ABSTRACT
Background
Asthma program in Finland decreased asthma-related mortality and expenses of care on national level, but there is lack of data on adherence to treatment guidelines and disease control on individual level. We aimed to assess adherence to guidelines and disease control among Finnish adult asthmatics.
Methods
Questionnaires were sent in Finland to 2000 randomly selected recipients aged 18–80 years, who had bought medication for obstructive airways disease during the previous 12 months. The questionnaire included questions on asthma medication, exacerbations, self-management and follow-up. Asthma symptom control was assessed by the Asthma Control Test (ACT).
Results
A high proportion (82.4%) of the 541 responders with physician-diagnosed asthma reported regular use of asthma medication and 97.1% of them used inhaled corticosteroids. Almost all (97.0%) of the asthmatics were taught how to use their inhaler and 78.4% had an asthma self-management plan, but only 35.7% reported regular annual follow-up visits. According to symptoms, 60.0% had their asthma well-controlled (ACT score ≥20). On the other hand, 29.2% had a course of oral corticosteroid and 21.8% had an asthma-related unscheduled health care visit during the previous year, but only 2.6% reported a hospitalization. Asthma control was better in those not using regular asthma medication.
Conclusions
The guidelines are well adopted in Finnish adult asthma care except for regular follow-up visits. Majority of patients had good symptom control and hospitalizations were rare. Better asthma control among those not using regular asthma medication implies they are not undertreated but have a mild disease.
KEYWORDS: Asthma, adult, control, symptom, management, guideline, medication, follow-up, exacerbation
Introduction
Asthma is a common disease causing significant economic burden and morbidity especially when uncontrolled [1]. Asthma guidelines therefore advocate lung function measurements in diagnosing asthma and treatment with inhaled corticosteroids (ICS) [2–4]. Finland and several other countries have also launched national asthma programs to implement the guidelines to reduce asthma mortality and morbidity [5–7]. The 10-year Finnish Asthma Program was initiated in 1994 and the aims of the program were early diagnosis of asthma confirmed with objective lung function tests, regular treatment with ICS, good asthma control, and reduction in the costs of asthma [6]. A key strategy of implementation was the establishment of local asthma coordinators in health care centers to coordinate and ensure high quality of asthma management in primary health care. The pharmacies also committed to provide instructions on asthma medication and proper inhalation technique for individual asthmatics. During the program, around 800 educational sessions were arranged with over 35,000 participants of health care professionals [6]. Despite the increase in asthma incidence during the program, the morbidity and costs of asthma decreased while the main responsibility of asthma diagnostics and treatment was successfully redirected to primary health care [6].
Mostly, the impact and success of implementation of national asthma programs have been assessed on societal level based on registry data on, e.g. mortality, sick days and hospitalizations [8–10]. The remaining asthma exacerbations and hospitalizations may reflect either poorly treated asthma or severe asthma that is not controlled with current medication [2]. Although register data show mortality and morbidity on national level, they do not reveal how treatment on individual level is associated to poor outcomes. There is less data on the impact of guidelines on individual asthmatics including the guidance and treatment they receive, and how this is associated to their symptom control and rate of asthma exacerbations. Asthma is usually well controlled in majority of patients in clinical trials [11], but less than 50% is reported controlled in most population-based studies [12–15]. This has raised concerns over implementation of guidelines and management of asthma in real-life.
The aim of this postal questionnaire study was to examine the application of national asthma guidelines on individual patient level, current control of asthma, and how these are related among Finnish adult asthmatics.
