Abstract
BACKGROUND
Telemedicine is the use of wireless communications and Web-based technologies to provide healthcare and services. The coronavirus disease 2019 (COVID-19) pandemic has posed an unprecedented challenge to healthcare providers, who have been forced to change their usual mode of service delivery and have been given an opportunity to adopt the concept of telemedicine.
OBSERVATIONS
A 40-year-old underprivileged and unseparated conjoined twin (pygopagus) had dorsal spine tuberculosis and was on a regular follow-up through telemedicine due to the ongoing COVID-19 pandemic and embarrassment they had to face in public appearances. After a few months, they contracted COVID-19 infection after which they were shifted to our tertiary care center. Several unique challenges were encountered during the 4-day course of management. Ultimately, they died and left us with questions of whether we are really prepared to tackle these challenges.
LESSONS
The general public should be made aware of such groups of patients and to encourage them to follow COVID-appropriate behavior. Vaccinations should be given on a priority basis to these subsets. A more robust approach of telemedicine consultation is required for management of patients in remote areas at the time of a pandemic. Ventilator management of these patients is still intriguing.
Keywords: COVID-19, conjoined twin, pygopagus, telemedicine, rural
ABBREVIATIONS : ARDS = acute respiratory distress syndrome, COVID-19 = corononavirus disease 2019, CT = computed tomography, ICU = intensive care unit, MRI = magnetic resonance imaging, PCV = pressure-controlled ventilation, PEEP = positive end-respiratory pressure
Telemedicine is the use of wireless communications and Web-based technologies to provide healthcare and services. It can be used as real-time video consultations and to transfer and analyze investigations such as radiographs, computed tomography (CT), magnetic resonance imaging (MRI), and blood and pathology reports from a remote area.1 Telemedicine has become more accessible as mobile phones and the Internet become more and more widely available.2 In the current era of the coronavirus disease 2019 (COVID-19) pandemic, mandatory social distancing has forced the suspension of outpatient physical visits and the role of telemedicine has come to light to provide continuum of care, especially in chronic diseases.2 This pandemic has in turn posed an unprecedented challenge to healthcare providers, who have been forced to change their usual mode of service delivery in order to transform and emphasis this potential toward advancement. Healthcare has transitioned from hospitals to patient’s homes as a result of this driving force, with reinforcing of home care and the execution of telemedicine as a tool in combating this pandemic.3 This article presents a case to emphasize the use of telemedicine to overcome social and economic barrier in addition to confronting this pandemic, so that medical assistance can reach rural areas and rare diseases can be kept under surveillance.
Illustrative Case
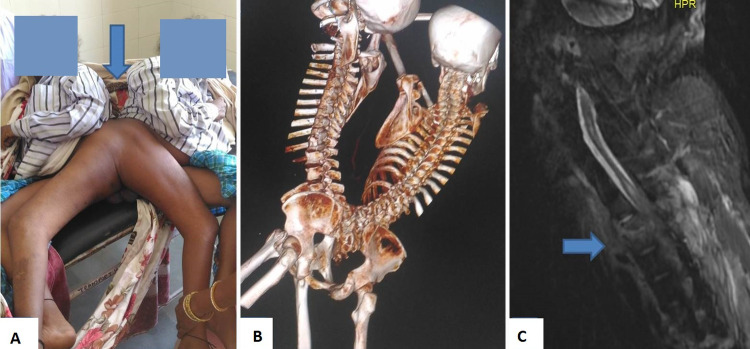
A 40-year-old underprivileged conjoined twin (patient A and patient B; pygopagus) presented to local hospital (200 km distant from our center, which is a tertiary healthcare facility) with high-grade fever (102°F), worsening dyspnea, cough, and severe fatigue for the past 3 days. The patients’ primary treatment was delayed due to transportation difficulties during the lockdown, as well as shame and reluctance on the part of family members to accompany them. The patients were managed by telemedicine video call from our center. As they presented primarily with respiratory symptoms at the time of the second wave of the COVID-19 pandemic, a presumptive diagnosis of COVID-19 infection was made. Nasopharyngeal swabs of both the patients were sent for testing of severe acute respiratory syndrome coronavirus 2 (SARS CoV-2). Both had positive reports with cycle threshold values of 13 and 12, respectively. The conjoined twins (patient A) were already receiving treatment from the neurosurgery outpatient department of our center for dorsal spine tuberculosis with paraparesis for the past year. Patient A was on antitubercular medications for past year. He had been provided with custom-fitted kyphotic brace made from a cast on his cervico-dorsal spine. They were kept on a regular follow-up through telemedicine due to ongoing COVID-19 pandemic; additionally, they were embarrassed to travel large distances for medical appointments. They also used to avoid crowded places since everyone would look at them as if they were aliens. Therefore, video consultations were provided, and routine liver function test were shared on our WhatsApp group. They did not have any other significant medical histories. However, they had a very poor hygiene due to their low socioeconomic status (Fig. 1A–C).
