Abstract
The course of the vertebral artery from its subclavian artery origin up to its termination at the vertebrobasilar junction is divided into four segments (V1–V4). This segmentation, based on schemes that have evolved since the late nineteenth century, should be a consistent and reproducible anatomical concept. However, the current literature offers conflicting definitions of that scheme, not infrequently within a single article or monograph. The principal inconsistency found in modern publications concerns the termination of the V2 segment, which is either set at the C2 or C1 transverse foramen depending on the scheme considered. Consequently, the portion of the vertebral artery extending between C2 and C1—a frequent site of pathological involvement—either belongs to the V2 or V3 segment. This discrepancy can affect the validity of studies evaluating the diagnosis and management of vertebral artery disorders. A V3 segment extending from the transverse foramen of C2 to the posterior atlanto-occipital membrane and subdivided into vertical, horizontal, and oblique subsegments—a pattern suggested by Barbieri in 1867 and adopted in some modern publications—would provide a simple, precise, and reliable solution without significantly altering the widely accepted division of the vertebral artery into four segments (V1–V4).
Keywords: Vertebral artery anatomy, segmentation, pitfall
Introduction
The vertebral artery (VA) is the main collateral branch of the subclavian artery, both in size and function. It ascends towards the skull base—partly concealed within the cervical spine's transverse canal—and gives its largest tributary, the posterior-inferior cerebellar artery, after piercing the posterior atlanto-occipital membrane. It then forms the vertebrobasilar junction by joining the opposite VA.
The VA is an adaptation of the primitive intersegmental vascularization pattern, found almost intact at the thoracic and lumbar levels, to the modified morphology of the cervical spine and skull base. It consists of a series of longitudinal anastomoses connecting the proatlantal artery, which runs between the skull base and the atlas, to the first five cervical intersegmental arteries (ISA) and the subclavian artery (SCA). The course of the VA has been subjected to various segmentation patterns. Widely accepted, its modern division into four segments (V1–V4) should be a reproducible concept. It is instead equivocal as the current literature provides conflicting descriptions of that scheme, sometimes within a single work.1–5 This review considers the chronological evolution of VA segmentation schemes, discusses their historical origins, and warns of the potential clinical misconceptions that may result from an inconsistent nomenclature.
Developmental segmentation of the vertebral artery
The developmental history of the VA constitutes a natural segmentation pattern, as the adult VA combines three portions of independent embryonic origin (Figure 1A) 6 :
The proximal portion corresponds to a persistent primitive ISA, generally the sixth cervical ISA.
The intermediate portion consists of a series of longitudinal anastomotic connections established between the first five cervical ISAs.
The distal portion, derived from the proatlantal artery, forms the terminal VA up the vertebrobasilar junction.
Figure 1.
Vertebral artery (VA) segmentation schemes (The red star represents a hypothetical injury involving the vertebral artery between C1 and C2; e.g. bow Hunter's syndrome). (a) Developmental segmentation pattern overlying the lateral view of a non-subtracted VA angiogram, showing three embryologically independent portions (proximal, intermediate, and distal VA). (b) 4-segment scheme proposed by Power in 1860. 7 (c) Modern 4-segment scheme A.2,3,8–10 (d) 4-segment scheme proposed by Barbieri in 1867–1868. 11 (e) Modern 4-segment scheme B.12–16 (f) Modern 4-segment scheme C. 17 (g) VA segmentation scheme described by Krayenbühl and Yasargil in 1957. 18 (h) Modern 4-segment scheme D. 19 (i) Modern 5-segment scheme. 20
The developmental history of the VA has important anatomical implications that may be summarized as follows:
The “normal” VA arises from the SCA and enters the transverse canal via the C6 transverse foramen (TF). The persistence of any other primitive ISA results in an aberrant origin, which can be identified by its point of entry into the transverse canal (e.g. a VA formed by a persistent fifth cervical ISA enters the C5 TF).
Portions of both proatlantal arteries persist at the adult stage to form several important vascular structures, including the vertebrobasilar junction, the anterior vertebrospinal trunks (anterior radiculomedullary arteries of C1), and the posterior vertebrospinal trunks (posterior radiculomedullary arteries of C1).
