Abstract
Purpose
“Double Reduction” Policy requires schools to reduce the burden of excessive homework and off-campus training for Chinese students to reduce their academic stress and promote mental health. We conducted a study in compulsory education students before and after the “Double Reduction” Policy to explore changes in mental health problems and relevant influential factors.
Methods
A total of 28,398 elementary and junior high school students completed both waves of the survey through electronic questionnaires. Depressive symptoms were assessed using the Patient Heath Questionnaire (PHQ-9), and anxiety symptoms were assessed using the Generalized Anxiety Disorder Scale (GDA-7). Demographic information was evaluated at baseline, and “Double Reduction” related factors and negative life events were measured at follow up.
Results
The overall depression and anxiety levels significantly decreased after the “Double Reduction” Policy. Girls, poor parental marital quality, chronic physical illness, and psychiatric family history were related to increased occurrence of mental health. Sleep duration > 8 h/night, reduced homework, more extracurricular activities more time with parents, and reduced academic stress were protective factors against mental health problems.
Conclusions
The “Double Reduction” Policy has improved the mental health symptoms of students to a certain extent. Appropriately increasing sleep time, participating in more extracurricular activities and parental involvement, and reducing the burden of homework are effective ways to promote the development of students’ mental health.
Keywords: Depression, Anxiety, Adolescents, “Double Reduction” policy, Stress
Introduction
Chinese parents tend to set high expectations for their children because of the higher standards of general education. Consequently, children’s academic pressure increases thus leading to poor health outcomes [1]. The literature has pointed out that academic motivational goals to compete to get good grades and to be rewarded for their performance were positively related to anxiety symptoms [2]. Zhao and colleagues have found that highly stressful educational environments put Chinese children and adolescents at higher risk of elevated anxiety symptoms [3]. Therefore, it is important to pay attention to the of adolescents’ academic stress, which is critical to promote adolescent mental health.
Students often need to complete a lot of homework and attend off-campus training to improve their academic performance. Studies have shown that students who spend more time on homework and after-school tutoring have later bedtime and shorter sleep duration [4, 5]. Meanwhile, they also suffer from more school-related stress and are more likely to give up activities or hobbies to make way for schoolwork [6, 7]. The stress hypothesis [8] echoes the above-mentioned situations. It argued that chronic stressor exposure (e.g., excessive homework and intensive off-campus training) could result in more severe psychopathology among adolescents. A recent study of students in Singapore found more time studying and doing homework was positively related to higher depressive symptoms [9].
The Chinese government attaches great importance to education; all Chinese children and adolescents can have a nine-year free and mandatory education. In recent years, relevant authorities have also been making efforts to reduce academic stress, preventing children and adolescents’ physical and mental health. In July 2021, the Chinese government implemented the “Double Reduction” Policy to reduce the academic burden of these students, relieve parents’ anxiety, and promote an overall healthy educational environment [10]. Specifically, the government requires schools to reduce the burden of excessive homework and off-campus training [10]. This move may relieve students’ academic pressure to a certain extent and improve their mental health. However, no existing studies have examined changes in mental health problems before and after the “Double Reduction” Policy and related predictors.
From April 21st 2021 to May 12th 2021 (Time 1, T1: before the “Double Reduction” Policy was released), we conducted a cross-sectional survey to investigate mental health in elementary and junior high school students in SZ City (a city in southern Guangdong province, China). From December 17 to 26, 2021 (Time 2, T2: after the “Double Reduction” Policy was implemented), we followed these participants again. This follow-up survey was an opportunity to explore how mental health problems changed in response to the “Double Reduction” Policy and to better understand of factors that affected the occurrence of adolescents’ poor mental health. Three specific objectives were: (a) to examine depression and anxiety prevalence rates among elementary and junior high school students at two surveys; (b) to identify the changes in depressive and anxiety symptoms before and after the “Double Reduction” Policy; and (c) to explore the predictors of changing patterns in these two variables.
Methods
Study population and data collection
This study was a two-point repeated cross-sectional survey with a nested longitudinal subsample. The first data collection wave was before the “Double Reduction” Policy and the second wave was after the “Double Reduction” Policy. Before this survey, all participants and their caregivers signed the electronic informed consent form. Our team designed a specialized platform for this project to protect data safety. The local education bureau and the department of mental health services of each school assisted in recruiting participants. All students used an anonymized student number that was assigned based on their registration status at school to log in to the platform to complete questionnaires. They were informed that they could feel free to withdraw from the study at any time. This study was approved by the Human Research Ethics Committee of South China Normal University (SCNU-PSY-2021-094). We also open a free psychological distress hotline named “Xinqing” to provide psychological services when participants needed.
