Abstract
Objectives
The aim of this study was to compare the effectiveness of conventional physical therapy (transcutaneous electrical nerve stimulation, hot pack, and therapeutic ultrasound) and extracorporeal shock wave therapy (ESWT) on pain, disability, functional status, and depression in patients with chronic low back pain (LBP).
Patients and methods
Ninety-one patients with chronic LBP were included in the study and randomized to groups that received ESWT or conventional physiotherapy; of these, 70 completed the study (37 males, 33 females; mean age: 46.4±13.3 years; range, 18 to 65 years). Outcome measures included the Visual Analog Scale, the pressure pain algometer, Oswestry Disability Index (ODI), Health Assessment Questionnaire (HAQ), fingertip-to-floor distance, and the Beck Depression Inventory. The assessments were made before treatment and at the first and 12th weeks after treatment.
Results
Extracorporeal shock wave therapy was more effective than conventional physical therapy in terms of Visual Analog Scale scores, the pressure algometer, ODI, HAQ, and fingertip-to-floor distance at the first and 12th week.
Conclusion
Extracorporeal shock wave therapy is superior to conventional physical therapy in terms of improving pain, spinal mobility, and functional status in patients with chronic LBP.
Introduction
Low back pain (LBP) is a common health problem around the world regardless of development level and a leading cause of morbidity.[1] The financial burden is also high due to both diagnosis and treatment costs and the resulting loss of productivity and physical disabilities.[2] The lifetime prevalence is reported to be as high as 84%.[2] Chronic LBP develops in approximately one-quarter of patients with LBP, and the rate of disability caused by LBP has been reported as 11 to 12%.[2]
Back pain lasting longer than three months is defined as chronic LBP.[3] It is sometimes associated with a precise etiology, such as radiculopathy or spinal stenosis, but most cases of LBP do not have a specific cause. This condition is classified as nonspecific LBP and constitutes at least 90% of those experiencing spinal pain; its diagnosis is based on the exclusion of other specific causes.[4-6]
Although the effect of physical therapy modalities in reducing pain is controversial, there are results showing that it is more successful than placebo.[7] The effectiveness of transcutaneous electrical nerve stimulation (TENS), which is one of the physical therapy agents, is controversial in acute pain, and it has been reported that TENS has short-term positive effects in chronic pain in randomized controlled studies conducted to compare TENS with placebo. It has been suggested that TENS exerts this effect through the gate-control mechanism.[7-9] In addition, it has been reported that hot pack application provides short-term relief in LBP.[10] Therapeutic ultrasound is effective in pain, some parameters of quality of life (QoL), functional performance, and depression in patients with chronic LBP.[11-13]
Extracorporeal shock wave therapy (ESWT) is a noninvasive method that uses single pulsed acoustic waves produced outside the body and focused on a specific area of the body. Studies have shown that ESWT is an effective and long-term pain-relieving method in soft tissue diseases, such as plantar fasciitis and Achilles tendinopathy.[14,15] Shockwaves stimulate axonal regeneration of peripheral nerves by various molecular reactions. Extracorporeal shock wave therapy induces analgesia through biochemical changes in the nerve fiber itself and reduces the inflammation of soft tissues.[14,15] Additionally, it has been stated that ESWT supports revascularization and stimulates or reactivates the healing process of connective tissues, including tendons and bones, thus reducing pain and improving function.[16] Few studies have been conducted with small patient numbers investigating the effects of ESWT on chronic LBP. Among these studies, no study has made evaluations using a pressure algometer or spinal mobility, which provide more objective data. In addition, although ESWT has been shown to be effective in LBP and conventional physiotherapy methods consisting of TENS, hot packs, and therapeutic ultrasound are frequently used for low back pain, the number of studies comparing these two treatment methods is also very few.[16-19] This study aimed to compare the effectiveness of conventional physical therapy (CPT) and ESWT on pain, disability, spinal mobility, functional status, and depression in patients with chronic LBP.
Patients and Methods
A total of 110 patients diagnosed with chronic nonspecific LBP in the Kırşehir Ahi Evran University Faculty of Medicine, Department of Physical Medicine and Rehabilitation between January 2019 and April 2019 were evaluated to be enrolled in the prospective, randomized controlled, open-label study. Ninety-one patients who met the inclusion criteria were randomized into two groups (the ESWT group and the CPT group) using the closed envelope method. The inclusion criteria were as follows: nonspecific, nonradicular (axial) chronic LBP diagnosis (LBP for at least three months), a Visual Analog Scale (VAS) score of 5 or higher, and sufficient cooperation. The exclusion criteria were determined as specific LBP (presence of a specific cause, such as radiculopathy, spinal stenosis, or infection),[4] radicular pain, surgical history in the lumbar spine area, vertebral compression fracture, spinal tumors, intervertebral disc infections, inflammatory rheumatic diseases, pregnancy, heart disease, and structural abnormalities in the lumbar region. The patients' age, sex, educational status, height-weight, body mass index (BMI), medications, whether there was any concomitant disease, and the duration of the symptoms were recorded.
Transcutaneous electrical nerve stimulation (in conventional mode, to the paravertebral region for 20 min), hot pack (20 min), ultrasound (in continuous mode, to paravertebral muscles, 1.5 w/cm2 , 5 min), and 10 sessions of CPT were given to the CPT group (n=44). Radial ESWT therapy was given to the ESWT group (n=47). Lumbar stretching, range of motion (ROM) exercises, and lumbar and abdominal strengthening exercises were given to all patients as an exercise program. The patients were provided a brochure containing schematic information regarding the exercises. The exercise program was practically demonstrated by the same physiotherapist during the first session of the treatment. Exercises were performed twice a day.
