Abstract
Purpose
Long-term compaction, compression, migration, and recurrence rates of the WovenEndoBridge devices remain unknown. The purpose of this study was to detect these rates and safety profiles of the WovenEndoBridge within 7 years period.
Materials and methods
Eighty-three aneurysms of 79 patients treated with the WovenEndoBridge device were retrospectively evaluated using an occlusion scale (e.g. complete occlusion, neck remnant, and aneurysm remnant) on angiography images.
Results
The residual aneurysm was observed in 11 (13%) aneurysms. The mean and median diameters of the recurrent aneurysms were 6 and 7 mm. Most of the recurrent aneurysms were complex type and/or ruptured. Mean diameters and the neck-to-body ratios of all residual aneurysms in the preoperative imaging exams were above 4 mm and 0.6, respectively. The median values of preoperative height and neck measurements were higher in the recurrent aneurysms than in the adequate occlusion group (p = 0.006, p = 0.019, respectively). There was a statistically significant positive relationship between preoperative height/neck measurements and the mean diameters of residual aneurysms (rs = 0.32 and p = 0.003; rs = 0.28 and p = 0.011, respectively). The WovenEndoBridge compaction/compression and migration were observed in 5 (45%) and 2 (18%) of the recurrent aneurysms. In 7 (64%) of the residual aneurysms, thrombosed areas were found within the aneurysm. In the follow-up period, four aneurysms (4.8%) were retreated due to widened residual aneurysm. Other aneurysms were improved or stable within 7 years.
Discussion
Our adequate occlusion rate was 87%. Occlusion rates are less favorable than aneurysms with a long height, wide neck, or high neck-to-body ratio. Our study confirms the high safety and efficiency of the WovenEndoBridge. Compaction, compression, and/or migration of the WovenEndoBridge and the presence of intra-aneurysmal thrombosis are the main reasons for the recurrences.
Keywords: Cerebral aneurysm, intrasaccular flow diverter, Woven EndoBridge, recurrence, embolization
Introduction
Wide necked or bifurcation aneurysms make up one-third of all brain aneurysms, and the endovascular or surgical treatment of these aneurysms is technically challenging and may require the use of additional devices or interventions.1–3 Recurrence or complication rates are higher of the wide neck and/or bifurcation aneurysms.1–3 Woven EndoBridge (WEB) has provided a paradigm change in endovascular treatment of these types of aneurysms.2,4
The significant advantages of the WEB are the lack of periprocedural and long-standing antiplatelet medication necessity and the quick nature of the intervention.3,5 Some studies have shown high safety and efficacy of the WEB in the short-term period.4–7 Animal and human pilot studies revealed that intra-aneurysmal thrombus, aneurysm morphology, device migration to the aneurysmal fundus, and compression/compaction of the WEB had been associated with recurrences.5–9 However, very few studies explored aneurysm characteristics potentially associated with occlusion rates in a midterm period.2,3,10 Also, long-term compaction, compression, migration, and recurrence rates of the WEB remain unknown. 7 The purpose of this study was to detect the rates and causes of recurrences and the safety of the WEB device within 7 years period.
Materials and methods
Study population
According to our institutional guidelines, an institutional review board approval was not required for this retrospective study. Informed consent was obtained from the subjects before all examinations and interventions. The clinical and imaging data of the cases treated with the WEB (Microvention, USA) device within 7 years were reviewed.
All endovascular treatments were performed by the experienced interventional neuroradiologist (O.A). Decisions related to treatment methods were made by multidisciplinary consensus between interventional neuroradiologists and neurovascular surgeons of our hospital in an interdisciplinary neurovascular conference. Therapeutic decisions were made case by case based on morphologic and clinical considerations. Risks, benefits, alternatives, potential complications, and different therapeutic approaches for cerebral aneurysm treatment of wide neck or bifurcation aneurysms had been extensively discussed with the patients and their families before the interventions. Treatment characteristics and clinical imaging findings of the patients were retrospectively retrieved from our picture archival and communications (PACS), and radiology information (RIS) systems. As a result, 83 WEB-assisted aneurysm embolization of 79 patients were included in this study.