The subjects of this study were Chinese students (primary, grades 1–6; junior high school students, grades 7–9) receiving compulsory education from 152 schools in Guangdong province. We did not include grades 1–4 with the concern that they may not well understand the questionnaire due to their young age. The 9th graders were also excluded so as to follow the students for at least 2 waves before they graduated from schools. A total of 89,283 students (grades 5–8) were recruited in the first timepoint (T1), and 77,236 students (grades 5–8) were recruited in the second timepoint. In T2 survey, the students of 5th graders did not participate in T1 survey, because they were still in 4th grade when T1 survey started. Through data integration, a total of 28,542 students participated in all two web-based surveys and provided complete data on all measures. The following exclusion criteria were used to improve data quality: (a) abnormal response time; (b) inconsistent survey contents (e.g., different demographic information); and (c) having current or history of mental health illness that were identified by the caregivers or teachers. We further excluded 144 participants based on the above-mentioned criteria. Consequently, 28,398 participants were included in the analyses. We used χ2 tests to compare the prevalence of depression and anxiety at T1 between participants who provided available data for both periods and those who had missing data at T2. There was a small but significant difference between these two groups (depression: 12.6% vs 10.2%, χ2 = 106.24, p = 0.034, Cramer’s V = 0.012; anxiety: 9.0% vs 7.7%, χ2 = 42.92, p < 0.001, Cramer’s V = 0.022).
Measures
Mental health indicators
Depressive symptoms were assessed using the Patient Heath Questionnaire (PHQ-9) [11]. It consists of 9 items, responses to which range from 0-not at all, 1-several days, 2-more than half the days, to 3-nearly every day. Higher summed scores indicate higher levels of depressive symptoms. Previous work has suggested 10 as a cut-off to screen clinical depressive symptoms [12]. Psychometric properties of the PHQ-9 have been described in the Chinese population [13]. In this study, PHQ-9 showed good internal consistency in the two surveys, and the Cronbach’s α was 0.90 and 0.92, respectively.
Generalized Anxiety Disorder Scale (GAD-7) was used for screening and diagnosis of anxiety [14, 15]. Seven items were assessed from 0 (not at all) to 3 (nearly every day), with a higher total score indicating greater anxiety symptoms. A cut-off score of 10 was suggested to identify the clinically significant anxiety symptoms [16]. In the present study, Cronbach’s α of the GAD-7 was 0.94 and 0.94 at T1 and T2, respectively.
“Double Reduction” policy related measures
Five self-devised questions were used to assess students’ study and living conditions after the “Double Reduction” Policy (i.e., T2) (1) reduced homework, (2) more extracurricular activities, (3) increased physical activity, (4) more time with parents, and (5) reduced academic stress. Each item is scored from 1 (significantly increase/decrease) 3 (no changes). In this study, we recorded the five items into two categories, with the original categories 1 and 2 being combined into a new category (1 = yes, 2 = no). The Cronbach’s α of the five items was 0.82. In addition, sleep duration was assessed with an item (“How much time do you sleep every day during the past 2 weeks?”). This item included five choices: 1 ≤ 5 h, 2 = 5–6 h, 3 = 6–7 h, 4 = 7–8 h, and 5 ≥ 8 h. Sleep duration > 8 h per night was considered as sleep sufficiency in this study [17, 18].
Covariates
Demographic information included sex (boys/girls), age, grade (grade 5–8), school types (public school/private school), boarding at school (yes/no), ethnicity (Han [the major ethnic group in China]/others), whether one child or not (yes/no), parental marital status (good/poor [included separated, divorced and widowed]), family income (monthly) (< ¥12,000/¥12,000–¥30,000/ > ¥30,000/unknown), caregivers’ education (below junior high school/senior high school/college or above), chronic physical illness (yes [having at least one of the following: arthritis, angina, asthma, diabetes, visual impairment or hearing problems [19]]/no), and family history of mental disorders (yes/no).
Negative life events over the past 6 months were assessed using the Chinese version of the Adolescent Self-Rating Life Events Checklist (ASLEC) at T2 [20]. The Checklist consists of 27 items covering interpersonal conflicts, academic stress, being punished, personal loss, physical health problems, and others. Participants rated each item on a five-point scale, from 1 (not at all) to 6 (extremely severe). A higher total score indicates the greater severity of stressful life events. The Cronbach’s α of the ASLEC was 0.97 in the current sample.
Statistical analysis
Analyses were performed using IBM SPSS Statistics for Version 23.0. The McNemar’s test was used to examine differences in the prevalence of depression and anxiety between T1 and T2. The Chi-square test was used to compare the prevalence rates of depression and anxiety between different groups of demographic characteristics. Based on the cut-off scores (i.e., 10) of the PHQ-9 and GAD-7 at T1 and T2, four patterns of symptoms trajectories were established: (1) Persistent: those scores at T1 and T2 were both above the cut-off value, (2) Remission: those scores were above the cut-off value but were below the value at T2 below the cutoff at T2; (3) New-onset: those did not have mental health problems but presented at T2; (4) Resistance: those did not have mental health problems across two periods. This classification has been used in some previous studies [21–23]. Multivariate logistic regressions were used to examine predictors for the occurrence and patterns of depression and anxiety. Our major aim was to explore the risk and protective factors associated with increased likelihood of developing non-resistance. We set the resistance group as the referent group and compared it with the new-onset group. We also explored the influential factors associated with the decreased likelihood of developing remission. Thus, we set the persistent group as the referent group and compared it with the remission group. In the multivariate logistic regression model, odds ratio (OR) and 95% confidence interval (CI) were used to quantify the strength of the association. Considering that our sample size was relatively large, all statistical significance was set to be p < 0.001 (2-sided tests). Adjusted odds ratios in 1.2–1.5 (or 0.7–0.9) and > 1.5 (or < 0.7) were regarded as weak/moderate and strong associations, respectively [24].