The ESWT group was given two sessions per week, a total of five sessions of ESWT, ending in two to three weeks. It was ensured that there were at least two days between each session. Two patients in the ESWT group did not want to continue the treatment after the first session due to pain. The ESWT probe was applied by placing the metallic head of the device perpendicular to the pain areas after applying the joining gel to facilitate the passage of the pressure waves through the skin. Consistent with the study of Walewicz et al.,[18] ESWT was applied to the areas that the patient reported as the most painful at the lumbar and sacral spine level. During the session, the patient was in a prone position. Extracorporeal shock wave therapy was performed using an Modus ESWT Touch Shock Waves device (Inceler Medical, Ankara, Türkiye) with a 20-mm applicator, a pressure of 2.8 bar, and a frequency of 10 Hz with 2600 shots. ESWT, CPT, and exercise training were performed by the same physiotherapist. There was no blinding in the study.
The VAS[20] and a pressure algometer[21] were utilized to evaluate the pain levels of the patients at pre-treatment and 1 and 12 weeks after treatment. Visual Analog Scale scores were evaluated over 100 mm. The pressure pain threshold (PPT) was measured from the forehead and lumbar region using a pressure algometer (Algometer Commander, JTECH Medical, Salt Lake City, UT, USA). In accordance with the literature, the following six bilateral points were selected: (i) quadratus lumborum muscle, 5 cm lateral to the L3 vertebra; (ii) paravertebral muscles (M. longissimus/M. Erector trunci), 3 cm lateral to the L1 vertebra; (iii) os ilium, the highest point on crista iliaca; (iv) iliolumbar ligament, middle of the triangle given by processus costarius of lumbar vertebra L4 and L5 as well as crista iliaca; (v) piriformis muscle, the intersection of the two lines from spina iliaca anterior superior to the coccyx and from the trochanter major to the spina iliaca posterior superior, representing the normal position of the piriformis muscle, which could partly be overlaid by the M. gluteus medius; (vi) greater trochanter, posterior to the trochanteric prominence (the forehead midpoint was taken as a reference point, and PPT value was measured).[21]
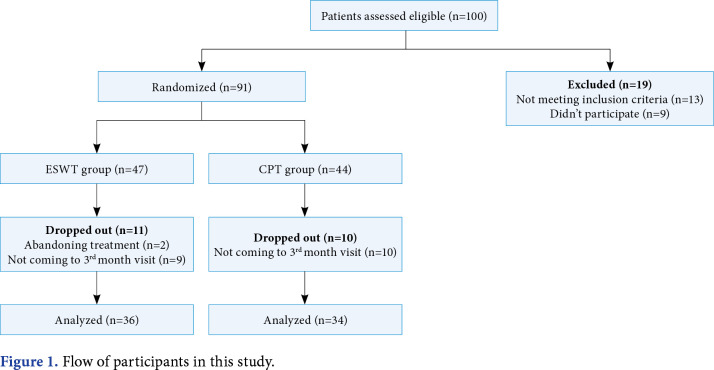
Disability was evaluated using the Oswestry Disability Index (ODI)[22] and the Health Assessment Questionnaire (HAQ).[23] Depression was assessed using the Beck Depression Inventory (BDI) developed by Beck et al.[24] Turkish validity and reliability of all these scales have been demonstrated.[25-27] The fingertip-to-floor distance (FTFD) was measured and recorded to evaluate spinal mobility. The FTFD assesses hip and spine mobility. Higher results indicate worse lumbar and hip mobility.[28] These evaluations were performed by a single physician before treatment and at the first and 12th weeks after treatment. In addition to the two patients in the ESWT group who did not want to continue the treatment after the first session, nine patients in the ESWT group and 10 patients in the CPT group did not attend the third-month follow-up. As a result, 70 patients (37 males, 33 females; mean age: 46.4±13.3 years; range, 18 to 65 years) were included in the final analysis, with 36 patients and 34 patients in the ESWT group and the CPT group, respectively (Figure 1).
Figure 1. Flow of participants in this study.
Statistical analysis
The power analysis was done using PASS 11 (NCSS, LLC. Kaysville, UT, USA) per the method of Hintze. Minimum group sample sizes of 29 and 29 were determined by a two-sided two-sample t-test power analysis with 80% power level and 5% alpha error level (Effect size Cohen's d=0.758; based on the study of Han et al.[17]). The patients were included in the study, considering that there would be dropouts from the study.
The data were analyzed by the IBM SPSS version 20.0 software (IBM Corp, Armonk, NY, USA). Frequency and percentage were preferred for displaying categorical data, and the mean ± standard deviation, median, and min-max were preferred for displaying continuous data. The compatibility of the data to normal distribution was tested using the Shapiro-Wilk test. The chi-square test was used for the comparison of categorical data. The MannWhitney U test was used in the comparison of means according to the compliance with normal distribution. In the analysis of repeated measures, the Friedman test was used according to the compliance with normal distribution. Pairwise comparisons were performed with the Bonferroni correction method. In addition, between-group comparisons of repeated measurements were performed by analyzing the differences between measurements with the Mann-Whitney U test. A p value of <0.05 was accepted as statistically significant.
