from outside the joint showing the punch being used for the lateral anchor while the NanoScope is being used to view from the same portal.
Fig 8.
Viewing the right shoulder with the arm in the lateral position from the lateral portal with the 0° NanoScope while punching from the same portal for the lateral row anchors.
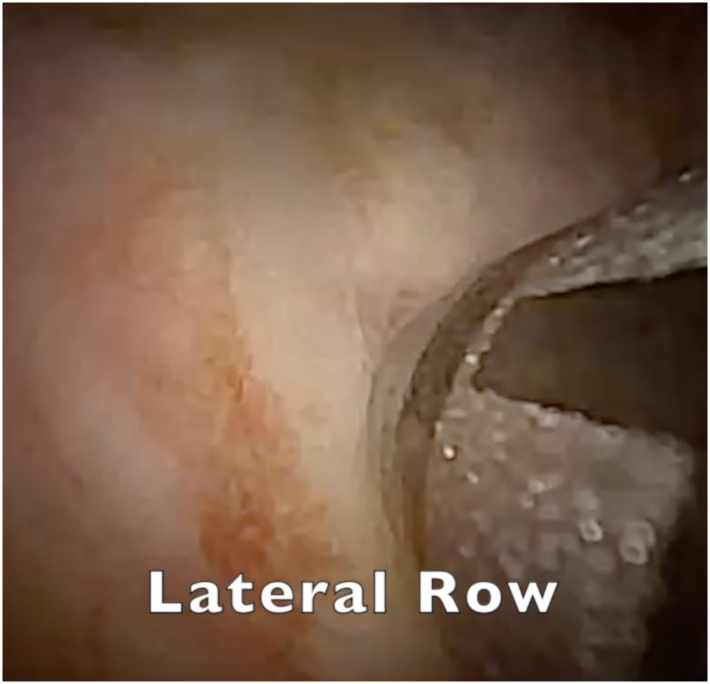
Fig 9.
Viewing the right shoulder with the arm in the lateral position from the lateral portal with the 0° NanoScope, the final rotator cuff repair can be seen.
Fig 10.
A final view of the right shoulder with the arm in the lateral position showing small portals and the posterior portal is percutaneous.
Discussion
The goal of developing minimally invasive arthroscopic techniques about the shoulder is to improve patient outcomes, decrease postoperative pain, and improve visualization of pathology. Postoperative pain following rotator cuff repair continues to be a significant problem. Clinicians have used a variety of analgesics, nerve blocks, and different rehabilitation protocols to decrease postoperative pain. In a recent systematic review, the authors advocated for the use of arthroscopic repair, paracetamol, nonsteroidal anti-inflammatory drugs, dexamethasone, a regional nerve block, and the prescription of opioids for breakthrough pain.5 The rationale for attempting to broaden the indication for the use of the NanoScope in arthroscopic rotator cuff surgery stems from our belief that smaller portals, less fluid irrigation through the joint, and less damage to the surrounding tissues may lead to quicker recovery, less postoperative pain, and decreased opioid use (Table 1). This is an area that still needs to be further studied.
Table 1.
Advantages and Disadvantages of Nanoscopic Rotator Cuff Repair
| Advantages |
| Smaller portals |
| Less need for fluid |
| Less swelling |
| Less damage to surrounding soft tissue |
| Disadvantages |
| The NanoScope is an added cost |
| Need more precise portals or may have difficult viewing angles |
Despite these potential advantages, the small diameter and decreased fluid flow when using the NanoScope can result in difficulty obtaining proper visualization. Additionally, the 0-degree viewing angle necessitates positioning the NanoScope closer to the pathology as compared to a standard 30-degree scope. This article demonstrates that the use of a flexible double-lumen cannula greatly improves visualization of the rotator cuff during repair. The cannula also facilitates smooth, nontraumatic passage of implants and instruments during the completion of the repair. Additionally, we demonstrate that the repair can be performed with minimal bursectomy, which may help decrease bleeding and improve healing by preserving mesenchymal stem cells in the area.6
Utilizing a NanoScope for rotator cuff repair does have other potential limitations and drawbacks. Indications for its use are limited by the type and size of the rotator cuff tear (Table 2). The surgeon may have difficulty manipulating and reducing large, significantly retracted tears when the NanoScope and working instruments are passed through the same dual-lumen cannula. If other procedures such as subscapularis repair, arthroscopic biceps tenodesis, or distal clavicle resection are performed during the shoulder surgery, a standard 30-degree arthroscope may be needed.4 The NanoScope may still be useful in these situations, however, as a hybrid dual-scope visualization technique with the NanoScope in the Passport laterally and standard scope posteriorly may aid in visualization of larger rotator cuff tears.
Table 2.
