Abstract
Aims
Data on the long-term outcomes of STEMI patients treated via a network in Asian countries are very limited. We aimed to evaluate the characteristics and outcomes of STEMI patients at two different periods, before and five years after the establishment of a regional STEMI network in Jakarta, Indonesia.
Methods and results
Out of 6,291 patients with STEMI admitted to hospital between January 2008 to January 2016, we compared the characteristics and outcomes of STEMI patients from two different periods, January 2008 to July 2009 (before instalment of the STEMI network, N=624), and from January 2015 to January 2016 (five years after the start of the network, N=1,052). The PCI hospital is an academic tertiary care cardiac hospital and initiated the regional STEMI network in 2010. Logistic regression was used to determine the adjusted association between treatment in the latter period and mortality. Compared with data from 2008/2009, in the 2015/2016 period, more primary PCI procedures were performed (N=589 [56%] vs. N=176 [28%], p<0.001), fewer patients did not receive reperfusion therapy (37% vs. 59%, p<0.001), and median door-to-device (DTD) times were shorter (82 vs. 94 minutes, p<0.001). Overall in-hospital mortality decreased from 9.6% to 7.1% (adjusted odds ratio 0.72, 95% CI: 0.50 to 1.03, p=0.07).
Conclusions
Half a decade after the implementation of the STEMI network in Jakarta, Indonesia, the result is better and faster care for patients with STEMI and this has been associated with lower in-hospital mortality.
Introduction
Both the European Society of Cardiology (ESC)1 and American Heart Association (AHA)2 guidelines on ST-elevation myocardial infarction (STEMI) emphasise the importance of STEMI networks in order to facilitate a rapid acute reperfusion therapy. Several established STEMI networks have consistently demonstrated that rapid transfer to a PCI centre is effective in reducing the mortality of STEMI patients in the region3,4,5. In contrast with the STEMI networks in developed countries, there are few data reporting the benefit of setting up STEMI networks in developing countries. The Jakarta Cardiovascular Care Unit Network System was set up in 2010 in Jakarta, Indonesia, in order to optimise the care of patients with acute myocardial infarction (AMI) in the region6,7. We compared the characteristics and outcomes of patients with STEMI seen during two time periods, before (2008-2009) and five years after establishment of the regional STEMI network (2015-2016) in a primary percutaneous coronary intervention (PCI) centre that implemented a regional STEMI network in 2010.
Methods
PATIENT POPULATION
A retrospective analysis of the Jakarta Acute Coronary Syndrome (JAC) registry was performed. Data consisted of all STEMI patients admitted to the emergency department of an academic tertiary care cardiac hospital (National Cardiovascular Center Harapan Kita) between January 2008 and January 2016. The hospital provides a 24/7 primary PCI service and it is the largest tertiary academic cardiovascular hospital across the nation, located in the capital city (Jakarta). In 2015, the hospital performed approximately 2,300 PCIs.
The STEMI network (Jakarta Cardiovascular Care Unit Network System) is the first regional STEMI system in the country and is coordinated by the STEMI call centre at the emergency department (ED) of the PCI hospital. The network was established as a multiple hubs system involving many PCI centres in the region and pioneered the development of the national emergency call centre. An ECG transmission system was adopted in the network through several methods of transmission (facsimile, email, WhatsApp or web-based) along with wide application of the pre-hospital triage protocols8,9.
The JAC registry was introduced and has been coordinated by the ED of the hospital since 2007. It is used as the main source of data for measuring the performance of the STEMI network in the region, as well as in the PCI hospitals. All consecutive patients admitted to the ED with an acute coronary syndrome (ACS) were recorded in the database of the registry. Data consist of demographic, clinical characteristics and acute care of the patients. The organisation of the network and registry was created in close collaboration with the local government of Jakarta and the Ministry of Health, Republic of Indonesia.
