Abstract
The great milestones in medicine almost always have their precursors, which help the great event to break through. So it was with allergen-specific immunotherapy (AIT) and the great work of Noon and Freeman and their world-renowned publication in 1911. In this article, we want to outline AIT’s long journey, from early attempts to achieve tolerance to allergens in the environment. Many very different methods were used; from homeopathy to the use of recombinant allergens. Initially, the allergen extracts were given only subcutaneously, but then also through other routes, such as nasal, rectal, intradermal, epicutaneous, in lymph nodes, or oral. It was the great merit of Bill Franklin, whom many of us still experienced as active participants in congresses, to point out that the effect of AIT must be documented not only by clinical observation but in a controlled form including placebo injections. AIT was thus transferred to evidence-based medicine, which we successfully apply today. We would like to express our gratitude to Bill Franklin himself and all others involved in the development of AIT with this summary of 111 years of immunotherapy.
Keywords: adjuvants, allergoids, allergen immunotherapy, hyposensitization, history, oral immunotherapy in food allergy, sublingual immunotherapy
Introduction
Allergen immunotherapy (AIT) (also called specific immunotherapy (SIT), allergen-specific immunotherapy (ASIT), desensitization, hyposensitization) is the administration of a specifically relevant allergen for the treatment of IgE-mediated allergic diseases [1, 2, 3, 4, 5, 6] through the sublingual or subcutaneous route.
Most publications see the introduction of this only available disease-modifying treatment option for allergic patients in 1911, referring to an article by Leonard Noon in the Lancet [7]. However, the idea was not totally new, there were some “precursors”.
Early precursors
The principle of inducing clinical tolerance against a harmful stimulus has been tried already 2,000 years ago by king Mithradates from Pontos who wanted to protect himself against being poisoned. King Mithradates VI. (132 – 63 B.C.) took increasing doses of snake venom to make himself immune against the venom. It is unknown whether this treatment really worked, but there is some probability, because when the Romans defeated him, he had to kill himself with a sword [8]. Scientifically – if it worked at all – it could be explained by a phenomenon like tachyphylaxis.
A more realistic precursor of AIT was the development of vaccination for protecting humans against smallpox infection using putrid secretions from cowpox. The observation was coming to Europe by the British Lady Montague in Turkey and then used by Edward Jenner (Figure 1). who developed a true “vaccine” and gave the name since the material was from cows [9]. He could prove the effects and introduced large vaccination programs, first in England and later all over Europe. It is interesting to note that the first country in the world where a smallpox vaccination was obligatory by law was the Kingdom of Bavaria in 1807 [10].
Figure 1. Edward Jenner (1749 – 1823) English doctor who helped create and popularize a vaccination for smallpox.

At the same time, Samuel Hahnemann brought forward the concept of “homeopathy” based on the observation that the same substances that can induce harm sometimes also may be able to induce protection or cure [11]. According to the philosophy “similia similibus” he tried to treat several diseases with dilutions of the respective elicitors [11]. Hahnemann himself was a scientist, contrary to his successors who continued to use his ideas almost like a religion and exaggerated the phenomenon of dilution by calling it “potentiation”. The biggest difference between homeopathy and AIT is that AIT follows a dose-response regimen, and its effects have been proven by many randomized double-blind placebo controlled clinical trials [12].
Early AIT attempt around the turn of the 19th/20th century
The breakthrough of scientific allergology came at the end of the 19th century following the seminal work of Charles Blackley [13] who proved that pollen are the cause of hay fever and that he could measure the sensitization by skin and provocation tests (Blackley 1873 [13], Figure 2).
Figure 2. Charles Blackley.
Already in 1899, the laryngologist H. Holbrock Curtis [14] (Figure 3) published an exciting article on “The immunizing cure of hay fever” in the Medical News of New York 1900 . In one case, he used subcutaneous injections of an extract of flowers and pollen. Later he treated a small series of patients with a pollen extract, probably by oral application.
Figure 3. H. Holbrooke Curtis.
Also in the United States of America, Rosenau and Anderson [15] observed that the application of heterologous sera (e.g., horse) induced immunity in individuals previously reacting with anaphylaxis. Clemens von Pirquet [16] (Figure 4) had observed similar findings which he noted in his book “Serum sickness” describing a self-experiment on doctor a certain “Doctor v.P.” who showed decreasing local reactions of the skin after intradermal injections.
Figure 4. Clemens Peter Freiherr von Pirquet ( 1874 – 1929) surrounded by colleagues and nurses.

As early as 1903, Philip Dunbar [17] in Hamburg tested the concept of protective immunity which had been developed in the treatment of diphtheria using anti-toxins by Behring [18] who received the first noble prize in Physiology or Medicine in 1901. He produced an hyperimmune serum in animals immunized with pollen extracts, called “pollantin” [17]. Probably this procedure was not really successful due to anaphylactic reactions against the animal serum.
At the same time, Alfred Wolff-Eisner, an immunologist and allergist in Berlin, realized that proteins in the pollen are the triggers of hay fever and performed a pilot study in hay fever patients using the ophthalmo test [19]. This study was not really taken up by the scientific community since it was published in German language in the Berlin “Monatsblätter für Augenheilkunde” [20]. Thus, one cannot criticize Leonard Noon for not quoting his colleague from Germany.