Results
Sample characteristics
Among 28,398 participants, 14,981 were boys and 13,417 were girls. The mean (SD) age was 12.28 (1.21) years. 13,934 students (49.1%) were from public schools, and 2317 (8.2%) boarded at schools. Other demographic characteristics are shown in Table 1.
Table 1.
Prevalence of depression and anxiety at two wave surveys by demographics (N = 28,398)
| Characteristics | N | Depression (%) | Anxiety (%) | ||
|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | ||
| Sex | |||||
| Boy | 14,981 | 7.1 | 6.5 | 5.3 | 4.7 |
| Girl | 13,417 | 13.0 | 12.5 | 9.8 | 9.8 |
| χ2 | 275.44*** | 301.85*** | 212.52*** | 275.70*** | |
| Grade [age, years] | |||||
| Grade 5 [11.14(0.62)] | 10,545 | 6.7 | 5.6 | 5.1 | 4.2 |
| Grade 6 [12.08(0.59)] | 5991 | 8.7 | 8.1 | 5.9 | 5.7 |
| Grade 7 [13.02(0.60)] | 7031 | 11.8 | 12.7 | 8.9 | 9.9 |
| Grade 8 [13.95(0.62)] | 4832 | 15.5 | 14.2 | 12.3 | 11.1 |
| χ2 | 333.64*** | 406.88*** | 289.72*** | 348.35*** | |
| School types | |||||
| Public school | 13,934 | 9.5 | 8.9 | 7.0 | 6.8 |
| Private school | 14,464 | 10.3 | 9.8 | 7.9 | 7.5 |
| χ2 | 5.83* | 6.87** | 7.67** | 5.84* | |
| Boarding at school | |||||
| Yes | 2317 | 11.3 | 10.4 | 7.9 | 7.8 |
| No | 26,081 | 9.8 | 9.3 | 7.4 | 7.1 |
| χ2 | 5.34* | 3.25 | 0.82 | 1.84 | |
| Ethnicity | |||||
| Han | 27,055 | 9.9 | 9.4 | 7.4 | 7.1 |
| Others | 1343 | 9.8 | 9.2 | 7.4 | 6.6 |
| χ2 | 0.01 | 0.03 | 0.01 | 0.68 | |
| Only-children family | |||||
| Yes | 5638 | 8.8 | 8.5 | 7.2 | 6.3 |
| No | 22,760 | 10.2 | 9.6 | 7.5 | 7.3 |
| χ2 | 9.45** | 6.65** | 0.70 | 7.47** | |
| Parental marital status | |||||
| Good | 27,047 | 9.6 | 9.1 | 7.2 | 6.9 |
| Poor | 1351 | 16.4 | 14.4 | 11.6 | 11.3 |
| χ2 | 66.55*** | 41.88*** | 36.30*** | 38.00*** | |
| Family income (monthly) | |||||
| < ¥12,000 | 12,506 | 9.7 | 9.2 | 7.1 | 6.9 |
| ¥12,000–¥30,000 | 7423 | 8.9 | 8.9 | 6.8 | 7.0 |
| > ¥30,000 | 2342 | 8.7 | 8.8 | 6.5 | 6.4 |
| Unknown | 6127 | 12.0 | 10.5 | 9.2 | 7.9 |
| χ2 | 43.17*** | 13.11** | 38.10*** | 8.06* | |
| Father’s education | |||||
| Junior high school or less | 8556 | 10.7 | 9.6 | 7.8 | 7.4 |
| Senior high school | 8459 | 9.2 | 9.4 | 7.2 | 6.7 |
| College or more | 11,383 | 9.8 | 9.2 | 7.3 | 7.2 |
| χ2 | 11.45** | 1.19 | 2.15 | 3.17 | |
| Mother’s education | |||||
| Junior high school or less | 10,236 | 10.5 | 9.4 | 7.7 | 7.2 |
| Senior high school | 7905 | 9.3 | 9.7 | 7.4 | 7.3 |
| College or more | 10,257 | 9.7 | 9.0 | 7.2 | 6.9 |
| χ2 | 6.80* | 2.66 | 2.14 | 1.19 | |
| Chronic physical illness | |||||
| Yes | 984 | 15.1 | 14.3 | 14.3 | 11.7 |
| No | 27,414 | 9.1 | 7.2 | 7.2 | 7.0 |
| χ2 | 64.10*** | 40.24*** | 70.64*** | 32.21*** | |
| Family history of mental disorders | |||||
| Yes | 267 | 24.0 | 20.2 | 21.0 | 12.4 |
| No | 28,131 | 9.8 | 9.3 | 7.3 | 7.1 |
| χ2 | 59.94*** | 37.54 | 71.95 | 11.21** | |
All demographics variables were measured at Time 1
*p < 0.05, **p < 0.01, **p < 0.001
The impact of the “Double Reduction” policy
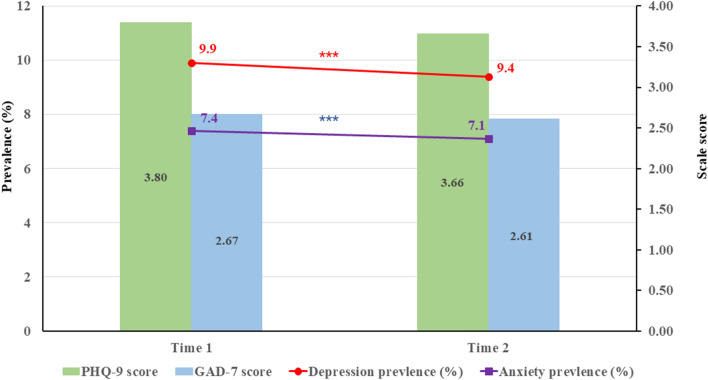
The PHQ-9 scores before the “Double Reduction” Policy were slightly higher than that of after the “Double Reduction” Policy (t = 4.92, p < 0.001, Cohen’s d = 0.030). Similar findings were observed in GAD-7 scores (t = 2.44, p = 0.015, Cohen’s d = 0.015). The prevalence of depressive and anxiety symptoms at T1 were 9.9% and 7.4% respectively, while rates slightly decreased at T2 (see Fig. 1). We further compared differences in the prevalence of depressive and anxiety symptoms at each wave in demographic characteristics (see Table 1).