STUDY SAMPLE
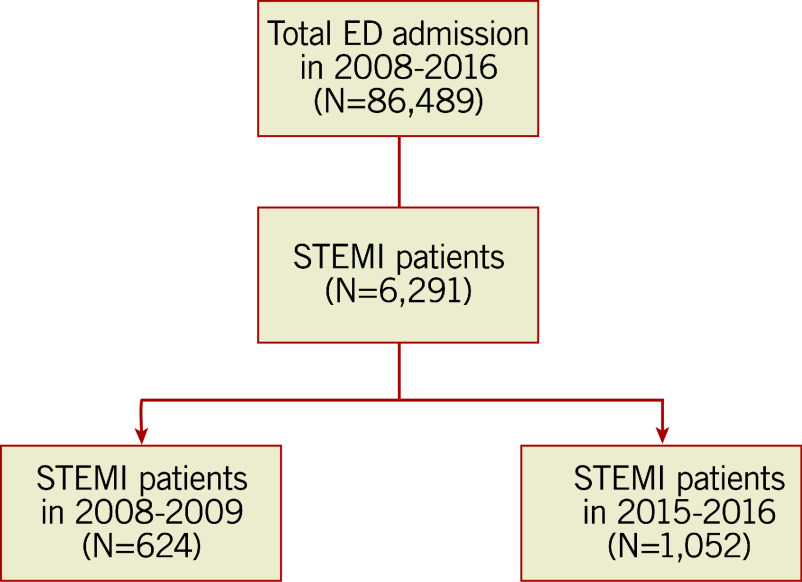
Out of 86,489 patients admitted to the ED of the hospital between January 2008 and January 2016, 6,291 were STEMI patients. The number of STEMI patients admitted between January 2008 and July 2009 was 624 and 1,052 for the period between January 2015 and January 2016 (Figure 1). We compared the characteristics and outcomes of STEMI patients between the two periods.
Figure 1. Study flow chart.
ED: emergency department; STEMI: ST-elevation myocardial infarction
MANAGEMENT PROTOCOL
The treatment protocol for patients with STEMI in the hospital is in accordance with the ESC guidelines on STEMI2. Primary PCI is recommended as the first choice of acute reperfusion therapy. A standardised pre-hospital triage form and check list for possible fibrinolytic therapy were used in the pre-PCI hospital as part of the STEMI network programme7.
Patients with STEMI who underwent primary PCI were pre-treated with 160-320 mg acetylsalicylic acid and 600 mg clopidogrel or ticagrelor 180 mg orally before primary PCI, followed by daily administration of 75 mg clopidogrel or 90 mg of ticagrelor twice daily for six to 12 months and 80-100 mg acetylsalicylic acid indefinitely. Fibrinolytic therapy (streptokinase or alteplase) was given either in the ED of the PCI hospital or in the referring centre. Not all health centres have the ability to perform fibrinolytic therapy. Unfractionated heparin was administered intravenously in the catheterisation laboratory (100 IU/kg) for all patients with STEMI who underwent primary PCI. The use of a glycoprotein IIb/IIIa inhibitor was at the operator’s discretion. PCI of the culprit lesion only was applied in the majority of the primary PCIs.
DATA COLLECTION
Demographic and clinical characteristic data were collected from the JAC registry electronic database. The quality of the registry data is maintained by a monthly evaluation of the data set by the primary investigator of the JAC registry (SD).
STUDY OUTCOME AND DEFINITIONS
The primary outcome of the study was the characteristics of STEMI patients, by means of the proportion of patients receiving acute reperfusion therapy (primary PCI or fibrinolytic therapy) between the two periods. Other outcomes were numbers of patients who did not receive reperfusion therapy, door-to-device time and in-hospital mortality.
The period of 2008-2009 was defined as the period before the STEMI network was introduced, while the period 2015-2016 was categorised as five years after STEMI network introduction.
Diagnosis of STEMI was made based on the presence of ischaemic symptoms and persistent (>20 minutes) ST-segment elevation in at least two contiguous leads, a new left bundle branch block, or a true posterior myocardial infarction confirmed by posterior leads2. Non-reperfused patients were defined as patients who did not receive any acute reperfusion therapy (either primary PCI or fibrinolytic therapy).
The JAC registry was approved by the local institutional review board committee.