Inclusion criteria
Patients with a history of the WEB-assisted embolization
Presence of CT angiography (CTA), MR angiography (MRA), and/or digital subtraction angiography (DSA) images in the postoperative period
Presence of a clinical and radiological follow-up of at least 1 month.
Exclusion criteria
Patient aged < 18 years and
Patients treated with a cerebral aneurysm embolization other than WEB device.
Procedural details
All patients were under general anesthesia during therapeutic endovascular interventions. Antiplatelet therapy was not started before the embolization. A standard 6-Fr 80–90 cm long sheath and common femoral approach with triaxial access were used for all the cases. Patients were fully heparinized with a 5000 IU bolus dose of heparin. After placing the 5F–6F Sofia guiding catheter (Microvention, USA), the WEB device is introduced through an appropriate size microcatheter (Via 17-33, Microvention, USA). We used 0.014-inch microwires with a soft tip for all interventions. Appropriate WEB size was determined based on the + 1/−1 rule. In emergencies, we have selected the most appropriate WEB device according to the ranges of the medical storage room of our hospital.
1000 IU doses of heparin were given per hour until the procedure was finished. Heparin was discontinued but not reversed at the end of the intervention. The final position of the WEB and the lack of any complications were documented on biplane control angiographic runs. In patients with peri- or postprocedural thromboembolism risk (e.g. presence of malposition or partial sagging), dual antiplatelet therapy is recommended (at least 6 months). No antiplatelet therapy was administered in patients treated with only WEB or WEB + coil(s). After endovascular interventions, patients were routinely surveyed at an intensive care unit for an appropriate time. Follow-up visits and imaging exams were performed after the 6th, 12th months, and every year. DSA was only performed if there was a suspicion of a recurrence.
Evaluated parameters
Morphological details of the aneurysms (e.g. maximum width/height, neck diameter, neck-to-body ratio, side, complexity, and localization), presence of a recurrent aneurysm, and clinical data of the patients were recorded. Aneurysms have irregular, multilobular, and/or blebs were accepted as complex type (score 1) aneurysms. Others are scored as smooth or basic (score 0). Any discrepancies between the authors were resolved through discussion until consensus was reached.
If a residual aneurysm was detected, the size of the residual aneurysm was measured in three planes, and the mean of these three measurements was accepted as the residual aneurysm diameter. The presence of initial preexisting intrasaccular thrombosis was determined based on CTA, MRA, and/or DSA images. Technical success was defined as a successful and previously planned WEB deployment into the aneurysm sac without using an additional device(s) or conversion to another technique.
Statistical analyses
Statistical analysis was performed using SPSS (IBM Corp. Released 2012 IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY: IBM, USA). The suitability of the variables to normal distribution was examined by the Shapiro–Wilk test. Independent samples Mann–Whitney-U test were used for comparisons between the groups according to the normality test result. Kruskal–Wallis test was used for comparisons between the three groups. Categorical variables were given with frequency and percentage values, and the Pearson's chi-squared test and Fisher–Freeman–Halton test were used for comparisons. The relationships between the variables were examined with the Spearman correlation coefficient (rs). P < 0.05 was considered statistically significant.
Results
The demographics of the patients and characteristics of the aneurysms were given in Table 1. Bilateral MCA (mirror) aneurysms were observed in 3 patients. Via 17 (WEB5), 21 (WEB4), 27 (WEB2), and 33 (WEB2) catheters were used in 39, 11, 24, and 9 aneurysms, respectively.
Table 1.
