Version Changes
Revised. Amendments from Version 1
There were modifications in the title, in the case report describing more the semiology of the abdominal pain.
Abstract
Pneumatosis cystoid intestinalis is a rare disease reported in the literature affecting 0.03% of the population. It has a variety of causes and its manifestation may change widely. It usually presents as a marginal finding resulting from various gastrointestinal pathologies. In the acute complicated form of pneumatosis intestinalis, management is challenging for physicians and surgeons.
We present a case of a 60-year-old patient who was admitted to our surgical department with a symptomatology suggestive of small bowel occlusion. Computed tomography demonstrated ileal volvulus associated with parietal signs suffering and pneumoperitoneum. An emergent exploratory laparoscopy followed by conversion was performed demonstrating segmental ileal pneumatosis intestinalis secondary to a small bowel volvulus due to an inflammatory appendix wrapping around the distal ileum. Further, detorsion, retrograde draining, and appendectomy were performed because there were no signs of necrosis and the appendix was pathological. The postoperative course was uneventful.
This case is exceedingly rare in the literature, because it was featured by the ileal volvulus due to appendicitis.This case report emphasizes the importance of surgical procedures in the management of symptomatic pneumatosis intestinalis associated to an acute abdomen.
Keywords: Pneumatosis cystoid intestinalis, small bowel volvulus, acute abdomen, case report
Introduction
Pneumatosis cystoid intestinalis (PCI) is a low-incidence pathology defined by the existence of air in the small intestine or colon wall. 1 PCI can affect any portion of the gastrointestinal tract and could be present in any layer such as the mucosa, submucosa, or subserosa. 1– 3 It can either be presented as a secondary form in 85% of cases or an idiopathic form in 15% of cases. 1, 2 The secondary pattern occurs more frequently in gastrointestinal causes such as bowel obstruction. 3, 4 The management of PCI is challenging to surgeons especially in symptomatic cases. 5 We report a rare case of ileal pneumatosis cystoides associated with small bowel volvulus, presenting with acute abdominal pain. This case is exceedingly rare in the literature, because it was featured by the ileal volvulus due to appendicitis.
Case report
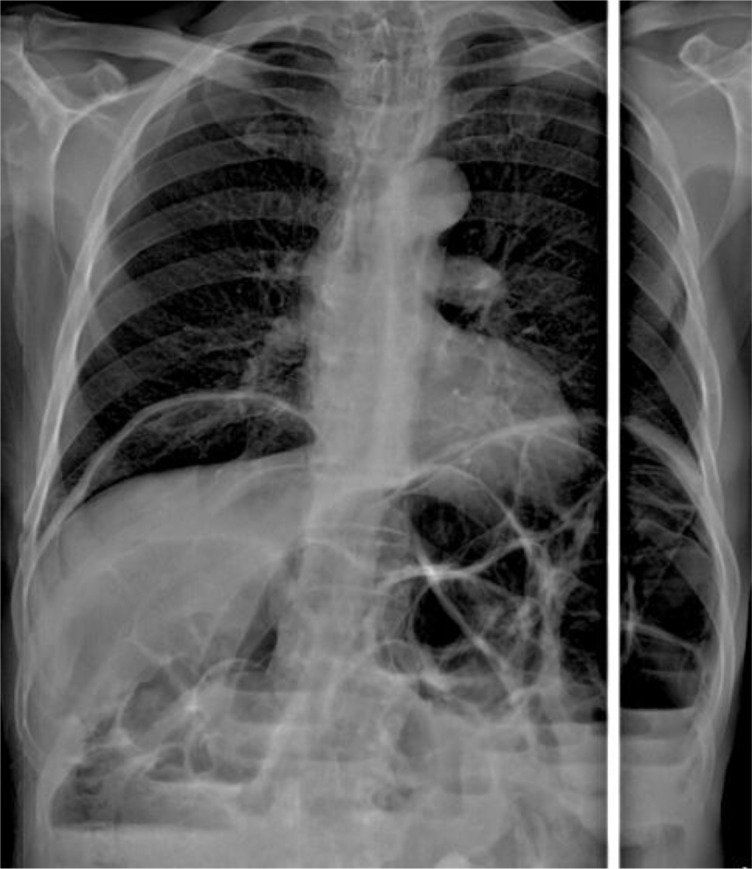
A 60-year-old retired, north African male patient without any medical or surgical history consulted the emergency department for 24 hours of abdominal pain, distension, and vomiting. The patient had experienced this pain a year earlier, but did not consult any doctor, and the pain faded away spontaneously. On physical examination, tachycardia and distended tympanic abdomen with mild tenderness were noted. White blood count was 8840 E/mm 3 and C reactive protein was 36 mg/l (normal values: White blood count: 4000E/mm 3, and C reactive protein: 1 mg/l). X-ray of thorax and abdomen showed dilated small bowel, multiple fluid levels and pneumoperitoneum ( Figure 1).