Fig. 1.
Prevalence rates and mean scores of depression and anxiety in two time points, ***p < 0.001
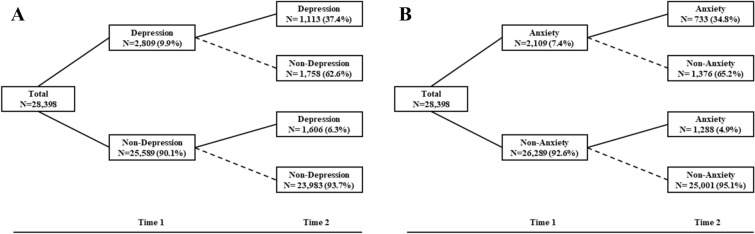
Changing patterns of depression and anxiety
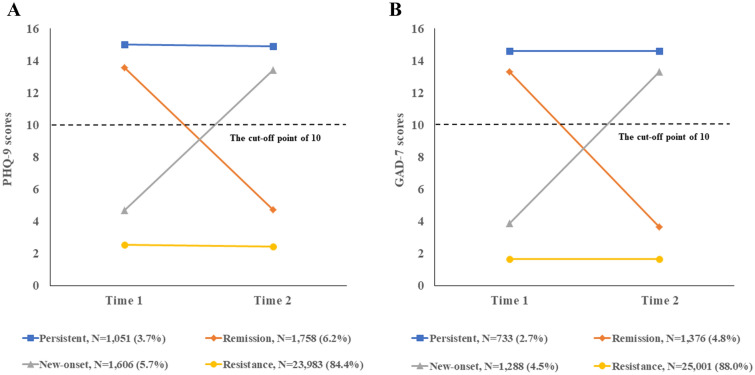
The changing patterns of depressive symptoms were presented in Fig. 2A. We further identified four groups of symptoms trajectory in Fig. 3A. The persistent group (3.7%, N = 1051): met criteria (PHQ-9 score ≥ 10) at both waves; the resistance group: 84.4% (N = 23,983) of participants did not meet criteria for depressive symptoms (i.e., PHQ-9 score < 10). The new-onset group: 5.7% of the sample (N = 1606) did not report depressive symptoms at T1 but had at T2. The remission group (N = 1758, 6.2%): participants reported depressive symptoms at T1 but recovered at T2. As for the changing patterns of anxiety symptoms, we adopted the same grouping method (see Fig. 2B). As shown in Fig. 3B: persistent (N = 733, 2.7%), remission (N = 1376, 4.8%), new-onset (N = 1288, 4.5%), resistance (N = 25,001, 88.0%).
Fig. 2.
Change patterns of mental health problems. A Change patterns of depressive symptoms; B change patterns of anxiety symptoms
Fig. 3.
Trajectories of mental health problems. A Trajectory for depressive symptoms. B Trajectory for anxiety symptoms
Predictors of changing patterns of depression/anxiety
As shown in Table 2, girls were more likely to show new-onset and persistent depressive or anxiety symptoms. The likelihood of developing new-onset depressive symptoms increased if the participants have a family history of mental disorders. Grade 6 students had lower odds of new-onset anxiety symptoms than other graders. Meanwhile, several predictors may also suggest a potential effect on depressive and anxiety symptoms but p values at a 0.01 level. For example, students reporting poor parental marital status were more likely to develop persistent depressive and anxiety symptoms. Those had a chronic physical illness may be at higher risk of experiencing new-onset depressive and anxiety symptoms.
Table 2.
