Summary
Background
Renin-angiotensin-system inhibitors (RASi), that include angiotensin converting enzyme inhibitors (ACEis) and angiotensin receptor blockers (ARBs) reduce proteinuria, delay chronic kidney disease (CKD) progression, protect against cardiovascular events and heart failure hospitalizations. We examined the associations of discontinuation of ACEi/ARBs with risk of clinical outcomes in Chinese patients with type 2 diabetes (T2D) and advanced-CKD (estimated-glomerular filtration rate [eGFR] <30 ml/min/1.73 m2).
Methods
We conducted a prospective, population-based cohort study including 10,400 patients with T2D in Hong Kong stratified by continuation of ACEi/ARBs within 6 months after reaching eGFR <30 ml/min/1.73 m2 from January 01, 2002 to December 31, 2018 and observed until December 31, 2019. The primary outcomes were death, major-adverse cardiovascular events (MACE), heart failure, end-stage kidney disease (ESKD), and all-cause mortality. Cox-model with time-dependent exposure and covariates was used to estimate the hazard ratio (HR) of outcomes in a propensity-score overlap-weighted cohort. The risk of occurrence of hyperkalemia (plasma potassium >5.5 mmol/L) in discontinued-ACEi/ARBs versus continued-ACEi/ARBs users was assessed in a register-based cohort.
Findings
In the population-based cohort of 10,400 ACEi/ARBs users with new-onset eGFR<30 ml/min/1.73 m2, 1766 (17.0%) discontinued ACEi/ARBs and 8634 (83.0%) persisted with treatment. During a median follow-up of 3.6 (interquartile range, IQR: 2.11–5.8) years (41,623 person-years), 13.5%, 12.9%, and 27.6% had incident MACE, heart failure and ESKD respectively, and 35.8% died. Discontinued-ACEi/ARBs use was associated with higher risk of MACE (HR = 1.27, 95% CI: 1.08–1.49), heart failure (HR = 1.85, 95% CI: 1.53–2.25) and ESKD (HR = 1.30, 95% CI: 1.17–1.43), and neutral risk of all-cause mortality (HR = 0.93, 95% CI: 0.86–1.01) compared to counterparts with continued use. In the register-based cohort (583 discontinued-ACEi/ARBs users and 3817 continued-ACEi/ARBs users), discontinued-ACEi/ARBs had neutral risk of hyperkalemia (HR = 0.95, 95% CI: 0.84–1.08).
Interpretation
Discontinuation of ACEi/ARBs was associated with increased risk of cardiovascular-renal events supporting their continued use in patients with T2D and advanced-CKD.
Funding
CUHK Impact Research Fellowship Scheme.
Keywords: Angiotensin-converting enzyme inhibitors, Angiotensin receptor antagonists, Cardiovascular disease, Mortality, Therapeutics, Diabetes, Chronic kidney disease
Research in context.
Evidence before this study
We searched PubMed with the terms “diabetes”, “chronic kidney disease (CKD)”, “angiotensin converting enzyme inhibitors (RASi)”, “angiotensin receptor blockers (ACEi)”, “angiotensin receptor blockers (ARBs)”, “hyperkalemia”, “death”, “mortality”, “cardiovascular disease”, “major adverse cardiovascular events (MACE)”, “heart failure”, and “end stage kidney disease (ESKD) or “end stage renal disease (ESRD)” for original articles and reviews published up to June 30, 2022. Most studies on the associations between RASi (ACEi/ARBs) use and risk of clinical outcomes including CVD, MACE, heart failure and ESKD were focused on people with hypertension. These studies have reported a reduction in proteinuria, delay CKD progression, protect against cardiovascular events and heart failure hospitalizations. Two studies also suggest that RASi therapy in people with declining kidney function is associated with cardiovascular benefits without excessive harm of ESKD. However, the associations between continued use of ACEi/ARBs in patients with type 2 diabetes and advanced-CKD remains controversial.
Added value of this study
In this cohort study that included 10,400 patients with type 2 diabetes and advanced-CKD, discontinued-RASi use was associated with higher risk of MACE, heart failure and ESKD, and neutral risk of all-cause mortality, compared with continued-RASi use.
Implications of all the available evidence
In this real-world study, permanent or transient discontinuation of RASi in patients with T2D and advanced-CKD was associated with increased risk of MACE, heart failure and ESKD. In accordance with international recommendations, anticipatory or corrective actions should be taken to ensure continuation of RASi for organ protection with more frequent monitoring of eGFR including the use of newer potassium binding agents. Our data support continuing use of RASi in patients with eGFR <30 ml/min/1.73 m2 for cardiovascular-renal protection.
Introduction
Renin-angiotensin-system inhibitors (RASi), that include angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARBs), reduce proteinuria, delay chronic kidney disease (CKD) progression, protect against cardiovascular-events and heart failure hospitalisations.1, 2, 3 While use of ACEi/ARBs in early CKD is widely accepted, the risk-benefits of RASi continuation in advanced-CKD has been a subject of debate. In real-world practice, 15–30% of patients with CKD had ACEi/ARBs discontinued upon reaching estimated-glomerular filtration rate (eGFR) < 30/min/1.73 m2, often due to a combination of dose-dependent hyperkalemia and acute eGFR decline.4,5 The incidence of hyperkalemia in CKD stages G4-G5 was estimated at 30%6 which might be more common in patients with diabetes who are prone to hyporeninemic hypoaldosteronism.7 Although post-hoc analyses of randomized-controlled-trials (RCT) suggested equal or greater protection of RASi against end-stage kidney disease (ESKD) in the lower eGFR range,8 there was conflicting evidence from observational studies with some suggesting that discontinuation of ACEi/ARBs might reduce risk of ESKD.4,5,9
In retrospective cohort studies in USA and Sweden, discontinuation of RASi below eGFR <30 ml/min/1.73 m2 in patients with or without diabetes was associated with higher risk of all-cause mortality and cardiovascular-events, but neutral or lower risk of kidney replacement therapy.4,5 Subgroup analyses showed no suggestions of heterogeneity by diabetes status. The Kidney Disease Improving Global Outcomes (KDIGO) 2020 diabetes in CKD guidelines recommended continuation of ACEi/ARBs unless serum creatinine level increase above 30% within 4 weeks of initiation, and discontinuation only if hyperkalemia is refractory to medical treatment or dose reduction.10
Due to clinical equipoise, there is a RCT evaluating the risk-benefit ratio of discontinuation of RASi in patients with eGFR <30 ml/min/1.73 m2.11 In this territory-wide population-based cohort using target trial emulation, we investigated the association of RASi discontinuation at onset of eGFR <30 ml/min/1.73 m2 with the risk of all-cause mortality, major-adverse cardiovascular-events (MACE), heart failure and ESKD among Chinese patients with type 2 diabetes (T2D). In a complementary register-based cohort, we compared the risk of hyperkalemia between continued-RASi and discontinued-RASi users among patients with T2D and eGFR<30 ml/min/1.73 m2.
Methods
Data sources
We conducted a prospective cohort study among Chinese patients with T2D with comprehensive baseline data captured in the module of the Risk-Assessment-and-Management-Programme-for-Diabetes-Mellitus (RAMP-DM) in the territory-wide Hong Kong-Diabetes-Surveillance-Database (HKDSD).12, 13, 14 The study was reported according to the Strengthening-the-Reporting-of-Observational-Studies-in-Epidemiology (STROBE) guidelines. This study was approved by the Joint-NTEC-CUHK Clinical Research Ethics Committee.