The short anastomotic segments that form the intermediate portion of the VA are prone to variations, including focal duplications or segmental agenesia. 21
A note on the nomenclature of the intersegmental arteries
Some confusion persists in the modern literature concerning the naming and numbering of the segmental or intersegmental arteries. Padget settled both points in her landmark 1954 contribution to the subject. 22 Padget notably emphasized that the dorsal branches stemming from the paired primitive dorsal aortas pass, on their way to the neural tube, in between somitic elements, as demonstrated by His in 1880. 23 Because of this intersomitic distribution, the term intersegmental artery, already used by Minot in his 1892 Human Embryology, 24 is preferred to the imprecise segmental artery.
The number of cervical ISAs (six or seven) is essential in determining which branch participates in the formation of the subclavian artery. In his study on the development of the cervical spine in oxen (1886), Froriep labeled the primitive ISAs as “interprotovertebral vessels” and highlighted the role played by the artery coursing along the first cervical nerve in the formation of the “cerebral” portion of the VA (arteria vertebralis cephalica) 25 (Figure 2A):
“The most cranial of these [interprotovertebral arteries] is the one along the first cervical spinal nerve, which later persists as a portion of the vertebral artery.” [auth. transl.]
Figure 2.
Development of the distal portion of the vertebral artery (distVA) and intersomitic course of the primitive intersegmental arteries (ISA). (a) Illustration reproduced from Froriep's Zur Entwickelungsgeschichte der Wirbelsäule, insbesondere des Atlas und Epistropheus under der Occipitalregion. II. Beobachtung an Säugethierembryonen (1886), depicting the intersomitic course of the interprotovertebral arteries (i.e. the primitive ISAs). Note that the first artery (ai1) courses along the first cervical nerve (gc1 indicates the first spinal ganglion) and passes in between the anlagen of the first cervical vertebra (bc1) and last occipital vertebra (bo) (i.e. the proatlas, part of the future occipital bone). Other legends: Ao = aorta, a3 = third aortic arch, a5 = fifth aortic arch, XI = accessory nerve. (b) Illustration reproduced from Schmeidel's Die Entwicklung der Arteria vertebralis des Menschen (1933), situating the developing distVA (labeled as A. verteb. cereb.) in a 6-mm embryo. The distVA joins its contralateral homolog to form the future vertebrobasilar junction (Verbindung zwischen den beiden Aa. Vertebr.cerebr.). The paired vessels extending from that point up to the posterior division of the internal carotid artery (caudaler Endast der A. carotis int., i.e. the future posterior communicating artery) correspond to the longitudinal neural arteries, that is, the future basilar artery. The distVA is the cranial extension of the post-occipital artery (A. postoccipit.), which corresponds to the modern proatlantal artery and runs with the first cervical nerve (Arterie, die mit dem N. cerv. I zieht). The longitudinal anastomoses between the cervical intersegmental arteries, which will become the intermediate portion of the vertebral artery, are not yet established. The subclavian artery (A. subclavia) corresponds to the sixth cervical intersegmental artery. Other legends: A. carotis int. = internal carotid artery, rostraler Endast der Carotis int. = anterior division of the internal carotid artery, segm. Arterien der Occipital region (Hypogloss. Aa.) = segmental arteries of the occipital region (hypoglossal arteries).
Subsequent works by Hochstetter in rabbits (1890) 6 and Schmeidel in humans (1933) 26 confirmed Froriep's description. In addition, Hochstetter and Schmeidel distinguished the vessel associated with the first nerve from the remainder of the cervical ISAs by naming it the post-occipital artery (arteria postoccipitalis) (Figure 2B). Padget agreed that “the intersegmental artery accompanying the first cervical nerve should not be numbered in the cervical series because it does not pass between two cervical segments” and coined the modern term proatlantal artery in 1954. The distinction established between the proatlantal artery and the cervical ISAs has two important consequences for the relevant nomenclature: the numbering of the cervical ISAs and nerves is shifted by one unit (e.g. the first cervical ISA courses with the second cervical nerve, etc.) and “the artery which becomes the stem of the subclavian and vertebral arteries, therefore, is the sixth cervical intersegmental artery (with the seventh cervical nerve).” 22
Anatomical segmentation of the vertebral artery
Historical background
VA segmentation schemes rely on the definition of segments or curves, alone or in combination. Segments concern the entire length of the vessel, while curves are generally limited to the portion of the VA extending between C2 and the posterior atlanto-occipital membrane.