In France, Alexandre Besredka [21] (Figure 5), a student of Metchnikoff, who believed that anaphylaxis also occurred in the brain – an early precursor of the concept of “psycho-neuro-immunology” – performed animal experiments with “vaccination anti-anaphylactique” with increasing doses of diluted allergen solutions.
Figure 5. Alexandre Besredka (1870 – 1940) at the right, next to Alexandre Elias Metchnikoff at the Institute Pasteur, Paris.
In a kind of local immunotherapy, Scheppegrell [22] used a powder of dried pollen applied into the nose as nasal therapy in patients with hay fever.
Noon’s and Freeman’s work
In 1911 Leonard Noon [7] published his seminal article on “prophylactic inocculation against hay fever” in the Lancet (Figure 6). He believed that hay fever is caused by a “soluble toxin” in pollen which is “innocuous to normal individuals”. To detect this “idiosyncrasy” he used an ophthalmo test, which is what we call today a conjunctival provocation test. After studying dose response curves in order to find the right amount, he treated patients with subcutaneous injections of aqueous extracts of pollen from different grasses and could show a reduction of the conjunctival and nasal reactions after the treatment and also provided future prospects to investigate “whether the immunity thus attained is sufficient to carry the patients through a season”, evidence filled by many clinical trials in the 20th century [12, 23, 24].
Figure 6. Leonard Noon (1878 – 1913) in the laboratory.

Unfortunately, Leonard Noon died too young from tuberculosis in 1912, but his work was continued by his colleague John Freeman who published “Further observations on the treatment of hay fever by hypodermic inoculations of pollen vaccine” ([25] (Figure 7). After these articles had appeared, the procedure was taken up rapidly all over the world by physicians treating hay fever patients. Yet it took decades until the first double-blind, placebo-controlled controlled trial was performed. In the 1950s, William “Bill” Frankland in England, who had worked with John Freeman and also with Alexander Fleming, performed a first controlled trial proving that hyposensitization was significantly more effective in higher doses than in a lower dose or when using placebo in the treatment of hay fever [26]. Bill Frankland was an enthusiastic and dedicated physician and researcher who inspired many young allergists not only in the United Kingdom (Figure 8). After a rich and adventurous life – he served as an army physician in Singapore and became imprisoned by the Japanese on the so-called “Hell’s Island” – he died of COVID-19 in 2020 at the age of 108 years [27, 28].
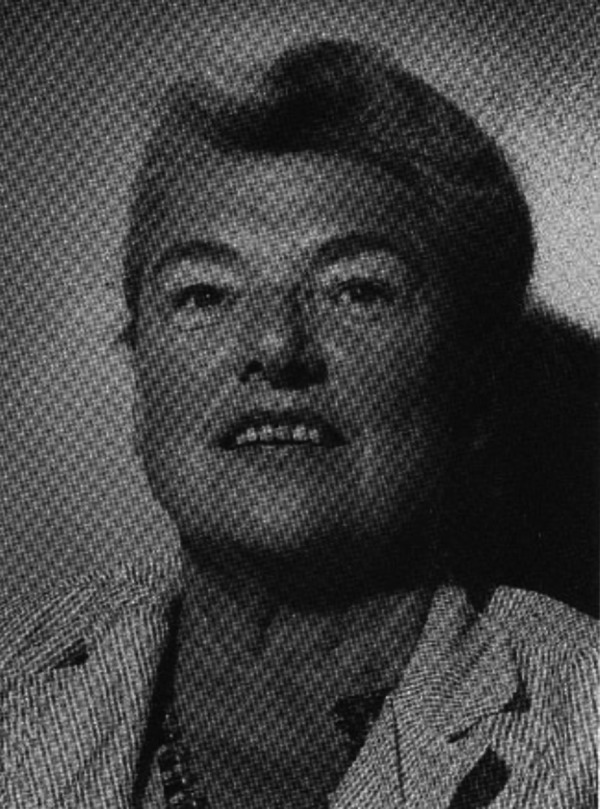
Figure 7. John Freeman (1877 – 1962).

Figure 8. Alfred William „Bill“ Frankland (1912 – 2020) one of the top allergists of the 20th century. Foto: Oliver Pfaar.

Application routes of AIT
AIT is used in many modalities with regard to extract production, modification, adjuvants used, and route of application. In addition to subcutaneous application, other routes have been tried, like oral, nasal, rectal, intradermal, or epicutaneous.
Also injection into a local lymph node was tested in order to induce a stronger immune response [29, 30].
At the end of the last millennium there was a heated and long-lasting debate between supporters of subcutaneous immunotherapy (SCIT) against the newly coming up oral [31, 32, 33, 34] or sublingual application (SLIT) [35]. This debate is closed (Figure 9): sublingual immunotherapy is as effective as the subcutaneous one, which has been proven by a number of excellent and large randomized placebo-controlled clinical trials [36, 37, 38]. Sublingual immunotherapy uses aqueous solutions as droplets and, more recently, lyophilized allergens tablets.
Figure 9. Cover page of the journal “Allergy”.
Innovations in SCIT as the first described AIT application route
Usually, aqueous extracts that were applied through the subcutaneous route (subcutaneous immunotherapy (SCIT)) were used for AIT.
A major problem was the purification of allergens from the plants or animals or house dust. Then, with improved purification procedures, standardization was crucial. In order to compare different allergen extracts, a variety of arbitrary units were used starting with the classical weight/volume (WV) units according to Noon, then advancing to the protein content as protein nitrogen units (PNU), or also describing biological activity with histamine equivalent prick (HEP) or biological allergy units (BAU).