Patient characteristics and morphological details of the aneurysms (83 aneurysms of 79 patients).
| Parameters | Values | Percentage |
|---|---|---|
| Age (mean/median) | 55/56 (range: 18–83) years | – |
| Sex (male/female) | 44/35 cases | 56/44 |
| Aneurysm side (left/right/midline) | 34/18/31 cases | 41/22/37 |
| Follow-up time (mean/median) | 17/13 (range: 1–80) months | – |
| Simple or complex type aneurysm | 12/71 aneurysms | 14/86 |
| Ruptured/non-ruptured aneurysm | 49/34 aneurysms | 59/41 |
| Presence/absence of complex shape aneurysm | 71/12 aneurysms | 86/14 |
| Localizations of the aneurysms | Numbers | % |
| Internal carotid artery terminus (ICA bifurcation) | 10 | 12 |
| Distal anterior cerebral artery (DACA) | 2 | 2 |
| Anterior communicating artery (ACOM) | 28 | 34 |
| Middle cerebral artery (MCA) | 32 | 39 |
| Basilar tip | 4 | 5 |
| Posterior communicating artery (PCOM) | 5 | 6 |
| Paraophthalmic area | 1 | 1 |
| Vertebral artery | 1 | 1 |
| Aneurysm sizes | Mean/median (range) | |
| Width | 6.9/6 (2–14) mm | – |
| Height | 6.9/6 (3–19) mm | – |
| Neck | 4.5/4 (2–9) mm | – |
| Neck-to-width ratio | 0.68/0.67 (0.36–1) | – |
Stent-assisted WEB embolization was performed in two aneurysms of two patients, and Flow-diverter (FD) assisted WEB embolization was performed in one aneurysm. Coil-assisted WEB embolization technique was used in five aneurysms. As a result, adjunctive techniques or additional devices were used in 8 (10%) aneurysms.
Two patients have recurrent aneurysms after clipping. Embolization with a single WEB device was performed for these patients. No rebleeds occurred during the postoperative period or follow-up for all the cases. One patient with a ruptured distal anterior cerebral artery (DACA) aneurysm was COVID-19 test positive. The time of groin puncture to end of the embolization with a single WEB device was 17 min in this case, uneventfully.
No adverse event was observed related to the device or procedure for all cases. The technical success rate was 86% (71/83). Neither periprocedural aneurysm rupture nor procedure-related mortality occurred. Periprocedural complications occurred in 6 (7%) of the aneurysms due to MCA territory subsegmental infarcts. In one of these cases, MCA branch occlusion was detected due to device malposition during the procedure. In this case, thrombectomy was performed and a low-profile stent was deployed to the affected segment.
Complete occlusion was observed in 63 (76%) aneurysms. Neck remnant was observed in 9 (11%) aneurysms. As a result, adequate occlusion was observed in 72 aneurysms (87%) (Figure 1). The residual aneurysm was observed in 11 (13%) aneurysms (Figure 2). The mean and median diameters of the recurrent aneurysms were 6 and 7 mm, respectively (range: 4–9 mm). Seven (64%) of the recurrent aneurysms were ruptured, and 10 (91%) of the recurrent aneurysms were of complex type. Mean diameters and the neck-to-body ratios of all residual aneurysms in the preoperative imaging exams were above 4 mm and 0.6, respectively (Table 2).
Figure 1.
Three-dimensional time of flight (a–c) digital subtraction angiogram (d and e) images showing the wide necked basilar tip aneurysm (arrows) of a 51-year-old female. A Woven EndoBridge (WEB) device was deployed to the aneurysm. Post-embolization angiographic run presenting the WEB device (arrow in (f)). First-year follow-up non-contrast CT (g–i) and CT angiogram (j–l) revealed an adequate occlusion (arrows) without complication.