STATISTICAL ANALYSIS
We grouped patients into two groups based on time of admission (2008-2009 and 2015-2016). Clinical characteristics, in-hospital mortality and time metrics data were compared between the two groups. Normally distributed continuous variables were expressed as mean±standard deviation or median and quartile range for skewed distribution. Differences between continuous variables were compared with the Student’s t-test or the Mann-Whitney U test. Categorical variables were expressed as percentages, and differences between groups were compared with the chi-square test or Fisher`s exact test as appropriate. Logistic regression analyses were used to examine the association between the time period and incidence of all-cause mortality during hospitalisation. Several baseline characteristics that are listed in Table 1 (symptom onset, time of admission, gender, location of MI) were considered as potential confounders for the in-hospital mortality and were included in the analysis.
Table 1. Characteristics of STEMI patients between the two periods (N=1,676).
| Year 2008/2009 (N=624) | Year 2015/2016 (N=1,052) | p-value | |
|---|---|---|---|
| Age, years | 55.59±10.36 | 55.71±10.23 | 0.76 |
| Age >65 years, n (%) | 104 (16.6%) | 169 (16%) | 0.74 |
| Male, n (%) | 532 (85%) | 895 (85%) | 0.92 |
| Off-hours admission, n (%) | 466 (74%) | 820 (78%) | 0.12 |
| Anterior MI, n (%) | 377 (60%) | 579 (55%) | 0.03 |
|
Symptom onset >12 hrs, n (%) |
232 (37%) | 306 (29%) | <0.01 |
| CAD risk factors, n (%) | |||
| Smoker | 414 (66%) | 660 (63%) | 0.13 |
| Hypertension | 334 (53%) | 560 (53%) | 0.90 |
| Diabetes mellitus | 190 (30%) | 282 (27%) | 0.10 |
| Dyslipidaemia | 297 (47%) | 315 (30%) | <0.001 |
| Family history | 162 (26%) | 172 (16%) | <0.001 |
| Source of referral, n (%) | |||
| Inter-hospital referral | 343 (55%) | 715 (68%) | <0.001 |
| Killip class 2 to 4, n (%) | 204 (32%) | 317 (30%) | 0.27 |
| TIMI risk score >4, n (%) | 238 (38%) | 436 (41%) | 0.18 |
| Dual antiplatelet therapy within 24 hrs, n (%) | |||
| Salicylic acid | 589 (94%) | 1,038 (98%) | <0.01 |
| Clopidogrel | 594 (95%) | 1,014 (96%) | 0.23 |
| Acute reperfusion therapy, n (%) | |||
| Primary PCI | 176 (28%) | 589 (56%) | <0.001 |
| Fibrinolytic therapy | 75 (12%) | 69 (6.5%) | <0.001 |
|
Non-reperfusion therapy, n (%) |
373 (59%) | 389 (37%) | <0.001 |
| Time metrics evaluation, minutes | |||
| Door-to-device time | 94 (72-122) | 82 (67-103) | <0.001 |
| In-hospital mortality, n (%) | 60 (9.6%) | 75 (7.1%) | 0.07 |
| CAD: coronary artery disease; MI: myocardial infarction; PCI: percutaneous coronary intervention; TIMI: Thrombolysis In Myocardial Infarction | |||
All statistical tests were two-tailed and a p-value <0.05 was considered significant. Statistical analyses were performed with SPSS for Windows, Version 17.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 1,676 patients with STEMI were included in the final analysis, consisting of 624 patients admitted during 2008-2009 and 1,052 patients admitted during 2015-2016.
Compared with the recent year (2015-2016), patients who were admitted during 2008-2009 had more anterior MI, dyslipidaemia and family history of coronary artery disease. Late onset STEMI patients (symptom onset >12 hrs) were found less frequently in the recent year (37% vs. 29%). The majority of STEMI patients were admitted through a transfer process (inter-hospital transfer) (Table 1). Most of the patients received salicylic acid and clopidogrel within the first 24 hrs after admission (Table 1).