Hong Kong has a population of 7.5 million people, mainly of Chinese descent with universal health coverage through care provision by the government-funded Hospital Authority (HA). The HKDSD (2000–2019) was captured from the territory-wide HA electronic-medical-record (EMR) system for research purposes.13 Due to the highly subsidized nature of HA services, over 90% of patients with diabetes were captured in the HA EMR system. The HKDSD provided comprehensive anonymised and de-identified data, and informed consent was not required. The HKDSD includes all people who have ever had a measurement of either fasting or random plasma glucose, fasting and 2-h plasma glucose during 75 g oral glucose tolerance test and/or glycated haemoglobin (HbA1c) in the EMR system since 2000. The HKDSD consists of a cohort of people with normal blood glucose levels, people with prediabetes, women with gestational diabetes, people with diabetes and a sub-group of people with diabetes who underwent structured risk assessment with data captured in the RAMP-DM module. Between 2000 and 2019, the HKDSD included 964,950 patients with diabetes diagnosed by physicians, medication use and/or laboratory values.15 A cohort of 581,811 patients with diabetes was curated in the RAMP-DM module. As part of a quality improvement program, all patients with diabetes can be referred by their doctors to undergo periodic structured assessments including eye, feet, blood and urine examination in hospital-based diabetes centre and community-based clinics guided by a uniform template in the RAMP-DM module. Details of the HKDSD and the RAMP-DM profiles was described elsewhere.13
Study design and patients
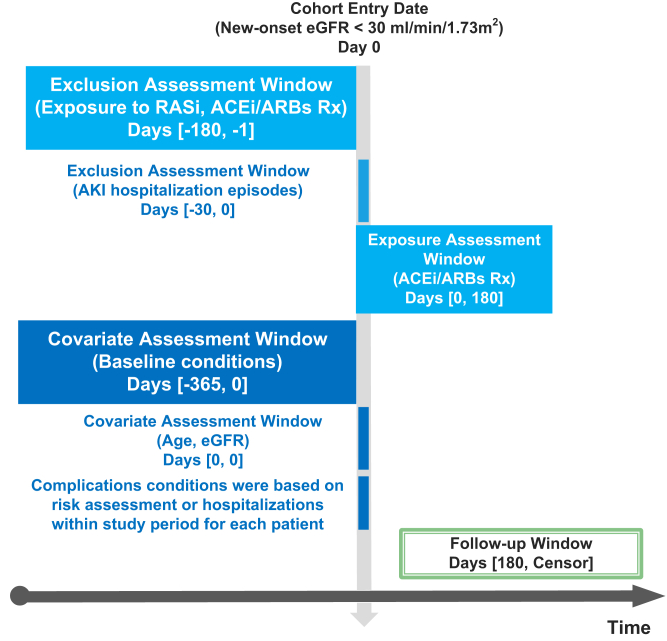
In this real-world study, we emulated a pragmatic clinical trial comparing the effects of stopping versus continuing RASi for 6 months upon reaching eGFR <30 mL/min/1.73 m2 on clinical outcomes in T2D patients with advanced chronic kidney disease. Further details are described in Supplementary Methods including the protocol of the pragmatic clinical trial, bias considerations and statistical analysis strategies.16 Fig. 1 shows the study design and time frame definitions.17 The index date was defined as the first measurement of eGFR reaching <30 ml/min/1.73 m2 after excluding values measured during a hospitalization episode due to acute-kidney-injury (AKI) defined by International Classification of Diseases, 9th-Revision (ICD-9) codes of 584.10 Considering the doctors seldom write a prescription that provides medications for a period of greater than 6 months in the HA EMR system, we adopted the landmark design, with landmark time at 6 months after the index date to classify patients and avoid the immortal time bias. We compared the strategies of continuation of RASi use within first 6 months after eGFR reaching <30 ml/min/1.73 m2 (index date) versus discontinued-RASi use, that was defined as the absence of dispensation of RASi within first 6 months after reaching eGFR <30 ml/min/1.73 m2.
Fig. 1.
Study design and time frame definitions. Rx = prescription. Censored at the earliest date of outcomes of interest or censor date (31 December 2019). Abbreviations: RASi, renin angiotensin system inhibitor; ACEi, angiotensin converting enzyme inhibitors; ARBs, angiotensin receptor blockers; eGFR, estimated glomerular filtration rate; AKI, acute kidney injury.
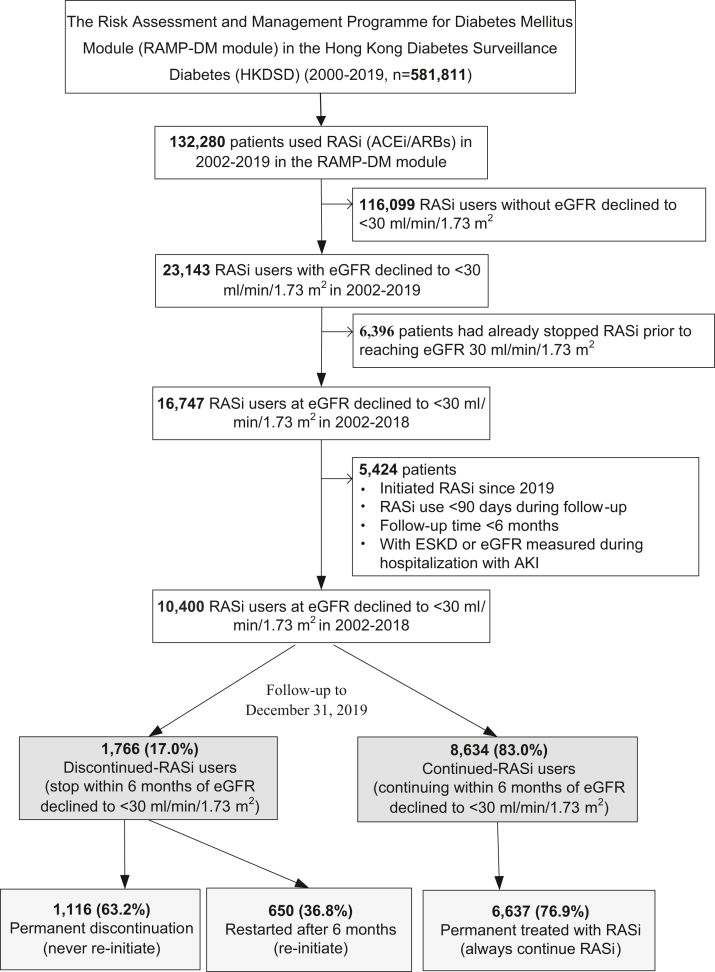
We used a 1-year period before the index date as the baseline period for definition of baseline covariates. The follow-up period started at 6 months after the index date and ended at the earliest date of outcomes of interest or censor date (December 31, 2019). We excluded patients enrolled in 2000–2001 to avoid bias from incomplete case records in the first two years of establishment of the HA EMR system, and identified 132, 280 patients who were initiated on RASi (ACEi/ARBs) in the RAMP-DM module in 2002–2019.15 We excluded patients with eGFR ≥30 ml/min/1.73 m2 (n = 116,099) throughout the observation period and those who had already stopped RASi prior to reaching eGFR <30 ml/min/1.73 m2 (n = 6396). We also excluded those who were initiated on RASi in 2019, with RASi exposure <90 days during the observation period and follow-up <6 months. This yielded 10,400 patients with T2D in the main analysis (Fig. 2). In further subgroups analyses, we compared the effects of those who subsequently re-initiated RASi after initial discontinuation in the first 6 months of the index date (stop-restart RASi) and those who permanently discontinued-RASi (stopping within 6 months and never re-initiate).
Fig. 2.
Flowchart of selection patient with type 2 diabetes.Abbreviations: RASi, renin angiotensin system inhibitor; MACE, major adverse cardiovascular events; ESKD, end-stage kidney disease; eGFR, estimated glomerular filtration rate; AKI, acute kidney injury.