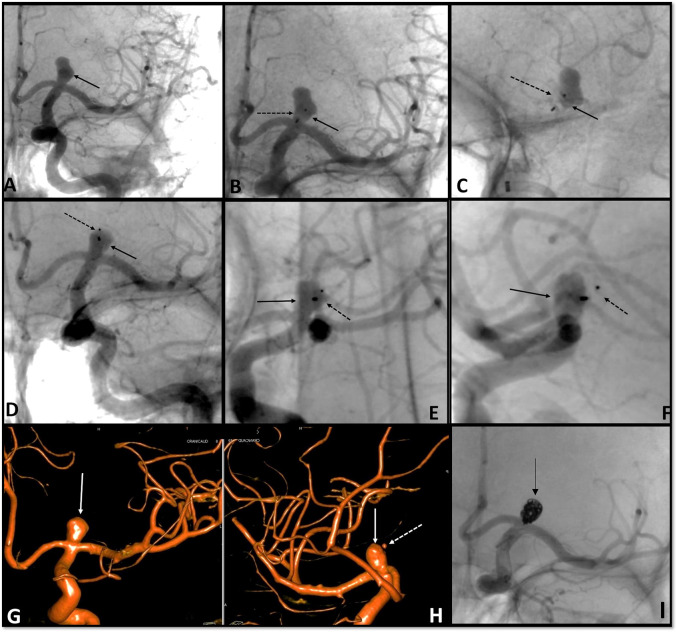
Figure 2.
Perioperative (a–c) images of a 58-year-old female with left ICA terminus aneurysm (arrows). (c) The Woven EndoBridge (WEB) (broken arrows) was placed to the neck of the aneurysm and there is a prominent contrast media stagnation on control digital subtraction angiography (DSA) images. (d–h) In the follow-up DSA images obtained 14 months after the embolization, it is seen a residual aneurysm (arrows) and migrated/compacted WEB toward to posterior part of the aneurysm dome (broken arrows). Stent-assisted coil embolization was performed for this residue aneurysm in a separate session (arrow: (i)).
Table 2.
Characteristics of recurrent aneurysms of the cases.
| Initial aneurysm sizes (mm) | Neck to body ratio | Presence of thrombosed aneurysm | Presence of SAH | Aneurysm location | Presence of complex aneurysm | Recent WEB status | Follow-up duration (months) | Residue diameter (mm) | Embolization devices | Via size |
|---|---|---|---|---|---|---|---|---|---|---|
| 10 × 12 | 0.9 | − | + | MCA | + | Compacted | 20 | 7 | W2-11-S | Via 33 |
| 6 × 6 | 0.68 | − | − | MCA | + | Compacted | 80 | 4 | W2-7-4 | Via 21 |
| 11 × 12 | 0.63 | + | + | MCA | + | Normal | 30 | 7 | W2-9-7 | Via 27 |
| 8 × 8 | 0.71 | + | + | ACOM | + | Normal | 14 | 7 | W5-7-5 + coils | Via 17 |
| 9 × 16 | 0.67 | + | + | ICA terminus | + | Normal | 16 | 9 | W2-9-7 + FD | Via 27 |
| 7 × 8 | 0.86 | − | − | ACOM | + | Compacted | 74 | 7 | W2-8-S | Via 27 |
| 9 × 11 | 0.67 | + | + | MCA | + | Normal | 21 | 7 | W2-11-9 | Via 33 |
| 5 × 7 | 0.8 | + | + | PCOM | + | Normal | 20 | 4 | W5-6-S | Via 17 |
| 13 × 19 | 0.62 | + | + | MCA | + | Normal | 16 | 5 | W2-9-6 + coils | Via 27 |
| 4 × 5 | 0.75 | − | − | ICA terminus | + | Migrated | 11 | 4 | W5-5-S | Via 17 |
| 6 × 6 | 0.67 | + | − | ICA terminus | − | Compacted/migrated | 14 | 4 | W5-7-5 | Via 17 |
ACOM: anterior communicating artery; ICA: internal carotid artery; MCA: middle cerebral artery; PCOM: posterior communicating artery; SAH: subarachnoid hemorrhage; WEB: Woven EndoBridge.
The median values of preoperative height and neck measurements were higher in the recurrent aneurysms than in the adequate occlusion group (p = 0.006, p = 0.019, respectively). The median neck size of the recurrent aneurysms was 6 (3–9) mm. This size was 4 (2–8) mm for the adequate occlusion group. There was no statistically significant relationship between neck-to-body ratio and aneurysm width in the preoperative period and recurrences (0.138 and 0.362, respectively). Recurrence or occlusion status was not associated with sex, age, laterality, presence of subarachnoid hemorrhage (SAH), additional device usage, or aneurysm location (p > 0.05).