The origin of the segmentation concept cannot be dated precisely, as the presence of curves and segments is implicit in many early VA descriptions. A simple but now obsolete division in pretransverse (proximal), transverse (intermediate), and post-transverse (distal) portions matched the VA developmental history (Figure 1A). This review considers the presence of a numbering system (e.g. “first curve,” “second stage,” or “third segment”) as the hallmark of a segmentation scheme. Extracts from Hoffmann's Lehrbuch der Anatomie des Menschen (1878) and Rauber's revised fourth edition of the same text (1893) illustrate the progressive evolution of the segmentation concept. While both describe the transition between the pretransverse and transverse portions without using a scheme, the revised edition introduces a numbering system for the VA curves:
“[The VA] […] extends obliquely upwards and backward and enters the foramen transversarium of the sixth, sometimes of the fifth cervical vertebra. The vessel then ascends within the canal formed by the openings in the transverse processes up to the second cervical vertebra, curves backward and outwards at the opening of this vertebra, enters the analogous opening of the atlas […]” (1878) [transl. from German]
“[The VA] […] courses upwards and backward behind the anterior scalene muscle and enters the foramen transversarium of the sixth, sometimes the fifth cervical vertebra. The vessel then ascends within the canal formed by the openings in the transverse processes up to the second cervical vertebra, curves backward and laterally in the foramen transversarium of this vertebra (first curve), arches towards the foramen transversarium of the atlas (second curve) […]” (1893) [transl. from German]
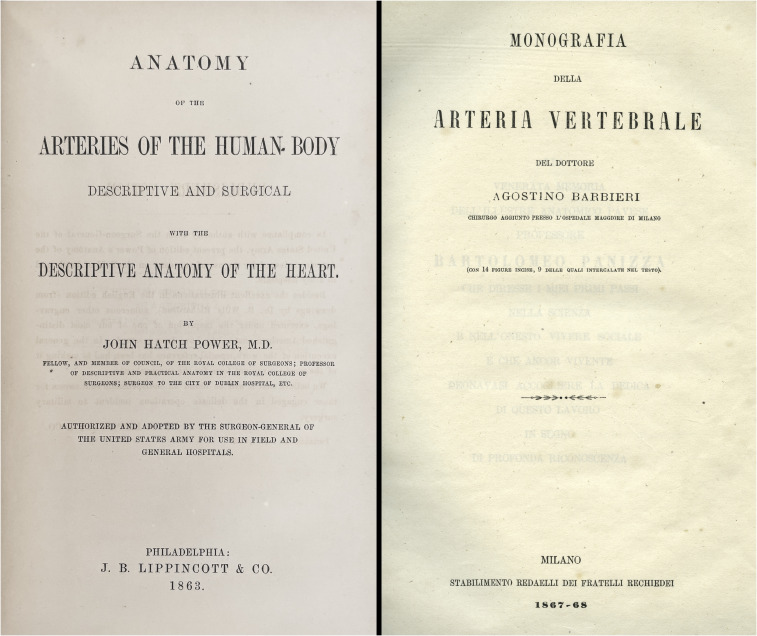
The two oldest segmentation schemes known to the author—both published in the second half of the 19th century—form the basis of all modern systems. In his Anatomy of the Arteries of the Human Body (1860) (Figure 3A), Power proposed segmentation schemes for various arteries, including the VA, which he divided into “four stages” 7 (Figure 1B):
“In the first it ascends almost vertically in the neck as high as the foramen in the transverse process of the sixth cervical vertebra: in the second it passes through the foramina of the transverse processes: in the third it passes horizontally inwards, behind the occipito-atlantoid articulation; and in the fourth it passes obliquely upwards, forwards, and inwards, on the side of the medulla oblongata.”
