Abstract
Black Americans have lower rates of depression and anxiety than Whites, despite greater exposure to stressors known to negatively impact mental health, characterized as the Black-White mental health paradox. This study revisited the paradox during the coronavirus pandemic. Drawing on stress process theory, minority stress theory, and the rejection-identification model of discrimination, in-group identity, and well-being, we analyzed original survey data from a quota sample of African American and White adults (N = 594). The survey included a range of stressors and coping resources, including those relevant to the pandemic (e.g., COVID-19 illness) and race (e.g., witnessing anti-Black police violence). Results indicate that despite African Americans’ greater exposure and vulnerability to racial discrimination, the Black-White mental health paradox holds, owing in part to protective effects of African American’s higher self-esteem. Directions for future exploration of the paradox are presented based on this study’s findings.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40615-022-01457-6.
Keywords: Race, Disparities, Mental health, Stressors, Coping resources
Researchers consistently find that despite an excess of exposure to stressors known to be associated with poor mental health, Black Americans tend to have as good if not better mental health as Whites [1, 2], a pattern known as the Black-White mental health paradox [3]. We investigate the paradox during a particularly stressful social context, 1 year into the global coronavirus pandemic. Our study contributes to understanding the Black-White mental health paradox by incorporating pandemic-specific stressors, and by testing multiple theoretically derived mechanisms that link stressors and coping resources to mental health. We also measure multiple outcomes including psychological distress, alternative measures of depression and anxiety, and self-reported somatic symptoms, an idiom of suffering that may be more typical of Black Americans than White Americans. In the following pages, we review evidence of the paradox, theoretical perspectives relevant to it, and research that attempts to explain it, all of which inform the research questions we test in this paper.
Background
Black Americans suffer from worse physical health outcomes than White Americans including higher rates of mortality [4], cardiovascular disease [5], stroke [6], and some cancers [7, 8]. Despite these health disparities, Black Americans’ mental health seems to fare equal or better than Whites. Nationally representative surveys conducted in the USA consistently find that Black Americans are significantly less likely to meet criteria for depression or anxiety disorders than White Americans [1, 2, 9–11] whereas racial differences in psychological distress are less clear. In a review of studies, Barnes and Bates [12] found that Black people reported higher levels of distress than Whites in 42 of 45 analyses, although most differences were not significant, the operationalization of distress varied, and most did not adjust for racial differences in education, employment, or income. Studies that do adjust for socioeconomic indicators find that Black adults have overall lower rates of distress than White adults [13], although low socioeconomic status (SES) Black adults have higher rates of distress than comparable White adults [14, 15], and increases in SES have diminishing returns to mental health for Black adults relative to White adults [16]. Studies that dichotomize the distress continuum tend to find higher rates of serious psychological distress (Kessler-6 ≥ 13) among Black people as compared to White people [17, 18].
According to stress process theory, stressors create stress that can manifest in mental health problems, but access to resources like social support, mastery, and self-esteem can directly improve health and reduce the impact of stressors (i.e., stress buffering) [19, 20]. The minority stress model [21] builds upon the stress process model by focusing on the roles of minority-specific stressors (e.g., racism and discrimination), in addition to minority-specific resources (e.g., racial identity). It posits that characteristics of identity may moderate the stress-mental health relationship [21]. For example, a strong racial identity may either buffer stress by deflecting the injury generated by racism or exacerbate the effects of stressors by rendering a person more vulnerable to minority-related stressors. In contrast, the rejection-identification model treats racial group identity as a mediator, wherein exposure to minority-group stress like racism increases in-group identification and sense of belonging, which in turn improve mental health [22].
Drawing on these theories, we explore four theoretical mechanisms that may explain the Black-White mental health paradox: differential exposure to stressors, differential access to resources, differential vulnerability to stressors, and differential efficacy of resources. The first mechanism, differential exposure to stressors, is unlikely to explain the paradox because Black Americans tend to experience more life event, financial, and race-related stressors than Whites [23, 24]. Moreover, they have been disproportionately impacted by infection with COVID-19, loss of loved ones to it [25–27], financial effects of the pandemic [28], and unlawful killings by the police [29].
Alternatively, the second theoretical mechanism, differential access to resources, suggests that Black people may have greater access to coping resources than Whites, which protects their mental health. Several coping resources have been tested in this regard, with mixed findings. Mouzon [30–32] found that while Black people often had greater social resources than White people (e.g., family interaction, fictive kin ties, support to/from church members, and religious involvement), none accounted for Black-White differences in mental disorders. Thomas Tobin, Erving, and Barve [33] found that Black people had greater family social support than White people, but Louie et al.’s [34] analyses of the same data found that Black people’s higher social support did not explain their mental health advantage. Past research consistently documents higher levels of religiosity among Black Americans than Whites [32, 34, 35] and although some researchers find religiosity accounts for a substantial portion of the paradox [34], most find that any differences in religious involvement do not fully account for better mental health among Black adults [32, 34].
In terms of personal resources, research consistently finds that Black Americans have higher self-esteem than Whites [33, 34, 36]. Moreover, Louie et al. [34] found that self-esteem mediated the race-mental health relationship accounting for 38% of Black-White differences in mental disorder and 79% of the Black-White difference in depressive symptoms. Regarding mastery, several studies found Black adults had significantly lower levels of mastery than White adults [37–40].
The rejection-identification model proposes that when exposure to discrimination leads members of minoritized groups to identify more closely with one another, the resulting in-group identity protects their mental health [22]. Black people have demonstrated greater “positive collective racial identity” than Whites [41], and studies have found that racial identity, self-esteem, and mental health are significantly inter-related among Black Americans [22, 42]. However, studies tend not to compare identity between Black and White people, perhaps because Black people’s identity has developed in response to historical and contemporary racism [43], whereas for White people, identity has been implicitly positive based on White privilege.
The third potential mechanism, differential vulnerability to stressors, might explain the Black-White mental health paradox if the effects of certain stressors have a greater negative impact on the mental health of White people than Black people, resulting in a Black mental health advantage despite greater stress exposure [44]. Recent evidence from the Health and Retirement Survey finds that despite greater chronic stress exposure across five life domains, older Black adults are less likely than older White adults to rank these experiences as stressful [45]. However, it is possible Black people are more vulnerable to stressors related to their race such as racial discrimination and exposure to racial violence than White people. In a national race-comparative study, Eichstaedt et al. [46] found that anger, sadness, depression and anxiety increased more among Black Americans than White Americans following the death of George Floyd in late May of 2020.
Lastly, the Black-White mental health paradox could be due to coping resources being more effective at protecting mental health for Black people relative to White people (differential efficacy of resources). Racial identity has been shown to buffer the negative mental health effects of discrimination among Black people [47], but it has also been found to exacerbate them [48]. Morin and Midlarsky [49] found that mastery was equally effective in reducing distress for Black and White adults. In contrast, Oates and Goode [50] found that mastery reduced distress more for White than for Black adults, whereas public religiosity (e.g., service attendance) reduced distress for Black adults only. There is also research supporting differential stress-buffering of religious resources by race among older adults [51].
Thus far, our theoretical exploration assumed the mental health paradox is objectively real; however, some scholars speculate that survey research does not accurately reflect the mental health of Black Americans, and that the apparent paradox is owing to methodological artifacts such as measurement and sampling biases. For example, racial minorities throughout the world, including Black Americans, often perceive mental illness as more stigmatized than racial majorities [52–54], and perceived stigma could cause Black people to downplay their mental health symptoms [3]. Additionally, measurement items used to categorize respondents as depressed in survey research focus on psychological symptoms (e.g., sad mood and anhedonia), but Black people may experience depression more somatically via bodily pains, resulting in underdiagnosis [12], an alternative we explore below.