FIG. 1.
A: Clinical photograph of adult pygopagus twins showing conjoined lower back areas. B: CT scan of whole spine showing conjoined sacral area. C: Contrast-enhanced MR image of cervicodorsal spine showing tuberculous infection of lower cervical spine.
After discussion with the treating team at the local hospital, it was decided to shift them to our tertiary care health center. On arrival, the patients were immediately shifted to the intensive care unit (ICU) on two combined beds. They were connected to high flow nasal cannula (60 L/min) and were maintaining an oxygen saturation of 80–84% that was not adequate. Arterial blood gas analysis was done, and it was observed that PaO2/FiO2 ratio of both patients were between 70 and 80. They had metabolic acidosis with high lactate and low bicarbonate (Table 1). As they were not maintaining adequate oxygen saturation and had very high respiratory rate along with worsening of ventilatory parameters, they were intubated and taken for mechanical ventilation. Intubation was done for each of them in lateral position. Two separate mechanical ventilators (Hamilton Medical) were kept and volume-controlled ventilation mode with FiO2 80–90% and positive end-respiratory pressure (PEEP) 6 to target a saturation of 94% was initiated. Deep sedation targeting Richmond Agitation Sedation Scale of −4 was initiated using titrated doses of fentanyl at the rate of 25–150 μg/hour and midazolam infusion at the rate of 1–3 mg/hour. But as persistent asynchrony was present with desaturation, muscle relaxant infusion with vecuronium 2 mg/hour was initiated. The airway tubing and intravenous lines of each patient were color coded to avoid confusion and drug errors. We could not place a central neck line as it was quite difficult to insert due to their position. Instead, a peripherally inserted central line was placed. To confirm absence of cross-circulation between them via the sacral venous plexus, atropine was given to patient A, who developed tachycardia but patient B had a normal pulse rate ensuring absence of any cross-circulation.4 After confirmation of absence of any cross-circulation, anti-COVID-19 medications were started as per their individual estimated body weight.
TABLE 1.
Clinical and laboratory parameters on the day of ICU admission
| Symptoms & Parameters | Patient A | Patient B |
|---|---|---|
| RT-PCR on COVID-19 swab test, CT value |
13 |
12 |
| Temperature, °F |
102 |
102.6 |
| Fatigue |
+ |
+ |
| Dyspnea |
+ |
+ |
| Cough |
+ |
+ |
| Heart rate, per min |
110 |
118 |
| Blood pressure, mm Hg |
140/80 |
144/90 |
| RR, per min |
32–35 |
30–35 |
| SpO2 (%) w/ O2 15 L/min |
75 |
72 |
| ABG (w/ O2 15 L/min) |
|
|
| pH |
7.053 |
6.8 |
| pCO2 |
86.2 |
98.7 |
| pO2 |
52 |
49.5 |
| Hb |
11.5 |
12.4 |
| HCO3 |
18.6 |
19.3 |
| Na |
138.7 |
139.5 |
| K |
4.5 |
5.5 |
| Ca |
0.36 |
1.21 |
| Mg |
0.36 |
0.46 |
| Lac |
4.4 |
7.6 |
| P/F ratio |
65 |
61.8 |
| ECG |
Normal sinus rhythm |
Normal sinus rhythm |
| Hemoglobin, g/dL (ref 13–17) |
12.0 |
11.6 |
| Total leukocyte count, cells/mm3 (neutrophils/lymphocytes) (ref N −4–10 × 103 cells/μL) |
19,850 (93.75/4.1) |
22,400 (94/3.7) |
| Platelet count (103 cells/mm3) (ref N −150–450 × 103/μL) |
173 |
135 |
| Prothrombin time/INR (ref 11–16 sec/0.8–1) |
16.8/1.26 |
15.05/1.12 |
| Plasma D-dimer, μg/mL (ref < 0.2) |
1.4 |
1.7 |
| CPK-MB, U/L (ref 5–25) |
12 |
11 |
| Troponin-I, ng/mL (ref 0.1–0.2) |
0.01 |
0.02 |
| Procalcitonin, ng/dL (ref < 0.500) |
0.938 |
0.792 |
| C-reactive protein, mg/L (ref 0–5) |
148 |
200 |
| Lactate dehydrogenase, U/L (ref 230–460) |
448 |
752 |
| Interleukin-6, pg/mL (ref < 6.6) |
50.2 |
61.1 |
| Serum ferritin, μg/L | 750 | 867 |
ABG = arterial blood gas; CPK-MB = creatine phosphokinase-MB; CT = cycle threshold; ECG = electrocardiograph; INR = international normalized ratio; P/F ratio = partial pressure of O2/fraction of inspired oxygen given; ref = reference range; RR = respiratory rate; RT-PCR = reverse transcription-polymerase chain reaction; SpO2 = saturation of oxygen.
