Introduction
Hidradenitis suppurativa (HS) is a chronic inflammatory condition with a complex pathophysiology, including genetic, environmental, and microbiological factors. One of the early pathogenic changes in the disease’s development is considered to be follicular occlusion in apocrine gland–bearing skin. The natural history of HS is characterized by the recurrent development of inflammatory nodules, abscesses, and sinus tracts with subsequent scarring. The disease is associated with significant morbidity and requires long-lasting, continuous care. Over the last 2 decades, various laser treatments have increasingly been used in HS management, primarily ablative CO2 (10,600 nm) with secondary intention healing and Nd:YAG (1064 nm) for selective destruction of the follicular unit.1 Ablative fractional lasers (AFLs) have also been reported to improve scarring and, in combination with Nd:YAG, reduce inflammation.2 To our knowledge, no reports on the use of non-ablative fractional lasers (NAFLs Ga-As, 1540 nm) exist to date, although NAFLs have been shown to improve inflammatory acne.3
Case series
Our experience with 8 patients presenting with HS Hurley stages II and III who were treated with a combination of AFLs and NAFLs is set out below. Data from medical records were collected between November 2019 and April 2021, including treatment outcomes and patient characteristics (Table I).
Table I.
Mixed-technology CO2 and Ga-As laser in patients with hidradenitis suppurativa
| Patient no. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Sex | Female | Male | Female | Male | Male | Female | Female | Female |
| Age (y) | 23 | 57 | 26 | 22 | 35 | 49 | 28 | 26 |
| Duration of hidradenitis suppurativa (y) | 3 | 7 | 1 | 8 | 9 | 42 | 15 | 4 |
| Body mass index (kg/m2) | 32 | 30.4 | 24.8 | 27.5 | 28 | 26.8 | 27.5 | 31 |
| Hurley grade | III | II | II | II | II | II | II | II |
| Current status of smoking | Yes | No | No | No | No | No | No | Yes |
| Skin type (Fitzpatrick) | III | IV | IV | I-II | IV | IV | IV | I-III |
| Date of the first treatment | April 21 | July 20 | April 21 | November 20 | February 20 | June 20 | January 21 | November 19 |
| Family history | No | No | No | Yes | Yes | Yes | No | Yes |
| No. of affected body sites∗ | 3 | 3 | 1 | 3 | 3 | 4 | 4 | 2 |
| No. of treatments | 5 | 33 | 5 | 19 | 14 | 26 | 8 | 19 |
Affected body sites: axilla, inguinal, genital, breast, gluteal and neck. Example; if both axillas where affected this was numbered as 1 affected body site.
Patients received treatment using mixed-technology CO2 and Ga-As laser (YouLaser MT, Quanta System) and 2 different settings based on the Fitzpatrick skin type (Table II).
Table II.
Settings for mixed-technology CO2 and Ga-As laser based on Fitzpatrick skin type
| Settings | Skin type I-III AFL (10,600 nm) |
Skin type I-III NAFL (1540 nm) |
Skin type IV-VI AFL (10,600 nm) |
Skin type-IV-VI NAFL (1540 nm) |
|---|---|---|---|---|
| Power (W) | 16.0 | 8.0 | 16.0 | 8.0 |
| Pulse width (ms) | 0.5 | 6.0 | 0.25 | 4.0 |
| Energy (mJ) | 8.0 | 48.0 | 4.0 | 32.0 |
AFL, Ablative fractional laser; NAFL, non-ablative fractional laser.
All patients had previously received both topical and at least 1 systemic treatment before the initiation of the treatment with the laser. The most common systemic treatments were adalimumab, tetracycline, acitretin, and metformin.
Discussion
All patients experienced improvement after NAFL + AFL treatment, with a reduction in the number of active lesions, reduced inflammation, and tenderness in treated nodules and less frequent flareups (Figs 1 and 2). In one of our best responders, all treated active inflamed lesions in 5 affected areas resolved after 6 rounds of treatment, also showing a good effect on 1 fistula and scarring. However, thereafter, new lesions occurred and treatment was continued. Two of the patients received >20 treatments. These patients had active disease and experienced the positive effect of laser treatments on new lesions, although other treatment regimens were ineffective.
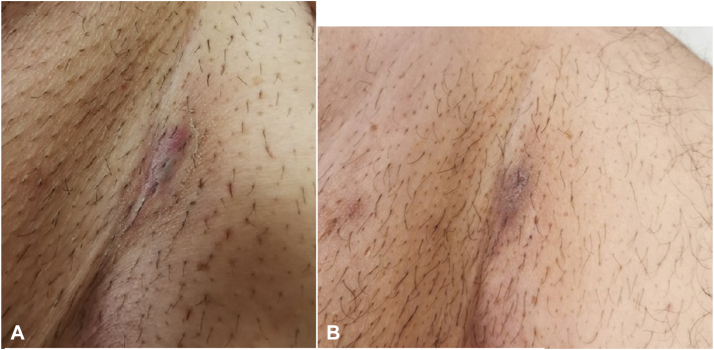
Fig 1.
Inguinal hidradenitis suppurativa lesion (patient 2) (A) just after treatment and (B) 1 week later showing a marked reduction in inflammation.