Outcomes definition
We used the principal discharge diagnosis in ICD-9 and death codes (ICD-10) to define the primary outcomes of ESKD, MACE, heart failure, and all-cause and cause-specific mortality. MACE outcome was defined as the first occurrence of nonfatal myocardial infarction (ICD-9 code: 410), non-fatal stroke (ICD-9 code: 430, 431, 434 and 436), and cardiovascular (CV) death (Table S1).18 ESKD included dialysis or kidney-replacement therapy or eGFR<15 mL/min/1.73 m2 on at least two occasions separated by ≥ 90 days. We excluded eGFR values measured within the same month of hospitalization episodes due to AKI hospitalizations (ICD-9 code: 584) in the definition of ESKD. We calculated eGFR from plasma creatinine values using the CKD-epidemiology (CKD-EPI) Equation.19
In Hong Kong, all hospital admissions, outpatient clinic records, and radiological images in the public health system have been recorded in the HA Clinical Data Analysis and Reporting System (CDARS) since 1996. We reviewed the original clinical records in the CDARS system among a sample of patients (n = 50) to determine the validity of the recorded diagnoses. Through the clinical data analysis and reporting system, a clinician (E.C.) reviewed the records, including clinical notes, electrocardiograms, computed tomograms, and echocardiography. Among 50 cases of heart failure, 38 cases were confirmed by echocardiography in the CDARS system. The overall positive predictive value (38/50) was 76.0% (95% confidence interval [CI]: 62.5%–86.4%). For specific CV events, the previously reported positive predictive value in the same HA system was 85.4% (95% CI: 78.8%–90.6%) for myocardial infarction and 91.1% (95% CI: 83.2%–96.1%) for stroke.20
RASi and other medications assessment
The HA-EMR system included individual-level longitudinal dispensing data of medications including name, dose, frequency, duration (days), start and end dates in 2000–2019. All medications were coded according to the Anatomical-Therapeutic-Chemical (ATC) classification system,14 including RASi, metformin, insulin and other glucose-lowering-drugs (GLDs) (sulfonylureas, thiazolidinediones, dipeptidyl-peptidase-4-inhibitors [DPP-4is], alpha-glucosidase-inhibitors [AGIs], glucagon-like peptide-1 receptor analogue [GLP-1RAs], and sodium-glucose co-transporter-2 inhibitors [SGLT2is]), statins and other medications (Table S2). Fixed-dose combination formulations were counted as two different medications based on the active ingredient. Time-varying exposure to RASi and other medications were based on start and end dates of dispensing records within each follow-up year for each patient.21 Prior treatment duration with each medication was defined based on start and end dates of dispensing records to the index date. We converted the daily dose of ACEi/ARBs into lisinopril-dose equivalent for each patient (Table S3),22 and calculated the time-weighted mean daily RASi dose based on the mean daily dose dispensed during the follow-up period.23
Covariates
Baseline covariates included clinical and laboratory data collected during structured diabetes assessments, including socio–demographic profile, history of comorbidities, clinical (blood pressure, body mass index [BMI], waist circumference [WC]) and laboratory values. These included HbA1c, lipids (triglyceride [TG], low-density lipoprotein cholesterol [LDL-C], high-density lipoprotein cholesterol [HDL-C], total cholesterol [TC]), urine albumin-creatinine-ratio (uACR) and eGFR. The laboratory values for plasma glucose, lipids, potassium levels, eGFR, comorbidities (hospitalizations due to renal, CVD, peripheral vascular disease [PVD], and cancer events defined by self-reported history at assessment or ICD-9 and ICD-10 codes) and dispensing records during the baseline and observation periods in the HKDSD were retrieved from the HA-EMR system. Details on covariate definitions are provided in Supplementary Methods.
Statistical analysis
All descriptive statistics were reported as counts (percentages), mean (standard deviation, SD), or median (interquartile range, IQR). Standardized mean difference (SMD) was used to check the balance of each covariate in the between-group comparisons.
In the population-based cohort, we performed risk association analyses on clinical outcomes in discontinued-RASi versus continued-RASi users after propensity-score overlap-weighting (PS-OW) to homogenize baseline data and address confounding by indication.24 We calculated the PS using a multivariate logistic model, and used the effect size of selected covariates to assign weights to balance all confounders at baseline for each patient using the PS-OW approach (Supplementary Methods and Table 1).24,25 Compared with the classic PS-based methods of matching and inverse-probability of treatment-weighting, PS-OW mimics attributes of RCTs and has better performance with respect to target population, balance and precision.24
Table 1.
Clinical profiles of patients categorized by RASi discontinuation when eGFR declined to <30 mL/min/1.73 m2 before and after propensity score (PS) overlap-weighting.
| Variables | Overall | Before PS overlap-weighting |
After PS overlap-weighting |
||||
|---|---|---|---|---|---|---|---|
| Continued | Discontinued | SMD | Continued | Discontinued | SMD | ||
| No | 10,400 | 8634 | 1766 | 8634 | 1766 | ||
| Men, % | 4835 (46.5) | 3979 (46.1) | 856 (48.5) | 0.048 | 48.2 | 48.2 | <0.001 |
| Women,% | 5565 (53.5) | 4655 (53.9) | 910 (51.5) | 0.032 | 51.8 | 51.8 | |
| Age at index date, years | 73.1 (11.4) | 73.1 (11.4) | 73.3 (11.0) | 0.023 | 73.3 (11.5) | 73.3 (11.0) | <0.001 |
| Duration of diabetes, years | 14.0 (8.1) | 14.1 (8.1) | 13.2 (8.2) | 0.117 | 13.4 (8.0) | 13.4 (8.2) | <0.001 |
| Family history, % | 4162 (40.0) | 3556 (41.2) | 606 (34.3) | 0.142 | 35.7 | 35.7 | <0.001 |
| Use of tobacco, % | 0.05 | <0.001 | |||||
| Never | 7080 (68.1) | 5854 (67.8) | 1226 (69.4) | 69.0 | 69.0 | ||
| Ever | 2204 (21.2) | 1832 (21.2) | 372 (21.1) | 21.2 | 21.2 | ||
| Current | 1116 (10.7) | 948 (11.0) | 168 (9.5) | 9.8 | 9.8 | ||
| Use of alcohol, % | 0.065 | <0.001 | |||||
| Never | 7995 (76.9) | 6615 (76.6) | 1380 (78.1) | 77.9 | 77.9 | ||
| Current | 1261 (12.1) | 1077 (12.5) | 184 (10.4) | 10.7 | 10.7 | ||
| Ever | 1144 (11.0) | 942 (10.9) | 202 (11.4) | 11.4 | 11.4 | ||
| Body mass index (BMI), kg/m2 | 25.7 (4.2) | 25.8 (4.2) | 25.3 (4.3) | 0.135 | 25.4 (4.0) | 25.4 (4.3) | <0.001 |
| BMI missing, % | 4.4 | 3.3 | 9.8 | ||||
| Waist circumference (WC), cm | 90.8 (10.4) | 90.9 (10.3) | 90.1 (10.7) | 0.078 | 90.2 (10.1) | 90.2 (10.7) | <0.001 |
| WC missing, % | 6.5 | 5.3 | 12.7 | ||||
| SBP, mmHg | 141.2 (14.0) | 141.2 (14.0) | 140.9 (13.9) | 0.021 | 141.0 (14.4) | 141.0 (13.9) | <0.001 |
| SBP missing, % | 2.1 | 1.2 | 6.8 | ||||
| DBP, mmHg | 73.0 (9.2) | 73.0 (9.3) | 73.0 (9.0) | 0.004 | 73.0 (9.7) | 73.0 (8.9) | <0.001 |
| DBP missing, % | 2.1 | 1.2 | 6.8 | ||||
| HDL-C, mmol/L | 1.2 (0.4) | 1.2 (0.4) | 1.2 (0.4) | 0.008 | 1.2 (0.4) | 1.2 (0.4) | <0.001 |
| HDL-C missing, % | 3.1 | 2.7 | 5 | ||||
| LDL-C, mmol/L | 2.4 (1.0) | 2.4 (1.0) | 2.5 (1.0) | 0.027 | 2.5 (1.0) | 2.5 (1.0) | <0.001 |
| LDL-C missing, % | 3.3 | 2.9 | 5.5 | ||||