The Current Study
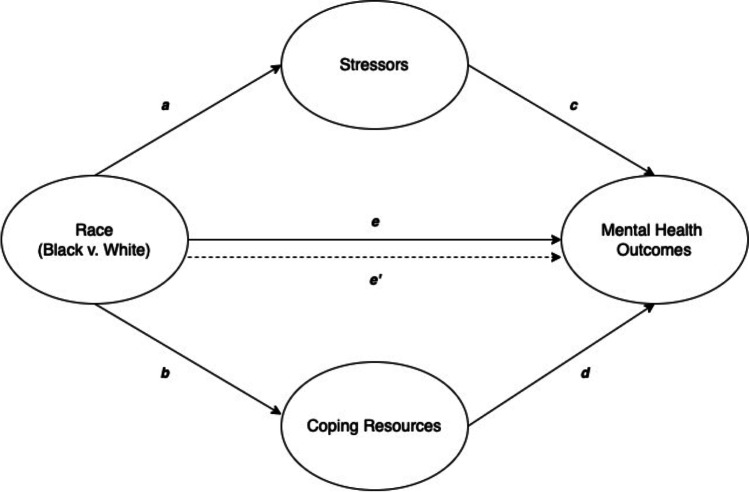
This study tests research questions derived from the four theoretical mechanisms described above in comparing the determinants of distress, somatic symptoms, depression, and anxiety between Black and White Americans using original survey data collected 1 year into the pandemic. Figure 1 depicts a mediation model that illustrates our first two research questions, which concern how differential exposure to stressors (path a) and access to resources (path b) may mediate any direct association we find between race and mental health (path e) via indirect pathways (a × c and b × d).
RQ1: Differential exposure: Are there racial differences in exposure to stressors that indirectly explain racial differences in mental health? (paths a x c)
RQ2: Differential access: Are there racial differences in access to resources that indirectly explain racial differences in mental health? (paths b x d)
Fig. 1.
Mediator model: differential exposure to stressors and differential access to resources
We expect that Black participants will be exposed to more pandemic-related and race-related stressors than White participants, which in turn will predict worse mental health for Black participants relative to Whites (RQ1). We also expect that Black participants will have greater self-esteem, racial identity, and religiosity than White participants (RQ2), resource differences that will indirectly predict better mental health outcomes for Black versus White participants.
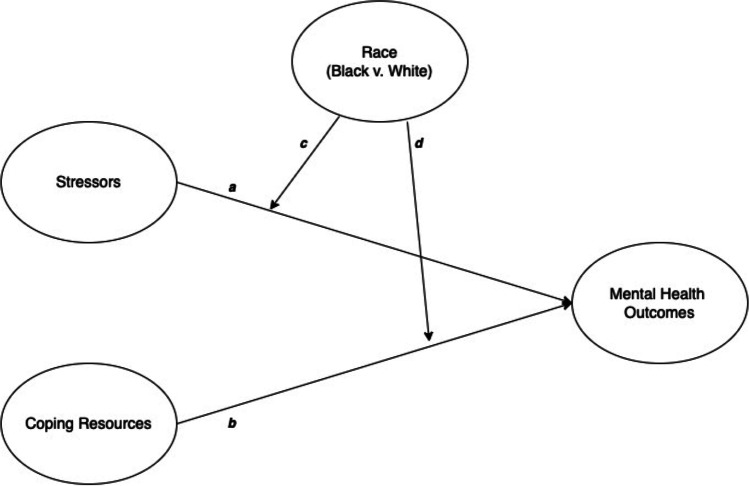
In Fig. 2, path a represents the expected negative effect of exposure to stressors on mental health, whereas path b represents the expected positive effect of resources. Paths c and d correspond to moderating mechanisms and illustrate our third and fourth research questions:
RQ3: Differential vulnerability: Are there racial differences in the impact of stressors on mental health? (path c)
RQ4: Differential efficacy: Are there racial differences in the impact of resources on mental health? (path d)
Fig. 2.
Moderator model: differential vulnerability to stressors and differential efficacy of resources by race
We expect Black participants will be more vulnerable to race-related stressors than White participants given that systemic racism disadvantages Black people, whereas Whites enjoy racial privilege. We also expect racial identity and religiosity will be more protective of mental health for Black participants than Whites and will attenuate the negative effects of stressors on mental health more for Black participants than for Whites.
Methods
This study analyzes online survey data collected from a quota sample of Black and White Americans throughout the USA between March 16 and April 17, 2021. The survey was programmed in Qualtrics and presented to research participants via Prolific Academia (www.prolific.co), a research recruitment website that facilitates quota sampling from respondents who tend to be less familiar with the purpose of research and less dishonest than Mturk workers [50]. Prolific recruits their users through social media advertising, a user referral scheme, and word-of mouth.
Respondents and Procedures
The sample included 297 African American respondents and 297 White respondents (total N = 594). We did not collect data from other Black-identifying groups (e.g., Afro-Caribbeans) and non-native Black people due to considerable between-group differences in mental health [56]; therefore, we refer to respondents as African Americans rather than Black Americans. Respondents had to be 18 or older, and we set quotas for quartiles of household income based on national estimates of the household income distribution for African Americans versus Whites to ensure our data captured variation in SES. The quartiles were (1) less than $10,000 to $29,999, (2) $30,000 to $59,999, (3) $60,000 to $99,999, and (4) $100,000 or more, and the quotas we set for each racial group were based on Current Population Survey household income data for African Americans and White Americans separately [57]. Potential respondents were invited to complete the survey on a first come-first serve basis. There were three attention-check items in the survey and four respondents were excluded owing to failing them. Respondents were paid $9.54 per hour and the survey took about 10 min.
Measures
The survey included existing validated measures and items designed to capture exposure to stressors specific to 2020 such as infection with the COVID-19 virus and witnessing police violence against Black people. Data were collected before COVID-19 vaccines were available to all US adults, so we did not inquire upon vaccination status. We provide a brief overview of the scales below and more detailed information including full lists of survey items in Online Supplemental File 1.
Stressors
Exposure to general stressors was measured by asking about events that occurred since February 2020 when the USA declared a public health emergency including a serious health condition (other than COVID-19), loss of a close family member or friend, serious relationship conflict, relationship dissolution, serious injury, legal troubles, or crime victimization. The events were summed and capped at two or more, which was the 90th percentile. Racial discrimination was measured with the 9-item Everyday Discrimination Scale (α = 0.95) [58]. The original scale did not link discriminatory acts to characteristics such as race or gender, whereas we reworded the question stem to make race salient: “In your day-to-day life, how often do any of the following things happen to you because you are [Black/White]?” Witnessing violence against Black people was measured by 3 items (α = 0.85) modeled after Tynes et al. [59] that asked respondents: “Since February 2020, how often have you seen images, videos, or in-person, Black people who were…,” followed by (1) arrested or detained by law enforcement officers, (2) shot or killed by law enforcement officers, (3) attacked by people who were not law enforcement.
We also included a series of measures relating to COVID-19. COVID-19 infection was measured by asking respondents if they had ever contracted COVID-19 and if so, what best characterized their symptom experience, resulting in a variable ranging from no known infection (0) to infection with severe symptoms (4). COVID-19’s impact on one’s social network was measured by asking how many close friends or family had been seriously ill with COVID-19 and how many died from COVID-19 illness. Because each distribution was positively skewed, we created two dichotomous variables where 1 = knew at least one person seriously ill with COVID-19, and 1 = knew at least one person who died from COVID-19 versus 0 = otherwise. Exposure to secondary pandemic-related stressors (caused by the pandemic but not the virus itself) was measured by asking if any of the following occurred since February 2020: began working or attending school from home, had a pay cut or reduction in work hours, job loss, unemployment, financial hardship, housing unaffordability, homelessness, or bankruptcy/major debt. The count of events was capped at four or more, which was the 90th percentile.