Furthermore, attempts to modify the allergens by chemical treatment were undertaken with the concept of “allergoids”; modification was done by formaldehyde or glutaraldehyde leading to preparations with increased immunogenicity but reduced allergenicity, meaning the frequency of adverse side reactions [39, 40].
Also a variety of adjuvants were used together with the allergens in order to increase the efficacy of the immunological effect in analogy to classical vaccines. Therefore, the most commonly used adjuvant was aluminum hydroxide in the form of semi-depot allergen preparations. Other modalities include tyrosine, calcium phosphate, and monophosphoryl lipid (MPL) [41]. Also in scientific studies, polyethylene glycol-coupled allergens were used [42], and later the Th1-stimulating CpG oligonucleotides [43].
Insect venom allergy
A special chapter in the history of allergen-specific immunotherapy is the treatment of insect venom anaphylaxis. This starts with the observation that beekeepers rarely develop anaphylaxis, while certain allergic individuals with insect venom allergy can suffer from fatal reactions. Therefore, hyposensitization was also tried to treat these conditions. Based on a note by Benson and Semenov who treated a beekeeper, who was anaphylactic and also suffered from asthma, with whole-body extract from bees. They found improvement [44]. Based on this report, a decades-long tradition of using whole-body extracts from bee and wasps started and even was accepted by official documents of the American Academy of Allergy. At the same time, Doctor Mary Loveless (Figure 10) was able to transfer the immunity with beekeeper’s serum thus establishing the concept of “blocking” antibodies [45]. The hobby beekeeper and gifted pharmacist Heinrich Mack from Illertissen, Southern Germany, had the idea to use electrical stimulation to produce a purified bee venom solution which he developed for treating rheumatic diseases under the name “Forapin” [46]. This Forapin was also used by allergists in the 1930s for hyposensitization in bee-sting-induced anaphylaxis [47]. Probably due to side effects, this treatment has never becoming routine.
Figure 10. Mary Hewitt Loveless.
It took until the 1970s in the United States when Larry Liechtenstein and co-workers in Baltimore performed the first double-blind placebo-controlled randomized clinical trial in insect venom allergy using placebo, whole-body extract, and purified bee venom. Whole-body extract was not better than placebo with still 40% of improvement, while bee venom showed an efficacy of over 90% [48]. This study also already showed the often high placebo response rate making clinical studies in allergology so difficult.
Recombinant allergens
A vision of modern allergy researchers was to overcome the standardization problems of allergen extracts by using recombinant allergens, since the molecular nature of major allergens had become known [49]. Some studies indeed showed efficacy of recombinant allergens both from bee venom [50] and from grass pollen [51]. Yet, due to technical and economic as well as regulatory aspects, no company finally was able to transform this concept into routine procedures. So allergists are still dreaming of measuring the allergenic potency of extracts in nanograms or micrograms of relevant molecularly defined allergens.
Guidelines
At the end of the 20th century, national or regional guidelines for allergen specific immunotherapy were developed in many countries and regions and also at an international level under the auspices of the World Allergy Organization [52]. Throughout the recent two decades, an increasing number of national and international systematic reviews, position papers, and guidelines have been published in the field of AIT (some examples: [3, 53, 54, 55]).
The guidelines are following internationally recognized standards, such as the AGREE-II or GRADE methodology, in consenting clinical recommendations based on solid evidence [12, 23, 24]. In addition several aspects of improving methodological standards in conducting clinical trials and assessing efficacy of AIT have been elaborated by international panels of experts in the field [4, 56, 57, 58, 59].
Special emphasis is given to the evidence available for various allergen preparations used in the treatment of allergic diseases. There is no generic efficacy in AIT (in both application routes SCIT and SLIT), and a product-specific evaluation of the safety and efficacy of the individual product investigated in clinical trials is mandatory.
Food allergy
While AIT is obviously effective in airway allergy, there is still a need for patients suffering from food allergy, especially food anaphylaxis [60]. While single case reports and pilot studies have shown efficacy of oral immunotherapy in food allergy, this has not become routine [61]. However, early desensitization protocols have been described already 50 years ago and have been further improved for patients with cow’s milk allergy by Wüthrich [62] in the subsequent decades.
Recently, a standardized preparation has been registered for treating peanut allergy by oral immunotherapy [63]. Other products for subcutaneous use are in the pipeline.
Atopic eczema
While atopic eczema/dermatitis used to be a contraindication for AIT, this is no longer the case. However, the indication for AIT to treat this skin disease is still not supported by the majority of guidelines, although there are pilot studies and also placebo-controlled randomized trials showing a beneficial effect in atopic dermatitis/eczema [64].
AIT during the COVID-19 pandemic
While COVID-19 emerged as a global pandemic as declared by the WHO in March 2020, it also impacted all medical disciplines. Very early during the pandemic, international guidance has been given by the European Academy of Allergy and Clinical Immunology (EAACI) aimed to ensure that patients with respiratory allergic diseases are adequately treated under pandemic restrictions [65, 66, 67, 68]. In addition, straightforward and consensus-based recommendations for both SCIT- and SLIT-treated patients have been proposed internationally [69] and have also been adapted to the situation in German-speaking countries [70]. However, a high grade of heterogeneity of adherence to the academic guidance given has been found in international [71] and national [72] surveys on COVID-19 and AIT suggesting some undertreatment of patients.