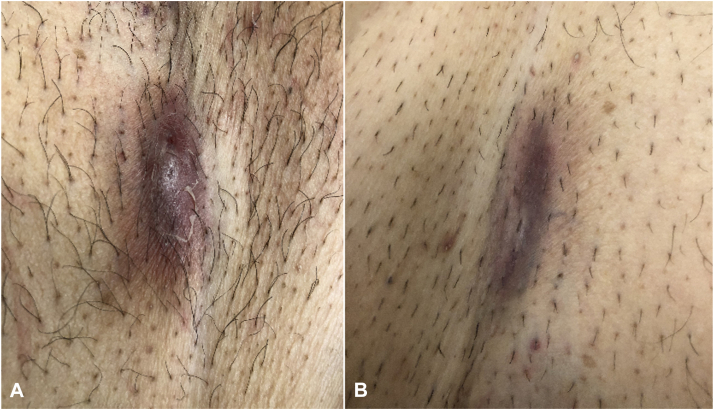
Fig 2.
Inguinal hidradenitis suppurativa lesion (patient 2) (A) before treatment (B) and after 9 treatments.
In accordance with previous studies, the mixed-technology laser (NAFL, AFL) was well tolerated by patients4; a temporary redness and slight burning sensation that lasted for 1 to 2 hours developed in all patients. At follow-up, hyperpigmentation or scarring due to the intervention had not developed in any of the patients.
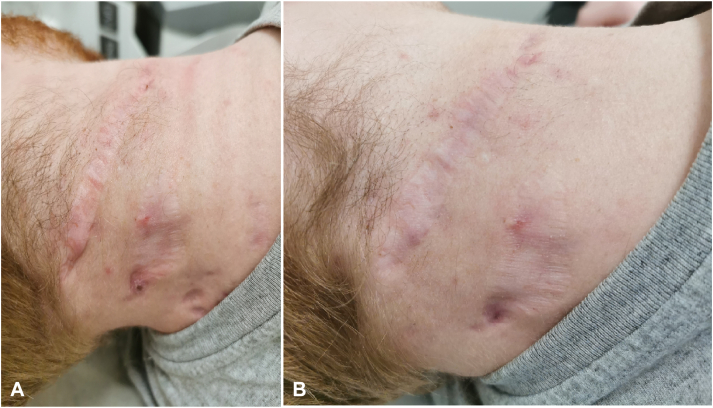
Mechanisms that could explain the positive effects observed with mixed-technology laser treatment are the reduction of follicular inflammation, remodeling of the extracellular matrix, reduction in sebum production, and follicular plugging, as well as possible effects on biofilm formation. Furthermore, AFLs increase the depth of penetration of NAFLs, possibly increasing their therapeutic effect.2 The use of a fractional mode decreases the side effects and shortens the downtime. Another benefit observed in our patient was increased mobility in tissue scarred by the disease, which was a benefit that had also been observed when treating other conditions using only AFLs5 (Fig 3).
Fig 3.
Hidradenitis suppurativa scars in the head and neck area (patient 4) (A) before and (B) after 3 rounds of treatment.
In conclusion, the findings of this case series indicate that the combination of AFLs and NAFLs is a promising treatment for patients with HS. Studies are needed to confirm the effectiveness and safety of this treatment, as well as investigate the mechanisms behind the effects.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Lyons A.B., Townsend S.M., Turk D., Narla S., Baah N., Hamzavi I.H. Laser and light-based treatment modalities for the management of hidradenitis suppurativa. Am J Clin Dermatol. 2020;21(2):237–243. doi: 10.1007/s40257-019-00491-1. [DOI] [PubMed] [Google Scholar]
- 2.Abdel Azim A.A., Salem R.T., Abdelghani R. Combined fractional carbon dioxide laser and long-pulsed neodymium: yttrium-aluminum-garnet (1064 nm) laser in treatment of hidradenitis suppurativa; a prospective randomized intra-individual controlled study. Int J Dermatol. 2018;57(9):1135–1144. doi: 10.1111/ijd.14075. [DOI] [PubMed] [Google Scholar]
- 3.Bogle M.A., Dover J.S., Arndt K.A., Mordon S. Evaluation of the 1,540-nm erbium: glass laser in the treatment of inflammatory facial acne. Dermatol Surg. 2007;33(7):810–817. doi: 10.1111/j.1524-4725.2007.33174.x. [DOI] [PubMed] [Google Scholar]
- 4.Asri E., Widayati R., Malik D. Effectiveness of combined 10,600 nm fractional CO2 and 1540-nm erbium Ga-As laser therapy on acne scar score alteration in patients with atrophic acne scars. Turk J Dermatol. 2019;13(4):126–130. doi: 10.4103/TJD.TJD_25_19. [DOI] [Google Scholar]
- 5.Shumaker P.R., Kwan J.M., Landers J.T., Uebelhoer N.S. Functional improvements in traumatic scars and scar contractures using an ablative fractional laser protocol. J Trauma Acute Care Surg. 2012;73(2 suppl 1):S116–S121. doi: 10.1097/TA.0b013e318260634b. [DOI] [PubMed] [Google Scholar]