Resources
Self-esteem was measured with the 10-item Rosenberg Self-Esteem Scale (α = 0.93) [60]. Mastery was measured through the 7-item Mastery Scale (α = 0.84) [61]. Emotional social support was measured with two items (α = 0.88) from Ross and Mirowsky [62] that ask participants how much they agreed that: “I have someone I can really talk to” and “I have someone I can turn to for support and understanding when things get rough.” The scale from low (1) to high (5) social support was negatively skewed so we dichotomized social support such that 1 = high social support (agreed or strongly agreed to the statements) and 0 = low social support (neutral or disagreed with statements).
Religiosity was measured with two items (α = 0.81): importance of religious or spiritual beliefs, ranging from not at all important (1) to extremely important (4), and religious service attendance, ranging from never (0) to several times a week (5). The two items were standardized and averaged owing to different response options. Racial identity was measured with the 8-item racial centrality subscale (α = 0.92) of the Multidimensional Inventory of Black Identity (MIBI) [43], with “White” substituted for White respondents. We also measured access to health care based on the expectation that differential health care access would be relevant to COVID-19 infection and to mental health. Three items measured how easy or difficult it is for respondents to access (1) health care in general, (2) COVID-19-related health care, and (3) COVID-19 testing, each measured on a scale from very difficult (1) to very easy (5).
Mental Health Outcomes
We measured four mental health outcomes: psychological distress, somatic symptom burden, and prior diagnoses of depression, and anxiety. Distress was measured by the 6-item Kessler Distress Scale (α = 0.90) [63]. We capped the summed scores at 13 or more out of 18 because that represented the 85th percentile and is the recommended cutoff [63]. Somatic symptoms were measured by the 8-item Somatic Symptom Scale-8 (α = 0.82) (SSS8) [64] to account for the possibility that Black people express reactions to stressors more somatically than psychologically [12]. We capped the summed scores at 16 or more, the 90th percentile, which indicates “very high” somatic symptom burden [64]. Depression and anxiety were measured by self-reports rather than diagnostic inventories. Specifically, we asked respondents if they had been “diagnosed with and/or received mental health treatment for” depression or anxiety in the past 2 years so as not to omit cases who were diagnosed before the onset of the pandemic. If they said yes, we asked whether they thought they currently had the condition.Depression and anxiety were coded as binary variables wherein respondents who had either never been diagnosed or who had been diagnosed in the past 2 years but did not believe they still had depression or anxiety were coded zero, and those who had been diagnosed and indicated they still had the condition were coded as one.
Control variables were measured as follows: age (years), education level (dummy for 1 = bachelor’s degree or more), total household income (1 = < $10,000–13 = > $150,000; see Supplemental File 2 for full ordinal scale), household size (number of residents), gender (dummy for 1 = female or transwomen), sexual orientation (1 = not heterosexual), relationship status (1 = in a relationship), work status (1 = working outside of the home), and political orientation (1 = very liberal–5 = very conservative).
Analytic Strategy
Analyses were conducted in IBM SPSS Statistics 28 (IBM Corp., Armonk, N.Y., USA). We conducted independent samples t tests to detect significant differences between African Americans and Whites in means on ordinal, interval, and ratio variables and proportions on nominal variables. We used ordinary least squares (OLS) regression to analyze the effects of race, stressors, resources, and covariates on distress and somatic symptoms, and binary logistic regression to analyze their effects on depression and anxiety. The impact of COVID-19 on family and friends and access to COVID-related health care and testing are not included in our results because they were invariably non-significant. All regressions presented passed assumption checks and details of those analyses are in Online Supplemental File 3.
We explored RQ1 (differential exposure) and RQ2 (differential access) by conducting mediation analyses with the Process macro for SPSS [65] to estimate all indirect effects of race on outcomes via differential exposure to stressors and differential access to resources simultaneously, net of controls. The continuous version of social support was used in the mediation analysis, as required by the Process macro; otherwise, the binary version was used because it was skewed. Indirect effects were deemed significant if 95% confidence intervals estimated from 10,000 bootstrap samples did not contain zero. We explored RQ3 (differential vulnerability) and RQ4 (differential vulnerability) by adding two-way interaction terms between race and each stressor and resource to the OLS and logistic regression models, first testing interaction terms individually and subsequently testing significant interaction terms together. We also explored interactions between race and socioeconomic status (income and education) considering the literature on diminishing returns, but none were significant. The final models include only those interaction terms that were simultaneously significant.
Results
Table 1 presents the descriptive statistics for the overall sample and by race. Notably, all racial comparisons in mental health outcomes in this sample are consistent with the Black-White mental health paradox, reflecting equal or better mental health among African Americans than White Americans. For example, African Americans and Whites did not significantly differ in average distress symptoms, somatic symptoms or in proportions of those diagnosed with depression. However, African Americans were less likely to have been diagnosed with anxiety than were Whites, and among those who were diagnosed with depression or anxiety, African Americans were less likely to report they still had either condition.
Table 1.
Descriptive statistics overall and by race with tests of mean and proportional differences
| Total | African Am | White | |||
|---|---|---|---|---|---|
| (N = 594) | (n = 297) | (n = 297) | |||
| Variables | Mean(sd)/prop | Min | Max | Mean(sd)/prop | Mean(sd)/prop |
| Outcomes | |||||
| Distress | 6.48(4.62) | 0.00 | 13.00 | 6.24(4.75) | 6.72(4.49) |
| Somatic symptoms | 7.06(5.10) | 1.00 | 16.00 | 6.72(5.11) | 7.40(5.07) |
| Depression (1 = diagnosed) | 0.23 | 0.00 | 1.00 | 0.21 | 0.26 |
| Depression (1 = diagnosed and ongoing) | 0.16 | 0.00 | 1.00 | 0.13* | 0.19* |
| Anxiety (1 = diagnosed) | 0.28 | 0.00 | 1.00 | 0.22** | 0.34** |
| Anxiety (1 = diagnosed and ongoing) | 0.23 | 0.00 | 1.00 | 0.17*** | 0.29*** |
| Stressors | |||||
| General stressors | 0.70(0.78) | 0.00 | 2.00 | 0.70(0.80) | 0.69(0.76) |
| Racial discrimination | 2.05(1.08) | 1.00 | 5.89 | 2.61***(1.14) | 1.48***(0.63) |
| Witnessing violence against Blacks | 8.81(2.74) | 3.00 | 15.00 | 8.93(3.07) | 8.69(2.36) |
| Secondary pandemic stressors | 1.71(1.39) | 0.00 | 4.00 | 1.91***(1.46) | 1.50***(1.29) |
| COVID-19 infection | 0.34(0.86) | 0.00 | 4.00 | 0.27*(0.75) | 0.41*(0.95) |
| Knew someone seriously ill with COVID-19 (1) | 0.33 | 0.00 | 1.00 | 0.35 | 0.30 |
| Knew someone who died of COVID-19 (1) | 0.14 | 0.00 | 1.00 | 0.14 | 0.14 |
| Resources | |||||
| Self-esteem | 3.75(0.97) | 1.00 | 5.00 | 3.84*(0.97) | 3.67*(0.97) |
| Mastery | 3.57(0.83) | 1.00 | 5.00 | 3.56(0.83) | 3.57(0.83) |
| Emotional social support | 4.20(1.04) | 1.00 | 5.00 | 4.09*(1.13) | 4.31*(0.93) |
| Emotional social support (1 = high) | 0.78 | 0.74* | 0.82* | ||