There was a statistically significant positive relationship between preoperative height/neck measurements and the mean diameters of residual aneurysms (rs = 0.32 and p = 0.003; rs = 0.28 and p = 0.011, respectively). Preoperative height measurements of the aneurysms were higher in the recurrent aneurysms (p = 0.022). Width and height measurements were found to be higher in complex aneurysms than simple aneurysms (p = 0.040, p = 0.028).
The WEB device compaction or compression, which means a decrease in the height of the device was observed in 5 (45%) of our recurrent aneurysms. It was determined that the cause of the residual aneurysm was device migration to aneurysm fundus in 2 (18%) cases (Table 2). In seven (64%) of the residual aneurysms, thrombosed areas were found within the aneurysm. In the follow-up period, four aneurysms (4.8%) were retreated due to widened residual aneurysm (Figure 3). Other aneurysms were improved or stable within this period.
Figure 3.
A male patient with a ruptured and partially thrombosed ICA terminus aneurysm (sizes: 9 × 16 mm). It has a wide neck and complex morphology which is observed on 3D (a), lateral (b), and anteroposterior (c) digital subtraction angiography (DSA) images (arrows). (d and e) Residual aneurysm (black arrows) is seen on TOF images obtained 7 months after Woven EndoBridge (WEB)-assisted embolization due to device compaction and migration (white arrows). The aneurysm was embolized with FD. Recurrence continued TOF and DSA images obtained the first year after the FD treatment (arrows in (f–i)). (j–l) On TOF images obtained 3 years after the FD treatment, it was observed that the aneurysm was completely closed (arrows: the WEB device, j–l).
Discussion
Adequate occlusion rates of the WEB implantations were reported as 56–97% for 1-year follow-up.2–8,10–16 Our first year and latest adequate occlusion rates (87% for both) are within the range of previously published papers and higher than other therapies for wide neck or bifurcation aneurysms.2,7,8,10–16 The recurrence rate of WEB implantations in our study was low (13%). Most of our aneurysms were improved or stable in a relatively long-term period.
Hemodynamic stress of the aneurysms is also significantly reduced by the WEB with similar rates when compared to FD. 17 Post-WEB recurrences are generally do not require reintervention. 15 Our retreatment rate (4.8%) was lower than many WEB studies.3,5,7,10,13–16
It was reported that the safety of the WEB for wide necked or bifurcation aneurysms is comparable with simple coiling, and it is better than both stent/balloon-assisted coiling and flow diversion. 5 Worsening of aneurysm occlusion between the procedure and 3 years was observed in 2–13% in the literature. 7 In our study, occlusion status was worsened in four aneurysms (4.8%). Also, we did not observe any adverse events related to the WEB in the long-term period. These results confirmed the safety and efficacy of the WEB. It may be considered the first-line choice for bifurcation or wide-neck aneurysms based on our results and the literature.1–4,11–13
Most of our recurrent aneurysms had a thrombosed segment and complex morphology, large size (preprocedural diameter ≥5 mm), and rupture history. Cagnazzo et al. found that there is a relationship between complexity (irregular sac) and recurrence. 18 Achieving optimal aneurysm access, appropriate WEB size, and/or successful WEB position is difficult in large, thrombosed, or complex aneurysms, especially for emergency conditions.2,19 We found that a high neck-to-body ratio (≥0.62) is a risk factor for the development of recurrence after the WEB treatment, as a first in the literature.
A wide neck size (4–9 mm) was shown to be more prone to aneurysmal remnants and the need for retreatment.2,5,15 Blood flow is faster and hemodynamic impact is more prominent in wide neck cerebral aneurysms. 19 Besides, the presence of a wide neck or intra-aneurysmal thrombosis might promote device displacement toward the aneurysmal fundus (migration) and the WEB compaction/compression.2,18 Also, we found that aneurysm height is associated with recurrences as described in the literature.5,19 These situations may be additional reasons for the recurrences.