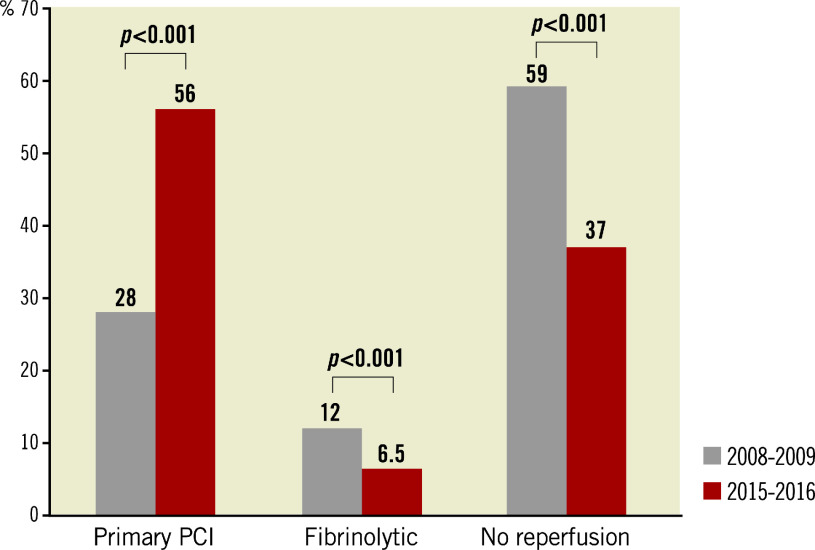
Compared with data from 2008-2009, STEMI patients who were admitted in 2015-2016 had more primary PCI procedures (N=588 [56%] vs. N=176 [28%], p<0.001) and there were fewer patients who did not receive reperfusion therapy (37% vs. 59%, p<0.001). Use of fibrinolytic therapy was lower during the recent time period (6.5% vs. 12%, p<0.001) (Table 1, Figure 2).
Figure 2. The characteristics of acute reperfusion therapy between the two periods.
PCI: percutaneous coronary intervention
The median door-to-device (DTD) time was significantly shorter during the recent time period (82 vs. 94 minutes, p<0.001) (Table 1).
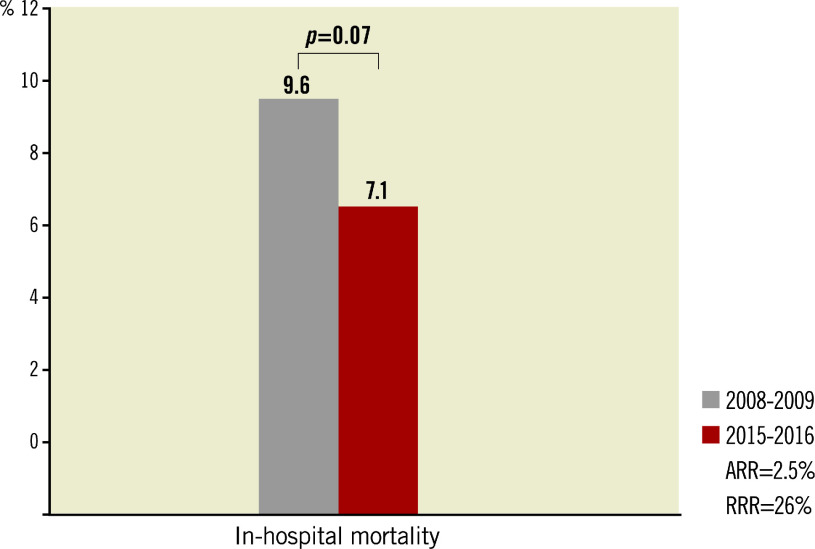
The overall in-hospital mortality of STEMI patients was lower in the recent year (7.1% vs. 9.6%; unadjusted odds ratio [OR] 0.72, 95% confidence interval [CI]: 0.50 to 1.02, p=0.07) (Table 2, Figure 3). After adjustment of several variables, the OR was 0.72, 95% CI: 0.50 to 1.03, p=0.07 (Table 3).
Table 2. Bivariate analysis of in-hospital mortality.
| Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| Year 2015/2016 | 0.72 | 0.50-1.02 | 0.07 |
Figure 3. In-hospital mortality.
ARR: absolute risk reduction; RRR: relative risk reduction
Table 3. Multivariate analysis of in-hospital mortality of STEMI patients.
| Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| Year 2015/2016 | 0.72 | 0.50-1.03 | 0.07 |
| Symptom onset >12 hrs | 1.08 | 0.74-1.58 | 0.66 |
| Off-hours admission | 1.42 | 0.90-2.24 | 0.12 |
| Female | 1.63 | 1.05-2.51 | 0.02 |
| Anterior MI | 1.15 | 0.80-1.66 | 0.44 |
Discussion
This study shows that, five years after the introduction of a STEMI network, more patients underwent primary PCI, fewer patients did not get reperfusion therapy, and DTD times were shorter, resulting in a numerically lower in-hospital mortality compared with the period before initiation of the STEMI network.