| Religiosity | 0(1) | − 1.41 | 1.30 | 0.29***(0.93) | − 0.29***(0.98) |
| Racial identity | 3.05(1.17) | 1.00 | 5.00 | 3.78***(0.95) | 2.32***(0.88) |
| General health care access | 4.05(1.01) | 1.00 | 5.00 | 4.02(0.97) | 4.08(1.05) |
| COVID-19 health care access | 3.92(0.99) | 1.00 | 5.00 | 3.92(0.93) | 3.93(1.04) |
| COVID-19 testing access | 3.97(0.97) | 1.00 | 5.00 | 3.90(0.99) | 4.05(0.96) |
| Controls | |||||
| Age | 35.84(12.57) | 18.00 | 78.00 | 33.32***(11.04) | 38.36***(13.48) |
| 18–24 | 0.20 | 0.00 | 1.00 | 0.22 | 0.17 |
| 25–34 | 0.36 | 0.00 | 1.00 | 0.42*** | 0.29*** |
| 35–54 | 0.34 | 0.00 | 1.00 | 0.30* | 0.38* |
| 55 and over | 0.11 | 0.00 | 1.00 | 0.06*** | 0.16*** |
| Education (1 = bachelor’s degree or more) | 0.55 | 0.00 | 1.00 | 0.52 | 0.59 |
| Total household income (13 = > $150,000) | 7.52(4.04) | 1.00 | 13.00 | 6.60***(3.97) | 8.44***(3.91) |
| Household size | 2.95(1.43) | 1.00 | 9.00 | 3.13**(1.57) | 2.78**(1.27) |
| Gender (1 = female) | 0.51 | 0.00 | 1.00 | 0.50 | 0.52 |
| Sexual orientation (1 = not heterosexual) | 0.15 | 0.00 | 1.00 | 0.14 | 0.15 |
| Relationship status (1 = in a relationship) | 0.60 | 0.00 | 1.00 | 0.52*** | 0.68*** |
| Work status (1 = works outside the home) | 0.40 | 0.00 | 1.00 | 0.40 | 0.39 |
| Political orientation (5 = very conservative) | 2.42(1.20) | 1.00 | 5.00 | 2.45(1.17) | 2.39(1.24) |
*p < .05, **p < .01, ***p < .001
In terms of stressors, African Americans experienced more racial discrimination and secondary pandemic stressors than Whites, whereas Whites reported more COVID-19 infection than African Americans. Regarding resources, self-esteem, religiosity, and racial identity were significantly higher among African Americans, whereas social support was higher among Whites. No other stressors or resources differed significantly between racial groups. On average, the sample was about 35 years old, and the majority had at least a bachelor’s degree, were female, heterosexual, had a total household income between $50,000 and $69,999, had about three people living in their household, were in a relationship, and worked from home. The sample leaned slightly liberal in political orientation. African Americans were significantly younger, of lower income, had more people living in their households and less likely to be in a relationship than Whites. There were no differences in education, gender, sexual orientation, work status, or political orientation by race.
RQ 1 and 2: Differential Exposure to Stressors and Access to Resources
We tested indirect effects of race on distress, somatic symptoms, depression, and anxiety to determine whether differential exposure to stressors (e.g., discrimination) and differential access to resources (e.g., self-esteem, racial identity) explain racial differences in mental health. Table 2 shows the significant indirect effects. There was an indirect effect of racial discrimination on distress and somatic symptoms, indicating that all else being equal, being African American was associated with increased distress and somatic symptoms because African Americans reported substantially more racial discrimination than Whites (RQ1). However, these indirect effects on distress and somatic symptoms were counterbalanced by the negative indirect effects of self-esteem, suggesting that African Americans tend to be less distressed and have fewer somatic symptoms than Whites because they have greater self-esteem. In contrast, there were no indirect effects of racial discrimination on self-reported depression or anxiety diagnoses, but the indirect effects of self-esteem on depression and anxiety remained.
Table 2.
Unstandardized indirect effects of race on mental health through racial discrimination, self-esteem
| Distress | Som. symptoms | Depression | Anxiety | |||||
|---|---|---|---|---|---|---|---|---|
| n = 594 | n = 594 | n = 584 | n = 582 | |||||
| Mediator variables | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI |
| Racial discrimination | 1.08 | (0.67, 1.53) | 1.16 | (0.62, 1.77) | –- | –- | –- | –- |
| Self-esteem | − 0.90 | (− 1.34, − 0.51) | − 0.62 | (− 0.99, − 0.31) | − 0.19 | (− 0.39, − 0.05) | − 0.21 | (− 0.41, − 0.08) |
Dashes are in place of non-significant coefficients. Indirect effects of all other stressors and resources were tested, but yielded non-significant results across all outcomes so they are omitted from the table. Results are adjusted for covariates
RQ 3 and 4: Differential Vulnerability to Stressors’ Effects and Efficacy of Resources
Table 3 presents the linear regressions of distress and somatic symptoms, indicating that all else being equal, African Americans had lower distress and fewer somatic symptoms than Whites. General stressors and racial discrimination were positively associated with distress and somatic symptoms. Self-esteem and mastery were negatively associated with distress and somatic symptoms. Social support was positively associated with somatic symptoms in the multivariate model, despite being associated with fewer somatic symptoms in the bivariate analysis (Supplemental File 2). This was due to negative suppression, which happens when controlling for a third variable reverses the sign of another predictor variable [66]. In this case, only when self-esteem was in the regression did social support have a positive coefficient rather than the expected negative coefficient. Since social support and self-esteem were positively correlated, the suppressor effect represents the predicted value of somatic symptoms in the unusual case that a person has high social support, but very low self-esteem. All interactions between race and each stressor, and race and each resource were non-significant, suggesting that the differential vulnerability and efficacy mechanisms do not explain racial differences in distress or somatic symptoms.
Table 3.
Distress and somatic symptoms regressed on race, stressors, psychosocial resources, and covariates (N = 594)
| Distress | Somatic Symptoms | ||
|---|---|---|---|
| Model 1 | Model 2 | ||
| Variables | b | b | |
| Constant | 17.27*** | 11.09*** | |
| Race (1 = African American) | − 1.30*** | − 1.65** | |
| General stressors | 0.64*** | 1.32*** | |
| Racial discrimination | 0.65*** | 0.84*** | |
| Witnessing violence against Blacks | 0.08 | 0.05 | |
| Secondary pandemic stressors | 0.07 | 0.27 | |
| COVID-19 infection | 0.02 | 0.01 | |
| Self-esteem | − 2.40*** | − 1.50*** | |
| Mastery | − 0.89*** | − 1.02*** | |
| Emotional social support (1 = high) | 0.35 | 1.05* | |
| Religiosity | 0.09 | 0.04 | |
| Racial identity | 0.03 | − 0.01 | |
| General health care access | − 0.06 | − 0.01 | |
| Age (reference group = 18–24) | |||
| 25–34 | 0.03 | 1.33* | |
| 35–54 | − 1.19** | 1.05 | |
| 55 and over | − 2.35*** | 0.60 | |
| Education (1 = bachelor's degree or more) | 0.04 | − 0.67 | |
| Total household income | 0.01 | − 0.01 | |
| Household size | 0.13 | 0.30 | |
| Gender (1 = female) | 0.77** | 1.47*** | |
| Sexual orientation (1 = not heterosexual) | − 0.16 | 0.08 | |
| Relationship status (1 = in a relationship) | − 0.18 | − 0.31 | |
| Work status (1 = works outside the home) | − 0.45 | 0.23 | |
| Political orientation (5 = conservative) | − 0.27* | − 0.08 | |
| Adjusted R-squared | 0.57 | 0.34 | |
*p < .05, **p < .01, ***p < .001
Table 4 presents logistic regressions of depression and anxiety, presenting direct effects in Models 3a and 4a and interactive effects in Models 3b and 4b. African Americans had lower odds of self-reported depression and anxiety diagnoses than Whites. General stressors were positively associated with both outcomes, whereas witnessing violence against Black people was positively associated with depression only. Self-esteem was negatively associated with depression and anxiety, but social support was positively associated with anxiety (owing to the suppressor effect involving self-esteem). Racial identity was positively associated with depression.