Future concepts
Over the last 20 years, many exciting and new therapeutic concepts have been followed in animal experimental and clinical studies, for instance coupling of allergens with microbial products, virus-like particles, or combination with biologics dampening the Th2 response; also T-cell-based epitope vaccines have been developed but have not reached routine clinical use [5, 73].
Also hybrid molecules [74] have been used equally as hypoallergenic iso-allergens [75]. DNA vaccination and gene therapy have been discussed and studied in experimental models [76, 77].
An original idea came from Switzerland with a concept of immunizing cats to induce neutralizing antibodies against the major allergen Fel d 1 [78].
Conclusion
The last 111 years – or 120 if we consider the early scientific reports – can be regarded as a success story of immunologic treatment of allergic diseases. AIT is the only causal treatment of a variety of common allergic diseases besides allergen avoidance, which is not entirely possible for most allergies. With AIT it is possible to modify the pathogenic immune deviation towards tolerance after contact with allergens. Together with allergy diagnosis it remains the backbone of allergological experience which was and is the individual (“personalized”) management of patients suffering from allergic diseases.
Funding
None.
Conflict of interest
JG, OP, KCB and JR declare no conflict of interest.
References
- 1. Ring J Allergy in Practice. Berlin, Heidelberg, New York: Springer;2005. [Google Scholar]
- 2. Bousquet J Khaltaev N Cruz AA Denburg J Fokkens WJ Togias A Zuberbier T Baena-Cagnani CE Canonica GW van Weel C Agache I Aït-Khaled N Bachert C Blaiss MS Bonini S Boulet LP Bousquet PJ Camargos P Carlsen KH Chen Y Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008; 63: 8–160. [DOI] [PubMed] [Google Scholar]
- 3. Roberts G Pfaar O Akdis CA EAACI Guidelines on Allergen Immunotherapy: Allergic rhinoconjunctivitis. Allergy. 2018; 73: 765–798. [DOI] [PubMed] [Google Scholar]
- 4. Bousquet J Pfaar O Togias A Schünemann HJ Ansotegui I Papadopoulos NG Tsiligianni I Agache I Anto JM Bachert C Bedbrook A Bergmann KC Bosnic-Anticevich S Bosse I Brozek J Calderon MA Canonica GW Caraballo L Cardona V Casale T 2019 ARIA Care pathways for allergen immunotherapy. Allergy. 2019; 74: 2087–2102. [DOI] [PubMed] [Google Scholar]
- 5. Pfaar O Agache I de Blay F Bonini S Chaker AM Durham SR Gawlik R Hellings PW Jutel M Kleine-Tebbe J Klimek L Kopp MV Nandy A Rabin RL van Ree R Renz H Roberts G Salapatek AM Schmidt-Weber CB Shamji MH Perspectives in allergen immunotherapy: 2019 and beyond. Allergy. 2019; 74: 3–25. [DOI] [PubMed] [Google Scholar]
- 6. Pfaar O Bousquet J Durham SR Kleine-Tebbe J Larché M Roberts G Shamji MH Gerth van Wijk R One hundred and ten years of Allergen Immunotherapy: A journey from empiric observation to evidence. Allergy. 2022; 77: 454–468. [DOI] [PubMed] [Google Scholar]
- 7. Noon L Cantar B Prophylactic Inoculation against Hay Fever. Lancet. 1911; 177: 1572–1573. [Google Scholar]
- 8. Schadewaldt H Geschichte der Allergie, Band 1-4. 1 ed. München-Deisenhofen: Dustri-Verlag; 1979-1983 [Google Scholar]
- 9. Jenner E An inquiry into the causes and effects of the variolae vacconae. A disease discovered in some of the western counties of England, particularly Gloucestershire. And known by the name oft he cow pox. Londin: Low; 1798. [Google Scholar]
- 10. Giel S Die Schutzpockenimpfung in Bayern, vom Anbeginn ihrer Entstehung und gesetzlichen Einführung bis auf gegenwärtige Zeit, dann mit besonderer Beachtung derselben in anderen Staaten. Munich: Biblitheca Regia Monacensis; 1830. 105. [Google Scholar]
- 11. Hahnemann S Die chronischen Krankheiten, ihre eigentümliche Natur und ihre homöopathische Heilung. Dresden und Leipzig: Arnoldinische Buchhandlung; 1828. [Google Scholar]
- 12. Dhami S Nurmatov U Arasi S Khan T Asaria M Zaman H Agarwal A Netuveli G Roberts G Pfaar O Muraro A Ansotegui IJ Calderon M Cingi C Durham S van Wijk RG Halken S Hamelmann E Hellings P Jacobsen L Allergen immunotherapy for allergic rhinoconjunctivitis: A systematic review and meta-analysis. Allergy. 2017; 72: 1597–1631. [DOI] [PubMed] [Google Scholar]
- 13. Blackley CH Experimental Researches on the Causes and Nature of Catarrhus Aestivus (HAy-Fever or Hay-Asthma). London;Bailliere, Tindeall and Cox; 1873. 73. [Google Scholar]
- 14. Curtis HH The immunizing cure of hay fever. NY Med J. 1900; 77: 16–18. [Google Scholar]
- 15. Rosenau MJ Anderson JF A new toxic Action of Horse Serum. J Med Res. 1906; 15: 179–208. [PMC free article] [PubMed] [Google Scholar]
- 16. Pirquet Cv Schick B Die Serumkrankheit. Leipzig-Wien: 1905. [Google Scholar]
- 17. Dunbar WP Zur Ursache und spec. Heil. Des Heufiebers. Dtsch Med Wochenschr. 1903; 99: 24–28. [Google Scholar]
- 18. Kitasato S. Über das Zustandekommen der Diphterie-Immunität und der Tetanus-Immunität bei Thieren. Dtsch Med Wochenschr. 1890; 16: 1113–1145. [PubMed] [Google Scholar]
- 19. Steidle B Zur Bedeutung der Arbeiten von Alfred Wolff-Eisner für die Immunologie und Allergologie. Monograph Dr thesis, Technical University Munich (TUM). 2022.