Materials and methods
Study design and population
The Finnish Social Insurance Institution (FSII) records all prescription medications bought in Finland. Since there are no over-the-counter medications available in Finland for obstructive airway diseases (the Anatomical Therapeutic Chemical [ATC] Classification System code R03) [16], all R03 medications bought are recorded with the patient identity. In 2017, the population of Finland was 5,513,130 subjects, and 539,078 of them had purchased any R03 medication at least once during the previous year. A postal questionnaire study was conducted in April 2017 to a random sample of 2000 Finnish speaking subjects aged 18–80 years, who had bought R03 medication during the previous 12 months and lived in Finland. Reminders were sent twice. The corrected sample size was 1978 subjects after exclusion of subjects with unsuccessful postal delivery of the questionnaire or non-analyzable data (Figure 1). A written informed consent included in the questionnaire was obtained from all responders. The study protocol was accepted by the Ethics Committee of Tampere University Hospital (Approval number R15186).
Figure 1.
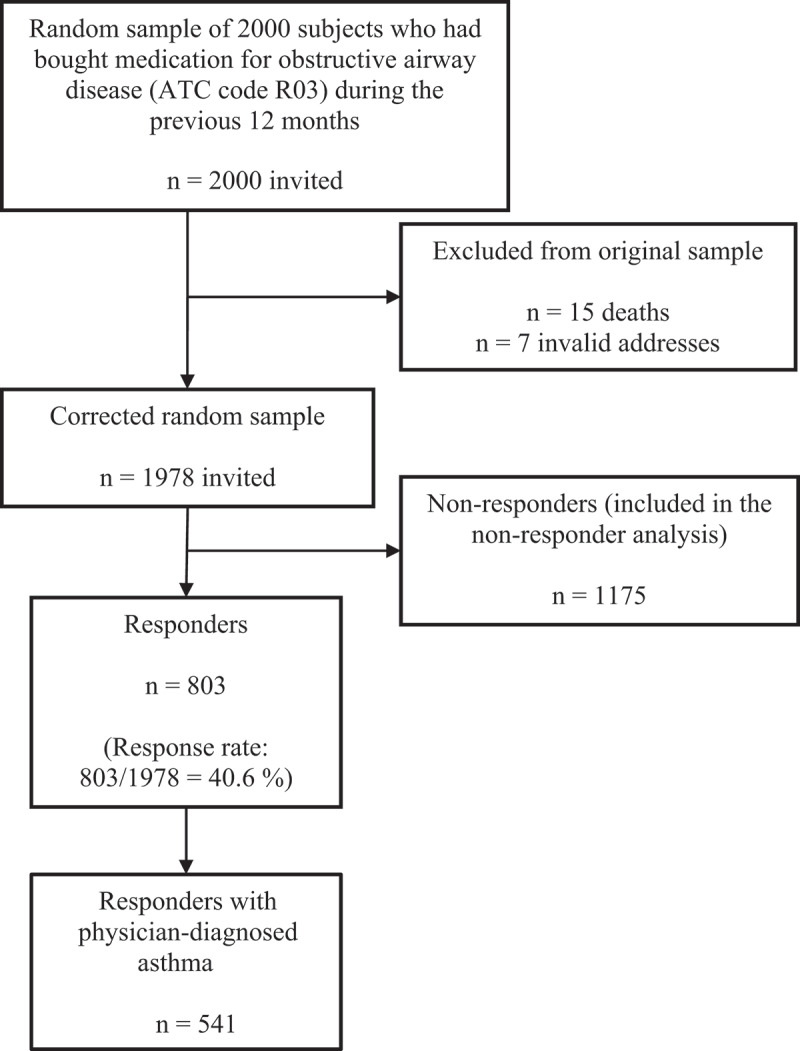
Study flow chart. ATC = the Anatomical Therapeutic Chemical Classification System.
Questionnaire and definitions
Questions and definitions most relevant to the present study are outlined below.
Asthma was defined by a positive answer to the question ‘Do you have a physician-diagnosed asthma?’.
Asthma medication and management
We inquired about the use of asthma medication both regularly/daily and as needed or short-term courses, and whether the responder had been taught how to correctly use their inhaler and had an asthma self-management plan. We also included questions on asthma follow-up visits (scheduled annual or other).
Asthma symptom control was assessed with the Asthma Control Test (ACT) and was considered well controlled with 20–25 points, partly controlled with 16–19 points and poorly controlled with 5–15 points [17].