Table 4.
Depression and anxiety regressed on race, stressors, resources, and covariates
| Depression (N = 584) | Anxiety (N = 582) | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 3a | Model 3b | Model 4a | Model 4b | |||||
| Variables | b | OR | b | OR | b | OR | b | OR |
| Constant | − 1.14 | 0.32 | 1.03 | 2.79 | − 2.20* | 0.11 | − 3.99** | 0.02 |
| Race (1 = African American) | − 1.75*** | 0.17 | − 6.79*** | 0.00 | − 1.42*** | 0.24 | 1.04 | 2.82 |
| General stressors | 0.76*** | 2.14 | 0.82*** | 2.27 | 0.56*** | 1.75 | 0.56*** | 1.76 |
| Racial discrimination | 0.27 | 1.31 | − 0.68 | 0.51 | 0.18 | 1.20 | 0.25 | 1.29 |
| Witnessing violence against Blacks | 0.14* | 1.15 | 0.17* | 1.18 | 0.04 | 1.04 | 0.19* | 1.21 |
| Secondary pandemic stressors | − 0.05 | 0.96 | − 0.08 | 0.92 | − 0.02 | 0.98 | − 0.04 | 0.96 |
| COVID-19 infection | 0.17 | 1.18 | 0.52** | 1.69 | − 0.09 | 0.92 | − 0.06 | 0.94 |
| Self-esteem | − 0.58** | 0.56 | − 0.91*** | 0.40 | − 0.61*** | 0.54 | − 0.62*** | 0.54 |
| Mastery | − 0.36 | 0.70 | − 0.44 | 0.64 | − 0.09 | 0.91 | − 0.11 | 0.90 |
| Emotional social support (1 = high) | 0.31 | 1.36 | 0.33 | 1.40 | 1.04** | 2.83 | 1.06** | 2.87 |
| Religiosity | − 0.16 | 0.85 | − 0.11 | 0.90 | − 0.23 | 0.79 | − 0.25 | 0.78 |
| Racial identity | 0.43* | 1.54 | 0.42* | 1.53 | 0.21 | 1.24 | 0.29 | 1.33 |
| General health care access | 0.13 | 1.13 | 0.13 | 1.14 | 0.24 | 1.27 | 0.26 | 1.30 |
| Age (reference group = 18–24) | ||||||||
| 25–34 | 0.86 | 2.37 | 1.07* | 2.91 | 1.06** | 2.88 | 1.14** | 3.12 |
| 35–54 | 0.42 | 1.53 | 0.55 | 1.73 | 0.62 | 1.85 | 0.62 | 1.86 |
| 55 and over | 0.87 | 2.40 | 0.93 | 2.54 | 0.31 | 1.36 | 0.38 | 1.47 |
| Education (1 = bachelor’s degree or more) | − 0.22 | 0.80 | − 0.24 | 0.79 | − 0.34 | 0.71 | − 0.40 | 0.67 |
| Total household income | − 0.04 | 0.97 | − 0.03 | 0.97 | − 0.04 | 0.96 | − 0.04 | 0.96 |
| Household size | − 0.24 | 0.79 | − 0.30* | 0.74 | 0.09 | 1.09 | 0.09 | 1.09 |
| Gender (1 = female) | 0.73* | 2.08 | 0.70* | 2.02 | 1.04*** | 2.84 | 1.06*** | 2.87 |
| Sexual orientation (1 = not heterosexual) | 0.56 | 1.76 | 0.77* | 2.17 | 0.82* | 2.26 | 0.84* | 2.31 |
| Relationship status (1 = in a relationship) | − 0.52 | 0.60 | − 0.54* | 0.58 | − 0.18 | 0.84 | − 0.22 | 0.80 |
| Work status (1 = works outside the home) | − 0.60 | 0.55 | − 0.68* | 0.51 | − 0.52* | 0.60 | − 0.54* | 0.58 |
| Political orientation (5 = conservative) | − 0.38* | 0.68 | − 0.34* | 0.71 | − 0.19 | 0.83 | − 0.16 | 0.85 |
| Differential vulnerability to stressors | ||||||||
| Afr. Am. × general stressors | –- | –- | –- | –- | ||||
| Afr. Am. × discrimination | 1.36** | 3.89 | –- | –- | ||||
| Afr. Am. × witnessing violence against Blacks | –- | –- | − 0.29** | 0.75 | ||||
| Afr. Am. × secondary pandemic stressors | –- | –- | –- | –- | ||||
| Afr. Am. × COVID-19 infection | − 1.32** | 0.27 | –- | –- | ||||
| Differential efficacy of resources | ||||||||
| Afr. Am. × self-esteem | 0.72* | 2.06 | –- | –- | ||||
| Afr. Am. × mastery | –- | –- | –- | –- | ||||
| Afr. Am. × emotional social support | –- | –- | –- | –- | ||||
| Afr. Am. × religiosity | –- | –- | –- | –- | ||||
| Afr. Am. × racial identity | –- | –- | –- | –- | ||||
| Afr. Am. × health care access | –- | –- | –- | –- | ||||
| Nagelkerke R-squared | 0.38 | 0.44 | 0.33 | 0.34 | ||||
*p < .05, **p < .01, ***p < .001
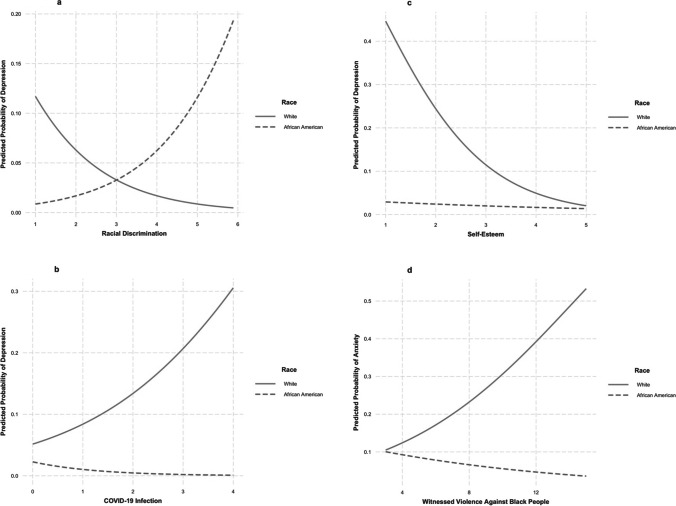
There were two significant interactions representing differential vulnerability to stressors and one representing differential efficacy of resources in the depression model (Model 3b). Race moderated the effects of discrimination (Fig. 3a), COVID-19 infection (Fig. 3b), and self-esteem (Fig. 3c). Racial discrimination increased the odds of depression for African Americans (b = 0.68, p < 0.001), but not Whites (b = − 0.68, p = 0.11), and COVID-19 infection increased the odds of depression for Whites (b = 0.52, p = 0.01), but decreased the odds for African Americans (b = − 0.80, p = 0.04). Self-esteem decreased the odds of depression for Whites (b = − 0.91, p < 0.001), but not for African Americans (b = − 0.19, p = 0.46). In the regression for anxiety (Model 4b), there was one significant interaction representing differential vulnerability to witnessing violence against Black people. Witnessing violence against Black people increased the odds of anxiety for Whites (b = 0.19, p = 0.01) but was not associated with anxiety for African Americans (b = − 0.09, p = 0.18) (Fig. 3d).