Figure 3.
Historical origin of the 4-segment vertebral artery segmentation schemes. (a) Title page of Power's Anatomy of the Arteries of the Human Body (1860), reproduced from the first American edition (1863), specifically designed to be used by Civil War's physicians. (b) Title page of Barbieri's Monografia della Arteria Vertebrale (1867–1868).
To the best of our knowledge, Power's segmentation scheme was only illustrated in 1957 by Henry (Figure 4A). 27 Barbieri described an alternate pattern seven years later in his Monografia della Arteria Vertebrale (1867–1868) (Figure 3B) 11 :
“In order to better describe the relationships of this artery [the VA], so important for practical views, and to enumerate its branches, represent its anastomoses, and discuss its physiology and pathology, it appears appropriate to distinguish four portions, thus following its anatomical arrangement.” [transl. from Italian]
Figure 4.
Evolution of the vertebral artery (VA) segmentation iconography (a) 4-segment pattern following Power’s scheme, reproduced from Henry's extensile exposure (1957). 27 Segments are still identified as “stages.” Henry's diagram leads to the modern 4-segment scheme A (Figure 1C). (b) Numerical segmentation scheme introduced by Fischer in 1938 (reproduced from. 28 ) (c) 4-segment pattern reproduced from Krayenbühl and Yasargil's Die Vaskulären Erkrankungen in Gebiet der Arteria Vertebralis und Arteria Basialis (1957). 18 Rather than illustrating the scheme proposed in the text, this illustration follows Barbieri's pattern, with the V3 segment extending from C2 to the dura rather than stopping at the C1 transverse foramen (see Figure 1G). To our best knowledge, this illustration introduced the V1 to V4 notation system (V1 not depicted). (d) Figure reproduced from Lazorthes's Vascularisation et Circulation Cérébrales (1961), 29 showing the portion of VA extending between C3 and the dura subdivided into five parts (v1–v5). This scheme's source is unclear, and the definition of the transition points between segments not precise; this scheme has not gained adoption (although v2-3, v4, and v5 resemble Barbieri's three curves, see Figure 1D). (e) Figure reproduced from Lang's Clinical Anatomy of the Cervical Spine (1993). 20 This diagram is the only 5-segment scheme known to the author. However, it is remarkable that an anatomist as meticulous as Lang could not avoid some confusion since another illustration of his monograph (Figure 156, p. 136) labels the intradural portion of the VA as “V4.”
Barbieri's scheme differed from Power's by setting the transition between the second and third portions of the VA at C2 rather than C1; it also refined the description of the third segment by adding “3 remarkable curves” (Figure 1D). Erich Fischer introduced an angiographic segmentation scheme for the anterior cerebral circulation in 1938; 28 his nomenclature—used nowadays in a slightly modified version—included, for example, an M1–M5 division of the middle cerebral artery (Figure 4B). Fischer did not address the VA, then beyond the reach of angiographic exploration. Krayenbühl and Yasargil proposed a new 4-segment pattern diverging from both Power's and Barbieri's in their 1957 monograph on the vertebrobasilar circulation 18 : their scheme individualized the VA between C1 and C2 as a separate segment, while the fourth segment—extending from C1 to the vertebrobasilar junction—included extra- and intradural portions (Figure 1G). Krayenbühl and Yasargil introduced the modern V1–V4 notation in the same monograph, but the illustration featuring the novel nomenclature showed a segmentation pattern matching Barbieri's scheme rather than their own (Figure 4C).
Finally, a rarely employed alternative—used, for example, by Lazorthes in 1961—divides the VA portion extending from the TF of C3 to the posterior atlanto-occipital membrane into five segments (Figure 4D). This scheme was credited to C. Miller Fisher,29,30 but our literature review could not confirm that attribution.