| Total cholesterol (TC), mmol/L | 4.4 (1.2) | 4.4 (1.2) | 4.4 (1.2) | 0.021 | 4.4 (1.2) | 4.4 (1.2) | <0.001 |
| TC missing, % | 2.4 | 2.1 | 3.9 | ||||
| Triglyceride (TG), mmol/L | 1.8 (1.2) | 1.8 (1.2) | 1.7 (1.1) | 0.101 | 1.7 (1.1) | 1.7 (1.1) | <0.001 |
| TG missing, % | 2.5 | 2.1 | 4.1 | ||||
| Blood haemoglobin (HB), g/dL | 11.4 (1.9) | 11.4 (1.9) | 11.4 (1.9) | 0.047 | 11.4 (1.9) | 11.4 (1.9) | <0.001 |
| HB missing, % | 3.4 | 3.4 | 3.3 | ||||
| HbA1c, % | 7.5 (1.6) | 7.5 (1.6) | 7.5 (1.7) | 0.003 | 7.5 (1.6) | 7.5 (1.7) | <0.001 |
| HbA1c missing, % | 0.7 | 0.5 | 1.6 | ||||
| eGFR, mL/min/1.73m2 | 29.2 (11.5) | 29.0 (11.0) | 29.9 (13.4) | 0.093 | 29.9 (12.3) | 29.9 (13.0) | <0.001 |
| Medications, % | |||||||
| Diuretics | 3326 (32.0) | 2825 (32.7) | 501 (28.4) | 0.095 | 28.9 | 28.9 | <0.001 |
| Beta-blockers | 4854 (46.7) | 4051 (46.9) | 803 (45.5) | 0.029 | 45.6 | 45.6 | <0.001 |
| Calcium-channel blockers | 7841 (75.4) | 6566 (76.0) | 1275 (72.2) | 0.088 | 72.8 | 72.8 | <0.001 |
| Statins | 6135 (59.0) | 5221 (60.5) | 914 (51.8) | 0.176 | 53.6 | 53.6 | <0.001 |
| Non-statins lipid-modifying | 588 (5.7) | 484 (5.6) | 104 (5.9) | 0.012 | 5.8 | 5.8 | <0.001 |
| Glucose-lowering drugs (GLDs) | |||||||
| Insulin | 2746 (26.4) | 2330 (27.0) | 416 (23.6) | 0.079 | 24.3 | 24.3 | <0.001 |
| Metformin | 8094 (77.8) | 6726 (77.9) | 1368 (77.5) | 0.011 | 77.7 | 77.7 | <0.001 |
| Sulfonylureas | 6798 (65.4) | 5633 (65.2) | 1165 (66.0) | 0.015 | 65.9 | 65.9 | <0.001 |
| AGIs | 147 (1.4) | 119 (1.4) | 28 (1.6) | 0.017 | 1.5 | 1.5 | <0.001 |
| TZD | 265 (2.5) | 229 (2.7) | 36 (2.0) | 0.041 | 2.1 | 2.1 | <0.001 |
| DPP-4is | 1229 (11.8) | 1057 (12.2) | 172 (9.7) | 0.08 | 10.2 | 10.2 | <0.001 |
| GLP-1RA | 130 (1.2) | 88 (1.0) | 42 (2.4) | 0.105 | 1.9 | 1.9 | <0.001 |
| SGLT2i | 32 (0.3) | 28 (0.3) | 4 (0.2) | 0.019 | 0.2 | 0.2 | <0.001 |
| Number of GLDs | 0.077 | <0.001 | |||||
| 0 | 599 (5.8) | 471 (5.5) | 128 (7.2) | 6.8 | 6.8 | ||
| 1 | 2751 (26.5) | 2290 (26.5) | 461 (26.1) | 26.3 | 26.3 | ||
| 2 | 4897 (47.1) | 4067 (47.1) | 830 (47.0) | 47.2 | 47.2 | ||
| ≥3 | 2153 (20.7) | 1806 (20.9) | 347 (19.6) | 19.7 | 19.7 | ||
| Medication treatment time, years | |||||||
| RASi | 4.5 (3.1) | 4.7 (3.1) | 3.9 (3.1) | 0.259 | 4.0 (2.9) | 4.0 (3.2) | <0.001 |
| Calcium-channel blockers | 5.6 (4.7) | 5.8 (4.8) | 4.8 (4.5) | 0.23 | 4.9 (4.5) | 4.9 (4.5) | <0.001 |
| Beta-blockers | 3.6 (4.6) | 3.7 (4.7) | 3.2 (4.4) | 0.119 | 3.3 (4.4) | 3.3 (4.5) | <0.001 |
| Diuretics | 1.4 (2.6) | 1.5 (2.7) | 1.1 (2.2) | 0.173 | 1.2 (2.3) | 1.2 (2.3) | <0.001 |
| Statins | 2.5 (3.1) | 2.7 (3.1) | 2.0 (2.8) | 0.209 | 2.1 (2.8) | 2.1 (2.9) | <0.001 |
| Metformin | 6.7 (4.5) | 6.8 (4.5) | 6.0 (4.4) | 0.181 | 6.2 (4.4) | 6.2 (4.4) | <0.001 |
| Sulfonylureas | 5.9 (4.7) | 6.0 (4.7) | 5.4 (4.5) | 0.125 | 5.5 (4.6) | 5.5 (4.5) | <0.001 |
| Insulin | 1.3 (3.0) | 1.3 (3.1) | 1.1 (2.9) | 0.081 | 1.1 (2.8) | 1.1 (3.0) | <0.001 |
| Complications history | |||||||
| CVD | 1743 (16.8) | 1443 (16.7) | 300 (17.0) | 0.007 | 16.9 | 16.9 | <0.001 |
| IHD | 1048 (10.1) | 891 (10.3) | 157 (8.9) | 0.049 | 9.2 | 9.2 | <0.001 |
| AMI | 472 (4.5) | 404 (4.7) | 68 (3.9) | 0.041 | 4 | 4 | <0.001 |
| Stroke | 672 (6.5) | 536 (6.2) | 136 (7.7) | 0.059 | 7.3 | 7.3 | <0.001 |
| Heart failure | 978 (9.4) | 868 (10.1) | 110 (6.2) | 0.14 | 6.8 | 6.8 | <0.001 |
| Cancer | 523 (5.0) | 418 (4.8) | 105 (5.9) | 0.049 | 5.8 | 5.8 | <0.001 |
| PVD | 397 (3.8) | 328 (3.8) | 69 (3.9) | 0.006 | 3.9 | 3.9 | <0.001 |
| Period of index year | 0.23 | <0.001 | |||||
| 2002–2006 | 409 (3.9) | 288 (3.3) | 121 (6.9) | 5.9 | 5.9 | ||
| 2007–2010 | 1299 (12.5) | 1011 (11.7) | 288 (16.3) | 15.4 | 15.4 | ||
| 2011–2014 | 3356 (32.3) | 2789 (32.3) | 567 (32.1) | 32.4 | 32.4 | ||
| 2015–2018 | 5336 (51.3) | 4546 (52.7) | 790 (44.7) | 46.4 | 46.4 | ||
SMD, standardized mean difference; RASi, renin angiotensin system inhibitors; BP, blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate; AGIs: alpha-glucosidase inhibitors; TZDs: thiazolidinediones; DPP-4i: dipeptidyl peptidase 4 inhibitors; GLP1-RA: glucagon-like peptide-1 receptor analogues; SGLT2i: sodium-glucose co-transporter 2 inhibitors; GLDs: glucose-lowering drugs; CVD, cardiovascular disease; IHD, Ischemic heart disease; AMI, acute myocardial infarction; PVD, peripheral vascular disease.
In the PS-OW weighted cohort, we performed Cox-model with time-varying RASi exposure to address immortal bias due to restart and/or discontinuation of RASi, adjustment for other time-varying covariates including HbA1c, lipids, use of GLDs and statins.26 For all-cause and cause-specific mortality analyses, we used fixed-time Cox-model to avoid overestimating the association due to discontinued-RASi at death. We tested assumptions of missing data using R ‘MissMech’ package. The data was non missing completely at random (MCAR). Missing values of covariates including baseline covariates and time-varying covariates (HbA1c, eGFR and lipids, proportion of missing <15%) were imputed using the chained-equations with multiple imputations by R ‘smcfcs’ package with inclusion of all covariates, the outcome of interest, and the exposure in each Cox regression model.27 We used the default number of imputed datasets to generate imputations in each Cox model (m = 5). This imputation method performs well for different types of missing patterns including non-MCAR.27
Subgroup analyses
We conducted subgroup analyses in permanently discontinued-RASi and stop-restart RASi versus continued-RASi users in separate PS-OW cohorts. We compared the risk associations of discontinued-RASi versus continued ACEi-only or ARBs-only use with outcomes of interest. Results were expressed as hazard ratio (HR) with 95% CI. We checked for violation of the assumption of proportional hazards using scaled-Schoenfeld-residual plots.28
Supporting and sensitivity analyses
To further address confounding by indication and time-varying confounders related to RASi discontinuation, we used Cox marginal-structural-model (Cox-MSM) to assess the discontinuation of RASi with risk of ESKD, MACE and heart failure.29 The Cox-MSM models estimate the “marginal” or “absolute” treatment effects in a population through weighting and reweighting observations based on baseline and time-dependent covariates. Potential confounding was controlled by the inverse probability of treatment weights (IPTWs) which utilized the patient's covariates to estimate the probability of therapy with RASi and the probability of being censored in the follow-up period. We applied the inverse probability of censoring weights (IPCW) to account for death to address bias introduced by informative censoring in this study. The outcome model was fitted by multiplying the IPTW and IPCW in the Cox-MSM model. Because the Cox-MSM model estimates can be unstable in the presence of disproportionately large IPTW, we used stabilized inverse probability treatment weights and truncated weights at 5th and 99th percentile (Supplementary Methods).30 We also limited the analysis to those with uACR data at new-onset eGFR<30 ml/min/1.73 m2 (n = 5249) and assessed the risk associations between RASi discontinuation and outcomes adjusted for uACR.