Figure 1. Dilated small bowel, multiple fluid levels and pneumoperitoneum on X-ray.
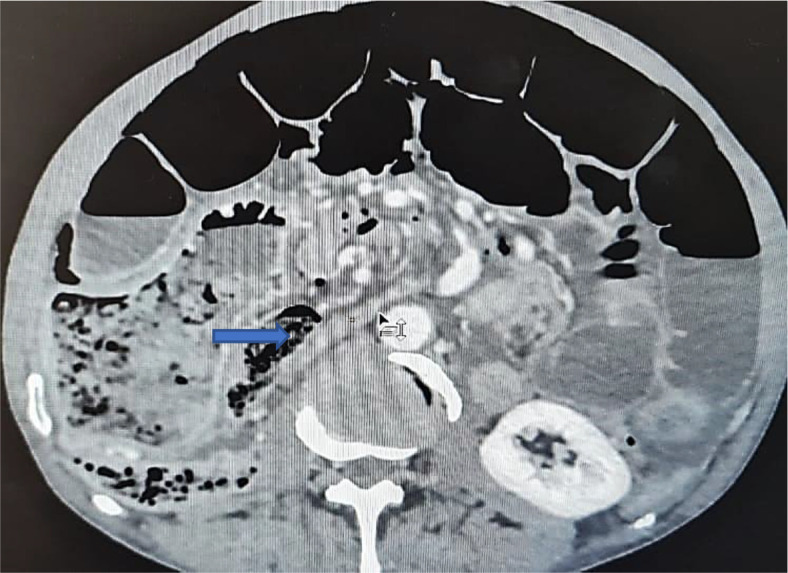
An abdominal CT scan was performed, revealing distended small bowel loops upstreaming transitional levels like a ‘whirl sign’ ( Figure 2), a bubbly pattern across the length of the small bowel associated with parietal suffering signs ( Figure 3), abundant pneumoperitoneum ( Figure 4), and a pathological meso-celiac appendix ( Figure 5). The CT scan suggested a diagnosis of ileal volvulus due to the meso-celiac appendix.
Figure 2. Ileal volvulus: dilated bowel segments associated with whirl sign.
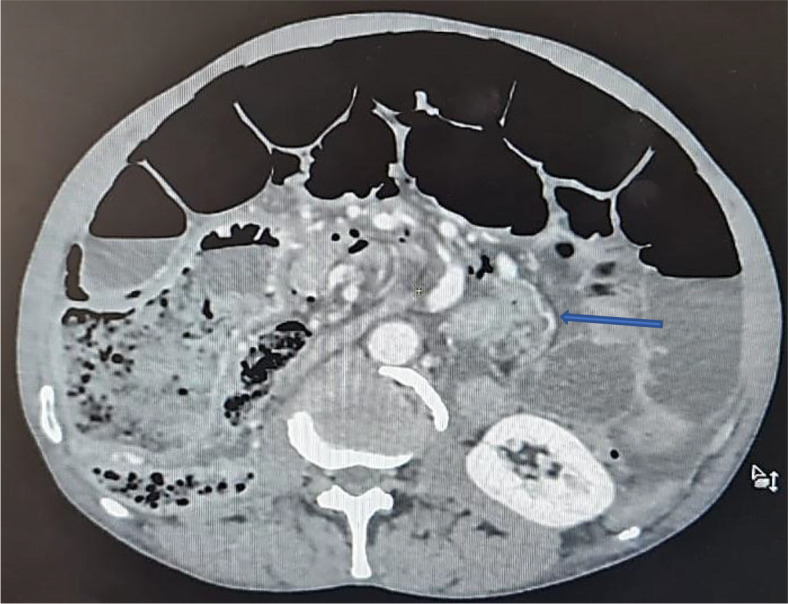
Figure 3. Multiple bubble lesions among ileal loops on Abdominal CT.