Modern segmentation schemes of the vertebral artery
We identified five segmentation schemes in the current literature, including four 4-segment schemes (A–D) (Figure 1C, E, F, and H) and one 5-segment scheme (Figure 1I); all preserve the original V1 segment definition (SCA to C6 TF), and most agree that the passage through the dura separates two segments (the latter point being a notable departure from Krayenbühl and Yasargil's scheme). Most modern schemes have four segments and differ by the point of transition between the second and third segments, either set at C1 or C2. To the author's best knowledge, a 5-segment scheme was only proposed once, in a diagram illustrating Lang's Clinical Anatomy of the Cervical Spine (1993), which depicted prevertebral, transverse, atlantoaxial, atlas, and subarachnoid VA portions (Figures 4E). 20
Lineages between historical and modern segmentation schemes are easily established:
The modern 4-segment scheme A (Figure 1C)2,3,8–10 derives from Power's system (Figure 1B).
The modern 4-segment scheme B (Figure 1E)12–16 derives from Barbieri's system (Figure 1D).
The modern 4-segment scheme C (Figure 1F) 17 derives from Barbieri's system, including the three curves Barbieri added to the third segment (Figure 1D).
The modern 4-segment scheme D (Figure 1H) 19 follows Krayenbühl and Yasargil's system (Figure 1G) and subdivides the post-transverse VA into “extradural or proximal” V4 and “intradural or distal” V4.
The modern 5-segment scheme (Figure 1I) 20 follows Krayenbühl and Yasargil's system (Figure 1H) but individualizes the intra- and extradural portions of the post-transverse VA as two separate segments
Brief literature survey
Table 1 lists a selection of modern contributions (from the year 2000 and later) describing or using a 4-segment pattern, including journal articles2,10,14–19 and single-authored9,20 or multi-authored3,8,12,13,31 books. The primary subject of these publications was general or surgical anatomy,3,8,13,20 surgical technique and therapy,10,12,17 neurological or vascular pathology,2,16,19 and imaging (both invasive 9 or noninvasive.14,15) The survey found examples of conflicting VA segmentation patterns across all fields and publication types. As expected, schools of thought play a role; for example, the modern 4-segment schemes B and C, derived from Barbieri and illustrated in Figures 1E and F, are predominantly used by authors linked to the Department of Neurological Surgery of the University of Florida.3,10,17
Table 1.
Modern examples of 4-segment schemes.
| Authors | PC | Year | V1 | V2 | V3 | V4 | Scheme |
|---|---|---|---|---|---|---|---|
| Campero et al. 3 | A | 2011 | SCA to C6 | C6 to C1 | C1 to DM | DM to VBJ | A |
| George and Bruneau 13 | A | 2016 | SCA to C6 | C6 to C2 | C2 to DM | DM to VBJ | B |
| Watkinson and Gleeson 8 | A | 2016 | SCA to C6 | C6 to C1 | C1 to DM | DM to VBJ | A |
| Rhoton 10 | S | 2000 | — | — | C1 to DM | — | A |
| Albuquerque and Spetzler 12 | S | 2001 | SCA to C6 | C6 to C2 | C2 to DM | — | B |
| Ulm et al. 17 | S | 2010 | SCA to C6 | C6 to C2 | C2 to DM | DM to VBJ | C |
| Kawchuk et al. 2 | NVP | 2008 | SCA to C6 | C6 to C1 or C2 | C1 or C2 to DM | DM to VBJ | A, B |
| Alterman et al. 16 | NVP | 2013 | SCA to C6 | C6 to C2 | C2 to DM | DM to VBJ | B |
| Simmonet et al. 19 | NVP | 2015 | SCA to C6 | C6 to C2 | C2 to C1 | C1 to VBJ | D |
| Buckenham and Wright 14 | IM | 2004 | SCA to C6 | C6 to C2 | C2 to DM | DM to VBJ | B |
| Pearse-Morris 9 | IM | 2007 | SCA to C6 | C6 to C1 | C1 to DM | DM to BJV | A |
| Hong et al. 15 | IM | 2008 | SCA to C6 | C6 to C2 | C2 to DM | DM to BJV | B |
Publication category (PC): A = general or surgical anatomy, S = surgical technique and therapy, NVP = neurological or vascular pathology, IM = imaging. Other abbreviations: DM = dura mater, SCA = subclavian artery, VBJ = vertebrobasilar junction, C1, C2, and C6 stand for the corresponding transverse foramina. The schemes A, B, C, and D correspond to the modern patterns shown in Figure 1.