Risk and protective factors of depression or anxiety new-onset [OR(95%CI)]
| Depression | Anxiety | |||
|---|---|---|---|---|
| New-onset vs Resistance | Persistent vs Remission | New-onset vs Resistance | Persistent vs Remission | |
| Measured at T1 | ||||
| Girls (boys as Ref.) | 1.40 (1.26, 1.56)*** | 1.59 (1.34, 1.88)*** | 1.49 (1.32, 1.68)*** | 1.64 (1.34, 1.99)*** |
| Grade (grade 8 as Ref.) | ||||
| Grade 5 | 0.80 (0.68, 0.94)** | 0.84 (0.67, 1.08) | 0.85 (0.71, 1.03) | 0.80 (0.60, 1.05) |
| Grade 6 | 0.74 (0.62, 0.87)** | 0.72 (0.56, 0.91)** | 0.70 (0.58, 0.84)*** | 0.63 (0.47, 0.85)** |
| Grade 7 | 1.01 (0.87, 1.17) | 1.02 (083, 1.26) | 1.09 (0.92, 1.28) | 0.91 (0.72, 1.16) |
| Private school (Public school as Ref.) | 1.10 (0.98, 1.25) | 1.21 (1.01, 1.46)* | 1.16 (1.01, 1.33)* | 1.05 (0.85, 1.30) |
| Boarding at school (No as Ref.) | 1.04 (0.86, 1.27) | 0.65 (0.47, 0.88)** | 0.99 (0.79, 1.23) | 0.68 (0.47, 0.98)* |
| Ethnicity Han (Others as Ref.) | 0.98 (0.76, 1.26) | 0.83 (0.57, 1.19) | 0.93 (0.70, 1.23) | 1.24 (0.79, 1.96) |
| Only-children family (No as Ref.) | 0.93 (0.81, 1.07) | 0.97 (0.78, 1.20) | 0.86 (0.73, 1.01) | 0.94 (0.73, 1.19) |
| Poor parental marital status (Good as Ref.) | 1.11 (0.88, 1.41) | 1.51 (1.12, 2.02)** | 1.24 (0.97, 1.60) | 1.64 (1.17, 2.32)** |
| Family income (monthly) (< ¥12,000 as Ref.) | ||||
| ¥12,000–¥30,000 | 0.91 (0.79, 1.05) | 1.11 (0.89, 1.37) | 0.93 (0.80, 1.09) | 1.15 (0.90, 1.48) |
| > ¥30,000 | 0.92 (0.74, 1.15) | 1.20 (0.86, 1.66) | 0.95 (0.75, 1.21) | 0.84 (0.57, 1.26) |
| Unknown | – | – | – | – |
| Father’s education (College or more as Ref.) | ||||
| Junior high school or less | 1.06 (0.89, 1.25) | 0.94 (0.73, 1.20) | 1.01 (0.84, 1.21) | 0.89 (0.67, 1.19) |
| Senior high school | 1.04 (0.90, 1.20) | 1.06 (0.85, 1.32) | 0.90 (0.77, 1.06) | 0.89 (0.69, 1.15) |
| Mother’s education (College or more as Ref.) | ||||
| Junior high school or less | 0.85 (0.80, 1.11) | 1.12 (0.88, 1.42) | 1.00 (0.83, 1.20) | 1.02 (0.77, 1.36) |
| Senior high school | 1.04 (0.90, 1.20) | 1.18 (0.95, 1.47) | 1.03 (0.88, 1.22) | 1.17 (0.90, 1.50) |
| Chronic physical illness (No as Ref.) | 1.49 (1.16, 1.91)** | 1.11 (0.80, 1.54) | 1.46 (1.11, 1.92)** | 1.06 (0.73, 1.53) |
| Family history of mental disorders (No as Ref.) | 2.30 (1.50, 3.53)*** | 1.09 (0.64, 1.84) | 1.31 (0.75, 2.28) | 0.79 (0.44, 1.45) |
| Measured at T2 | ||||
| Negative life events (contact variable) | 1.03 (1.03, 1.04)*** | 1.03 (1.03, 1.03)*** | 1.04 (1.04, 1.04)*** | 1.03 (1.03, 1.04)*** |
| Sleep duration > 8 h/n (No as Ref.) | 0.33 (0.26, 0.43)*** | 0.38 (0.25, 0.57)*** | 0.35 (0.27, 0.47)*** | 0.46 (0.29, 0.75)*** |
| Reduced homework (No as Ref.) | 0.78 (0.68, 0.89)*** | 0.85 (0.70, 1.04) | 0.77 (0.67, 0.89)*** | 0.81 (0.65, 1.02) |
| More extracurricular activities (No as Ref.) | 0.77 (0.66, 0.88)*** | 0.84 (0.68, 1.04) | 0.73 (0.63, 0.86)*** | 0.71 (0.55, 0.91)** |
| Increased physical activity (No as Ref.) | 0.98 (0.85, 1.11) | 0.90 (0.74, 1.10) | 1.01 (0.87, 1.16) | 1.08 (0.86, 1.36) |
| More time with parents (No as Ref.) | 0.52 (0.46, 0.59)*** | 0.58 (0.48, 0.71)*** | 0.48 (0.41, 0.55)*** | 0.71 (0.57, 0.90)** |
| Reduced academic stress (No as Ref.) | 0.59 (0.51, 0.68)*** | 0.60 (0.48, 0.75)*** | 0.50 (0.42, 0.59)*** | 0.45 (0.34, 0.59)*** |
Bold: p < 0.001 and OR > 1.2 (or < 0.9) were considered to have scientific and public health significance
Furthermore, changes in lifestyles after the implementation of “Double Reduction” Policy have significant effects on develop depressive and anxiety symptoms after controlling for demographics and negative life events. Specifically, reduced homework, more extracurricular activities, more time with parents, and reduced academic pressure were protective factors against poor mental health. In addition, students with sleep duration > 8 h per night were less likely to have new-onset and persistent mental symptoms in comparison to those who reported sleep duration ≤ 7 h per night.