- 20. Wolff-Eisner A. Über Heufieberbehandlung, speziell über Pollenschutzapparate. Wochenschrift für Therapie und Hygiene des Auges Berlin. 1909; Oktober 1909: 1: 2-3 und 2: 4-16. [Google Scholar]
- 21. Besredka A Comment empecher l’anaphylaxie? CR Soc Biol. 1907; 59: 1053. [Google Scholar]
- 22. Scheppegrell W The Immunizing Treatment of Hay Fever. NY Med J. 1909; 90: 1099. [Google Scholar]
- 23. Kristiansen M Dhami S Netuveli G Halken S Muraro A Roberts G Larenas-Linnemann D Calderón MA Penagos M Du Toit G Ansotegui IJ Kleine-Tebbe J Lau S Matricardi PM Pajno G Papadopoulos NG Pfaar O Ryan D Santos AF Timmermanns F Allergen immunotherapy for the prevention of allergy: A systematic review and meta-analysis. Pediatr Allergy Immunol. 2017; 28: 18–29. [DOI] [PubMed] [Google Scholar]
- 24. Dhami S Kakourou A Asamoah F Agache I Lau S Jutel M Muraro A Roberts G Akdis CA Bonini M Cavkaytar O Flood B Gajdanowicz P Izuhara K Kalayci Ö Mosges R Palomares O Pfaar O Smolinska S Sokolowska M Allergen immunotherapy for allergic asthma: A systematic review and meta-analysis. Allergy. 2017; 72: 1825–1848. [DOI] [PubMed] [Google Scholar]
- 25. Freeman J Further observations on the treatment of hay fever by hypodermic inoculations of pollen vaccine. Lancet. 1911; 178: 814–817. [PubMed] [Google Scholar]
- 26. Frankland AW Augustin R Prophylaxis of summer hay-fever and asthma: a controlled trial comparing crude grass-pollen extracts with the isolated main protein component. Lancet. 1954; 266: 1055–1057. [DOI] [PubMed] [Google Scholar]
- 27. Ring J William Frankland – obituary. Allergo J Int. 2021.
- 28. Illman J William Frankland: the “grandfather of allergy”. BMJ. 2020; 369: m1717. [Google Scholar]
- 29. Johansen P Häffner AC Koch F Zepter K Erdmann I Maloy K Simard JJ Storni T Senti G Bot A Wüthrich B Kündig TM Direct intralymphatic injection of peptide vaccines enhances immunogenicity. Eur J Immunol. 2005; 35: 568–574. [DOI] [PubMed] [Google Scholar]
- 30. Senti G Prinz Vavricka BM Erdmann I Diaz MI Markus R McCormack SJ Simard JJ Wüthrich B Crameri R Graf N Johansen P Kündig TM Intralymphatic allergen administration renders specific immunotherapy faster and safer: a randomized controlled trial. Proc Natl Acad Sci USA. 2008; 105: 17908–17912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Laetsch C Wüthrich B Zur peroralen Desensibilisierung von Inhalationsallergien im Kindesalter: Behandlungsergebnisse. Schweiz Med Wochenschr. 1973; 103: 342–347. [PubMed] [Google Scholar]
- 32. Clasen I Wüthrich B Neuere Ergebnisse der peroralen Hyposensibilisierung beim kindlichen Asthma bronchiale. Monatsschr Kinderheilkd. 1976; 124: 248. [PubMed] [Google Scholar]
- 33. Wüthrich B Pollinosis des Kindes als Prototyp einer atopischen Krankheit. Monatsschr Kinderheilkd. 1976; 124: 702–705. [PubMed] [Google Scholar]
- 34. Kägi MK Wüthrich B Die orale Hyposensibilsierung und andere Formen der lokalen Immuntherapie. In: Manuale allergologicum. Fuchs E, Schulz KH (eds). München-Deisenhofen: Dustri-Verlag;1999. [Google Scholar]
- 35. Scadding GK Brostoff J Low dose sublingual therapy in patients with allergic rhinitis due to house dust mite. Clin Allergy. 1986; 16: 483–491. [DOI] [PubMed] [Google Scholar]
- 36. Pfaar O Bachert C Kuna P Panzner P Džupinová M Klimek L van Nimwegen MJ Boot JD Yu D Opstelten DJE de Kam PJ Sublingual allergen immunotherapy with a liquid birch pollen product in patients with seasonal allergic rhinoconjunctivitis with or without asthma. J Allergy Clin Immunol. 2019; 143: 970–977. [DOI] [PubMed] [Google Scholar]
- 37. Durham SR Emminger W Kapp A Long-term clinical efficacy in grass pollen-induced rhinoconjunctivitis after treatment with SQ-standardized grass allergy immunotherapy tablet. J Allergy Clin Immunol. 2010; 125: 131-138. [DOI] [PubMed] [Google Scholar]
- 38. Compalati E Canonica GW Passalacqua G Baena-Cagnani CE Considerations about the evaluation of the SLIT meta-analyses. J Allergy Clin Immunol. 2010; 125: 509–, author reply 509-510.. [DOI] [PubMed] [Google Scholar]
- 39. Norman PS Lichtenstein LM Marsh DG Studies on allergoids from naturally occurring allergens. IV. Efficacy and safety of long-term allergoid treatment of ragweed hay fever. J Allergy Clin Immunol. 1981; 68: 460–470. [DOI] [PubMed] [Google Scholar]