Results
The ESWT group was found to be statistically similar to the CPT group in terms of age, sex, educational status, BMI, and disease duration (Table 1). Significant improvement was found in VAS, HAQ, ODI, FTFD, total PPT, and BDI scores in the ESWT group at the first and 12th weeks after the treatment compared to pre-treatment. In the CPT group, only the VAS, ODI, and BDI scores improved at the first and 12th weeks compared to pre-treatment (Table 2). Initially, there was no difference between the VAS, HAQ, ODI, total PPT, and BDI scores of the two groups; however, the ESWT group had significantly lower scores in terms of VAS, HAQ, ODI at the first and 12th weeks and in terms of BDI at the 12th week compared to the CPT group (Figures 2, 3 and 4). The ESWT group had significantly higher scores in terms of total PPT at the first and 12th weeks. There were significantly higher FTFD scores in the ESWT group before the treatment, whereas there was no significant difference between the two groups at one and 12 weeks.
Table 1. General characteristics of the participants.
| ESWT group (n=36) | CPT group (n=34) | p | |||||
| n | % | Mean±SD | n | % | Mean±SD | ||
| Age (year) | 47.4±14.3 | 45.3±12.2 | 0.375† | ||||
| Sex | |||||||
| Male | 23 | 63.9 | 14 | 41.2 | 0.057‡ | ||
| Female | 13 | 36.1 | 20 | 58.8 | |||
| Education status | |||||||
| Primary school graduate | 14 | 38.9 | 19 | 55.9 | 0.356‡ | ||
| High school graduate | 11 | 30.6 | 7 | 20.6 | |||
| Graduated from a university | 11 | 30.6 | 8 | 23.5 | |||
| Body mass index (kg/m2) | 28.6±4.9 | 35.2±36.2 | 0.617† | ||||
| Duration of illness (month) | 80.2±85.1 | 60.4±42.5 | 0.972† | ||||
| ESWT: Extracorporeal shock wave therapy, CPT: Conventional physical therapy; SD: Standard deviation; † Statistical comparison of measurements between groups with the Mann-Whitney U test; ‡ Statistical comparison of measurements between groups with the chi- square test. | |||||||
Table 2. Visual Analog Scale, HAQ, ODI, FTFD, total PPT, and BDI scores of the patients in the ESWT and CPT groups.
| ESWT group | CPT group | p | |||||
| Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | ||
| VAS score | |||||||
| Pre-treatment | 65.8±15.7 | 70a* | 20-90 | 61.9±14.9 | 60a* | 30-100 | 0.215† |
| 1st week | 31.1±19.8 | 30b* | 0-65 | 47.5±18.9 | 50b* | 10-70 | 0.001† |
| 12th weeks | 28.1±18.6 | 25b* | 0-60 | 47.7±18.5 | 50b* | 10-80 | 0.001† |
| P in repeated measurements | 0.001‡ | 0.001‡ | |||||
| HAQ score | |||||||
| Pre-treatment | 9.3±7.6 | 8a* | 0-26 | 9.5±6.5 | 9.5a* | 0-31 | 0.702† |
| 1st week | 5.3±6.4 | 3.5b* | 0-32 | 8.4±6.6 | 7a* | 0-25 | 0.018† |
| 12th weeks | 4.0±6.3 | 1.5b* | 0-30 | 9.7±7.5 | 8.5a* | 0-29 | 0.001† |
| P in repeated measurements | 0.001‡ | 0.655‡ | |||||
| ODI score | |||||||
| Pre-treatment | 20.8±10.5 | 20a* | 5-41 | 22.4±7.8 | 22a* | 8-43 | 0.466† |
| 1st week | 11.0±9.8 | 8b* | 0-34 | 19.2±8.3 | 20a,b* | 0-33 | 0.001† |
| 12th weeks | 9.7±7.8 | 7b* | 0-32 | 19.7±9.1 | 19.50b* | 2-34 | 0.001† |
| P in repeated measurements | 0.001‡ | 0.018‡ | |||||
| FTFD | |||||||
| Pre-treatment | 8.8±8.4 | 7.5a* | 0-32 | 6.1±10.8 | 0a* | 0-40 | 0.038† |
| 1st week | 5.9±7.3 | 3.5b* | 0-30 | 4.7±9.5 | 0a* | 0-44 | 0.100† |
| 12th weeks | 5.0±6.5 | 2b* | 0-28 | 4.9±10.8 | 0a* | 0-51.9 | 0.093† |
| P in repeated measurements | 0.001‡ | 0.278‡ | |||||
| TPPT | |||||||
| Pre-treatment | 328.2±164.3 | 350.3a* | 83-667.1 | 365.9±162.0 | 400.2a* | 82.4-664 | 0.312† |
| 1st week | 489.0±169.7 | 494.3b* | 189-878.2 | 375.1±169.7 | 379.3a* | 118.6-855.9 | 0.006† |
| 12th weeks | 455.8±147.2 | 445.2b* | 228.3-795 | 338.1±147.1 | 336.4a* | 99.8-708.8 | 0.002† |
| P in repeated measurements | 0.001‡ | 0.539‡ | |||||
| BDI score | |||||||
| Pre-treatment | 10.3±8.0 | 8.5a* | 0-28 | 12.9±9.0 | 10a* | 0-33 | 0.251† |
| 1st week | 6.5±7.8 | 4.5b* | 0-34 | 7.2±8.6 | 5.5b* | 21-30 | 0.282† |
| 12th weeks | 4.9±6.9 | 2b* | 0-33 | 8.9±9.7 | 6b* | 17-34 | 0.008† |
| P in repeated measurements | 0.001‡ | 0.001‡ | |||||
| HAQ: Health Assessment Questionnaire; ODI: Oswestry Disability Index; FTFD: Fingertip-to-floor distance; PPT: Pressure pain threshold; BDI: Beck Depression Inventory; ESWT: Extracorporeal shock wave therapy; CPT: Con-ventional physical therapy; SD: Standard deviation; VAS: Visual analog skala; TPPT: Total pressure pain threshold; † Statistical comparison of measurements between groups with the Mann-Whitney U test; ‡ Statistical comparison of repeated measurements within groups with the Friedman test; In repeated measurements within the group (statistical comparison of values pre-treatment, 1st first week, and 12th week), the same letters (a and b) indicate that there is no statistically significant difference according to pairwise comparisons with the Bonferroni correction method. | |||||||
Figure 2. Comparison of the VAS scores between groups. VAS: Visual Analog Scale; ESWT: Extracorporeal shock wave therapy; CPT: Conventional physical therapy.