Figure 4. Abundant pneumoperitoneum.
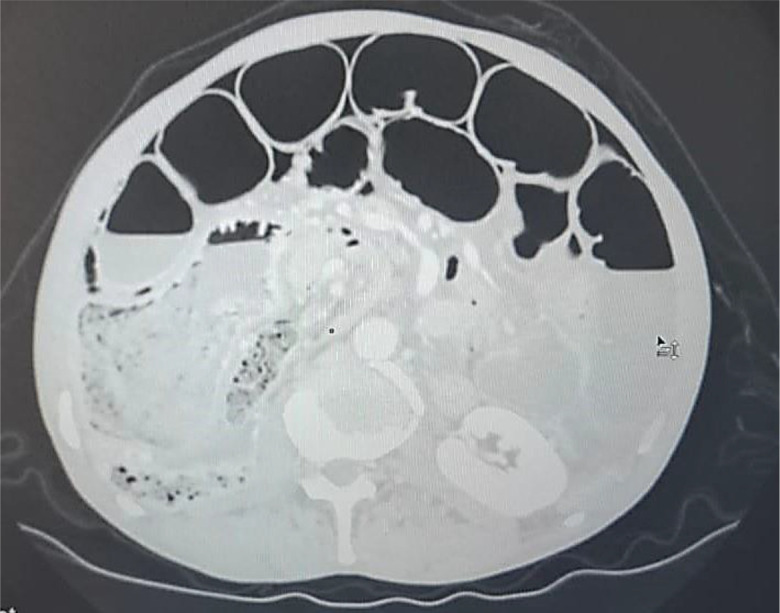
Figure 5. The inflammatory appendix.
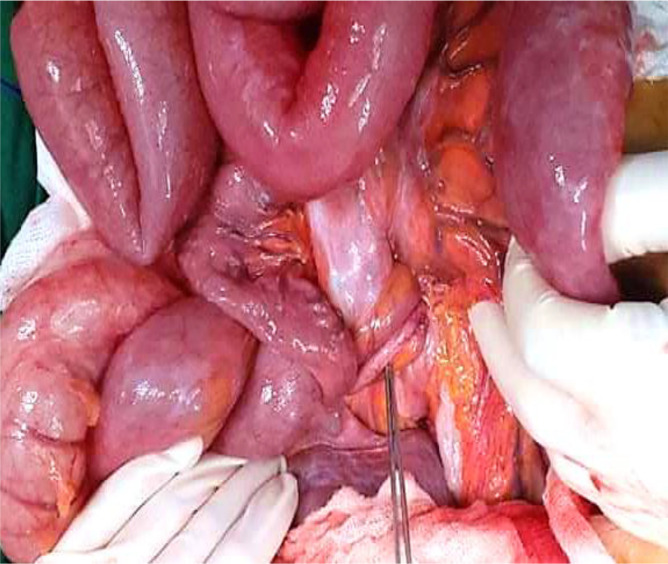
We initially decided to perform laparoscopy. Intraoperatively, small bowel loops were much dilated not allowing intraperitoneal exploration. Gas-filled cystic lesions on small bowel serosa were identified. There was no evidence of perforation. We did choose to convert into midline incision for better and prudent exploration. A volvulus was found, involving a two-and-a-half clockwise turn around a long, pendulous small bowel mesentery, the strangled bowel was greatly congested ( Figure 6). At the base of the volvulus, an inflammatory appendix was wrapped around the last loop of the ileum ( Figure 7). Also, multiple gas-filled subserosal cysts, differently sized, on the wall of the ileum were encountered ( Figure 8). When the ileum was re-rotated, small bowel loops had preserved vitality. The entire colon was normal. Detorsion, retrograde draining, and appendectomy were performed because there were no signs of necrosis and the appendix was pathological.
Figure 6. Ileal loop volvulus, involving a two-and-a-half clockwise turn around a long, pendulous small bowel mesentery.
Figure 7. At the base of the volvulus, the inflammatory appendix wrapped around the last loop of the ileum.
Figure 8. Segmental pneumatosis intestinalis involving the ileal loops.