Incidence of hyperkalemia in the registry-based cohort
As plasma potassium data was not available in the population-based cohort, we conducted a complementary analysis to determine the occurrence of hyperkalemia with RASi discontinuation versus continuation in a register-based cohort - the Hong Kong Diabetes Register (HKDR) with available data. The HKDR12 first established in 1995, is an ongoing research-driven quality improvement program with a structured-protocol for periodic comprehensive assessment of risk factors and complications that is linked to the HA-EMR system. Personal data and clinical measurements were documented during structured-assessments upon enrolment to the HKDR. Laboratory assessments such as plasma potassium, lipids, HbA1c and eGFR, and use of medications were curated from the HA-EMR system. In the HKDR, we curated data from 30,503 patients with diabetes enrolled in 2001–2020 observed until 30 June 2021.18 Using the same inclusion and exclusion criteria as the main analysis, we identified 4400 RASi-users in whom eGFR decreased to <30 ml/min/1.73 m2 with 3817 (86.7%) continued-RASi and 583 (13.3%) discontinued-RASi users within first 6 months after reaching eGFR <30 ml/min/1.73 m2 (Fig. S1).
We defined hyperkalemia events based on occurrence of plasma potassium ≥5.5 mmol/L after eGFR reached to <30 ml/min/1.73 m2 excluding values measured during hospitalization with AKI. Hyperkalemia events separated by more than one month were regarded as separate events. We calculated cumulative incidence of hyperkalemia among discontinued-RASi users and continued-RASi users in the follow-up. We compared the risk associations between discontinued-RASi and continued-RASi users with first occurrence of hyperkalemia adjusted for potential confounders including plasma potassium at new-onset eGFR<30 ml/min/1.73 m2 in the PS-OW weighted cohort. We estimated the relationships of time-weighted mean daily dose of lisinopril-dose equivalent with risk of first event of hyperkalemia by using penalized spline curve in the PS-OW weighted cohort. Likelihood-ratio test was used to select the spline models with 3-knots. We further explored the dose–response relationships of time-weighted mean daily dose of lisinopril-dose equivalent with risk of hyperkalemia, and the interaction between baseline uACR (<3, 3–30, >30 mg/mmol) and RASi discontinuation (discontinued- and continued RASi use) by including cross-product terms in the model.31
All analyses were implemented using R software (Version 4.0.0). We used PSweight and survey packages to fit the PS-OW weighted models and Cox-models. A two-sided P value of <0.05 was considered statistically significant.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. A.L. had full access to HKDSD data. E.C. is the guarantor of this work with final responsibility for the decision to submit for publication.
Results
We curated a cohort of 10,400 patients with new-onset eGFR<30 ml/min/1.73 m2 from the RAMP-DM module including 1766 (17.0%) discontinued-RASi and 8634 (83.0%) continued-RASi users during a median 3.6 (IQR: 2.1–5.8) years of follow-up to death (41,623 person-years). Amongst 19,400 patients, 89.3% patients had a subsequent eGFR <30 ml/min/1.73 m2 within first 2 years of follow-up. The median of follow-up to death was 4.1 (IQR: 2.3–6.5) years for discontinued-RASi users and 3.6 (IQR: 2.1–5.7) years for continued-RASi users. Amongst 1766 discontinued-RASi users, 63.2% (n = 1116) had permanently discontinued-RASi and 36.8% (n = 650) stopped then restarted RASi treatment. The mean age at baseline was 73.1 years, with a mean diabetes duration of 14.0 years. At baseline, continued-RASi users were more likely to have heart failure and treated with statins and DPP-4is than discontinued-RASi users. In the PS-OW weighted cohort, all characteristics were well-balanced between the two groups (Table 1).
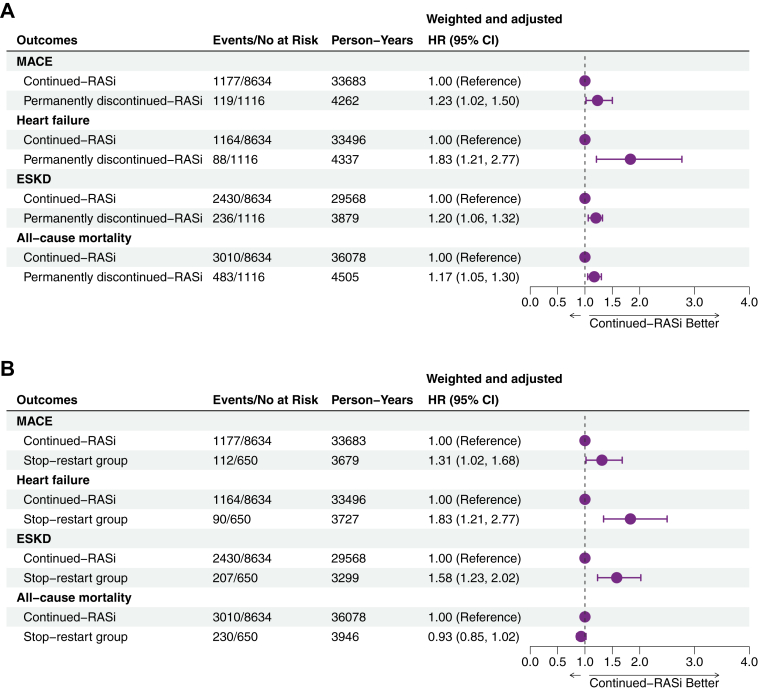
Discontinued-RASi use, incidence of clinical outcomes and mortality
The respective crude-incidence (95% CI) in discontinued-RAS and continued-RASi users were 29.1 (25.5–33.1) and 34.9 (33.0–37.0) events for MACE, 22.1 (18.9–25.6) and 34.8 (32.8–36.8) events for heart failure, 61.7 (56.1–67.7) and 82.2 (78.9–85.5) events for ESKD, and 84.4 (78.3–90.8) and 83.4 (80.5–86.5) events for all-cause mortality per 1000-person-years. Compared to continued-RASi, discontinued-RASi was associated with higher risk of MACE (weighted and adjusted HR = 1.27, 95% CI: 1.08–1.49), heart failure (HR = 1.85, 95% CI: 1.53–2.25) and ESKD (HR = 1.30, 95% CI: 1.17–1.43) (Fig. 3), but neutral risk of all-cause mortality (HR = 0.93, 95% CI: 0.86–1.01) as well as CV (HR = 0.89, 95% CI: 0.73–1.08), cancer (HR = 0.0.97, 95% CI: 0.76–1.22), and other (HR = 0.94, 95% CI: 0.85–1.04) cause-specific mortalities (Table S4).
Fig. 3.
Number of clinical events (A) and weighted and adjusted Kaplan–Meier curves of discontinued-RASi versus continued-RASi use for MACE (B), heart failure (C), ESKD (D), and all-cause mortality (E) in patients with type 2 diabetes and advanced chronic kidney disease (eGFR reached 30 mL/min/1.73 m2). Weighted and adjusted hazard ratio (HRs) and 95% CIs of MACE, heart failure, and ESKD were yielded using Cox model with time-varying RASi use, adjusting for time-varying HbA1c, lipids, age, medications, and comorbidities in the overlap-weighted cohort. Results of all-cause mortality was yielded using time-fixed Cox model in the overlap-weighed cohort. Abbreviations: RASi, renin angiotensin system inhibitor; MACE, major adverse cardiovascular events; ESKD, end-stage kidney disease; eGFR, estimated glomerular filtration rate.
Subgroup analyses
We performed the two subgroups of the discontinued-RASi (permanently and stop-restart) versus continued-RASi use (Table S5). Compared with continued-RASi use, both permanently and stop-restart discontinued-RASi use were similarly associated with higher risk of MACE, heart failure, and ESKD (Fig. 4). The respective higher and neutral risk of all-cause mortality was observed in permanently discontinued-RASi (HR = 1.17, 95% CI: 1.05–1.30) (Fig. 4A) and stop-restart RASi (HR = 0.93, 95% CI: 0.85–1.02) (Fig. 4B). Discontinued-RASi was associated with higher risk of MACE (HR = 1.32, 95% CI: 1.12–1.56), heart failure (HR = 1.78, 95% CI: 1.46–2.17) and ESKD (HR = 1.24, 95% CI: 1.12–1.37) versus continued ACEi-only use (Fig. S2). The higher risk of heart failure and ESKD, and neutral risk of MACE and all-cause mortality were observed in the continued ARBs-only versus discontinued-RASi users (Fig. S2).