Discussion
This is the first study to explore the impact of the “Double Reduction” Policy on mental health among adolescents in China. We examined changing patterns of depressive and anxiety symptoms before and after the “Double Reduction” Policy. Four different patterns were identified. We further explore the influential factors of these patterns.
It is noteworthy that the prevalence of depression (9.9% vs. 9.4%) and anxiety (7.4% vs. 7.1%) slightly decreased after the policy was implemented. These findings indicated that the “Double Reduction” Policy might relieve adolescents’ mental health, echoing the literature that academic burden negatively impacts on mental health [9, 25]. We acknowledge that this decreasing trend is small. Several assumptions might help us understand this atmosphere. First, the implementation of the “Double Reduction” Policy is still in its early stage. It is possible that the obvious positive impacts will be observed with long-term multiple follow-ups. Second, lifestyle changes caused by COVID-19 pandemic (e.g., restrictions on social activities, online classes) may adversely affect adolescents’ mental health [26, 27]. However, it is a pity that we did not have available data to tease out its impacts. These reasons may influence the effectiveness of the “Double Reduction” Policy.
The changing patterns of depressive and anxiety symptoms showed that the majority of students exhibited very mild or no mental health at two surveys (84.4% and 88.0% for resistance of depressive and anxiety symptoms respectively). Previous studies also suggested that approximately more than half of the children and adolescents maintain a stable healthy functioning over time [28]. Costello and colleagues found that about 28.7% of adolescents reported non-depressed mood symptoms and 59.4% had low symptoms patterns across 6 years [29]. Moreover, a very small percentage of children and adolescents have persistent (all rates were about 3%) or new-onset (all rates were about 5%) mental health problems in the current study. The potential explanation for those who suffer from persistent or new-onset mental health problems, as follows: Without additional support from off-campus training courses, some students may be concerned about their grades. Meanwhile, an increase in extracurricular activities increases the risk of some students’ excessive Internet use [30], which may also affect their mental health.
We found that participants who had reduced academic stress after the “Double Reduction” Policy were less likely to report persistent and new-onset mental health problems than those who had not. Greenberger and colleagues have found that the association between academic stress and poor mental health appears stronger among Chinese students than those in western countries [31]. Academic stress is associated with the notably high learning/testing standards, outcomes, and expectations of secondary schools in China, which may play a significant role in explaining high incidences of anxiety and depression among Chinese adolescents [32]. Our analyses of the “Double Reduction” Policy related measures found that reduced homework and more extracurricular activities were protective against depressive and anxiety symptoms. Previous work has indicated that adolescents who spent long hours on homework reported higher depression level [9]. Longer homework/studying durations were associated with less nocturnal sleep and greater academic stress [6, 7], leading to increased anxious symptoms [9]. In addition, we found participation in extracurricular activities could improve adolescents’ health, which is consistent with the literature [33, 34].
Results in the logistic model showed that those who had sleep duration more than 8 h per night may be less likely to report new onset and persistent mental health symptoms. Consistent with the literature [35, 36], insufficient sleep can disturb an individual’s emotional regulation, which may increase depressive and anxiety symptoms. Furthermore, coincides with previous findings [37], adolescents who spend more time with their parents are less likely to have persistent and new onset mental health problems prospectively. Parental presence may provide continuous support to the adolescent when she/he encounters challenges. It is also possible that engaging in tasks together with parents may help to minimize adolescents’ ruminative processes and facilitate greater behavioral activation; these two factors have been identified as potential mechanisms of psychotherapy for depression [38, 39]. When considering the influence of demographic factors, our results echo previous findings that girls [40], poor parental marital status [41], chronic physical illness [42], and family history of mental disorders [43] were associated with poor mental health. Students in Grade 6 have a lower risk of new-onset anxiety, which may be explained by the fact that they were in the first stage of junior high school when we conducted our second survey. At that time, they had already passed the junior high school entrance examination and thus their study pressure was relatively lower. We suggest future psychosocial interventions in adolescents may need to take these factors into consideration.
Several limitations need to be acknowledged. Firstly, depressive and anxiety symptoms were assessed by self-report questionnaires rather than clinical interviews, as well as two surveys were administered using a web-based questionnaire, which may result in potential reporting bias. Second, there was a high attrition rate, which may impact the accuracy of changes in symptoms. In the second survey (December 2021), students in grades 6 entered junior high schools through the entrance examination, and only a small number of students who stayed in the local school participated in the second survey. Although mild significant differences with small effect sizes (Cramer’s V = 0.012 and 0.022) were found for the baseline prevalence between participants who were followed up and those lost to follow-up, the results need to be interpreted with caution. Third, we used only dichotomous variables to measure lifestyle change, which provides a limited interpretation of the specific impact of the “Double Reduction” Policy on students’ learning and lives. Furthermore, the duration between two waves was 8 months, which only reflect a temporary change before and after the “Double Reduction” Policy. To our knowledge, there are no other studies to examine the effect of the “Double Reduction” Policy on students’ mental health, and our study is the first evaluation of the effect of the policy on students’ well-being. Longer follow-ups are needed to explore the long-term effects of this policy implementation on students’ well-being.