Two schemes are listed for Kawchuk and coauthors, as their text specifies that the V3 segment “is connected to the region of the cervical spine with the greatest range of motion (C1–C2)” (scheme B), but their illustration shows the C1-C2 portion of the vertebral artery belonging to the V2 segment (scheme A).
Surveyed publications dealing with VA dissections showed striking inconsistencies, the description of segmental patterns of injuries following, in our sample, three conflicting schemes.2,16,19 For example, a 2015 article discussing extracranial VA dissections in children labeled a common injury location as the “proximal extracranial” or “extradural” V4 segment (between C1 and the posterior atlanto-occipital membrane), 19 following Krayenbühl and Yasargil's nowadays rarely used scheme.
Clinical implications
Conflicting VA segmentation patterns have important diagnostic and therapeutic implications. For example, when Sorensen described the bow hunter's syndrome in 1978, he documented a VA injury at the C1-C2 level 32 —a lesion identified as an injury to either the V2 or V3 segment depending on which modern scheme is adopted (see star in Figure 1). Dynamic VA compression also occurs at other levels, notably between C5 and C7, but C1-C2 remains its most common location; Zaidi and coauthors likely avoided a nomenclature dilemma by labeling that level “V2-V3.” 33
Assuming that the segmentation of the VA is an implicitly shared notion can also be detrimental. For example, a multicenter study looking at various characteristics of 195 VA dissections, including an analysis of their segmental distribution, used the labels “pars transversaria” for V2 and “atlas loop” for V3. 34 It is thus unclear what exactly was meant by V2 and V3 in that study and whether the participating institutions used the same segmentation pattern. Conflicting schemes not infrequently coexist in a single work: e.g., a recent article concluding that most VA dissections, regardless of etiology, involve the V3 segment offered diverging definitions of that segment in the text (C2 to dura) and the accompanying illustration (C1 to dura). 2 In extreme situations, conflicting statements may appear within a single paragraph, as in a 2011 article discussing VA blunt trauma 5 :
“The vertebral arteries are composed of four segments. […]. V2 is the foraminal segment where the artery passes through the transverse foramina from C6 to C1. V3, the extraspinal segment begins at the foramen transversarium of C2. […].”
While there may not be, as Kawchuk and colleagues noted, 2 “an absolute region of preferential dissection in the vertebral artery,” underlying mechanisms can involve specific segments, notably when they are linked to a particular anatomical feature, such as a cervical rib (pretransverse portion) or an arcuate foramen (C1). 35 VA injuries complicating underlying conditions can also show regional predilections, including neurofibromatosis type I, 36 osteophytic compression, loop formation (transverse portion), 1 or compression by a fibrous band (pretransverse portion). 12 The use of conflicting schemes renders both the characterization of these lesions and the comparison between clinical studies challenging.
The only discrepancy separating the modern 4-segment schemes A and B—the most used segmentation patterns in clinical practice (Figures 1C and E)—concerns the portion of the VA extending between C2 and C1, which belongs to V2 in one scheme and to V3 in the other. This portion has unique anatomical, physiological, and pathological characteristics that were not fully appreciated when 4-segment schemes became popular but now appear to justify its designation as a separate segment. Adopting a 5-segment division, such as the one suggested by Lang, would satisfy that requirement, but renaming the intracranial VA “V5” is unlikely to gain wide acceptance at this time. The alternative favored by the author is to follow Barbieri's scheme, including a V2–V3 transition at the TF of C2 and a subdivision of the V3 segment into three subsegments (vertical, horizontal, and oblique), as used, for example, by Ulm and coauthors 17 (Figure 1F). This option enhances the accuracy of the segmentation scheme while preserving the V1–V4 format familiar to most anatomists and clinicians. For instance, the injury characterizing Sorensen's bow hunter syndrome could be precisely identified as a lesion of the vertical portion of the V3 segment.