- 40. Johansson SG Miller AC Mullan N Overell BG Tees EC Wheeler A Glutaraldehyde-pollen-tyrosine: clinical and immunological studies. Clin Allergy. 1974; 4: 255–263. [DOI] [PubMed] [Google Scholar]
- 41. Johnson AG Tomai M Solem L Beck L Ribi E Characterization of a nontoxic mono phosphoryl lipid. Rev Infect Dis. 1987; 9: 512–516. [DOI] [PubMed] [Google Scholar]
- 42. Lee WY Sehon AH Abrogation of reaginic antibodies with modified allergens. Nature. 1977; 267: 618–619. [DOI] [PubMed] [Google Scholar]
- 43. Creticos PS Schroeder JT Hamilton RG Balcer-Whaley SL Khattignavong AP Lindblad R Li H Coffman R Seyfert V Eiden JJ Broide D Immunotherapy with a ragweed-toll-like receptor 9 agonist vaccine for allergic rhinitis. N Engl J Med. 2006; 355: 1445–1455. [DOI] [PubMed] [Google Scholar]
- 44. Benson RL Semenov H Allergy in its relation to bee sting. J Allergy. 1930; 1: 105–116. [Google Scholar]
- 45. Loveless MH Cann JR Distribution of allergic and blocking activity in human serum proteins fractionated by electrophoresis convection. Science. 1953; 117: 105–108. [DOI] [PubMed] [Google Scholar]
- 46. Hahn G Ostermayer H Über das Bienengift. Ber Dtsch Chem Ges. 1936; 11: 2407–2419. [Google Scholar]
- 47. Lotter G Sensibilisierung für Bienengift durch Typhus-Antitoxin und Desensibilisierung mit Forapin. Munch Med Wochenschr. 1939; 833: 330–331. [Google Scholar]
- 48. Hunt KJ Valentine MD Sobotka AK Benton AW Amodio FJ Lichtenstein LM A controlled trial of immunotherapy in insect hypersensitivity. N Engl J Med. 1978; 299: 157–161. [DOI] [PubMed] [Google Scholar]
- 49. Breiteneder H Pettenburger K Bito A Valenta R Kraft D Rumpold H Scheiner O Breitenbach M The gene coding for the major birch pollen allergen Betv1, is highly homologous to a pea disease resistance response gene. EMBO J. 1989; 8: 1935–1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Müller U Akdis CA Fricker M Akdis M Blesken T Bettens F Blaser K Successful immunotherapy with T-cell epitope peptides of bee venom phospholipase A2 induces specific T-cell anergy in patients allergic to bee venom. J Allergy Clin Immunol. 1998; 101: 747–754. [DOI] [PubMed] [Google Scholar]
- 51. Jutel M Jaeger L Suck R Meyer H Fiebig H Cromwell O Allergen-specific immunotherapy with recombinant grass pollen allergens. J Allergy Clin Immunol. 2005; 116: 608–613. [DOI] [PubMed] [Google Scholar]
- 52. Bousquet J Lockey R Malling HJ Allergen immunotherapy: therapeutic vaccines for allergic diseases. A WHO position paper. J Allergy Clin Immunol. 1998; 102: 558–562. [DOI] [PubMed] [Google Scholar]
- 53. Muraro A Roberts G Halken S Agache I Angier E Fernandez-Rivas M Gerth van Wijk R Jutel M Lau S Pajno G Pfaar O Ryan D Sturm GJ van Ree R Varga EM Bachert C Calderon M Canonica GW Durham SR Malling HJ EAACI guidelines on allergen immunotherapy: Executive statement. Allergy. 2018; 73: 739–743. [DOI] [PubMed] [Google Scholar]
- 54. Agache I Lau S Akdis CA Smolinska S Bonini M Cavkaytar O Flood B Gajdanowicz P Izuhara K Kalayci O Mosges R Palomares O Papadopoulos NG Sokolowska M Angier E Fernandez-Rivas M Pajno G Pfaar O Roberts GC Ryan D EAACI Guidelines on Allergen Immunotherapy: House dust mite-driven allergic asthma. Allergy. 2019; 74: 855–873. [DOI] [PubMed] [Google Scholar]
- 55. Pfaar O Bachert C Bufe A Buhl R Ebner C Eng P Friedrichs F Fuchs T Hamelmann E Hartwig-Bade D Hering T Huttegger I Jung K Klimek L Kopp MV Merk H Rabe U Saloga J Schmid-Grendelmeier P Schuster A Guideline on allergen-specific immunotherapy in IgE-mediated allergic diseases: S2k Guideline of the German Society for Allergology and Clinical Immunology (DGAKI), the Society for Pediatric Allergy and Environmental Medicine (GPA), the Medical Association of German Allergologists (AeDA), the Austrian Society for Allergy and Immunology (ÖGAI), the Swiss Society for Allergy and Immunology (SGAI), the German Society of Dermatology (DDG), the German Society of Oto- Rhino-Laryngology, Head and Neck Surgery (DGHNO-KHC), the German Society of Pediatrics and Adolescent Medicine (DGKJ), the Society for Pediatric