An oversized WEB device braces itself against the aneurysm wall and bridges the neck completely. 1 If the WEB has adequate or significant lateral compression, it can maintain its initial shape under pressure. 1 According to our results and the literature, the + 1/−1 rule may be revised as + 2/−1 for complex-shaped, wide-neck (neck-to-body ratio>0.6), thrombosed, and/or larger (≥6 mm) aneurysms to prevent a recurrence.5,18,19 However, oversizing may cause WEB protrusion into the parent artery. The + 2/−1 technique can be applied with dual antiplatelet therapy to prevent thromboembolic events. This approach should be investigated in future studies.
The recanalization mechanisms of the WEB are not yet fully understood and still debated.6,17,18 WEB device compression or compaction may be a part of the healing process related to clot formation, organization, or retraction as for coils. 8 Wide-neck and complex shape are risk factors for compression or compaction of the WEB and recurrences. 18 Cagnazzo et al. state that compression or compaction was higher in the incompletely occluded aneurysms than occluded ones (50% vs. 17.5%). 18 In our study, the WEB device compaction/compression and migration to aneurysm fundus were observed in 45% and 18% of the recurrent aneurysms. We did not find any compaction, compression, or migration in the adequate occlusion group.
We used a lower profile 0.017-inch microcatheter (Via 17, Microvention) to place the newest (fifth generation) WEB in many cases. Navigation with the Via 17 is more comfortable than other VIA microcatheters. 3 According to our experiences, Via 17 is useful for preventing vasospasm or tortuosity-related difficulties compared to other Via catheters. Unlike other Via catheters, Via 17 has two markers. This is an additional advantage for the placement of adjunctive micro-stent or coil(s) placement as we did in our patients.
A residual aneurysm was observed in 5 (38%) of 13 large aneurysms (diameter >10 mm). Parallel with our results, Fujimoto et al. state that the aneurysm sizes were inversely proportional to the success of the WEB implantation. 12 These situations may be related to the limited size and shape ranges of the WEB devices.
The periprocedural complication rate is 7% in our study. This rate is lower or equal to other studies.10,14,15 All complications observed in our study were thromboembolic impingements of M1–M2 segments of MCA. All of them except one aneurysm had complex or irregular morphology. Therefore, preventive dual antiplatelet administration may be used for complex aneurysms, especially for complex type MCA aneurysms. In these aneurysms, effective antiplatelet administration allows the potential use of adjunctive devices if necessary and may allow the reduction of thromboembolic complications.1,3 Will this new approach have an impact on treatment safety or complications? Further studies are needed before this approach can be widely recommended.
According to our own experience and the literature, antiplatelet therapy is unnecessary for simple and noncomplicated WEB-assisted embolization other than MCA and its branches. 19 Lack of antiplatelet therapy is also valuable in case of invasive procedures or surgery, and prevention of risk of rebleeding/hemorrhagic events. 11
There was no perioperative, intraoperative or long-term rupture in our study. Short- and midterm rebleeding rates were reported as 0–3.5% in the literature.5,7,12,16 Long-term rebleeding or rupture rates of recurrent aneurysms treated by WEB device are not known. The technical success rate was 86% in our study. Periprocedural complication, technical success, treatment-related morbidity, and mortality rates were in line with previously published data.3,5,8,10–12,15,16 Postprocedural subarachnoid hemorrhage was not seen in our patients through a follow-up period consistent with some studies.11,14 Our additional device usage rate was 10% for the WEB-assisted treatments in the range of the literature.3,6,16 Cagnozzo et al. described that additional device usage did not significantly influence the latest occlusion results, as observed in our study. 18
Fluoroscopy times and radiation exposures of the WEB implantations were lower than the other options for wide-necked or bifurcation aneurysms. 20 Also, the WEB reduces the contact of the endovascular team with the coronavirus-positive patients, as observed in this study.