Fig. 4.
Subgroup analyses of discontinued-RASi users comparing permanently discontinued (A) and stop-restart (B) groups versus continued-RASi use with risk of clinical events in patients with type 2 diabetes and advanced chronic kidney disease (eGFR reached 30 mL/min/1.73 m2). Weighted and adjusted hazard ratio (HRs) and 95% CIs of MACE, heart failure, and ESKD were yielded using Cox model with time-varying RASi use, adjusting for time-varying HbA1c, lipids, age, medications, and comorbidities in the overlap-weighted cohort. Results of all-cause mortality were yielded using the time-fixed Cox model in the overlap-weighed cohort. Abbreviations: RASi, renin-angiotensin system inhibitor; MACE, major adverse cardiovascular events; ESKD, end-stage kidney disease; eGFR, estimated glomerular filtration rate.
Sensitivity analyses
In the Cox-MSM model, the higher risk of MACE (HR = 1.37, 95% CI: 1.20–1.56), heart failure (HR = 2.00, 95% CI: 1.72–2.34), and ESKD (HR = 1.12, 95% CI: 1.03–1.22) in discontinued-RASi users remained consistent. In the sub-cohort of 5249 patients with baseline uACR data, the respective proportion of patients with uACR<3, 3–30 and > 30 mg/mmol in continued-RASi and discontinued-RASi users was 22.4%-versus-28.8%, 38.6%-versus-40.7%, and 38.9%-versus-30.5% (Table S6). We observed higher risk of MACE (HR = 1.36, 95% CI: 1.03–1.81), heart failure (HR = 1.84 95% CI: 1.34–2.51) and ESKD (HR = 1.17, 95% CI: 1.01–1.37), and neutral risk of all-cause mortality (HR = 1.11, 95% CI: 0.97–1.28) in discontinued-RASi (n = 820) versus continued-RASi users (n = 4429) in the PS-OW weighted cohort (Fig. S3).
RASi discontinuation and risk of hyperkalemia
In the register-based cohort, we included 4400 patients with new-onset eGFR<30 ml/min/1.73 m2 (583 discontinued-RASi and 3817 continued-RASi users). The cumulative incidence of hyperkalemia (≥5.5 mmol/L) was 58.2% (n = 2565 of 4400 patients) during a median follow-up of 5.0 (IQR: 2.8–7.8) years to death (25,702 person-years) (51.1%, n = 298 of 583 for discontinued-RASi users, and 59.4%, n = 2267 of 3817 for continued-RASi users).
Overall, the crude-incidence of first hyperkalemia event was 99.8 (95% CI: 96.0–103.7) per-1000-patient-years. The respective rates were 101.2 (95% CI: 90.1–113.4) events per-1000-patient-years for discontinued-RASi users, and 99.6 (95% CI: 95.6–103.8) events per-1000-patient-years for continued-RASi users. After balancing characteristics of the two groups in the PS-OW cohort (Table S7), we observed neutral risk of first event of hyperkalemia in discontinued-RASi versus continued-RASi users (HR = 0.95, 95% CI: 0.84–1.08) (Table S8). In the spline analysis, there was a non-linear relationship for time-weighted mean daily dose of RASi with the risk of first hyperkalaemia event which increased above a lisinopril-equivalent dose of 20 mg daily (Fig. S4). We observed interactions between baseline uACR, RASi discontinuation with risk of hyperkalemia (Table S9). Those with abnormal uACR (≥30 mg/mmol) had highest risk of hyperkalemia overall. In patients with abnormal baseline uACR (≥30 mg/mmol), the risk of hyperkalemia was higher in continued-RASi users versus discontinued users. However, the risk of hyperkalemia was higher in discontinued-RASi users with normal baseline uACR (P interaction = 0.011).
Discussion
In this cohort analysis of over 10,000 patients with T2D and advanced-CKD, discontinued-RASi use was consistently associated with 1.2–1.8-fold higher risk of MACE, heart failure and ESKD but neutral risk of death versus continued-RASi use. Similarly, increased risks were observed in those who permanently discontinued-RASi and those who discontinued within 6 months of new-onset eGFR <30 ml/min/1.73 m2 but later restarted RASi versus continued-RASi users. Our findings were robust to sensitivity analyses using marginal-structured-modelling to account for time-dependent confounders and adjusting for albuminuria. Discontinued-RASi was associated with neutral risk of hyperkalemia in the register-based cohort.
Our findings are consistent with the Swedish-Renal-Registry, which examined risks of MACE in 10,254 prevalent-RASi users (50% with diabetes), comparing those who discontinued versus continued RASi within 6 months of new-onset eGFR <30 ml/min/1.73 m2.5 Stopping RASi was associated with higher 5-year risk of MACE (47.6% versus 59.5%, absolute-risk-difference: 11.9 per-100-patients). In another retrospective PS-matched analysis of 3909 patients with CKD in a US health system, those who discontinued-RASi within 6 months of eGFR<30 ml/min/1.73 m2 were at 1.4-fold higher risk of MACE.4 Both of these studies4,5 did not report heart failure as a separate outcome. In our analysis, discontinued-RASi users had higher risk of heart failure. This real-world data are in agreement with RCT evidence where ARBs such as losartan was confirmed to reduce the risk of hospitalizations due to heart failure by 32% versus placebo in 1533 patients with T2D with CKD.1 Given the frequent coexistence of CKD and heart failure, our findings support continuation of RASi in patients with advanced-CKD to reduce risk of heart failure, albeit with monitoring of serum potassium and dose adjustment as necessary.
In our study, discontinued-RASi use was associated with a 1.3-fold higher risk of ESKD versus continued-RASi use. In the Swedish-Renal-Registry, there was a 8% decrease in absolute risk of initiating kidney-replacement therapy in discontinued-RASi users.5 In a US retrospective cohort with 3909 patients, the risk of ESKD was similar between discontinued-RASi and continued-RASi users (HR = 1.19, 95% CI: 0.86–1.65).4 In the RENAAL study,32 protective benefits of losartan were observed across the eGFR range, and the greatest absolute reduction in kidney failure was observed in the lowest eGFR tertile. We also observed a neutral risk of discontinued-RASi use on death which differed from other observational cohorts which reported higher incidence of death in discontinued-RASi users.4,5 This may reflect differences in patient populations and overall pattern of deaths, with non-vascular deaths exceeding cardiovascular deaths among patients with diabetes in Hong Kong.33, 34, 35
We found that both permanently and stop-restart discontinued-RASi use were associated with worse outcomes than continued-RASi use. The stop-restart regimen might reflect the efforts of care providers to adjust treatment to improve tolerability although the observational nature of these data did not allow to us to explore this hypothesis systematically. Other observational studies also indicated that discontinued-RASi or down-titration of RASi were associated with higher risk of cardiovascular-events in the general population.36, 37, 38, 39 Taken together, patients who could not tolerate RASi with permanent or transient treatment discontinuation might have vulnerable renal or cardiac status which could compromise eGFR with hyperkalemia, putting them at high risk of adverse events.