Pneumology (GPP), the German Respiratory Society (DGP), the German Association of ENT Surgeons (BV-HNO), the Professional Federation of Paediatricians and Youth Doctors (BVKJ), the Federal Association of Pulmonologists (BDP) and the German Dermatologists Association (BVDD). Allergo J Int. 2014; 23: 282–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pfaar O Demoly P Gerth van Wijk R Bonini S Bousquet J Canonica GW Durham SR Jacobsen L Malling HJ Mösges R Papadopoulos NG Rak S Rodriguez del Rio P Valovirta E Wahn U Calderon MA Recommendations for the standardization of clinical outcomes used in allergen immunotherapy trials for allergic rhinoconjunctivitis: an EAACI Position Paper. Allergy. 2014; 69: 854–867. [DOI] [PubMed] [Google Scholar]
- 57. Shamji MH Kappen JH Akdis M Jensen-Jarolim E Knol EF Kleine-Tebbe J Bohle B Chaker AM Till SJ Valenta R Poulsen LK Calderon MA Demoly P Pfaar O Jacobsen L Durham SR Schmidt-Weber CB Biomarkers for monitoring clinical efficacy of allergen immunotherapy for allergic rhinoconjunctivitis and allergic asthma: an EAACI Position Paper. Allergy. 2017; 72: 1156–1173. [DOI] [PubMed] [Google Scholar]
- 58. Pfaar O Bastl K Berger U Buters J Calderon MA Clot B Darsow U Demoly P Durham SR Galán C Gehrig R Gerth van Wijk R Jacobsen L Klimek L Sofiev M Thibaudon M Bergmann KC Defining pollen exposure times for clinical trials of allergen immunotherapy for pollen-induced rhinoconjunctivitis - an EAACI position paper. Allergy. 2017; 72: 713–722. [DOI] [PubMed] [Google Scholar]
- 59. Pfaar O Agache I Bergmann KC Bindslev-Jensen C Bousquet J Creticos PS Devillier P Durham SR Hellings P Kaul S Kleine-Tebbe J Klimek L Jacobsen L Jutel M Muraro A Papadopoulos NG Rief W Scadding GK Schedlowski M Shamji MH Placebo effects in allergen immunotherapy-An EAACI Task Force Position Paper. Allergy. 2021; 76: 629–647. [DOI] [PubMed] [Google Scholar]
- 60. Pajno GB Fernandez-Rivas M Arasi S Roberts G Akdis CA Alvaro-Lozano M Beyer K Bindslev-Jensen C Burks W Ebisawa M Eigenmann P Knol E Nadeau KC Poulsen LK van Ree R Santos AF du Toit G Dhami S Nurmatov U Boloh Y EAACI Guidelines on allergen immunotherapy: IgE-mediated food allergy. Allergy. 2018; 73: 799–815. [DOI] [PubMed] [Google Scholar]
- 61. de Silva D Rodríguez Del Río P de Jong NW Khaleva E Singh C Nowak-Wegrzyn A Muraro A Begin P Pajno G Fiocchi A Sanchez A Jones C Nilsson C Bindslev-Jensen C Wong G Sampson H Beyer K Marchisotto MJ Fernandez Rivas M Meyer R Allergen immunotherapy and/or biologicals for IgE-mediated food allergy: A systematic review and meta-analysis. Allergy. 2022; 77: 1852–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wüthrich B Oral desensitization with cow’s milk in cow’s milk allergy. Pro! In: Highlights of Food Allergy (hrsg) Wüthrich B, Ortolani C, Monogr Allergy. Vol 32 Basel: Karger; 1996. 236-240. [PubMed] [Google Scholar]
- 63. O’B Hourihane J Beyer K Abbas A Fernández-Rivas M Turner PJ Blumchen K Nilsson C Ibáñez MD Deschildre A Muraro A Sharma V Erlewyn-Lajeunesse M Zubeldia JM De Blay F Sauvage CD Byrne A Chapman J Boralevi F DunnGalvin A O’Neill C Efficacy and safety of oral immunotherapy with AR101 in European children with a peanut allergy (ARTEMIS): a multicentre, double-blind, randomised, placebo-controlled phase 3 trial. Lancet Child Adolesc Health. 2020; 4: 728–739. [DOI] [PubMed] [Google Scholar]
- 64. Werfel T Breuer K Ruéff F Przybilla B Worm M Grewe M Ruzicka T Brehler R Wolf H Schnitker J Kapp A Usefulness of specific immunotherapy in patients with atopic dermatitis and allergic sensitization to house dust mites: a multi-centre, randomized, dose-response study. Allergy. 2006; 61: 202–205. [DOI] [PubMed] [Google Scholar]
- 65. Bousquet J Akdis CA Jutel M Bachert C Klimek L Agache I Ansotegui IJ Bedbrook A Bosnic-Anticevich S Canonica GW Chivato T Cruz AA Czarlewski W Del Giacco S Du H Fonseca JA Gao Y Haahtela T Hoffmann-Sommergruber K Ivancevich JC Intranasal corticosteroids in allergic rhinitis in COVID-19 infected patients: An ARIA-EAACI statement. Allergy. 2020; 75: 2440–2444. [DOI] [PubMed] [Google Scholar]