Postoperatively, the patient completed a five-day course of intravenous metronidazole 500 mg three times a day. There were no postoperative complications. Anatomopathological examination revealed an inflammatory appendix without malignancy. A lower endoscopy was completed after surgery. It showed the presence of two polyps on the rectum and the transverse colon in low-grade dysplasia with no other lesions that were resected. There was no malignancy on the anatomopathological examination. The patient was monitored regularly, and the long-term post-operative course was uneventful.
Discussion
PCI is an uncommon disease (0.03% of adults) 6 and its pathogenesis is still not clear. 7 According to its etiology, literature classifies this entity mainly as primary or secondary type. 8 There is also an idiopathic type which usually affects the left colon and is rarely reported in the literature. We found that thirteen cases of primary PCI have been described in the international literature ( Table 1). The secondary type frequently affects the small intestine and the right colon. 9 Its pathogenesis is multifactorial and can be explained by 3 theories: mucosal disruption, bacterial theory, and pulmonary disease. 1, 7, 10, 11 The mucosal disruption is due to the dissemination of bowel gas through a mucosal defect into lymphatic channels. 1, 10 Wu et al. 12 found that high altitude is a new theory explaining PCI’s pathogenesis. Highland areas induce passage of intraluminal gas into the submucosa damaging the mucosa. Mucosal damage can result from bowel occlusion, inflammatory process, and cytotoxic medical treatment. 11 The pulmonary cause is confirmed in patients with asthma and chronic bronchitis. In these cases, the rupture of alveoli causes the migration of air bubbles from interstitial spaces through the mediastinum and from the retroperitoneum to the blood vessel of the intestinal wall. 1, 8, 10 However, the bacterial theory is explained by entry of bacterial gas due to a defect on the bowel wall lymphoid tissue. 8, 10 This mechanism can justify the use of antibiotics. 1 Chemotherapy or hormonal therapy, and systemic sclerosis were also reported in the literature as a cause of PCI. 1 Finally, while keeping in mind these theories, their pathogenesis has not been yet fully clarified. 1
Table 1. Review of the literature (2008-2021) illustrating cases of idiopathic PCI, and PCI secondary to surgical etiologies.
| Author | Age | Physical examination | Abdominal radiography | CT scan | Treatment | Etiology of PCI |
|---|---|---|---|---|---|---|
| Year | M/F | |||||
|
González
et al.
20
2021 |
66 Y | Normal | __ | Intestinal pneumatosis | Conservative: surveillance | Primary |
| M | ||||||
|
Moyon
et al.
6
2020 |
79 Y | Tachycardia
Abdominal distension Mild pain on the lower abdomen without tenderness |
-- | The bubbly pattern across the length of the small bowel, Multiple cystic round shapes in the wall of the jejunum, and its mesentery, Large pneumoperitoneum | 1/
Conservative:
surveillance+ oxygen+ broad-spectrum antibiotics
2/Worsening pain laparoscopy : No evidence of perforation/gas-filled cystic lesions |
Primary |
| M | ||||||
|
Takahashi
et al.
21
2019 |
17 Y | Mobile mass in the right lower quadrant | __ | Colocolic intussusception of the ascending colon with air in the bowel wall | Endoscopy: fine-needle aspiration | Primary |
| F | ||||||
|
Suda
et al.
22
2018 |
80 Y | Slight abdominal distention | Dilatation and retention of gas in a segment of the small intestinal wall | Massive gas-filled cysts within the wall and mesentery of the small intestine
No portal venous gas No intestinal ischemia |
Conservative: antibiotics | Primary |
| M | ||||||
|
Wang
et al.
23
2018 |
56 Y | Normal | Normal | -- | High-frequency electrosurgical resection of the gas cysts + ATB Bifidobacterium | Primary |
| M | ||||||
|
Romano-Munive
et al.
24
2017 |
54 Y | Normal | __ | Pneumatosis cystoides intestinalis | Conservative | Primary |
| F | ||||||
|
Furihata
et al.
15
2016 |
81 Y | Severe epigastric tenderness + distension No peritoneal signs | Massive free gas bilaterally in the subdiaphragmatic spaces | Massive free gas
bilaterally under the diaphragm |
Conservative: intravenous infusion of antibiotics, and nasogastric intubation | Secondary to chronic obstipation |
| M | ||||||
|
Fraga
et al.
25
2016 |
66 Y | Abdominal distention
No signs of peritonitis |
-- | Gas in the abdominal wall, at the level of the transverse and rectosigmoid colon | Conservative | Primary |
| F | ||||||
|
Tseng
et al.