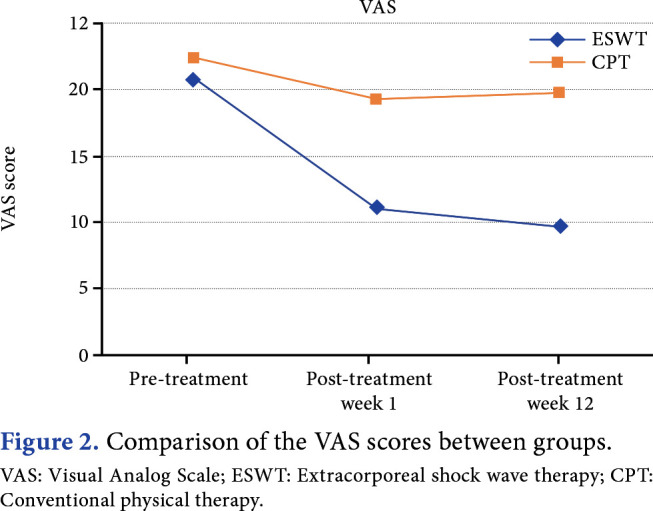
Figure 3. Comparison of total PPT scores between groups. TPPT: Total pressure pain threshold; ESWT: Extracorporeal shock wave therapy; CPT: Conventional physical therapy.
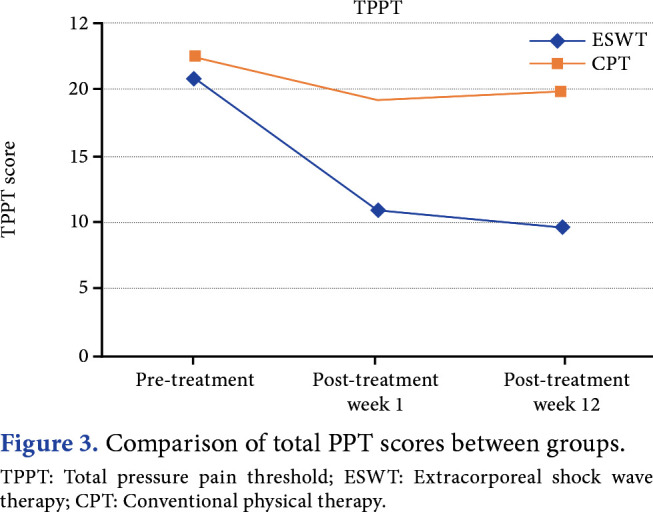
Figure 4. Comparison of the ODI scores between groups. ODI: Oswestry Disability Index; ESWT: Extracorporeal shock wave therapy; CPT: Conventional physical therapy.
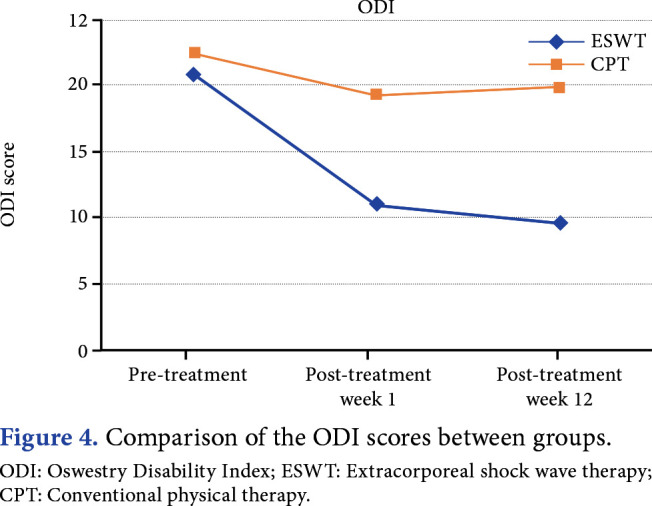
Decreases in the VAS score, HAQ score, ODI score, and FTFD were significantly higher in the ESWT group than in the CPT group after one and 12 weeks. The increase in total PPT was significantly higher in the ESWT group than in the CPT group both after one and 12 weeks. We found no significant difference between the groups in terms of change in BDI scores after one and 12 weeks (Table 3).