Fig. 3.
Plotted interactions for (a) differential vulnerability to discrimination, (b) differential vulnerability to COVID-19, (c) differential efficacy of self-esteem, and (d) differential vulnerability to witnessing violence against Black people
Discussion
Consistent with past research on the Black-White mental health paradox, and in contrast to physical health disparities that disproportionately affect African Americans, this study found that African Americans had equal if not better mental health than White Americans. We found no differences in levels of distress or somatic symptoms between groups, and when controlling for stressors, resources, and covariates, African Americans had significantly lower levels of distress and somatic symptoms. The absence of elevated distress among African Americans is consistent with some studies [13] but contradicts studies that measure distress as a binary variable [12, 17, 18]. The lack of elevated somatic symptoms among African Americans is a novel finding that does not support the argument that the paradox is an artifact of how mental health is measured [12], although African Americans may under-report them.
We also found that African Americans were less likely than Whites to report a diagnosis of depression or anxiety and to think they still had either condition. Despite using a different method of measuring depression and anxiety that requires access to health care to have received a diagnosis, our findings are consistent with psychiatric epidemiological studies of nationally representative samples [1, 2, 9–11] that use algorithms to diagnose survey respondents, regardless of whether they have sought treatment. While these findings support the paradox, they could also reflect several biases. First, mental illness stigma among African Americans, which is common among racial minorities [52–54], may discourage them from seeking treatment or identifying symptoms as depression or anxiety [67]. Second, even when African Americans do seek help, mental health providers have the tendency to diagnose them with more severe psychotic disorders than Whites such as bipolar and schizophrenia [68, 69]. Ultimately, all measures of mental illness, whether categorical or continuous, self-reported or diagnosed by a clinician, are limited by the absence of objective measures or biomarkers of specific psychiatric disorders [70], and depend instead upon the presentation and interpretation of symptoms and behaviors. Despite this inherent limitation, the Black-White mental health paradox is consistent across different types of measures of mental illness, including the self-report measures used in this paper, the symptom algorithms utilized in psychiatric epidemiology surveys [1, 2, 9–11], and clinical data [71].
As expected, we found no support that racial differences in mental health outcomes were attributed to Whites being exposed to more stressors than African Americans (RQ1). Rather, African Americans were more exposed to racial discrimination than Whites, which indirectly increased their distress and somatic symptoms. In fact, if it were not for the role of resources, African Americans might well have reported worse mental health relative to Whites owing to racism. However, differential access to self-esteem partially explained the paradoxical differences in mental health (RQ2). Self-esteem was higher among African Americans than Whites, consistent with past studies [33, 34, 36], which indirectly reduced distress, somatic symptoms, depression, and anxiety. The counterbalancing between the effects of racial discrimination and self-esteem on distress and somatic symptoms may account for the lack of mean differences between racial groups in these outcomes, as Louie and Wheaton found in their study of adolescents [72].
Regarding differential vulnerability (RQ3), the findings differed by race depending on the stressor in question. African Americans were more vulnerable to the effects of racial discrimination, as it was associated with depression for African Americans, but not for Whites. However, contrary to our expectations and prior research by Eichstaedt et al. [46], Whites appeared more vulnerable to witnessing violence against Black people as it was associated with increased anxiety for Whites only. This unexpected finding could reflect Whites’ lack of life experience with racial discrimination, discomfort with and unpreparedness for the graphic footage of racial violence such as the videotaped murder of George Floyd, an African American man, by a White police officer. It could also reflect the process of rejection identification wherein exposure to oppression of one’s racial group increases racial identity which in turn protects the mental health of minority group members [22]. However, we did not find any protective effects of racial identity, which is the key mediator in the rejection-identification model so this framework must be more thoroughly investigated.
Whites’ mental health also appeared more vulnerable to COVID-19 infection and illness, which was associated with increased odds of depression for Whites and decreased odds for African Americans. This divergent pattern could be an artifact of limitations in our data. Namely, only 14 Whites (5%) had depression and COVID-19, and even fewer African Americans (4, or 1%) had both. Second, depression may have preceded infection, given that pre-existing mental illness may increase susceptibility to COVID-19 illness [73].
Self-esteem was the only resource that was differentially efficacious (RQ4), but not for African Americans, as expected. Rather, it reduced the odds of depression for Whites only, even though African Americans reported higher self-esteem, and it indirectly protected their mental health from the ill effects of discrimination. This finding could simply reflect the low probability of depression for African Americans across all levels of self-esteem, which is clear in Fig. 3c.
This study is limited by relying on cross-sectional data, which is especially relevant for the analyses of depression and anxiety that could have existed prior to the stressors we measured during the pandemic. Additionally, while our quota sample mirrors the distributions of household income in the US population by race, the sample is not nationally representative. Unlike the general US population, the majority in both White and African American groups were college educated and worked from home. The inconsistencies in representativeness may explain why the data did not capture the known disproportionate impact of COVID-19 illness on African Americans, but did capture the disproportionate secondary impacts of the pandemic, which are more closely related to income. Future research on the Black-White mental health paradox should collect panel data from a probability sample to track changes in stressors, resources, and mental health with measures of multiple dimensions of racial identity. Longitudinal panel data including these constructs could be used to ascertain how aspects of racial identity develop in response to racism and influence psychological responses to future racism. Additionally, they could demonstrate whether stress “immunity” develops over time in response to cumulative exposure to racism, which could explain why witnessing violence against Black people was only associated with anxiety for White Americans.
In conclusion, despite the disproportionate impact of the global pandemic on African Americans and heightened attention to systemic racism, this study finds that the Black-White mental health paradox persists. Although racial discrimination continues to put African American mental health at risk, self-esteem appears to counteract racism’s pernicious effects, such that African Americans are no more distressed or in physical pain than Whites, whereas Whites are more likely to have depression and anxiety. Nonetheless, the struggle among African Americans to protect their mental health in response to racism continues and should not be minimized.
Supplementary Information
Below is the link to the electronic supplementary material.
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Megan LaMotte and Marta Elliott. The first draft of the manuscript was written by Megan LaMotte and Marta Elliott, and all authors participated in revising the first draft and all subsequent drafts of the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded internally by the School for Social Research and Justice Studies at the University of Nevada, Reno.
Data Availability
For requests to view data and/or research materials, email the corresponding author.
Code Availability
For requests to view code used in data analysis, email the corresponding author.
Declarations
Ethics Approval
This study was granted exemption from review by the University of Nevada, Reno Institutional Review Board.