The benefits of regional STEMI networks have been described in many developed countries3,4,5. In Jakarta, Indonesia, the STEMI network was initiated in 2010 with the goal of offering reperfusion therapy to all STEMI patients in the metropolitan area6,7,8,9. This study suggests that it took several years to obtain a significant improvement in the processes of care for STEMI within the network. Furthermore, the results of the present study indicate that there was a shift in choice of reperfusion therapy from 2008 to 2015, whereby primary PCI has markedly increased and the use of fibrinolysis therapy has declined (Figure 2).
It was also observed that the proportion of late STEMI presenters (symptom onset >12 hrs) has dropped significantly (29% vs. 37%, p<0.01). These results suggest that the pre-hospital time delay has improved recently. The awareness of the population of the importance of early treatment might have improved since more patients were coming to a health centre to seek help early after onset of symptoms. In addition, better knowledge of the benefits of reperfusion therapy by the primary physicians (mostly general practitioners) has probably played a significant role as well, as suggested by the higher numbers of STEMI patients transferred to the PCI hospital.
In spite of the progress made over recent years, the Jakarta STEMI network is still facing many serious challenges. City traffic during day time often results in huge delays, many PCI centres in Jakarta do not provide a 24/7 primary PCI service and the number of catheterisation labs and interventional cardiologists is low when compared with Western countries.
In order to select the best reperfusion strategy for a particular patient, collaboration among primary physicians, the emergency ambulance service, the STEMI call centre and the interventional cardiologists all working with a commonly agreed protocol is needed. When timely primary PCI is not possible, e.g., because the ambulance is stuck in a traffic jam, a pharmaco-invasive strategy as studied in the STREAM trial10,11 and in many registries may need to be developed in the near future.
TIME DELAYS IN THE PCI HOSPITAL
It is often difficult to achieve a DTD time <90 minutes in all primary PCI cases, as recommended by both the ESC and AHA guidelines12,13. The DTD time in our hospital has improved in recent years (median 94 vs. median 82 minutes, p<0.001). This means that the flow of STEMI patients in the hospital has improved starting from admission to the ED and transferring the patient to the catheterisation laboratory. The improvement is due to the centralisation of all administration processes in the ED, an increase in the number of interventional cardiologists in the hospital, and the presence of on-site cardiologists and nurses in the catheterisation laboratory 24/7. Similar to the USA14, the key indicator used by the Ministry of Health Republic of Indonesia to evaluate the performance of our hospital as the national cardiovascular centre is that a DTD time ≤90 minutes should be achieved in more than 80% of primary PCI. However, delays in reperfusion therapy are more often due to suboptimal pre-hospital care15. Therefore, improving STEMI care in the referring hospitals is critically important. This should include informing and training of GPs and nurses in the use of a common protocol. This training programme has been carried out routinely in our ED and was initiated in close collaboration with the local government.
IN-HOSPITAL MORTALITY
The in-hospital mortality of patients with STEMI has been lower in recent years (7.1% vs. 9.6%, p=0.07) (Figure 3). This absolute difference was borderline significant and corresponds with a 26% relative reduction of in-hospital mortality since the initiation of the network. After adjustment for several clinical variables, the odds ratio remained unchanged (OR 0.72; p=0.07). The mortality reduction achieved in recent years is the result of more patients getting reperfusion therapy, higher numbers of primary PCI and shorter DTD time.
In order to make further progress, education of GPs and nurses who are working in the referring centres focusing on all aspects of pre-PCI care is critically important.
The pre-hospital triage form should also be used in the ambulance setting along with improvement of the ambulance navigation system. PCI centre performance can be improved by sending patients directly to the catheterisation laboratory (bypassing the ED). Furthermore, a public promotion campaign to encourage the population to dial the emergency medical service number (1-1-9) in case of chest pain may be helpful as well. A public campaign has been associated with an improved system of care of AMI16.