Conclusions
Researchers and clinicians must be mindful of discrepancies regarding the definition of VA segments in the current literature. Modern schemes principally differ in their delimitation of the V2 and V3 segments. Depending on the adopted scheme, the portion of VA running between the first and second transverse foramina belongs to one segment or the other, a divergence that can impact the validity of studies evaluating the diagnosis and management of VA pathologies. Adopting a V2–V3 transition point at the TF of C2 and subdividing the V3 segment into three subsegments would provide a simple, precise, and reproducible segmentation scheme.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Philippe Gailloud https://orcid.org/0000-0003-0768-3273
References
- 1.George B, Cornelius J. Vertebral artery: surgical anatomy. Oper Tech Neurosurg 2001; 4: 168–181. [Google Scholar]
- 2.Kawchuk GN, Jhangri GS, Hurwitz EL, et al. The relation between the spatial distribution of vertebral artery compromise and exposure to cervical manipulation. J Neurol 2008; 255: 371–377. [DOI] [PubMed] [Google Scholar]
- 3.Campero A, Rubino PA, Rhoton AR, Jr. Anatomy of the vertebral artery. In: George B, Bruneau M, Spetzler RF. (eds) Pathology and surgery around the vertebral artery. Paris; London: Springer, 2011, pp. 29–40. [Google Scholar]
- 4.Bruneau MG, B. Surgical approaches to the V3 segment of the vertebral artery. In: George B, Bruneau M, Spetzler RF. (eds) Pathology and surgery around the vertebral artery. Paris; London: Springer, 2011, pp. 330–360. [Google Scholar]
- 5.Desouza RM, Crocker MJ, Haliasos N, et al. Blunt traumatic vertebral artery injury: a clinical review. Eur Spine J 2011; 20: 1405–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hochstetter F. Uber die entwicklung der A. Vertebralis beim kaninchen, nebst bemerkungen über die entstehung des ansa vieussenii. Morphologische Jahrbuch 1890; 16: 572–586. [Google Scholar]
- 7.Power JH. Anatomy of the arteries of the human body, descriptive and surgical, with the descriptive anatomy of the heart. Dublin: Fannin and Co, 1860. [Google Scholar]
- 8.Watkinson J, Gleeson M. Chapter 29: neck. In: Standring S. (ed) Gray’s anatomy: the anatomical basis of clinical practice. Forty-first edition. New York:: Elsevier Limited, 2016, pp. 442–474. [Google Scholar]
- 9.Morris P. Practical neuroangiography. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2007, p.xi, 543 p. [Google Scholar]
- 10.Rhoton AL, Jr. The far-lateral approach and its transcondylar, supracondylar, and paracondylar extensions. Neurosurgery 2000; 47: S195–S209. [DOI] [PubMed] [Google Scholar]
- 11.Barbieri A. Monografia della arteria vertebrale. Milano: Stabilimento Redaelli dei Fratelli Rechiedei, 1867-68. [Google Scholar]
- 12.Albuquerque FC, Spetzler RF. Vertebral artery revascularization. Oper Tech Neurosurg 2001; 4: 195–201. [Google Scholar]
- 13.George B, Bruneau M. Bergman’s comprehensive encyclopedia of human anatomic variation 2016: 487–500. Hoboken, New Jersey. [Google Scholar]
- 14.Buckenham TM, Wright IA. Ultrasound of the extracranial vertebral artery. Br J Radiol 2004; 77: 15–20. [DOI] [PubMed] [Google Scholar]
- 15.Hong JT, Park DK, Lee MJ, et al. Anatomical variations of the vertebral artery segment in the lower cervical spine: analysis by three-dimensional computed tomography angiography. Spine (Phila Pa 1976) 2008; 33: 2422–2426. [DOI] [PubMed] [Google Scholar]