- 66. Bousquet J Jutel M Akdis CA Klimek L Pfaar O Nadeau KC Eiwegger T Bedbrook A Ansotegui IJ Anto JM Bachert C Bateman ED Bennoor KS Berghea EC Bergmann KC Blain H Bonini M Bosnic-Anticevich S Boulet LP Brussino L ARIA-EAACI statement on asthma and COVID-19 (June 2, 2020). Allergy. 2021; 76: 689–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Pfaar O Klimek L Jutel M Akdis CA Bousquet J Breiteneder H Chinthrajah S Diamant Z Eiwegger T Fokkens WJ Fritsch HW Nadeau KC O’Hehir RE O’Mahony L Rief W Sampath V Schedlowski M Torres MJ Traidl-Hoffmann C Wang Y COVID-19 pandemic: Practical considerations on the organization of an allergy clinic-An EAACI/ARIA Position Paper. Allergy. 2021; 76: 648–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hagemann J Onorato GL Jutel M Akdis CA Agache I Zuberbier T Czarlewski W Mullol J Bedbrook A Bachert C Bennoor KS Bergmann KC Braido F Camargos P Caraballo L Cardona V Casale T Cecchi L Chivato T Chu DK Differentiation of COVID-19 signs and symptoms from allergic rhinitis and common cold: An ARIA-EAACI-GA LEN consensus. Allergy. 2021; 76: 2354–2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Klimek L Jutel M Akdis C Bousquet J Akdis M Bachert C Agache I Ansotegui I Bedbrook A Bosnic-Anticevich S Canonica GW Chivato T Cruz AA Czarlewski W Del Giacco S Du H Fonseca JA Gao Y Haahtela T Hoffmann-Sommergruber K Handling of allergen immunotherapy in the COVID-19 pandemic: An ARIA-EAACI statement. Allergy. 2020; 75: 1546–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Pfaar O Klimek L Worm M [Handling of allergen immunotherapy in the COVID-19 pandemic: An ARIA-EAACI-AeDA-GPA-DGAKI Position Paper (Pocket-Guide)]. Laryngorhinootologie. 2020; 99: 676–679. [DOI] [PubMed] [Google Scholar]
- 71. Pfaar O Agache I Bonini M Brough HA Chivato T Del Giacco SR Gawlik R Gelincik A Hoffmann-Sommergruber K Jutel M Klimek L Knol EF Lauerma A Ollert M O’Mahony L Mortz CG Palomares O Riggioni C Schwarze J Skypala I COVID-19 pandemic and allergen immunotherapy-an EAACI survey. Allergy. 2021; 76: 3504–3516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Pfaar O Hamelmann E Klimek L Taube C Vogelberg C Wagenmann M Werfel T Worm M Allergen immunotherapy during the COVID-19 pandemic-A survey of the German Society for Allergy and Clinical Immunology. Clin Transl Allergy. 2022; 12: e12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Haselden BM Larché M Meng Q Shirley K Dworski R Kaplan AP Bates C Robinson DS Ying S Kay AB Late asthmatic reactions provoked by intradermal injection of T-cell peptide epitopes are not associated with bronchial mucosal infiltration of eosinophils or T(H)2-type cells or with elevated concentrations of histamine or eicosanoids in bronchoalveolar fluid. J Allergy Clin Immunol. 2001; 108: 394–401. [DOI] [PubMed] [Google Scholar]
- 74. Linhart B Hartl A Jahn-Schmid B Verdino P Keller W Krauth MT Valent P Horak F Wiedermann U Thalhamer J Ebner C Kraft D Valenta R A hybrid molecule resembling the epitope spectrum of grass pollen for allergy vaccination. J Allergy Clin Immunol. 2005; 115: 1010–1016. [DOI] [PubMed] [Google Scholar]
- 75. Valenta R Ferreira F Focke-Tejkl M Linhart B Niederberger V Swoboda I Vrtala S From allergen genes to allergy vaccines. Annu Rev Immunol. 2010; 28: 211–241. [DOI] [PubMed] [Google Scholar]
- 76. Bauer R Scheiblhofer S Kern K Gruber C Stepanoska T Thalhamer T Hauser-Kronberger C Alinger B Zoegg T Gabler M Ferreira F Hartl A Thalhamer J Weiss R Generation of hypoallergenic DNA vaccines by forced ubiquitination: preventive and therapeutic effects in a mouse model of allergy. J Allergy Clin Immunol. 2006; 118: 269–276. [DOI] [PubMed] [Google Scholar]
- 77. Steptoe RJ Ritchie JM Harrison LC Transfer of hematopoietic stem cells encoding autoantigen prevents autoimmune diabetes. J Clin Invest. 2003; 111: 1357–1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Thoms F Jennings GT Maudrich M Vogel M Haas S Zeltins A Hofmann-Lehmann R Riond B Grossmann J Hunziker P Fettelschoss-Gabriel A Senti G Kündig TM Bachmann MF Immunization of cats to induce neutralizing antibodies against Fel d 1, the major feline allergen in human subjects. J Allergy Clin Immunol. 2019; 144: 193–203. [DOI] [PubMed] [Google Scholar]