Bedside chest radiograph was obtained, which showed multiple infiltrates, linear and ground glass opacities in both the lungs with consolidation in right lung of patient A. Patient B had consolidation in bilateral lung fields, suggestive of severe acute respiratory distress syndrome (ARDS; Fig. 2A and B). His biochemical parameters were suggestive of cytokine storm. There was significant leukocytosis with neutrophilia. His renal function and serum electrolytes were normal. C-reactive protein and ferritin was highly elevated suggestive of inflammatory cycle. Procalcitonin and D-dimer were markedly raised suggesting ongoing septicemia and thrombosis. However, liver function and lipid profile were normal. Lactate dehydrogenase and interleukin-6 were significantly elevated in both the patients suggestive of severe COVID-19 infection. Cardiac profile, myocardial creatinine phosphokinase-MB, and troponin-I were normal. Electrocardiogram showed normal sinus rhythm. Echocardiogram did not show any valvular malfunction or defect.
FIG. 2.
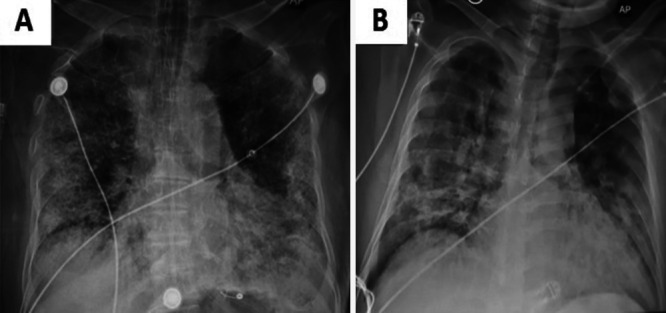
Chest radiographs (A and B) of patients A and B showing infiltrates, consolidation, and linear thickenings.
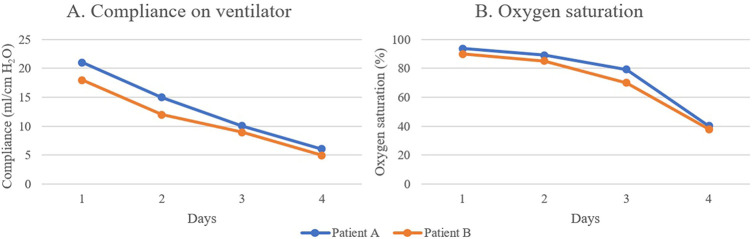
Injection of methylprednisolone (pulse dose) 500 mg once per day was given to both of them separately for 3 consecutive days. Low molecular weight heparin was also started to both patients at a dose of 60 mg twice per day along with intravenous injections of piperacillin and tazobactam (4.5 g) three times daily. An injection of tocilizumab was also given to both of them. For next 3 days, both of them were kept on maximum ventilator support (FiO2%, 100%; pressure-controlled ventilation [PCV] mode, Pi-30; PEEP, 18 cmH2O). We changed the mode to pressure control mode to prevent any barotrauma arising out of increasing airway pressures. During this period, the compliance gradually decreased with increasing plateau pressure (around 40–50) (Fig. 3A). However, despite providing ventilatory support their oxygen saturation was not adequate (SPO2, 85%). However due to conjoint sacroiliac junction, they would always maintain obliquity in their posture (lateral position). It was nearly impossible to provide them with ventilation while in the prone position despite having moderate to severe ARDS. Gradually their saturation level dropped down from 85% to 30–40% in next 3 days (Fig. 3B) with 100% FiO2 and PCV mode, Pi 38, and 18 PEEP and unfortunately they suffered cardiac arrest. Patient B died on day 3 of admission and patient A died on day 4 of admission. The hemodynamic parameters were stable until the last day of treatment before patient A died.
FIG. 3.
Compliance and oxygen saturation of patient A and B on mechanical ventilator from day 1 to day 4.