Consent to Participate
Informed consent was obtained from all respondents included in the study.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams DR, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on alcoholism and related conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 3.Keyes CLM. The Black-White paradox in health: flourishing in the face of social inequality and discrimination. J Pers. 2009;77(6):1677–1706. doi: 10.1111/j.1467-6494.2009.00597.x. [DOI] [PubMed] [Google Scholar]
- 4.Curtin SC, Arias E. Mortality trends by race and ethnicity among adults aged 25 and over, 2000–2017. NCHS Data Brief, no 342. Hyattsville, MD: National Center for Health Statistics. 2019. https://www.cdc.gov/nchs/products/databriefs/db342.htm. [PubMed]
- 5.Leigh JA, Alvarez M, Rodriguez CJ. Ethnic minorities and coronary heart disease: an update and future directions. Curr Atheroscler Rep. 2016;18(2):9. doi: 10.1007/s11883-016-0559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11(3):238–245. doi: 10.2174/1573403X11666141122220003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baquet CR, Mishra SI, Commiskey P, Ellison GL, DeShields M. Breast cancer epidemiology in blacks and whites: disparities in incidence, mortality, survival rates and histology. J Natl Med Assoc. 2008;100(5):480–488. doi: 10.1016/s0027-9684(15)31294-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Du XL, Meyer TE, Franzini L. Meta-analysis of racial disparities in survival in association with socioeconomic status among men and women with colon cancer. Cancer. 2007;109(11):2161–2170. doi: 10.1002/cncr.22664. [DOI] [PubMed] [Google Scholar]
- 9.Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151(7):979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 10.Weissman MM, Leaf PJ, Tischler GL, Blazer DG, Karno M, Bruce ML, Florio LP. Affective disorders in five United States communities. Psychol Med. 1988;18(1):141–153. doi: 10.1017/S0033291700001975. [DOI] [PubMed] [Google Scholar]
- 11.Williams DR, Gonzalez HM, Neighbors H, Neese R, Abelson JM, Sweetman J, Jackson JS. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 12.Barnes DM, Bates LM. Do racial patterns in psychological distress shed light on the Black-White depression paradox? A systematic review. Soc Psychiatry and Psychiatr Epidemiol. 2017;52(8):913–928. doi: 10.1007/s00127-017-1394-9. [DOI] [PubMed] [Google Scholar]
- 13.Bratter JL, Eschbach K. Race/ethnic differences in nonspecific psychological distress: evidence from the National Health Interview Survey. Soc Sci Q. 2005;86(3):620–644. doi: 10.1111/j.0038-4941.2005.00321.x. [DOI] [Google Scholar]
- 14.Kessler RC, Neighbors HW. A new perspective on the relationships among race, social class, and psychological distress. J Health Soc Behav. 1986;27(2):107–115. doi: 10.2307/2136310. [DOI] [PubMed] [Google Scholar]
- 15.Nuru-Jeter A, Williams CT, LaVeist TA. A methodological note on modeling the effects of race: the case of psychological distress. Stress Health. 2008;24(5):337–350. doi: 10.1002/smi.1215. [DOI] [Google Scholar]
- 16.Assari S, Lapeyrouse LM, Neighbors HW. Income and self-rated mental health: Diminished returns for high income Black Americans. Behav Sci. 2018;8(5):50. doi: 10.3390/bs8050050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reeves WC, Strine TW, Pratt LA, Thompson W, Ahluwalia I, Dhingra SS, McKnight-Eily LR, Harrison L, D’Angelo DV, Williams L, Morrow B, Gould D, Safran MA. Mental illness surveillance among adults in the United States. In: Morbidity and Mortality Weekly Report. Centers for Disease Control. 2011. https://www.cdc.gov/mmwr/preview/mmwrhtml/su6003a1.htm [PubMed]
- 18.Roxburgh S. Untangling inequalities: gender, race, and socioeconomic differences in depression. Sociol Forum. 2009;24(2):357–381. doi: 10.1111/j.1573-7861.2009.01103.x. [DOI] [Google Scholar]
- 19.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22(4):337–356. doi: 10.2307/2136676. [DOI] [PubMed] [Google Scholar]
- 20.Turner RJ. Understanding health disparities: the relevance of the stress process model. Soc Ment Health. 2013;3(3):170–186. doi: 10.1177/2156869313488121. [DOI] [Google Scholar]
- 21.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African Americans: implications for group identification and well-being. J Pers Soc Psychol. 1999;77(1):135–149. doi: 10.1037/0022-3514.77.1.135. [DOI] [Google Scholar]
- 23.Lee RT, Perez AD, Boykin CM, Mendoza-Denton R. On the prevalence of racial discrimination in the United States. PLoS ONE. 2019 doi: 10.1371/journal.pone.0210698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams DR. Race, stress, and mental health: findings from the Commonwealth Minority Health Survey. In: Hogue C, Hargraves M, Scott-Collins K, editors. Minority health in America: findings and policy implications from the Commonwealth Fund Minority Health Survey. Baltimore, MD: Johns Hopkins University Press; 2000. pp. 209–243. [Google Scholar]
- 25.CDC. Risk for COVID-19 infection, hospitalization, and death by race/ethnicity. Centers for Disease Control and Prevention. 2020. (https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html). Accessed 19 Oct 2021.
- 26.Goldstein A, Guskin E. Almost one-third of Black Americans know someone who died of Covid-19, survey shows. Washington Post. 2020. https://www.washingtonpost.com/health/almost-one-third-of-black-americans-know-someone-who-died-of-covid-19-survey-shows/2020/06/25/3ec1d4b2-b563-11ea-aca5-ebb63d27e1ff_story.html. Accessed 17 Jul 2020
- 27.Stafford K, Fingerhut H. Black Americans most likely to know a COVID-19 victim. AP News. 2020. https://apnews.com/article/52ed0842bd17102560e5d896be79d38c
- 28.Enriquez D, Goldstein A. COVID-19’s socioeconomic impact on low-income benefit recipients: early evidence from tracking surveys. Socius. 2020;6:1–17. doi: 10.1177/2378023120970794. [DOI] [Google Scholar]
- 29.Fagan J, Campbell AD. Race and reasonableness in police killings. Boston University Law Review. 2020;100:951. [Google Scholar]
- 30.Mouzon DM. Can family relationships explain the race paradox in mental health? J Marriage Fam. 2013;75(2):470–485. doi: 10.1111/jomf.12006. [DOI] [Google Scholar]
- 31.Mouzon DM. Relationships of choice: can friendships or fictive kinships explain the race paradox in mental health? Soc Sci Res. 2014;44:32–43. doi: 10.1016/j.ssresearch.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 32.Mouzon DMM. Religious involvement and the Black-White paradox in mental health. Race Soc Probl. 2017;9(1):63–78. doi: 10.1007/s12552-017-9198-9. [DOI] [Google Scholar]
- 33.Thomas Tobin CS, Erving CL, Brave A. Race and SES differences in psychosocial resources: implications for social stress theory. Soc Psychol Q. 2021;84(1):1–25. doi: 10.1177/0190272520961379. [DOI] [Google Scholar]
- 34.Louie P, Upenieks L, Erving CL, Thomas Tobin CS. Do racial differences in coping resources explain the Black-White paradox in mental health? A test of multiple mechanisms. J Health Soc Behav. 2021;00:1–16. doi: 10.1177/00221465211041031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chatters LM, Taylor RJ, Bullard KM, Jackson JS. Race and ethnic differences in religious involvement: African Americans, Caribbean Blacks, and Non-Hispanic Whites. Ethn Racial Stud. 2009;32:1143–1163. doi: 10.1080/01419870802334531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Twenge JM, Crocker J. Race and self-esteem: meta-analyses comparing Whites, Blacks, Hispanics, Asians, and American Indians and comment on Gray-Little and Hafdahl (2000) Psychol Bull. 2002;128(3):371–408. doi: 10.1037/0033-2909.128.3.371. [DOI] [PubMed] [Google Scholar]
- 37.Assari S. Race, sense of control over life, and short-term risk of mortality among older adults in the United States. Arch Med Sci. 2017;13(5):1233–1240. doi: 10.5114/aoms.2016.59740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bruce MA, Thornton MC. It’s my world? Exploring Black and White perceptions of personal control. Sociol Q. 2004;45(3):597–612. doi: 10.1111/j.1533-8525.2004.tb02305.x. [DOI] [Google Scholar]