Finally, the JAC registry (www.jacregistry.pjnhk.go.id) which is currently the main source of data to evaluate the performance of the STEMI network in the region should be used and updated on a regular basis.
Study limitations
We have limited data on the details of the fibrinolytic therapy that was given in the pre-PCI centres, or the number of patients with a pharmaco-invasive strategy. Furthermore, the results of the present analysis cannot be generalised to other hospitals in the region due to differences in the numbers of catheterisation laboratories and those that do not provide a 24/7 primary PCI service.
Conclusions
Half a decade after the implementation of the STEMI network in Jakarta, Indonesia, the result is better and faster care of patients with STEMI and this has been associated with lower in-hospital mortality.
Impact on daily practice
The results of this study will increase the awareness of treating patients with STEMI in the region and may encourage other developing countries in Asia to carry out routine performance measures of their STEMI networks in order to give insights into improving patient care.
Acknowledgments
Acknowledgements
The critical revision of the manuscript by Dr Frans Van de Werf is greatly appreciated.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Abbreviations
- AHA
American Heart Association
- AMI
acute myocardial infarction
- CI
confidence interval
- DTD
door-to-device
- ED
emergency department
- ECG
electrocardiography
- ESC
European Society of Cardiology
- GP
general practitioners
- IU
international unit
- JAC
Jakarta Acute Coronary Syndrome
- MI
myocardial infarction
- OR
odds ratio
- PCI
percutaneous coronary intervention
- STEMI
ST-segment elevation myocardial infarction
Contributor Information
Surya Dharma, Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Indonesia, Indonesian Cardiovascular Research Center, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Hananto Andriantoro, Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Indonesia, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Iwan Dakota, Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Indonesia, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Isman Firdaus, Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Indonesia, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Siska Suridanda Danny, Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Indonesia, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Dian Zamroni, Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Indonesia, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Bambang Budi Siswanto, Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Indonesia, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia.
Sunil V. Rao, The Duke Clinical Research Institute, Durham, NC, USA.
References
- O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso JE, Tracy CM, Woo YJ, Zhao DX CF/AHA Task Force. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:529–55. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- Kalla K, Christ G, Karnik R, Malzer R, Norman G, Prachar H, Schreiber W, Unger G, Glogar HD, Kaff A, Laggner AN, Maurer G, Mlczoch J, Slany J, Weber HS, Huber K Vienna STEMI Registry Group. Implementation of guidelines improves the standard of care: the Viennese registry on reperfusion strategies in ST-elevation myocardial infarction (Vienna STEMI registry). Circulation. 2006;113:2398–405. doi: 10.1161/CIRCULATIONAHA.105.586198. [DOI] [PubMed] [Google Scholar]
- Danchin N, Puymirat E, Steg PG, Goldstein P, Schiele F, Belle L, Cottin Y, Fajadet J, Khalife K, Coste P, Ferrières J, Simon T FAST-MI 2005 Investigators. Five-year survival in patients with ST-segment-elevation myocardial infarction according to modalities of reperfusion therapy: the French Registry on Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) 2005 Cohort. Circulation. 2014;129:1629–36. doi: 10.1161/CIRCULATIONAHA.113.005874. [DOI] [PubMed] [Google Scholar]
- Peterson ED, Roe MT, Rumsfeld JS, Shaw RE, Brindis RG, Fonarow GC, Cannon CP. A call to ACTION (Acute Coronary Treatment and Intervention Outcomes Network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:491–9. doi: 10.1161/CIRCOUTCOMES.108.847145. [DOI] [PubMed] [Google Scholar]