26
2014 |
50 Y | Abdominal distension without tenderness | Gas in the bowel wall | Pneumatosis intestinalis of the right side of the colon | Conservative | Primary |
| F | ||||||
|
Slesser
et al.
5
2011 |
74 Y | Abdominal distention
Soft and non-tender |
Bilateral free subdiaphragmatic air | Extensive pneumatosis intestinalis involving the small bowel with free intraperitoneal air
secondary to malrotation of the proximal small bowel |
Laparotomy: Extensive and bulky pneumatosis intestinalis extending from the duodenal–jejunal flexure to the terminal ileum | Primary |
| M | ||||||
|
Nagata
et al.
27
2010 |
23 Y | Tenderness in the right iliac fossa | -- | Intussusception of the ascending colon
Ovoid radiolucencies with smooth margins |
Intussusception easily resolved by
colonoscopy
Laparoscopy-assisted partial ascending colectomy was performed 1 month after his initial presentation |
Primary |
| M | ||||||
|
Arora
et al.
4
2009 |
27 Y | Signs of acute abdomen | Gas under the diaphragm | -- | Laparotomy: Perforated duodenal ulcer + The terminal 180 cm of the small bowel to the ileocecal junction showed multiple thin-walled, tense, air-filled cysts on the serosal surface → Limited right colectomy and resection of the involved small bowel | Secondary to a surgical cause |
| M | ||||||
|
Liau
et al.
3
2008 |
76 Y | Signs of generalized peritonitis | Massive subdiaphragmatic air and multiple dilated loops of small bowel with well-demarcated wall | Pneumoperitoneum gas-filled cysts on the wall of small bowel loops |
Laparotomy:
extensive small bowel infarction due to volvulus of most of the small bowels, multiple gas-filled subserosal cysts on the wall of the ileum
small bowel resection+ jejunoileal anastomosis |
Secondary to a congenitally long mesentery |
| M |
Besides, the disease’s location on the digestif tractus may be helpful to guide the etiology. So pyloric stenosis or gastric cancer can lead to a proximal pathology; however distant one might be due to mesenteric ischemia or diverticulitis. 9
PCI is a rare entity reported in the literature, but nowadays PCI reports’ number has been increasing because of the widespread use of CT scan and colonoscopy. 9 This pathology is more frequently asymptomatic. 1 Whereas in some cases, they may present with symptoms such as abdominal pain, constipation, distension, diarrhea, or bleeding. 8, 9 Incidentally PCI can induce surgical complications such as bowel obstruction, intestinal perforation, volvulus, intussusception, and bleeding, which require surgical intervention. 13
Intestinal obstruction can be a rare complication of PCI. This event depends on the size and number of the cysts which lead in certain cases to a reduction of the intestinal lumen, volvulus, perforation, and hemorrhage. 7, 11 In the literature, PCI associated with volvulus is much more uncommon. Besides this association, one of the highlights of our case is the long and hypermobile small bowel mesentery. Moreover, PCI is discussed to be a mechanical factor leading to irreversible volvulus, also it is disputed that volvulus contributes to ischemia which is an etiological factor leading to PCI. 3, 14
Imaging findings may be helpful to confirm PCI diagnosis, especially on CT scans. 1, 6 Computed tomography can show a grape cluster aspect within the wall of the intestine. 1 Three patterns of pneumatosis have been reported in the literature using CT scan imaging: bubble cystoid, a linear pattern, and a circular pattern. 1
Pneumoperitoneum can be explained by the rupture of the cyst on the wall intestine, without any evidence of peritoneal irritation or digestive perforation, like in our case. So that we should be wise to correlate clinical and radiographic findings, when free air is present below the diaphragm in chest X-ray. 8, 9 Pneumatosis intestinalis and portomesenteric venous gas (PVG) are generally debated independently in the literature. This association of radiological findings usually concludes to the presence of mesenteric infarction, but they may indicate occasionally nonischemic conditions. So that their presence should not be always regarded as signs of severity. 13, 15, 16 Moreover, according to literature, the rare findings of PCI and PVG can be present in asymptomatic patients without ominous signs, as described in the series of Sooby et al., 17 including 88 patients with PCI/PVG of which 19 with benign PCI, and of these 19, 6 patients had both PCI and PVG. These patients were put under surveillance, and they had no uneventful recovery.