With the progressive technical improvements, the WEB devices are increasingly used for all types of aneurysms (e.g. bifurcation/sidewall/irregular, ruptured/unruptured, narrow-necked, clipped, and/or complex large aneurysms) as an alternative for stent-assisted coiling or flow diverters.5,7,15,18 The WEB was successfully deployed in off-labeled locations, including PCOM, pericallosal aneurysms or distal locations, and paraophthalmic areas, as we did. 2
This study has several limitations. The mean follow-up time of all aneurysms was 17 months. Long-term follow-up data of 20 cases (25%) of the patients could not be reached. These cases may affect our occlusion or residue rates. Treatment and follow-up results were assessed by the authors of a single hospital and not by a core laboratory, which could bias the radiological and clinical results. 15 Operators' experience generally increased over time for the WEB, and it may have resulted in better outcomes. 15 All the procedures were performed by a single operator, this could be another limitation. To reach more definite conclusions, prospective and randomized comparative studies are required to assess the efficacy and safety of the WEB and other techniques.
Conclusion
Complications, rupture, recurrence, morbidity, and mortality rates of our WEB implantations are within the range of previously published studies. The WEB has many advantages compared to other techniques. It promises good long-term occlusion and safety for wide necked or bifurcation aneurysms. Additional device usage and retreatment necessity are rare. Recurrence rates after WEB implantation are strongly dependent on the morphology of the aneurysm, the presence of the thrombosed segment, and the device migration/compaction/compression. More comprehensive, prospective, comparative, and long-term follow-up studies are necessary to evaluate the efficacy and safety of the WEB. We think that technological and size range developments in the WEB will result in higher occlusion rates and stability.
Acknowledgements
We thank our neurosurgery/radiology teams and linguist Guven Mengu for their contributions. Also, the authors acknowledge that the analyzed patients in this paper were from a similar database used in our previous paper. However, the present study is unique in its objectives. This paper completely differs from the previous article.
Footnotes
Availability of data and material: None.
Code availability: None.
Authors’ contributions: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data: O.A. Statistical analyses: S.C. Drafting the work or revising it critically for important intellectual content: O.A., G.A.
Ethics approval: According to respective our institutional guidelines, an institutional review board approval was not required for this retrospective study.
Consent to participate: Informed consent was obtained from all subjects before all exams and interventions.
Consent for publication: Approved by all authors.
Compliance with ethical standards: All procedures performed in the studies involving human participants were following the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval was waived by the local Ethics Committee of University A given the retrospective nature of the study and all the procedures being performed were part of the routine care.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Oktay Algin https://orcid.org/0000-0002-3877-8366
Gıyas Ayberk https://orcid.org/0000-0002-9258-4001
References
- 1.Goyal N, Hoit D, DiNitto J, et al. How to WEB: a practical review of methodology for the use of the woven EndoBridge. J Neurointerv Surg 2020; 12: 512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Limbucci N, Leone G, Rosi A, et al. Endovascular treatment of unruptured intracranial aneurysms by the woven endobridge device (WEB): are there any aspects influencing aneurysm occlusion? World Neurosurg 2018; 109: e183–e193. [DOI] [PubMed] [Google Scholar]