Table 3. Changes in VAS, HAQ, ODI, FTFD, total PPT, and BDI scores of the patients in the ESWT and CPT groups.
| ESWT group | CPT group | p | |||||
| Mean±SD | Median | Min-Max | Mean±SD | Median | Min-Max | ||
| VAS score | |||||||
| Pre-treatment vs. 1st week | -34.7±18.4 | -30 | -80 to -10 | -14.4±21.5 | -15 | -70 to 25 | 0.001† |
| Pre-treatment vs. 12th weeks | -37.8±17.6 | -30 | -80 to -10 | -14.3±19.2 | -12.5 | -70 to 20 | 0.001† |
| HAQ score | |||||||
| Pre-treatment vs. 1st week | -3.9±6.3 | -3 | -19 to 12 | -1.1±6.8 | -0.5 | -18 to 22 | 0.048† |
| Pre-treatment vs. 12th weeks | -5.3±6.0 | -4 | -23 to 4 | 0.2±6.7 | -0.5 | -12 to 23 | 0.001† |
| ODI score | |||||||
| Pre-treatment vs. 1st week | -9.8±8.7 | -10.5 | -34 to 12 | -3.2±6.8 | -3.5 | -20 to 16 | 0.001† |
| Pre-treatment vs. 12th weeks | -11.1±7.2 | -9.5 | -28 to 3 | -2.7±7.2 | -3.5 | -20 to 14 | 0.001† |
| FTFD | |||||||
| Pre-treatment vs. 1st week | -2.9±4.6 | -1 | -17 to 5 | -1.4±8.3 | 0 | -38.7 to 20 | 0.020† |
| Pre-treatment vs. 12th weeks | -3.7±4.8 | -2 | -18.5 to 1 | -1.3±10.4 | 0 | -38.7 to 39.9 | 0.009† |
| TPPT | |||||||
| Pre-treatment vs. 1st week | 160.9±66.8 | 155.15 | 35.3 to 291.7 | 9.2±100.2 | -3.25 | -245.3 to 285.1 | 0.001† |
| Pre-treatment vs. 12th weeks | 127.7±78.8 | 124.1 | -9.2 to 339 | -27.8±102.0 | -10.35 | -325.8 to 182.4 | 0.001† |
| BDI score | |||||||
| Pre-treatment vs. 1st week | -3.8±7.7 | -3 | -22 to 18 | -5.7±9.9 | -3 | -43 to 9 | 0.953† |
| Pre-treatment vs. 12th weeks | -5.4±6.5 | -4.5 | -22 to 12 | -3.9±6.7 | -3 | -20 to 12 | 0.349† |
| VAS: Visual Analog Scale; HAQ: Health Assessment Questionnaire; ODI: Oswestry Disability Index; FTFD: Fingertip-to-floor distance; PPT: Pressure pain threshold; BDI: Beck Depression Inventory; ESWT: Extracorporeal shock wave therapy; CPT: Conventional physical therapy; SD: Standard deviation; TPPT: Total pressure pain threshold; † Statistical comparison of change in measurements between groups with the Mann-Whitney U test; Negative values represent decrease in scores and positive values represent increase in scores. | |||||||
Two patients in the ESWT group felt severe pain during the first session of the procedure and did not want to continue the study. The pain of these two patients at the first hour and the first day of the first session was the same as before the procedure. No adverse events were observed in other patients.
Discussion
In the present study, ESWT was found to be superior to CPT in patients with chronic non-specific LBP in terms of FTFD, VAS, HAQ, ODI, and total pain threshold scores. This study has the largest number of participants among studies evaluating the effects of ESWT on chronic LBP. It is also the first in which pressure algometry and spinal mobility assessments were performed.
The effectiveness of ESWT in chronic pain syndromes is known, and today, ESWT is widely used in the treatment of diseases such as plantar fasciitis, lateral epicondylitis, tendinopathies, stress fractures, nonhealing fractures, and myofascial pain syndrome.[29] There are few studies in the literature on the effectiveness of ESWT in chronic LBP, with a small number of participants.[16,17,19] Therefore, this study was conducted to obtain more detailed and precise information about the effectiveness of ESWT in chronic LBP.
In the evaluation of VAS scores, although a decrease was observed in the measurements performed in the first and 12th weeks after the treatment in both groups, it was observed that ESWT was significantly more effective in terms of pain severity. In the study of Han et al.[17] with 30 patients with chronic LBP (15 ESWT, 15 CPT), they found that ESWT was significantly more effective on pain severity, as evaluated using VAS. Similarly, in the present study, a more significant VAS improvement was found with ESWT. In addition, the three-month evaluation and evaluation with an algometer were among the strengths of the present study. In a study conducted by Lee et al.,[16] 28 patients (13 ESWT, 15 CPT) with chronic LBP were investigated for the effectiveness of ESWT in terms of dynamic balance abilities and pain severity, and the BioRescue results were evaluated to measure the dynamic balance of the patients in the ESWT group. Although improvement was observed in all directions in the ESWT group, improvement was observed only in the left and posterior directions in the CPT group. In addition, according to the post-treatment VAS results, they obtained significantly superior results in the ESWT group compared with the conservative group. Çelik et al.[19] conducted a study with 45 patients (25 ESWT, 20 placebo ESWT) with chronic LBP and found that ESWT was significantly more effective than placebo in terms of pain. Nedelka et al.[30] compared the efficacy of facet joint corticosteroid injections, radiofrequency neurotomy, and ESWT in their study involving 60 patients with LBP originating from facet joints. They found that ESWT and radiofrequency neurotomy were significantly more effective than corticosteroid injections. Similar to these studies, ESWT provided significantly superior improvements in VAS scores in the present study. In addition, unlike other studies, the algometer and FTFD were used as a relatively objective assessment tool in this study. In the evaluation performed in six bilateral areas detected in the lumbar region with an algometer for the pain threshold, a statistically significant increase was found in the ESWT group in the one-and 12-week measurements compared to pre-treatment. Consequently, it is understood that ESWT reduces pain and increases the pain threshold. In addition, in the present study, the spinal mobility of the patients was evaluated using FTFD. No improvement in FTFD was observed with treatment in the CPT group, whereas a significant improvement in FTFD was detected in the ESWT group at one and 12 weeks compared to pre-treatment. Another advantage of ESWT over CPT is that it provides these results with fewer sessions.