The management of PCI is not well established, there are no standard therapeutic rules. 10 However, the mandatory in its management is to judge whenever it is benign or life-threatening. 11 So that it is established that if a CT scan shows intestinal infarction, urgent surgery is mandated. If no signs of intestinal damage is found, a conservative treatment is regarded to be ideal. 13 The common conservative procedure is to use metronidazole Antibiotics, which affects intestinal bacteria by the suppression of hydrogen production, and hyperbaric oxygen therapy. 2, 6, 8, 10 Nevertheless, a surgical procedure is indicated in complications such as peritoneal irritation or intestinal obstruction. 2, 10
The second particularity in our case is that the volvulus of the small bowel is due to acute appendicitis. This entity is explained by the wrapping of the appendix, due to its particular length, around the ileum occurring volvulus and strangulation. 18, 19 According to the literature, this mechanism resulted from adhesion of the inflamed appendix to the posterior peritoneum forming a turn of the spire of the ileum last loop resulting in volvulus. 18, 19 In summary, our case is exceedingly rare in the literature, featured by the ileal volvulus due to appendicitis.
Conclusion
PCI is a rare disease whose diagnosis is offering a challenge for surgeons. This rare condition can often be associated with benign diseases or it can be proof of intestinal necrosis. Although surgery is mandatory in the complicated pattern, the treatment of asymptomatic forms is more likely conservative. Besides, both surgical and medical approaches can efficiently compete with these challenging diagnoses.
Data availability
All data underlying the results are available as part of the article and no additional source data are required.
Consent
Written informed consent was obtained from the patient regarding the publication of this case report.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 2; peer review: 1 approved
References
- 1. Sugihara Y, Harada K, Ogawa H, et al. : Pneumatosis Cystoides Intestinalis. 2018;4. [Google Scholar]
- 2. Ling F, Guo D, Zhu L: Pneumatosis cystoides intestinalis: a case report and literature review. BMC Gastroenterol. déc 2019;19(1):176. 10.1186/s12876-019-1087-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Liau S-S, Cope C, MacFarlane M, et al. : A lethal case of pneumatosis intestinalis complicated by small bowel volvulus. Clin J Gastroenterol .févr 2009;2(1):22–26. 10.1007/s12328-008-0038-8 [DOI] [PubMed] [Google Scholar]
- 4. Arora R, El-Hameed AA, Harbi OA: Pneumatosis Intestinalis of Small Bowel in an Adult: A Case Report. Kuwait Med J. 2009;3. 10.1007/s005950170178 [DOI] [PubMed] [Google Scholar]
- 5. Slesser AAP, Patel PH, Das SC, et al. : A rare case of segmental small bowel pneumatosis intestinalis: A case report. Int J Surg Case Rep. 2011;2(7):185–187. 10.1016/j.ijscr.2011.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moyon FX, Molina GA, Tufiño JF, et al. : Pneumoperitoneum and Pneumatosis cystoides intestinalis, a dangerous mixture. A case report. Int J Surg Case Rep. 2020;74:222–225. 10.1016/j.ijscr.2020.07.086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rachid MG, Sadok T, Narjis Y, et al. : Occlusive syndrome in intestinal cystic pneumatosis, medical treatment or surgery. PAMJ Clin Med. 2020 [cité 11 janv 2021];2. 10.11604/pamj-cm.2020.2.65.21291 Reference Source [DOI] [Google Scholar]
- 8. Üstüner MA, Dalgıç T, Bostancı EB: Pneumatosis Cystoides Intestinalis: Three Case Reports. Indian J Surg .août 2020;82(4):690–692. 10.1007/s12262-019-02010-2 [DOI] [Google Scholar]
- 9. Fujiya T, Iwabuchi M, Sugimura M, et al. : A Case of Intussusception Associated with Pneumatosis Cystoides Intestinalis. Case Rep Gastroenterol. 12 sept 2016;10(2):494–498. 10.1159/000448876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Di Pietropaolo M, Trinci M, Giangregorio C, et al. : Pneumatosis cystoides intestinalis: case report and review of literature. Clin J Gastroenterol .févr 2020;13(1):31–36. 10.1007/s12328-019-00999-3 [DOI] [PubMed] [Google Scholar]
- 11. Rathi C, Pipaliya N, Poddar P, et al. : A Rare Case of Hypermobile Mesentery With Segmental Small Bowel Pneumatosis Cystoides Intestinalis. Intest Res. 2015;13(4):346. 10.5217/ir.2015.13.4.346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wu L-L: A systematic analysis of pneumatosis cystoids intestinalis. World J Gastroenterol. 2013;19(30):4973. 10.3748/wjg.v19.i30.4973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brighi M, Vaccari S, Lauro A, et al. : “Cystamatic” Review: Is Surgery Mandatory for Pneumatosis Cystoides Intestinalis? Dig Dis Sci .oct 2019;64(10):2769–2775. 10.1007/s10620-019-05767-4 [DOI] [PubMed] [Google Scholar]
- 14. Alves SC, Seidi M, Pires S, et al. : Pneumatosis intestinalis and volvulus: a rare association. 2.