- 3.van Rooij S, Sprengers ME, Peluso JP, et al. A systematic review and meta-analysis of woven EndoBridge single layer for treatment of intracranial aneurysms. Interv Neuroradiol 2020; 26: 455–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Algin O, Yuce G, Koc Uet al. et al. A comparison between the CS-TOF and the CTA/DSA for WEB device management. Interv Neuroradiol 2021. DOI: 10.1177/15910199211014708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Beule T, Boulanger T, Heye Set al. et al. The woven endobridge for unruptured intracranial aneurysms: results in 95 aneurysms from a single center. Interv Neuroradiol 2021; 27(5): 594–601. DOI: 10.1177/15910199211003428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alpay K, Nania A, Parkkola Ret al. et al. The outcomes of recurrent wide-necked intracranial aneurysms treated with the woven EndoBridge (WEB): a retrospective bicenter study. J Neuroradiol 2021. DOI: 10.1016/j.neurad.2021.05.008 [DOI] [PubMed] [Google Scholar]
- 7.Pierot L, Szikora I, Barreau X, et al. Aneurysm treatment with WEB in the cumulative population of two prospective, multicenter series: 3-year follow-up. J Neurointerv Surg 2021; 13: 363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen HA, Soize S, Manceau PFet al. et al. Persistent blood flow inside the woven endobridge device more than 6 months after intracranial aneurysm treatment: frequency, mechanisms, and management-a retrospective single-center study. AJNR Am J Neuroradiol 2020; 41: 1225–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ding Y, Dai D, Rouchaud A, et al. WEB Device shape changes in elastase-induced aneurysms in rabbits. AJNR Am J Neuroradiol 2021; 42: 334–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harker P, Regenhardt RW, Alotaibi NM, et al. The woven EndoBridge device for ruptured intracranial aneurysms: international multicenter experience and updated meta-analysis. Neuroradiology 2021; 63(11): 1891–1899. DOI: 10.1007/s00234-021-02727-6 [DOI] [PubMed] [Google Scholar]
- 11.Al Saiegh F, Hasan D, Mouchtouris N, et al. Treatment of acutely ruptured cerebral aneurysms with the woven endobridge device: experience post-FDA approval. Neurosurgery 2020; 87: E16–E22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujimoto M, Lylyk I, Bleise Cet al. et al. Long-term outcomes of the web device for treatment of wide-neck bifurcation aneurysms. AJNR Am J Neuroradiol 2020; 41: 1031–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arthur AS, Molyneux A, Coon AL, et al. WEB-IT Study investigators. The safety and effectiveness of the woven EndoBridge (WEB) system for the treatment of wide-necked bifurcation aneurysms: final 12–month results of the pivotal WEB intrasaccular therapy (WEB-IT) study. J Neurointerv Surg. 2019; 11: 924–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Monteiro A, Lazar AL, Waqas M, et al. Treatment of ruptured intracranial aneurysms with the woven EndoBridge device: a systematic review. J Neurointerv Surg 2021. DOI: 10.1136/Neurosurg-2021-017613 [DOI] [PubMed] [Google Scholar]
- 15.Goertz L, Liebig T, Siebert E, et al. Intrasaccular flow disruption with the woven endobridge for narrow-necked aneurysms: a safety and feasibility study. World Neurosurg 2021; 151: e278–e285. [DOI] [PubMed] [Google Scholar]
- 16.Kaya HE, Bakdık S, Keskin Fet al. et al. Endovascular treatment of intracranial aneurysms using the woven EndoBridge (WEB) device: retrospective analysis of a single-center experience. Clin Imaging 2020; 59: 25–29. [DOI] [PubMed] [Google Scholar]
- 17.Gölitz P, Luecking H, Hoelter Pet al. et al. What is the hemodynamic effect of the woven EndoBridge? An in vivo quantification using time-density curve analysis. Neuroradiology 2020; 62: 1043–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cagnazzo F, Ahmed R, Zannoni R, et al. Predicting factors of angiographic aneurysm occlusion after treatment with the woven endobridge device: a single-center experience with midterm follow-up. AJNR Am J Neuroradiol 2019; 40: 1773–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al Saiegh F, Velagapudi L, Khanna O, et al. Predictors of aneurysm occlusion following treatment with the WEB device: systematic review and case series. Neurosurg Rev 2021. DOI: 10.1007/s10143-021-01638-7 [DOI] [PubMed] [Google Scholar]
- 20.Forbrig R, Ozpeynirci Y, Grasser Met al. et al. Radiation dose and fluoroscopy time of modern endovascular treatment techniques in patients with saccular unruptured intracranial aneurysms. Eur Radiol 2020; 30: 4504–4513. [DOI] [PMC free article] [PubMed] [Google Scholar]