Current Indications and Contraindications for Needle Arthroscopy of the Shoulder
| Indications |
| Partial-thickness tears |
| Isolated bursal or articular-sided tears |
| Smaller or nonretracted rotator cuff tears |
| Anterior or posterior labral tears |
| Relative contraindications |
| Larger or retracted rotator cuff tears |
| Concomitant procedures such as distal clavicle excision, biceps tenodesis |
| Subscapularis repair |
As we continue to try and expand the use of the NanoScope in the shoulder, we hope that describing the use of the dual-lumen cannula and its improved visualization will help those who may have concerns about using the NanoScope for rotator cuff repairs. Indications for needle arthroscopy are constantly expanding and are mostly surgeon dependent. Visualization using a 0-degree scope is technically demanding and requires optimal portal placement. As more experience is gained, needle arthroscopy may have an increasing role in the management of orthopaedic shoulder pathology.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A spinal needle is used to create a location for the standard lateral portal, and using a hemostat, the Passport Dual Lumen Cannula (Arthrex) is then inserted to be a working and viewing portal. A spinal needle is seen from superior, and lateral to the acromion, the placement for the medial 2 knotless anchors is located. A small stab incision is made and the punch is brought in, and while viewing from lateral, the medial anchors are placed. The medial swivel lock (Arthrex) anchors loaded with sutures are then placed in standard fashion. While viewing through the lateral portal with the NanoScope in the axillary lumen, a suture retriever is used to retrieve the suture tape coming out of the anterior-most anchor, and it is loaded into a Scorpion (Arthrex) suture passer. This passer is then used through the main lumen from the lateral portal to pass the anterior and posterior respective sutures through the rotator cuff. Those are then retrieved superiorly and cut to give 4 separate sutures. One anterior suture and 1 posterior suture are retrieved from lateral while still viewing with the NanoScope through the axillary lumen. These are placed through a knotless swivel lock, and the lateral row anchors are punched for from laterally in standard fashion. The anchors are then tensioned and placed into the bone while directly visualizing from the lateral portal. Final views of the repair and the shoulder are then seen.
References
- 1.Tashjian R.Z. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604. doi: 10.1016/j.csm.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Codman E.A. Complete rupture of the supraspinatus tendon. Operative treatment with report of two successful cases. 1911. J Shoulder Elbow Surg. 2011;20(3):347–349. doi: 10.1016/j.jse.2010.10.031. [DOI] [PubMed] [Google Scholar]
- 3.Liu J., Fan L., Zhu Y., Yu H., Xu T., Li G. Comparison of clinical outcomes in all-arthroscopic versus mini-open repair of rotator cuff tears. Medicine (Baltimore) 2017;96(11):e6322. doi: 10.1097/MD.0000000000006322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lavender C., Lycans D., Sina Adil S.A., Berdis G. Single-incision rotator cuff repair with a needle arthroscope. Arthrosc Tech. 2020;9(4):e419–e423. doi: 10.1016/j.eats.2019.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toma O., Persoons B., Pogatzki-Zahn E., Van de Velde M., Joshi G.P. PROSPECT guideline for rotator cuff repair surgery: Systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2019;74(10):1320–1331. doi: 10.1111/anae.14796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freislederer F., Dittrich M., Scheibel M. Biological augmentation with subacromial bursa in arthroscopic rotator cuff repair. Arthrosc Tech. 2019;8(7):e741–e747. doi: 10.1016/j.eats.2019.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A spinal needle is used to create a location for the standard lateral portal, and using a hemostat, the Passport Dual Lumen Cannula (Arthrex) is then inserted to be a working and viewing portal. A spinal needle is seen from superior, and lateral to the acromion, the placement for the medial 2 knotless anchors is located. A small stab incision is made and the punch is brought in, and while viewing from lateral, the medial anchors are placed. The medial swivel lock (Arthrex) anchors loaded with sutures are then placed in standard fashion. While viewing through the lateral portal with the NanoScope in the axillary lumen, a suture retriever is used to retrieve the suture tape coming out of the anterior-most anchor, and it is loaded into a Scorpion (Arthrex) suture passer. This passer is then used through the main lumen from the lateral portal to pass the anterior and posterior respective sutures through the rotator cuff. Those are then retrieved superiorly and cut to give 4 separate sutures. One anterior suture and 1 posterior suture are retrieved from lateral while still viewing with the NanoScope through the axillary lumen. These are placed through a knotless swivel lock, and the lateral row anchors are punched for from laterally in standard fashion. The anchors are then tensioned and placed into the bone while directly visualizing from the lateral portal. Final views of the repair and the shoulder are then seen.
A spinal needle is used to create a location for the standard lateral portal, and using a hemostat, the Passport Dual Lumen Cannula (Arthrex) is then inserted to be a working and viewing portal. A spinal needle is seen from superior, and lateral to the acromion, the placement for the medial 2 knotless anchors is located. A small stab incision is made and the punch is brought in, and while viewing from lateral, the medial anchors are placed. The medial swivel lock (Arthrex) anchors loaded with sutures are then placed in standard fashion. While viewing through the lateral portal with the NanoScope in the axillary lumen, a suture retriever is used to retrieve the suture tape coming out of the anterior-most anchor, and it is loaded into a Scorpion (Arthrex) suture passer. This passer is then used through the main lumen from the lateral portal to pass the anterior and posterior respective sutures through the rotator cuff. Those are then retrieved superiorly and cut to give 4 separate sutures. One anterior suture and 1 posterior suture are retrieved from lateral while still viewing with the NanoScope through the axillary lumen. These are placed through a knotless swivel lock, and the lateral row anchors are punched for from laterally in standard fashion. The anchors are then tensioned and placed into the bone while directly visualizing from the lateral portal. Final views of the repair and the shoulder are then seen.