In the register-based cohort, over 50% of patients with T2D experienced at least one episode of hyperkalemia with a higher cumulative incidence of hyperkalemia in continued-RASi users versus discontinued-RASi users (59.4% versus 51.1%). These high figures indicated that hyperkalemia is not an uncommon event in people with diabetes who are at risk of developing CKD. After balancing all characteristics, the discontinued-RASi had similar risk of first event of hyperkalemia as the continued-RASi (HR = 0.95, 95% CI: 0.84–1.08) which contrasts with some previous studies. In the current study, we showed a non-linear association between weighted mean daily RASi dose with increased risk of first event of hyperkalemia, but only at a lisinopril equivalent dose of greater than 20 mg. In further analyses, those with macroalbuminuria had the highest risk of hyperkalemia which was increased in continued-RASi users. However, within the subset of normoalbuminuric CKD patients with greater renovascular component to their disease, there was a paradoxically higher risk of hyperkalemia amongst discontinued-RASi users. These may partially explain the inconsistencies in hyperkalemia risk compared with previous studies. Pending further evidence, our findings suggest interruptions to RASi therapy might cause harm and that anticipatory actions such as correction of metabolic acidosis, avoidance of nephrotoxic drugs and foods with high potassium content, dose adjustment with frequent monitoring of renal function should be considered in order to persist the use of these organ protective drugs.40,41
The strengths of this study included a large prospective cohort of patients with T2D and advanced-CKD with a median 3.6 year of follow-up. To date, there are few dedicated studies in Asians known to have high prevalence of diabetes and CKD.42 We conducted detailed analyses and used PS-OW weighted cohort to control for confounding by indication and time-related bias with adjustment for time-varying RASi exposure and other key covariates. There are several limitations. Unfortunately, the exact reasons for RASi discontinuation were not captured in the HKDSD. However, within the registry-based cohort, the prevalence of hyperkalemia >5.5 mmol/L was nearly threefold higher in discontinued versus continued users at baseline. Withdrawal due to angioedema/or cough is less likely since most of patients have been treated with these agents several years prior. Discontinuation due to hypotension is less likely, as most patients are treated with additional non-RASi antihypertensives at baseline in this cohort. In clinical practice, reasons for RASi discontinuation are frequently multifactorial but hyperkalemia and eGFR decline are likely to be the main causes. Due to suboptimal adherence to the assessment protocol in the RAMP-DM module, uACR data could only be included in a sensitivity analysis. We were unable to assess drug adherence as medication exposure was based on dispensing data. We also lacked detailed records on use of potassium-sparing, thiazide or loop diuretics, potassium supplements and binders, as well as data on metabolic acidosis, which might confound associations. There were too few patients on SGLT2i to evaluate their potential synergistic effects with RASi on glomerular filtration.39 Although we performed multiple time-related methods to minimize the time-related bias and confounding by indication with the availability of detailed information during follow-up, residual confounding and time-related bias remained possible.
In conclusion, in this real-world study, permanent or transient discontinuation of RASi in patients with T2D and advanced-CKD was associated with increased risk of MACE, heart failure and ESKD. In accordance to international recommendations, anticipatory or corrective actions should be taken to ensure continuation of RASi for organ protection with more frequent monitoring of eGFR including the use of newer potassium binding agents.43 The STOP-ACEi Trial, now published since acceptance of this article, also reported a non-statistically significant association of RASi discontinuation with increased risk of ESKD (HR = 1.28, 95% CI: 0.99–1.65) among 411 patients with advanced-CKD over a 3-year follow-up period.44 Our real-world data support continuing use of RASi in patients with eGFR <30 ml/min/1.73 m2 for cardiovascular-renal protection.45
Contributors
AY and EC contributed to conception of the article, statistical analysis, interpretation of results, drafting, revision and approval of the manuscript. AY and MS accessed and verified the underlying data. HW, ESHL, MS, BF, and XZ contributed to interpretation of results, revised the manuscript critically and approved the final version. APSK, RCWM, AOYL, and JCNC contributed to conception of the article, revised the manuscript critically and approved the final version. EC is the guarantor of this work and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Data sharing statement
We welcome collaborative research. Aggregate data may be available upon reasonable request. Proposals for future collaborations can be submitted to the HKDSD investigators (andrealuk@cuhk.edu.hk) for consideration.
Declaration of interests
JCNC has received research grants and/or honoraria for consultancy or giving lectures, from AstraZeneca, Bayer, Boehringer Ingelheim, Eli Lilly & Co, Hua Medicine, Lee Powder, Merck Serono, Merck Sharp & Dohme, Pfizer, Servier, Sanofi and Viatris Pharmaceutical. APSK has received research grants and/or speaker honoraria from Abbott, AstraZeneca, Bayer, Boehringer Ingelheim, Eli-Lilly, Kyowa Kirin, Merck Serono, Nestle, Novo Nordisk, Pfizer and Sanofi. AOYL has served as a member of advisory panel for Amgen, AstraZeneca, Boehringer Ingelheim and Sanofi and received research support from Amgen, Asia Diabetes Foundation, Bayer, Boehringer Ingelheim, Lee's Pharmaceutical, MSD, Novo Nordisk, Roche, Sanofi, Sugardown Ltd, Takeda. None of these relationships had any influence on the content of the present manuscript. RCWM has received research funding from AstraZeneca, Bayer, Merck Sharp & Dohme, Novo Nordisk, Pfizer and Tricida Inc. for carrying out clinical trials, and has received speaker honorarium or consultancy in advisory boards from AstraZeneca, Bayer and Kyowa Kirin. All proceeds have been donated to the Chinese University of Hong Kong to support diabetes research. Other authors have no conflicts of interest to disclose.
Acknowledgments
We acknowledge the Hong Kong Hospital Authority for providing the clinical data. AY was supported by a CUHK Impact Research Fellowship Scheme. Part of this work has been presented as an oral abstract at the 82nd American Diabetes Association Scientific Sessions, New Orleans.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2022.101751.
Appendix A. Supplementary data
References
- 1.Brenner B.M., Cooper M.E., De Zeeuw D., et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–869. doi: 10.1056/NEJMoa011161. [DOI] [PubMed] [Google Scholar]
- 2.Dagenais G.R., Yusuf S., Bourassa M.G., et al. Effects of ramipril on coronary events in high-risk persons. Circulation. 2001;104(5):522–526. doi: 10.1161/hc3001.093502. [DOI] [PubMed] [Google Scholar]
- 3.Lewis E.J., Hunsicker L.G., Clarke W.R., et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–860. doi: 10.1056/NEJMoa011303. [DOI] [PubMed] [Google Scholar]
- 4.Qiao Y., Shin J.-I., Chen T.K., et al. Association between renin-angiotensin system blockade discontinuation and all-cause mortality among persons with low estimated glomerular filtration rate. JAMA Intern Med. 2020;180(5):718. doi: 10.1001/jamainternmed.2020.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fu E.L., Evans M., Clase C.M., et al. Stopping renin-angiotensin system inhibitors in patients with advanced CKD and risk of adverse outcomes: a nationwide study. J Am Soc Nephrol. 2021;32(2):424–435. doi: 10.1681/ASN.2020050682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmidt M., Mansfield K.E., Bhaskaran K., et al. Adherence to guidelines for creatinine and potassium monitoring and discontinuation following renin–angiotensin system blockade: a UK general practice-based cohort study. BMJ Open. 2017;7(1) doi: 10.1136/bmjopen-2016-012818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hunter R.W., Bailey M.A. Hyperkalemia: pathophysiology, risk factors and consequences. Nephrol Dial Transplant. 2019;34(Supplement_3) doi: 10.1093/ndt/gfz206. iii2-iii11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruggenenti P., Perna A., Remuzzi G. ACE inhibitors to prevent end-stage renal disease: when to start and why possibly never to stop: a post hoc analysis of the REIN trial results. Ramipril Efficacy in Nephropathy. J Am Soc Nephrol. 2001;12(12):2832–2837. doi: 10.1681/ASN.V12122832. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed A.K., Kamath N.S., El Kossi M., El Nahas A.M. The impact of stopping inhibitors of the renin-angiotensin system in patients with advanced chronic kidney disease. Nephrol Dial Transplant. 2010;25(12):3977–3982. doi: 10.1093/ndt/gfp511. [DOI] [PubMed] [Google Scholar]