Low back pain has been associated with disability.[31,32] In the study of Salvetti et al.[33] evaluating the incidence of disability and factors affecting it with 177 patients with chronic LBP, it was shown that individuals with severe disability had higher pain severity and were exposed to pain for a longer time. In the study conducted by Kim et al.[31] in patients with chronic LBP, it was shown that there is a positive relationship between VAS scores and the ODI and Roland Morris Disability Questionnaire scores, which evaluate the disability. The HAQ and ODI were used to assess disability in the present study, and ESWT provided significantly greater improvement in ODI and HAQ scores compared to CPT. Similar to the present study, Han et al.[17] compared the efficacy of ESWT and CPT in patients with chronic LBP and demonstrated that ESWT was significantly more effective than CPT on disability, as in many parameters. Çelik et al.[19] also found that ESWT was more effective on disability than placebo.
Chronic pain has been associated with depressive disorders.[34] Although the pathophysiology of the relationship between chronic pain and depressive disorders has not been clarified, it is a known fact that pain increases depression and depression increases pain.[35] Chronic pain disrupts the patient’s business, family, and social life, distancing them from previously enjoyed activities, causing job loss and decreased QoL, and revealing psychiatric signs and symptoms.[36] Therefore, when evaluating patients with pain, psychological and behavioral aspects should be considered as well as sensory aspects. It is necessary to evaluate the emotional state of the patient. Therefore, the BDI was administered to both groups to evaluate the depressive mood and post-treatment changes in the patients participating in the study. In both groups, BDI scores decreased statistically significantly after treatment compared to pre-treatment. There was no significant difference between the groups in terms of the change in BDI scores at one week and 12 weeks. In a study conducted by Dündar et al.[37] with 83 participants (41 chronic LBP, 42 healthy participants), they found that BDI scores were significantly higher in patients with chronic LBP compared to healthy participants, which negatively affected the QoL. They also concluded that psychiatric evaluation would contribute to treatment outcomes and QoL in patients with chronic LBP.
There are various opinions about the mechanisms of action of ESWT. Extracorporeal shock wave therapy increases axonal regeneration of peripheral nerves and also induces analgesia by reducing inflammation in soft tissues and through some biochemical changes in neurons.[14,15] Additionally, it reduces pain by activating the healing process in tendons, bones, and connective tissues.[16] Extracorporeal shock wave therapy has been reported to stimulate nitric oxide production by stimulating neurogenesis, angiogenesis, and neuronal nitric oxide synthase through the vascular endothelial growth factor.[38-40] It has been determined that the increase in nitric oxide slows down the conduction of pain, reduces pain through an opiate-like effect, increases perfusion by stimulating vasodilation, and results in nerve recovery.[41] These positive effects of ESWT may have led to the results in this study.
Although TENS, ultrasound, and superficial heat treatments are frequently applied in LBP, their effects are controversial. In their meta-analysis, Jauregui et al.[8] reported that TENS was effective in reducing pain and the need for analgesics in chronic LBP. In the systematic review of Khadilkar et al.,[42] it was reported that current evidence does not support the use of TENS in the treatment of chronic LBP. Khan et al.[12] found that adding therapeutic ultrasound to exercise in chronic LBP is effective in reducing pain. Ebadi et al.,[43] in their systematic review examining the effect of ultrasound in chronic LBP, reported few studies revealing that therapeutic ultrasound is effective in the short term; however, current evidence does not support the use of therapeutic ultrasound in chronic LBP. Although conventional physical therapy methods, such as TENS and ultrasound, are frequently used in the treatment of chronic LBP, their effectiveness is controversial in the literature, and they are less effective than ESWT in the current treatment. Therefore, ESWT may be an alternative to conventional physical therapy methods in chronic LBP.
This study had some limitations. There was no long-term follow-up, analgesic use was not recorded, and the participants' daily activities and compliance with given exercises could not be completely controlled. To make a comparison independent of the effectiveness of the exercise, having a third group prescribed only an exercise routine could improve the quality of the study. The absence of a third group that was given only exercise therapy is another limitation of the study. The absence of blinding in the study is another limitation. However, our study has the highest number of participants among the studies examining ESWT in LBP, and it is the first study in which pressure algometry and spinal mobility assessments were performed and depression and disability were considered.
In conclusion, ESWT treatment was found to be more effective on pain, disability, functional status, spinal mobility, and depression in patients with chronic LBP compared to CPT. However, studies evaluating the longer-term effects of ESWT in chronic LBP are required.
Footnotes
Ethics Committee Approval: The study protocol was approved by the Kırşehir Ahi Evran University Faculty of Medicine Clinical Research Ethics Committee (Date: 13.11.2018, No: 2018-21/173) and the Türkiye Ministry of Health, Pharmaceuticals and Medical Devices Agency (Date: 11/12/2018 Number of paperwork No. 71146310-511.06- E.213625). The study was conducted in accordance with the principles of the Declaration of Helsinki.