Discussion
Since 2003, there have been a total of five pandemic outbreaks: SARS (2003), swine flu (2009), Ebola (2014), Zika (2015), and the most recent, COVID-19.1 Every new pandemic has brought with it a high infection rate and a significant surge in death toll when compared to the preceding pandemic. This has revolutionized the healthcare delivery system and given an opportunity to adopt telemedicine. Telemedicine is a rapidly evolving service that enables faster diagnosis of health-related issues, lower costs for both healthcare services and patients, and protection from community infection risks.1 Telemedicine can also aid in the evaluation and monitoring of patients in remote and underserved areas.5 Telemedicine allows patients to stay in the comfort of their own care setting, but the main limitation is an inability to perform physical examinations.6 Nevertheless, the slow growth of this type of care has been attributed to constrained administrative regulations, reluctance to adopt new system, and a lack of strong legislative framework.3 Our article addresses how a rare unseparated adult conjoined twin was first managed using telemedicine due to the existing social barrier, which also resulted in a reduction in their medical expenses. However, when they required rapid transfer to a tertiary care institution as a result of a COVID-19 infection, they were sent without hesitation. There were several challenges in their management. First, it was difficult to intubate the patients because of not being able to attain the ideal position. Second, these patients are known to have restrictive lung disorder of extrathoracic origin given the kyphotic disorder they had because of their stance and posture. Hence they developed respiratory acidosis after admission because of decreased thoracic compliance. Third, the prone position, which is known to be useful in improving the ventilation perfusion mismatch and drainage of secretions, could not be achieved.7 Other than these issues, it was also difficult to place central lines. There were certain logistic issues as well such as arranging ICU beds and conduction of chest radiography. To the best of our knowledge, this is the first case of longest surviving adult pygopagus twins who died due to COVID-19–related complications.
Observations
Telemedicine has been around for a long period of time, but modern technology has made it much more attainable than ever before, and COVID-19 has rendered it more useful than it has ever been. Barriers to access, on the other hand, continue to persist, and are particularly noticeable in remote and technologically underdeveloped populations. The governments of various countries, as well as regulatory authorities, should promote this innovative technique of consultation. However, never hesitate to call patients into outpatient departments for physical examination.
Lessons
It is rightly said that prevention is better than cure. Given the extreme difficulty in management of conjoined twins along with risk to two lives, it is even truer. The general public should be made aware of such groups of patients and to encourage them to follow COVID-19 appropriate behavior. Vaccination should be given on priority basis to these subsets. A more robust approach of telemedicine consultation is required for management of patients in remote areas at the time of pandemic. Intubation was also a challenge in our case. There must be difficult airway cart at hand before intubation. Ultrasound-guided central line placement should be the norm. Prone positioning is difficult in such patients. An alternative to this should be turning both patients in toto around. But in practice this is difficult and requires a lot of manpower. Ventilator management of these patients is still intriguing. We failed to maintain oxygen saturation with volume control mode and a high airway pressure. We changed the mode to pressure control mode targeting improved oxygen saturation. However, it was still very challenging to ventilate.
Acknowledgments
We acknowledge all our professors and consultants in the Department of Neurosurgery for the guidance and assistance.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Singh. Acquisition of data: all authors. Analysis and interpretation of data: all authors. Drafting the article: all authors. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Singh. Statistical analysis: all authors. Study supervision: Singh.
References
- 1. Gillman-Wells CC, Sankar TK, Vadodaria S. COVID-19 reducing the risks: telemedicine is the new norm for surgical consultations and communications. Aesthetic Plast Surg. 2021;45(1):343–348. doi: 10.1007/s00266-020-01907-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Goyal JP, Kumar P. Telemedicine during the COVID-19 Pandemic: moving from physical to virtual outpatient care. Indian J Pediatr. 2021;88(10):959–960. doi: 10.1007/s12098-021-03924-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Community Health. 2020;11:2150132720980612. doi: 10.1177/2150132720980612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kaniyil S, Pavithran P, Mubarak KK, Mohamed T. Anaesthetic challenges in conjoined twins’ separation surgery. Indian J Anaesth. 2016;60(11):852–855. doi: 10.4103/0019-5049.193685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sclafani AP, Shomorony A, Stewart MG, Grunstein E, Overdevest JB. Telemedicine lessons learned during the COVID-19 pandemic: The augmented outpatient otolaryngology teleconsultation. Am J Otolaryngol. 2021;42(4):102960. doi: 10.1016/j.amjoto.2021.102960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fusaro MV, Becker C, Pandya S, et al. International teleconsultation on conjoined twins leading to a successful separation: a case report. J Telemed Telecare. 2018;24(7):482–484. doi: 10.1177/1357633X17715377. [DOI] [PubMed] [Google Scholar]
- 7. McNicholas B, Cosgrave D, Giacomini C, Brennan A, Laffey JG. Prone positioning in COVID-19 acute respiratory failure: just do it? Br J Anaesth. 2020;125(4):440–443. doi: 10.1016/j.bja.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]