- Dharma S, Juzar DA, Firdaus I, Soerianata S, Wardeh AJ, Jukema JW. Acute myocardial infarction system of care in the third world. Neth Heart J. 2012;20:254–9. doi: 10.1007/s12471-012-0259-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharma S, Siswanto BB, Firdaus I, Dakota I, Andriantoro H, Wardeh AJ, van der, Jukema JW. Temporal Trends of System of Care for STEMI: Insights from the Jakarta Cardiovascular Care Unit Network System. PLoS One. 2014;9:e86665. doi: 10.1371/journal.pone.0086665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharma S, Andriantoro H, Dakota I, Purnawan I, Pratama V, Isnanijah H, Yamin M, Bagus T, Hartono B, Ratnaningsih E, Suling F, Basalamah MA. Organization of reperfusion therapy for STEMI in a developing country. Open Heart. 2015;2:e000240. doi: 10.1136/openhrt-2015-000240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharma S, Andriantoro H, Purnawan I, Dakota I, Basalamah F, Hartono B, Rasmin R, Isnanijah H, Yamin M, Wijaya IP, Pratama V, Gunarto TB, Juwana YB, Suling FR, Witjaksono AM, Lasanudin HF, Iskandarsyah K, Priatna H, Tedjasukmana P, Wahyumandradi U, Kosasih A, Budhiarti IA, Pribadi W, Wirianta J, Lubiantoro U, Pramesti R, Widowati DR, Aminda SK, Basalamah MA, Rao SV. Characteristics, treatment and in-hospital outcomes of patients with STEMI in a metropolitan area of a developing country: an initial report of the extended Jakarta Acute Coronary Syndrome Registry. BMJ Open. 2016;6:e012193. doi: 10.1136/bmjopen-2016-012193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Danays T, Lambert Y, Sulimov V, Rosell Ortiz, Ostojic M, Welsh RC, Carvalho AC, Nanas J, Arntz HR, Halvorsen S, Huber K, Grajek S, Fresco C, Bluhmki E, Regelin A, Vandenberghe K, Bogaerts K, Van de STREAM Investigative Team. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2013;368:1379–87. doi: 10.1056/NEJMoa1301092. [DOI] [PubMed] [Google Scholar]
- Sinnaeve PR, Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Lambert Y, Danays T, Soulat L, Halvorsen S, Ortiz FR, Vandenberghe K, Regelin A, Bluhmki E, Bogaerts K, Van de STREAM investigators. ST-segment-elevation myocardial infarction patients randomized to a pharmaco-invasive strategy or primary percutaneous coronary intervention: Strategic Reperfusion Early After Myocardial Infarction (STREAM) 1-year mortality follow-up. Circulation. 2014;130:1139–45. doi: 10.1161/CIRCULATIONAHA.114.009570. [DOI] [PubMed] [Google Scholar]
- Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW, Curtis JP. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124:1038–45. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen SD, Laut KG, Fajadet J, Kaifoszova Z, Kala P, Di Mario, Wijns W, Clemmensen P, Agladze V, Antoniades L, Alhabib KF, De Boer, Claeys MJ, Deleanu D, Dudek D, Erglis A, Gilard M, Goktekin O, Guagliumi G, Gudnason T, Hansen KW, Huber K, James S, Janota T, Jennings S, Kajander O, Kanakakis J, Karamfiloff KK, Kedev S, Kornowski R, Ludman PF, Merkely B, Milicic D, Najafov R, Nicolini FA, Noč M, Ostojic M, Pereira H, Radovanovic D, Sabaté M, Sobhy M, Sokolov M, Studencan M, Terzic I, Wahler S, Widimsky P European Association for Percutaneous Cardiovascular Interventions. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: current status in 37 ESC countries. Eur Heart J. 2014;35:1957–70. doi: 10.1093/eurheartj/eht529. [DOI] [PubMed] [Google Scholar]
- Krumholz HM, Bradley EH, Nallamothu BK, Ting HH, Batchelor WB, Kline-Rogers E, Stern AF, Byrd JR, Brush JE. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008;1:97–104. doi: 10.1016/j.jcin.2007.10.006. [DOI] [PubMed] [Google Scholar]
- Miedema MD, Newell MC, Duval S, Garberich RF, Handran CB, Larson DM, Mulder S, Wang YL, Lips DL, Henry TD. Causes of delay and associated mortality in patients transferred with ST-segment-elevation myocardial infarction. Circulation. 2011;124:1636–44. doi: 10.1161/CIRCULATIONAHA.111.033118. [DOI] [PubMed] [Google Scholar]
- Regueiro A, Rosas A, Kaifoszova Z, Faixedas MT, Curos A, Tresserras R, Sabaté M. Impact of the “ACT NOW. SAVE A LIFE” public awareness campaign on the performance of a European STEMI network. Int J Cardiol. 2015;197:110–2. doi: 10.1016/j.ijcard.2015.06.040. [DOI] [PubMed] [Google Scholar]