Conclusions
A declined trend in depression and anxiety among Chinese adolescents was observed after the “Double Reduction” Policy. More attention needs to be drawn to those at higher risk of developing persistent or new-onset mental health problems. In addition, developing psychological interventions aiming at increasing sleep duration, extending time with parents, and taking part in extracurricular activities, as well as reducing homework load and academic pressure is critical for the prevention of essential mental health problems.
Acknowledgements
The authors want to express their sincere gratitude to all participants for participating in the study.
Author contributions
DW contributed significantly to acquisition and interpretation of data, drafting and revising of the manuscript for publication. XC and ZM were significantly involved in the conception, design, and analysis of the data. XL contributed to the drafting and revision of the manuscript and gave final approval to its publication. FF was significantly involved in the conception and design of the study as well as the revision of the manuscript and final approval of its publication. All authors read and approved the final manuscript.
Funding
The present study was funded by National Natural Science Foundation of China (Grant No. 31871129); Research on the Processes and Repair of Psychological Trauma in Youth, Project of Key Institute of Humanities and Social Sciences, MOE (Grant No. 16JJD190001); Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (GDUPS2016).
Availability of data and materials
The dataset used and/or analyzed during the current study are available from the corresponding author (FF) on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Human Research Ethics Committee of South China Normal University (SCNU-PSY-2021-094). The survey was under the principle of voluntary participation. The participants and their guardians carefully read, signed and returned the informed consent form to the researcher.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhao X, Selman RL, Haste H, Cheng M. Academic stress in Chinese schools and a proposed preventive intervention program. Cogent Edu. 2015;2(1):1000477. doi: 10.1080/2331186X.2014.1000477. [DOI] [Google Scholar]
- 2.Essau CA, Leung PW, Conradt J, Cheng H, Wong T. Anxiety symptoms in Chinese and German adolescents: their relationship with early learning experiences, perfectionism, and learning motivation. Depress Anxiety. 2008;25(9):801–810. doi: 10.1002/da.20334. [DOI] [PubMed] [Google Scholar]
- 3.Zhao J, Xing X, Wang M. Psychometric properties of the Spence Children’s Anxiety Scale (SCAS) in Mainland Chinese children and adolescents. J Anxiety Disord. 2012;26(7):728–736. doi: 10.1016/j.janxdis.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Twenge JM, Krizan Z, Hisler G. Decreases in self-reported sleep duration among U.S. adolescents 2009–2015 and association with new media screen time. Sleep Med. 2017;39:47–53. doi: 10.1016/j.sleep.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Street NW, McCormick MC, Austin SB, Slopen N, Habre R, Molnar BE. Examining family and neighborhood level predictors of sleep duration in urban youth. Fam Syst Health. 2018;36(4):439–450. doi: 10.1037/fsh0000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galloway M, Conner J, Pope D. Nonacademic effects of homework in privileged, high-performing high schools. J Exp Educ. 2013;81(4):490–510. doi: 10.1080/00220973.2012.745469. [DOI] [Google Scholar]
- 7.Galloway M, Pope D. Hazardous homework? The relationship between homework, goal orientation, and well-being in adolescence. Encounter. 2007;20(4):25–31. [Google Scholar]
- 8.Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 9.Yeo SC, Tan J, Lo JC, Chee M, Gooley JJ. Associations of time spent on homework or studying with nocturnal sleep behavior and depression symptoms in adolescents from Singapore. Sleep Health. 2020;6(6):758–766. doi: 10.1016/j.sleh.2020.04.011. [DOI] [PubMed] [Google Scholar]
- 10.State Council of the People’s Republic of China. Views on further reducing the burden of homework and off-campus training for students at the compulsory education stage. 2021. http://www.gov.cn/zhengce/2021-07/24/content_5627132.htm.
- 11.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184(3):E191–6. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 14.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 15.Tong X, An D, McGonigal A, Park SP, Zhou D. Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. 2016;120:31–36. doi: 10.1016/j.eplepsyres.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 16.Lowe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell JA, Morales KH, Williamson AA, Huffnagle N, Ludwick A, Grant S, et al. Changes in sleep duration and timing during the middle-to-high school transition. J Adolesc Health. 2020;67(6):829–836. doi: 10.1016/j.jadohealth.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, Lloyd RM, et al. Consensus statement of the american academy of sleep medicine on the recommended amount of sleep for healthy children: methodology and discussion. J Clin Sleep Med. 2016;12(11):1549–1561. doi: 10.5664/jcsm.6288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koyanagi A, Stubbs B, Lara E, Veronese N, Vancampfort D, Smith L, et al. Psychotic experiences and subjective cognitive complaints among 224 842 people in 48 low- and middle-income countries. Epidemiol Psychiatr Sci. 2018;29:e11. doi: 10.1017/S2045796018000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu X, Liu L, Yang J, Chai F, Wang A, Sun L. Reliability and validity of the adolescents self-rating life events checklist. China J Clin Psychol. 1997;1:39–41. [Google Scholar]