- 15. Furihata T, Furihata M, Ishikawa K, et al. : Does massive intraabdominal free gas require surgical intervention? World J Gastroenterol. 2016;22(32):7383. 10.3748/wjg.v22.i32.7383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wiesner W, Mortelé KJ, Glickman JN, et al. : Pneumatosis Intestinalis and Portomesenteric Venous Gas in Intestinal Ischemia: Correlation of CT Findings with Severity of Ischemia and Clinical Outcome. Am J Roentgenol. déc 2001;177(6):1319–1323. 10.2214/ajr.177.6.1771319 [DOI] [PubMed] [Google Scholar]
- 17. Sooby P, Harshen R, Joarder R: An unusual triad of pneumatosis intestinalis, portal venous gas and pneumoperitoneum in an asymptomatic patient. J Surg Case Rep. 8 avr 2015;2015(4):rjv035–rjv035. 10.1093/jscr/rjv035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harrison S, Mahawar K, Brown D, et al. : Acute appendicitis presenting as small bowel obstruction: two case reports. Cases J. déc 2009;2(1):9106. 10.1186/1757-1626-2-9106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Assenza M, Ricci G, Bartolucci P, et al. : Mechanical small bowel obstruction due to an inflamed appendix wrapping around the last loop of ileum. 6. [PubMed]
- 20. Rodríguez González M, de los Á Mejías Manzano M, Sobrino López AM, et al. : Primary or idiopathic intestinal pneumatosis: a rare casual endoscopic finding. Rev Esp Enfermedades Dig. 2021 [cité 6 juin 2021]. Reference Source [DOI] [PubMed]
- 21. Takahashi K, Fujiya M, Ueno N, et al. : Endoscopic Fine-Needle Aspiration Is Useful for the Treatment of Pneumatosis Cystoides Intestinalis With Intussusception. Am J Gastroenterol. janv 2019;114(1):13–13. 10.14309/ajg.0000000000000069 [DOI] [PubMed] [Google Scholar]
- 22. Suda T, Shirota Y, Wakabayashi T: Pneumatosis Cystoides Intestinalis. Clin Gastroenterol Hepatol .mars 2019;17(4):A33–A34. 10.3748/wjg.v17.i44.4932 [DOI] [PubMed] [Google Scholar]
- 23. Lin W-C, Wang K-C: Pneumatosis Cystoides Intestinalis Secondary to Use of an α-Glucosidase Inhibitor. Radiology. mars 2019;290(3):619–619. 10.1148/radiol.2019182186 [DOI] [PubMed] [Google Scholar]
- 24. Romano-Munive AF, Barreto-Zuñiga R: Pneumatosis cystoides intestinalis. 1. 10.3748/wjg.v17.i44.4932 [DOI] [PubMed]
- 25. Fraga M, da Silva MJN, Lucas M: Idiopathic Pneumatosis Intestinalis, Radiological and Endoscopic Images. GE Port J Gastroenterol. sept 2016;23(5):270–2. 10.1016/j.jpge.2016.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tseng P-Y, Tarng D-C, Yang W-C, et al. : Benign Pneumatosis Intestinalis. Intern Med. 2014;53(14):1589–1590. [DOI] [PubMed] [Google Scholar]
- 27. Nagata S, Ueda N, Yoshida Y, et al. : Pneumatosis coli complicated with intussusception in an adult: Report of a case. Surg Today. mai 2010;40(5):460–464. 10.1007/s00595-009-4087-5 [DOI] [PubMed] [Google Scholar]