- 39.Hill-Joseph EA. Coping while Black: chronic illness, mastery, and the Black-White health paradox. J Racial Ethn Health Disparities. 2019;6(5):935–943. doi: 10.1007/s40615-019-00594-9. [DOI] [PubMed] [Google Scholar]
- 40.Shaw BA, Krause N. Exploring race variations in aging and personal control. J Gerontol. 2001;56(2):S119–124. doi: 10.1093/geronb/56.2.S119. [DOI] [PubMed] [Google Scholar]
- 41.Crocker J, Luhtanen R, Blaine B, Broadnax S. Collective self-esteem and psychological well-being among White, Black, and Asian college students. Pers Soc Psychol Bull. 1994;20(5):503–513. doi: 10.1177/0146167294205007. [DOI] [Google Scholar]
- 42.Ida AK, Christie-Mizell CA. Racial group identity, psychosocial resources, and depressive symptoms: exploring ethnic heterogeneity among Black Americans. Sociol Focus. 2012;45:1–23. doi: 10.1080/00380237.2012.630900. [DOI] [Google Scholar]
- 43.Sellers RM, Smith MA, Shelton JN, Rowley SAJ, Chavous TM. Multidimensional model of racial identity: a reconceptualization of African American racial identity. Pers Soc Psychol Rev. 1998;2(1):18–39. doi: 10.1207/s15327957pspr0201_2. [DOI] [PubMed] [Google Scholar]
- 44.Sternthal MJ, Slopen N, Williams DR. Racial disparities in health: How much does stress really matter? Du Bois Rev. 2011;8(1):95–113. doi: 10.1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brown LL, Abrams LR, Mitchell UA, Ailshire JA. Measuring more than exposure: does stress appraisal matter for Black-White differences in anxiety and depressive symptoms among older adults? Innov Aging. 2020;4(5):1–15. doi: 10.1093/geroni/igaa040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eichstaedt JC, Sherman GT, Giorgi S, Roberts SO, Reynolds ME, Ungar LH, Guntuku SC. The emotional and mental health impact of the murder of George Floyd on the US population. Proc Natl Acad Sci. 2021 doi: 10.1073/pnas.2109139118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chae DH, Lincoln KD, Jackson JS. Discrimination, attribution, and racial group identification: implications for psychological distress among Black Americans in the National Survey of American Life (2001–2003) Am J Orthopsychiatry. 2011;81(4):498–506. doi: 10.1111/j.1939-0025.2011.01122.x. [DOI] [PubMed] [Google Scholar]
- 48.Burrow AL, Ong AD. Racial identity as a moderator of daily exposure and reactivity to racial discrimination. Self and Identity. 2010;9(4):383–402. doi: 10.1080/15298860903192496. [DOI] [Google Scholar]
- 49.Morin RT, Midlarsky E. Social support, mastery, and psychological distress in Black and White older adults. Int J Aging Hum Dev. 2016;82(2–3):209–228. doi: 10.1177/0091415015627161. [DOI] [PubMed] [Google Scholar]
- 50.Oates GL, Goode J. Racial differences in effects of religiosity and mastery on psychological distress: evidence from national longitudinal data. Soc Ment Health. 2013;3(1):40–58. doi: 10.1177/2156869312455930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bierman A. Does religion buffer the effects of discrimination on mental health? Differing effects by race. J Sci Study Relig. 2006;45(4):551–565. doi: 10.1111/j.1468-5906.2006.00327.x. [DOI] [Google Scholar]
- 52.Anglin DM, Link BG, Phelan JC. Racial differences in stigmatizing attitudes toward people with mental illness. Psychiat Serv. 2006;57(6):6. doi: 10.1176/ps.2006.57.6.857. [DOI] [PubMed] [Google Scholar]
- 53.Corrigan PW, Watson AC. The stigma of psychiatric disorders and the gender, ethnicity, and education of the perceiver. Community Ment Health J. 2007;43(5):439–458. doi: 10.1007/s10597-007-9084-9. [DOI] [PubMed] [Google Scholar]
- 54.Eylem O, De Wit L, Van Straten A, Steubl L, Melissourgaki Z, Topgüloǧlu Danlşman G, De Vries R, Kerkhof AJFM, Bhui K, Cuijpers P. Stigma for common mental disorders in racial minorities and majorities: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):1–20. doi: 10.1186/s12889-020-08964-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peer E, Brandimarte L, Samat S, Acquisti A. Beyond the Turk: alternative platforms for crowdsourcing behavioral research. J Exp Soc Psychol. 2017;70:153–163. doi: 10.1016/j.jesp.2017.01.006. [DOI] [Google Scholar]
- 56.Williams DR, Haile R, Gonzalez HM, Neighbors H, Baser R, Jackson JS. The mental health of Black Caribbean immigrants: results from the National Survey of American Life. Am J Public Health. 2007;97(1):52–59. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Flood A, King M, Rodgers R, Ruggles S, Warren JR. Current population survey: version 7.0 . IPUMS. 2020. 10.18128/D030.V7.0
- 58.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 59.Tynes BM, Willis HA, Stewart AM, Hamilton MW. Race-related traumatic events online and mental health among adolescents of color. J Adolesc Health. 2019;65(3):371–377. doi: 10.1016/j.jadohealth.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 60.Rosenberg M. Society and the adolescent self-image. Princeton, N.J: Princeton University Press; 1965. [Google Scholar]
- 61.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21. doi: 10.2307/2136319. [DOI] [PubMed] [Google Scholar]
- 62.Ross CE, Mirowsky J. Explaining the social patterns of depression: control and problem solving or support and talking? J Health Soc Behav. 1989;30(2):206–219. doi: 10.2307/2137014. [DOI] [PubMed] [Google Scholar]
- 63.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SLT, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 64.Gierk B, Kohlmann S, Kroenke K, Spangenberg L, Zenger M, Brahler E, Lowe B. The Somatic Symptom Scale (SSS-8): a brief measure of somatic symptom burden. JAMA Internal Med. 2014;174(3):399–407. doi: 10.1001/jamainternmed.2013.12179. [DOI] [PubMed] [Google Scholar]
- 65.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY, US: Guilford Press; 2013. [Google Scholar]
- 66.Martinez Gutierrez N, Cribbie R. Incidence and interpretation of statistical suppression in psychological research. Can J of Behav Sci. 2021;53:480–488. doi: 10.1037/cbs0000267. [DOI] [Google Scholar]
- 67.Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Morgan C, Rüsch N, Brown JSL, Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- 68.Nazroo JY, Bhui KS, Rhodes J. Where next for understanding race/ethnic inequalities in severe mental illness? Structural, interpersonal and institutional racism. Sociol Health Illn. 2020;42(2):262–276. doi: 10.1111/1467-9566.13001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Neighbors HW, Jackson JS, Campbell L, Williams D. The influence of racial factors on psychiatric diagnosis: a review and suggestions for research. Community Ment Health J. 1989;25(4):301–311. doi: 10.1007/BF00755677. [DOI] [PubMed] [Google Scholar]
- 70.Kirkpatrick RH, Munoz DP, Khalid-Khan S, Booij L. Methodological and clinical challenges associated with biomarkers for psychiatric disease: a scoping review. J Psychiatr Res. 2021;143:572–579. doi: 10.1016/j.jpsychires.2020.11.023. [DOI] [PubMed] [Google Scholar]
- 71.Sclar DA, Robison LM, Skaer TL. Ethnicity/race and the diagnosis of depression and use of antidepressants by adults in the United States. Int Clin Psychopharmacol. 2008;23:106–109. doi: 10.1097/YIC.0b013e3282f2b3dd. [DOI] [PubMed] [Google Scholar]
- 72.Louie P, Wheaton B. The Black-White paradox revisited: understanding the role of counterbalancing mechanisms during adolescence. J Health Soc Behav. 2019;60(2):169–187. doi: 10.1177/0022146519845069. [DOI] [PubMed] [Google Scholar]
- 73.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
For requests to view data and/or research materials, email the corresponding author.
For requests to view code used in data analysis, email the corresponding author.