- 10.Navaneethan S.D., Zoungas S., Caramori M.L., et al. Diabetes management in chronic kidney disease: synopsis of the 2020 KDIGO clinical practice guideline. Ann Intern Med. 2020;174(3):385–394. doi: 10.7326/M20-5938. [DOI] [PubMed] [Google Scholar]
- 11.Bhandari S., Ives N., Brettell E.A., et al. Multicentre randomized controlled trial of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker withdrawal in advanced renal disease: the STOP-ACEi trial. Nephrol Dial Transplant. 2015:gfv346. doi: 10.1093/ndt/gfv346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan J.C., Lim L.-L., Luk A.O., et al. From Hong Kong diabetes register to JADE program to RAMP-DM for data-driven actions. Diabetes Care. 2019;42(11):2022–2031. doi: 10.2337/dci19-0003. [DOI] [PubMed] [Google Scholar]
- 13.Wu H., Lau E.S.H., Yang A., et al. Data resource profile: the Hong Kong diabetes surveillance database (HKDSD) Int J Epidemiol. 2021;51(2):e9–e17. doi: 10.1093/ije/dyab252. [DOI] [PubMed] [Google Scholar]
- 14.Yang A., Wu H., Lau E.S., et al. Trends in glucose-lowering drug use, glycemic control, and severe hypoglycemia in adults with diabetes in Hong Kong, 2002–2016. Diabetes Care. 2020;43(12):2967–2974. doi: 10.2337/dc20-0260. [DOI] [PubMed] [Google Scholar]
- 15.Yang A., Wu H., Lau E.S., et al. Glucose-lowering drug use, glycemic outcomes, and severe hypoglycemia: 18-Year trends in 0· 9 million adults with Diabetes in Hong Kong (2002–2019) Lancet Reg Health West Pacific. 2022;26 doi: 10.1016/j.lanwpc.2022.100509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hernán M.A., Robins J.M. Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol. 2016;183(8):758–764. doi: 10.1093/aje/kwv254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schneeweiss S., Rassen J.A., Brown J.S., et al. Graphical depiction of longitudinal study designs in health care databases. Ann Intern Med. 2019;170(6):398–406. doi: 10.7326/M18-3079. [DOI] [PubMed] [Google Scholar]
- 18.Yang A., Shi M., Wu H., et al. Long-term metformin use and risk of pneumonia and related death in type 2 diabetes: a registry-based cohort study. Diabetologia. 2021;64(8):1760–1765. doi: 10.1007/s00125-021-05452-0. [DOI] [PubMed] [Google Scholar]
- 19.Levey A.S., Stevens L.A., Schmid C.H., et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong A.Y., Root A., Douglas I.J., et al. Cardiovascular outcomes associated with use of clarithromycin: population based study. BMJ. 2016:352. doi: 10.1136/bmj.h6926. [DOI] [PubMed] [Google Scholar]
- 21.Yang A., Wu H., Lau E.S.H., et al. Effects of RAS inhibitors on all-site cancers and mortality in the Hong Kong diabetes surveillance database (2002-2019) EBioMedicine. 2022;83 doi: 10.1016/j.ebiom.2022.104219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Houston B.A., Schneider A.L., Vaishnav J., et al. Angiotensin II antagonism is associated with reduced risk for gastrointestinal bleeding caused by arteriovenous malformations in patients with left ventricular assist devices. J Heart Lung Transplant. 2017;36(4):380–385. doi: 10.1016/j.healun.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 23.Yang A., Lau E.S.H., Wu H., et al. Attenuated risk association of end-stage kidney disease with metformin in type 2 diabetes with eGFR categories 1-4. Pharmaceuticals. 2022;15(9) doi: 10.3390/ph15091140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas L.E., Li F., Pencina M.J. Overlap weighting: a propensity score method that mimics attributes of a randomized clinical trial. JAMA. 2020 doi: 10.1001/jama.2020.7819. [DOI] [PubMed] [Google Scholar]
- 25.Westreich D., Cole S.R., Funk M.J., Brookhart M.A., Stürmer T. The role of the c-statistic in variable selection for propensity score models. Pharmacoepidemiol Drug Saf. 2011;20(3):317–320. doi: 10.1002/pds.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fu E.L., van Diepen M. Comment on Kwon et al. The Long-term Effects of Metformin on Patients With Type 2 Diabetic Kidney Disease. Diabetes Care. 2020;43:948-955. Diabetes Care. 2020;43(11) doi: 10.2337/dc19-0936. [DOI] [PubMed] [Google Scholar]
- 27.Murad H., Dankner R., Berlin A., Olmer L., Freedman L.S. Imputing missing time-dependent covariate values for the discrete time Cox model. Stat Methods Med Res. 2020;29(8):2074–2086. doi: 10.1177/0962280219881168. [DOI] [PubMed] [Google Scholar]
- 28.Stensrud M.J., Hernán M.A. Why test for proportional hazards? JAMA. 2020;323(14):1401–1402. doi: 10.1001/jama.2020.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pazzagli L., Linder M., Zhang M., et al. Methods for time-varying exposure related problems in pharmacoepidemiology: an overview. Pharmacoepidemiol Drug Saf. 2018;27(2):148–160. doi: 10.1002/pds.4372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hernán M.A., Brumback B., Robins J.M. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11(5):561–570. doi: 10.1097/00001648-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Yang J., Yang A., Wang Z., et al. Interactions between serum folate and human papillomavirus with cervical intraepithelial neoplasia risk in a Chinese population-based study. Am J Clin Nutr. 2018;108(5):1034–1042. doi: 10.1093/ajcn/nqy160. [DOI] [PubMed] [Google Scholar]
- 32.Remuzzi G. Continuum of renoprotection with losartan at all stages of type 2 diabetic nephropathy: a post hoc analysis of the RENAAL trial results. J Am Soc Nephrol. 2004;15(12):3117–3125. doi: 10.1097/01.ASN.0000146423.71226.0C. [DOI] [PubMed] [Google Scholar]
- 33.Wu H., Lau E.S., Ma R.C., et al. Secular trends in all-cause and cause-specific mortality rates in people with diabetes in Hong Kong, 2001–2016: a retrospective cohort study. Diabetologia. 2020;63(4):757–766. doi: 10.1007/s00125-019-05074-7. [DOI] [PubMed] [Google Scholar]
- 34.Chan J.C., Wat N.M., So W.-Y., et al. Renin angiotensin aldosterone system blockade and renal disease in patients with type 2 diabetes: an Asian perspective from the RENAAL study. Diabetes Care. 2004;27(4):874–879. doi: 10.2337/diacare.27.4.874. [DOI] [PubMed] [Google Scholar]
- 35.Imai E., Chan J.C., Ito S., et al. Effects of olmesartan on renal and cardiovascular outcomes in type 2 diabetes with overt nephropathy: a multicentre, randomised, placebo-controlled study. Diabetologia. 2011;54(12):2978–2986. doi: 10.1007/s00125-011-2325-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xie X., Liu Y., Perkovic V., et al. Renin-angiotensin system inhibitors and kidney and cardiovascular outcomes in patients with CKD: a bayesian network meta-analysis of randomized clinical trials. Am J Kidney Dis. 2016;67(5):728–741. doi: 10.1053/j.ajkd.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 37.Kovesdy C.P. Management of hyperkalaemia in chronic kidney disease. Nat Rev Nephrol. 2014;10(11):653–662. doi: 10.1038/nrneph.2014.168. [DOI] [PubMed] [Google Scholar]
- 38.Epstein M. Hyperkalemia constitutes a constraint for implementing renin-angiotensin-aldosterone inhibition: the widening gap between mandated treatment guidelines and the real-world clinical arena. Kidney Int Suppl (2011) 2016;6(1):20–28. doi: 10.1016/j.kisu.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leon S.J., Whitlock R., Rigatto C., et al. Hyperkalemia-related discontinuation of renin-angiotensin-aldosterone system inhibitors and clinical outcomes in CKD: a population-based cohort study. Am J Kidney Dis. 2022;80(2):164–173.e1. doi: 10.1053/j.ajkd.2022.01.002. [DOI] [PubMed] [Google Scholar]
- 40.De Boer I.H., Caramori M.L., Chan J.C.N., et al. Executive summary of the 2020 KDIGO Diabetes Management in CKD Guideline: evidence-based advances in monitoring and treatment. Kidney Int. 2020;98(4):839–848. doi: 10.1016/j.kint.2020.06.024. [DOI] [PubMed] [Google Scholar]
- 41.Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;98(4s):S1–S115. doi: 10.1016/j.kint.2020.06.019. [DOI] [PubMed] [Google Scholar]
- 42.Luk A.O., Li X., Zhang Y., et al. Quality of care in patients with diabetic kidney disease in Asia: the Joint Asia diabetes evaluation (JADE) registry. Diabet Med. 2016;33(9):1230–1239. doi: 10.1111/dme.13014. [DOI] [PubMed] [Google Scholar]
- 43.Georgianos P.I., Agarwal R. Revisiting RAAS blockade in CKD with newer potassium-binding drugs. Kidney Int. 2018;93(2):325–334. doi: 10.1016/j.kint.2017.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhandari S., Mehta A., Cleland J.G.F. Renin-angiotensin system inhibition in advanced chronic kidney disease. N Engl J Med. 2022 doi: 10.1056/NEJMoa2210639. [DOI] [PubMed] [Google Scholar]
- 45.Bakris G.L., Agarwal R., Anker S.D., et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020;383(23):2219–2229. doi: 10.1056/NEJMoa2025845. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.