- 21.Wang D, Zhou L, Wang J, Sun M. The bidirectional associations between insomnia and psychotic-like experiences before and during the COVID-19 pandemic. Nat Sci Sleep. 2021;13:2029–2037. doi: 10.2147/NSS.S335508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang D, Ross B, Zhou X, Meng D, Zhu Z, Zhao J, et al. Sleep disturbance predicts suicidal ideation during COVID-19 pandemic: A two-wave longitudinal survey. J Psychiatr Res. 2021;143:350–356. doi: 10.1016/j.jpsychires.2021.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Y, Zhao J, Ma Z, McReynolds LS, Lin D, Chen Z, et al. Mental health among college students during the COVID-19 Pandemic in China: a 2-wave longitudinal survey. J Affect Disord. 2021;281:597–604. doi: 10.1016/j.jad.2020.11.109. [DOI] [PubMed] [Google Scholar]
- 24.Monson R. Occupational epidemiology. 2. Boca Raton: CRC Press; 1990. [Google Scholar]
- 25.Wang L. The analysis of mathematics academic burden for primary school students based on PISA data analysis. Front Psychol. 2021;12:600348. doi: 10.3389/fpsyg.2021.600348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Samji H, Wu J, Ladak A, Vossen C, Stewart E, Dove N, Long D, Snell G. Review: mental health impacts of the COVID-19 pandemic on children and youth—a systematic review. Child Adolesc Ment Health. 2022;27(2):173–189. doi: 10.1111/camh.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li F. Impact of COVID-19 on the lives and mental health of children and adolescents. Front Public Health. 2022;10:925213. doi: 10.3389/fpubh.2022.925213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shore L, Toumbourou JW, Lewis AJ, Kremer P. Review: longitudinal trajectories of child and adolescent depressive symptoms and their predictors—a systematic review and meta-analysis. Child Adolesc Ment Health. 2018;23(2):107–120. doi: 10.1111/camh.12220. [DOI] [PubMed] [Google Scholar]
- 29.Costello DM, Swendsen J, Rose JS, Dierker LC. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J Consult Clin Psychol. 2008;76(2):173–183. doi: 10.1037/0022-006X.76.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaess M, Klar J, Kindler J, Parzer P, Brunner R, Carli V, et al. Excessive and pathological Internet use—risk-behavior or psychopathology? Addict Behav. 2021;123:107045. doi: 10.1016/j.addbeh.2021.107045. [DOI] [PubMed] [Google Scholar]
- 31.Greenberger E, Chen C, Tally SR, Qi D. Family, peer, and individual correlates of depressive symptomatology among U.S. and Chinese adolescents. J Consult Clin Psychol. 2000;68(2):209–19. doi: 10.1037//0022-006x.68.2.209. [DOI] [PubMed] [Google Scholar]
- 32.Liu H, Shi Y, Auden E, Rozelle S. Anxiety in rural Chinese children and adolescents: comparisons across provinces and among subgroups. Int J Environ Res Public Health. 2018;15(10):2087. doi: 10.3390/ijerph15102087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oberle E, Ji XR, Guhn M, Schonert-Reichl KA, Gadermann AM. Benefits of extracurricular participation in early adolescence: associations with peer belonging and mental health. J Youth Adolesc. 2019;48(11):2255–2270. doi: 10.1007/s10964-019-01110-2. [DOI] [PubMed] [Google Scholar]
- 34.McCabe KO, Modecki KL, Barber BL. Participation in organized activities protects against adolescents' risky substance use, even beyond development in conscientiousness. J Youth Adolesc. 2016;45(11):2292–2306. doi: 10.1007/s10964-016-0454-x. [DOI] [PubMed] [Google Scholar]
- 35.Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014;37(2):239–244. doi: 10.5665/sleep.3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Merikanto I, Partonen T. Eveningness increases risks for depressive and anxiety symptoms and hospital treatments mediated by insufficient sleep in a population-based study of 18,039 adults. Depress Anxiety. 2021;38(10):1066–1077. doi: 10.1002/da.23189. [DOI] [PubMed] [Google Scholar]
- 37.Manczak EM, Ordaz SJ, Singh MK, Goyer MS, Gotlib IH. Time spent with parents predicts change in depressive symptoms in adolescents with major depressive disorder. J Abnorm Child Psychol. 2019;47(8):1401–1408. doi: 10.1007/s10802-019-00526-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Watkins E, Scott J, Wingrove J, Rimes K, Bathurst N, Steiner H, et al. Rumination-focused cognitive behaviour therapy for residual depression: a case series. Behav Res Ther. 2007;45(9):2144–2154. doi: 10.1016/j.brat.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 39.Jacobson N, Martell C, Dimidjian S. Behavioral activation treatment for depression: returning to contextual roots. Clin Psychol Sci Pract. 2001;8(3):255–270. doi: 10.1093/clipsy.8.3.255. [DOI] [Google Scholar]
- 40.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Spence SH, Najman JM, Bor W, O'Callaghan MJ, Williams GM. Maternal anxiety and depression, poverty and marital relationship factors during early childhood as predictors of anxiety and depressive symptoms in adolescence. J Child Psychol Psychiatry. 2002;43(4):457–469. doi: 10.1111/1469-7610.00037. [DOI] [PubMed] [Google Scholar]
- 42.Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29(5):409–416. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 43.Jansen K, Cardoso TA, Fries GR, Branco JC, Silva RA, Kauer-Sant'Anna M, et al. Childhood trauma, family history, and their association with mood disorders in early adulthood. Acta Psychiatr Scand. 2016;134(4):281–6. doi: 10.1111/acps.12551. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used and/or analyzed during the current study are available from the corresponding author (FF) on reasonable request.