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions: Data collection, literature review, analysis, writing the article: Ö.K.; Idea/concept, design, control/ supervision, analysis, data collection, critical review, literature review: M.O.; Design, control/supervision, critical review: F.T.; Control/supervision, critical review, analysis: F.A.K.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
Patient Consent for Publication: A written informed consent was obtained from each patient.<br><br><b>Data Sharing Statement:</b><br> The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Hoy D, March L, Brooks P, Woolf A, Blyth F, Vos T, et al. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol. 2010;24:155–165. doi: 10.1016/j.berh.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Balagué F, Mannion AF, Pellisé F, Cedraschi C. Nonspecific low back pain. Lancet. 2012;379:482–491. doi: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 3.Delitto A, George SZ, Van Dillen L, Whitman JM, Sowa G, Shekelle P, et al. Low back pain. A1-57J Orthop Sports Phys Ther. 2012;42 doi: 10.2519/jospt.2012.42.4.A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Minobes-Molina E, Nogués MR, Giralt M, Casajuana C, de Souza DLB, Jerez-Roig J, et al. Effectiveness of specific stabilization exercise compared with traditional trunk exercise in women with non-specific low back pain: A pilot randomized controlled trial. e10304PeerJ. 2020;8 doi: 10.7717/peerj.10304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine (Phila Pa 1976) 1997;22:427–434. doi: 10.1097/00007632-199702150-00015. [DOI] [PubMed] [Google Scholar]
- 6.Haldeman S, Kopansky-Giles D, Hurwitz EL, Hoy D, Mark Erwin W, Dagenais S, et al. Advancements in the management of spine disorders. Best Pract Res Clin Rheumatol. 2012;26:263–280. doi: 10.1016/j.berh.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Quittan M. Management of back pain. Disabil Rehabil. 2002;24:423–434. doi: 10.1080/09638280110108850. [DOI] [PubMed] [Google Scholar]
- 8.Jauregui JJ, Cherian JJ, Gwam CU, Chughtai M, Mistry JB, Elmallah RK, et al. A meta-analysis of transcutaneous electrical nerve stimulation for chronic low back pain. Surg Technol Int. 2016;28:296–302. [PubMed] [Google Scholar]
- 9.Cheing GL, Hui-Chan CW. Transcutaneous electrical nerve stimulation: Nonparallel antinociceptive effects on chronic clinical pain and acute experimental pain. Arch Phys Med Rehabil. 1999;80:305–312. doi: 10.1016/s0003-9993(99)90142-9. [DOI] [PubMed] [Google Scholar]
- 10.French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. A Cochrane review of superficial heat or cold for low back pain. Spine (Phila Pa 1976) 2006;31:998–1006. doi: 10.1097/01.brs.0000214881.10814.64. [DOI] [PubMed] [Google Scholar]
- 11.Durmuş D, Akyol Y, Cengiz K, Terzi T, Cantürk F. Effects of therapeutic ultrasound on pain, disability, walking performance, quality of life, and depression in patients with chronic low back pain: A randomized, placebo controlled trial. Turk J Rheumatol. 2010;25:82–87. doi: 10.1007/s00296-009-1072-7. [DOI] [PubMed] [Google Scholar]
- 12.Khan S, Shamsi S, Alyaemni A, Abdelkader S. Effect of ultrasound and exercise combined and exercise alone in the treatment of chronic back pain. Indian Journal of Physiotherapy and Occupational Therapy - An International Journal. 2013;7:202–202. [Google Scholar]
- 13.Ebadi S, Ansari NN, Naghdi S, Jalaei S, Sadat M, Bagheri H, et al. The effect of continuous ultrasound on chronic non-specific low back pain: A single blind placebocontrolled randomized trial. BMC Musculoskelet Disord. 2012;13:192–192. doi: 10.1186/1471-2474-13-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mariotto S, de Prati AC, Cavalieri E, Amelio E, Marlinghaus E, Suzuki H. Extracorporeal shock wave therapy in inflammatory diseases: Molecular mechanism that triggers anti-inflammatory action. Curr Med Chem. 2009;16:2366–2372. doi: 10.2174/092986709788682119. [DOI] [PubMed] [Google Scholar]
- 15.Ciampa AR, de Prati AC, Amelio E, Cavalieri E, Persichini T, Colasanti M, et al. Nitric oxide mediates antiinflammatory action of extracorporeal shock waves. FEBS Lett. 2005;579:6839–6845. doi: 10.1016/j.febslet.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 16.Lee S, Lee D, Park J. Effects of extracorporeal shockwave therapy on patients with chronic low back pain and their dynamic balance ability. J Phys Ther Sci. 2014;26:7–10. doi: 10.1589/jpts.26.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han H, Lee D, Lee S, Jeon C, Kim T. The effects of extracorporeal shock wave therapy on pain, disability, and depression of chronic low back pain patients. J Phys Ther Sci. 2015;27:397–399. doi: 10.1589/jpts.27.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walewicz K, Taradaj J, Rajfur K, Ptaszkowski K, Kuszewski MT, Sopel M, et al. The effectiveness of radial extracorporeal shock wave therapy in patients with chronic low back pain: A prospective, randomized, single-blinded pilot study. Clin Interv Aging. 2019;14:1859–1869. doi: 10.2147/CIA.S224001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Çelik A, Altan L, Ökmen BM. The effects of extracorporeal shock wave therapy on pain, disability and life quality of chronic low back pain patients. Altern Ther Health Med. 2020;26:54–60. [PubMed] [Google Scholar]