- 16.Alterman DM, Heidel RE, Daley BJ, et al. Contemporary outcomes of vertebral artery injury. J Vasc Surg 2013; 57: 741–746; discussion 746. [DOI] [PubMed] [Google Scholar]
- 17.Ulm AJ, Quiroga M, Russo A, et al. Normal anatomical variations of the V(3) segment of the vertebral artery: surgical implications. J Neurosurg Spine 2010; 13: 451–460. [DOI] [PubMed] [Google Scholar]
- 18.Krayenbühl H, Yasargil M. Die vaskulären erkrankungen in gebiet der arteria Vertebralis und arteria basialis. Eine anatomsiche und pathologische, klinische und neuroradiologische studie. Stuttgart: Georg Thieme Verlag, 1957. [PubMed] [Google Scholar]
- 19.Simonnet H, Deiva K, Bellesme C, et al. Extracranial vertebral artery dissection in children: natural history and management. Neuroradiology 2015; 57: 729–738. [DOI] [PubMed] [Google Scholar]
- 20.Lang J. Clinical anatomy of the cervical spine. 1st ed. Stuttgart New York: Georg Thieme Verlag, 1993. [Google Scholar]
- 21.Gailloud P, Gautam A, Caplan J. Unilateral segmental agenesis of the vertebral artery at the C2 level. Surg Radiol Anat 2020; 42: 189–192. [DOI] [PubMed] [Google Scholar]
- 22.Padget DH. Designation of the embryonic intersegmental arteries in reference to the vertebral artery and subclavian stem. Anat Rec 1954; 119: 349–356. [DOI] [PubMed] [Google Scholar]
- 23.His W. Anatomie menschlicher embryonen. II. Gestalt- und grössentwicklung bis zum schluss des 2. Monats. Leipzig: Verlag von F.C.W. Vogel, 1882. [Google Scholar]
- 24.Minot CS. Human embryology. 1st ed. New York: William Wood and Company, 1892. [Google Scholar]
- 25.Froriep A. Zur entwickelungsgeschichte der wirbelsäule, insbesondere des atlas und epistropheus under der occipitalregion. II. Beobachtung an säugethierembryonen. Archiv für Anatomie und Physiologie - Anatomiche Abtheilung 1886: 69–145. [Google Scholar]
- 26.Schmeidel G. Die entwicklung der arteria vertebralis des menschen. Morphol Jahrb 1933; 71: 315–435. [Google Scholar]
- 27.Henry AK. Extensile exposure. 2nd ed. Baltimore: The Williams and Wilkins Company, 1957. [Google Scholar]
- 28.Fischer E. Die lageabweichungen der vorderen hirnarterie im gefäßbild. Zentralblatt für Neurochirurgie 1938; 3: 300–313. [Google Scholar]
- 29.Lazorthes G. Vascularisation et circulation cérébrales. 1st ed. Paris: Masson & Cie, Éditeurs, 1961. [Google Scholar]
- 30.Francke J, Di Marino V, Pannier M, et al. Les artères vertébrales (arteria vertebralis). segments atlanto-axoidien V3 et intracrânien V4 - collatérales. Anat Clin 1980; 2: 229–242. [Google Scholar]
- 31.George B, Bruneau M, Spetzler RF. Pathology and surgery around the vertebral artery. Paris; London: Springer, 2011, p.xiv, 677 p. [Google Scholar]
- 32.Sorensen BF. Bow hunter’s stroke. Neurosurgery 1978; 2: 259–261. [DOI] [PubMed] [Google Scholar]
- 33.Zaidi HA, Albuquerque FC, Chowdhry SA, et al. Diagnosis and management of bow hunter’s syndrome: 15-year experience at barrow neurological institute. World Neurosurg 2014; 82: 733–738. [DOI] [PubMed] [Google Scholar]
- 34.Arnold M, Bousser MG, Fahrni G, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke 2006; 37: 2499–2503. [DOI] [PubMed] [Google Scholar]
- 35.Ahn J, Duran M, Syldort S, et al. Arcuate foramen: anatomy, embryology, Nomenclature, pathology, and surgical considerations. World Neurosurg 2018; 118: 197–202. [DOI] [PubMed] [Google Scholar]
- 36.Schubiger O, Yasargil MG. Extracranial vertebral aneurysm with neurofibromatosis. Neuroradiology 1978; 15: 171–173. [DOI] [PubMed] [Google Scholar]