- 20.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) S240-52Arthritis Care Res (Hoboken) 2011;63 Suppl 11 doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 21.Schenk P, Laeubli T, Klipstein A. Validity of pressure pain thresholds in female workers with and without recurrent low back pain. Eur Spine J. 2007;16:267–275. doi: 10.1007/s00586-006-0124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smeets R, Köke A, Lin CW, Ferreira M, Demoulin C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and RolandMorris Disability Questionnaire (RDQ) S158-73Arthritis Care Res (Hoboken) 2011;63 Suppl 11 doi: 10.1002/acr.20542. [DOI] [PubMed] [Google Scholar]
- 23.Pennington B, Davis S. Mapping from the Health Assessment Questionnaire to the EQ-5D: The impact of different algorithms on cost-effectiveness results. Value Health. 2014;17:762–771. doi: 10.1016/j.jval.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 25.Yakut E, Düger T, Oksüz C, Yörükan S, Ureten K, Turan D, et al. Validation of the Turkish version of the Oswestry Disability Index for patients with low back pain. Spine (Phila Pa 1976) 2004;29:581–585. doi: 10.1097/01.brs.0000113869.13209.03. [DOI] [PubMed] [Google Scholar]
- 26.Küçükdeveci AA, Sahin H, Ataman S, Griffiths B, Tennant A. Issues in cross-cultural validity: Example from the adaptation, reliability, and validity testing of a Turkish version of the Stanford Health Assessment Questionnaire. Arthritis Rheum. 2004;51:14–19. doi: 10.1002/art.20091. [DOI] [PubMed] [Google Scholar]
- 27.Hisli N. Beck depresyon envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji Dergisi. 1989;7:3–13. [Google Scholar]
- 28.Perret C, Poiraudeau S, Fermanian J, Colau MM, Benhamou MA, Revel M. Validity, reliability, and responsivenessof the fingertip-to-floor test. Arch Phys Med Rehabil. 2001;82:1566–1570. doi: 10.1053/apmr.2001.26064. [DOI] [PubMed] [Google Scholar]
- 29.Fricová J, Rokyta R. The effects of extracorporeal shock wave therapy on pain patients. Neuro Endocrinol Lett. 2015;36:161–164. [PubMed] [Google Scholar]
- 30.Nedelka T, Nedelka J, Schlenker J, Hankins C, Mazanec R. Mechano-transduction effect of shockwaves in the treatment of lumbar facet joint pain: Comparative effectiveness evaluation of shockwave therapy, steroid injections and radiofrequency medial branch neurotomy. Neuro Endocrinol Lett. 2014;35:393–397. [PubMed] [Google Scholar]
- 31.Kim SH, Park KN, Kwon OY. Pain intensity and abdominal muscle activation during walking in patients with low back pain: The STROBE study. e8250Medicine (Baltimore) 2017;96 doi: 10.1097/MD.0000000000008250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Evcik D, Sonel B. Kronik mekanik bel ağrılı olgularda spinal mobilite, ağrı ve özürlülük ilişkisinin değerlendirilmesi. Turkish Journal of Physical Medicine and Rehabilitation. 2001;47 [Google Scholar]
- 33.Salvetti Mde G, Pimenta CA, Braga PE, Corrêa CF. Disability related to chronic low back pain: Prevalence and associated factors. Rev Esc Enferm USP. 2012 doi: 10.1590/s0080-62342012000700003. 46 Spec No:16- 23. Portuguese. [DOI] [PubMed] [Google Scholar]
- 34.Madenci E, Herken H, Yağız E, Keven S, Gürsoy S. Kronik ağrılı ve fibromiyalji sendromlu hastalarda depresyon düzeyleri ve ağrı ile başa çıkma becerileri. Türk Fiz Tıp Rehab Derg. 2006;52:19–21. [Google Scholar]
- 35.Tütüncü R, Günay H. Kronik ağrı, psikolojik etmenler ve depresyon. Dicle Tıp Dergisi. 2011;38:257–262. [Google Scholar]
- 36.Ataoğlu S, Özçetin A, Ataoğlu A, İçmeli C, Makarç S, Yağlı M. Fibromyaljili ve romatoid artritli hastalarda ağrı şiddeti ile anksiyete ve depresyon ilişkisi. Anadolu Psikiyatri Dergisi. 2002;3:223–226. [Google Scholar]
- 37.Dündar Ü, Solak Ö, Demirdal ÜS, Toktaş H, Kavuncu V. Kronik bel ağrılı hastalarda ağrı, yeti yitimi ve depresyonun yaşam kalitesi ile ilişkisi. Genel Tip Dergisi. 2009;19:99–104. [Google Scholar]
- 38.Mariotto S, Cavalieri E, Amelio E, Ciampa AR, de Prati AC, Marlinghaus E, et al. Extracorporeal shock waves: From lithotripsy to anti-inflammatory action by NO production. Nitric Oxide. 2005;12:89–96. doi: 10.1016/j.niox.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 39.Ito K, Fukumoto Y, Shimokawa H. Extracorporeal shock wave therapy as a new and non-invasive angiogenic strategy. Tohoku J Exp Med. 2009;219:1–9. doi: 10.1620/tjem.219.1. [DOI] [PubMed] [Google Scholar]
- 40.Sun Y, Jin K, Childs JT, Xie L, Mao XO, Greenberg DA. Vascular endothelial growth factor-B (VEGFB) stimulates neurogenesis: Evidence from knockout mice and growth factor administration. Dev Biol. 2006;289:329–335. doi: 10.1016/j.ydbio.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 41.Takahashi N, Wada Y, Ohtori S, Saisu T, Moriya H. Application of shock waves to rat skin decreases calcitonin gene-related peptide immunoreactivity in dorsal root ganglion neurons. Auton Neurosci. 2003;107:81–84. doi: 10.1016/S1566-0702(03)00134-6. [DOI] [PubMed] [Google Scholar]
- 42.Khadilkar A, Odebiyi DO, Brosseau L, Wells GA. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. CD003008Cochrane Database Syst Rev. 2008;2008 doi: 10.1002/14651858.CD003008.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ebadi S, Henschke N, Forogh B, Nakhostin Ansari N, van Tulder MW, Babaei-Ghazani A, et al. Therapeutic ultrasound for chronic low back pain. CD009169Cochrane Database Syst Rev. 2020;7 doi: 10.1002/14651858.CD009169.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]