Asthma exacerbation rate was assessed during 12 months prior to the survey by asking whether the responder in this time had to temporarily increase their asthma controller medication (mild exacerbation), required a course of oral corticosteroid (OCS) or had an asthma-related unscheduled health care visit or emergency department [ED] visit (moderate exacerbation), or hospitalization (severe exacerbation).
Entitlement to special reimbursements for asthma medication
A person with a persistent physician-diagnosed asthma confirmed by lung function tests and a need for long-term asthma medication is entitled to special reimbursement for expenses of asthma medication granted by the FSII.
English translations of the questions in the postal questionnaire are in the supplementary material (Supplementary Figure E1).
Statistical analysis
Statistical analyses were performed using SPSS Statistics version 25 (IBM Corp., Amonk, NY, USA). Mann–Whitney U test was used for continuous and Pearson chi-square -test for categorical variables. A p-value < 0.05 was considered significant.
Results
A total of 803 subjects responded yielding a response rate of 40.6%. The responders were on average slightly older, more often women, and they had slightly less often special reimbursement for asthma medication (Supplementary Table E1).
Characteristics of responders with physician-diagnosed asthma
Of the 803 responders, 541 (67.4%) reported a physician-diagnosed asthma (Table 1). Smokers were included in the study population and the ever-smokers had smoked a median of 10.0 pack-years (Interquartile range [IQR] 3.8–20.8). Of the responders with asthma, 46 (8.5%) reported also a physician-diagnosed chronic obstructive pulmonary disease (COPD). Other reported respiratory diseases were acute bronchitis, emphysema, sarcoidosis, bronchiectasis, pulmonary fibrosis, asbestosis, sleep apnoea, pulmonary embolism, lung cancer, tuberculosis, pulmonary hypertension, pulmonary lymphoma, chronic lung transplant rejection, lung atelectasis, bronchiolitis obliterans organizing pneumonia, lymphangioleiomyomatosis and sequalae of lung resection.
Table 1.
Characteristics of responders with physician-diagnosed asthma.
| Total | 541 |
|---|---|
| Age (years) | 62.0 (50.0–70.0) |
| Females | 333 (61.6) |
| BMI (kg/m2) | 27.4 (24.3–31.2) |
| Smoking status* Current Ex Never |
74 (13.8) 177 (33.0) 286 (53.2) |
| Physician-diagnosed COPD | 46 (8.5) |
| Physician-diagnosed allergy to pollen or animals or both | 276 (51.0) |
Data are presented as n (%) or median (IQR) *4 subjects excluded because of missing answer on smoking habits. BMI = body mass index. COPD = chronic obstructive pulmonary disease.
Use of asthma medication
Of the responders with physician-diagnosed asthma, 446 (82.4%) reported using regular asthma medication (Table 2), and 433 (97.1%) of them reported having an ICS and 264 (59.2%) long-acting β2-agonist (LABA) containing regimen. Thirteen responders reported regular use of asthma medication but not using ICS. Among these responders, four used leukotriene receptor antagonist (LTRA), eight used short-acting β2-agonist (SABA) regularly, and one reported only regular use of OCS. None reported using LABA or long-acting muscarinic antagonist (LAMA) regularly without concurrent ICS or LTRA.
Table 2.
Use of asthma medication among responders with physician-diagnosed asthma.
| All responders with asthma | Responders reporting regular use of asthma medication | Responders reporting courses or as-needed use of asthma medication | |
|---|---|---|---|
| Total | 516* | 446 | 70 |
| ICS** | 489 (94.8) | 433 (97.1) | 56 (80.0) |
| LABA** | 286 (55.4) | 264 (59.2) | 22 (31.4) |
| LAMA** | 41 (7.9) | 41 (9.2) | 0 (0.0) |
| LTRA | 84 (16.3) | 81 (18.2) | 3 (4.3) |
| SABA/SAMA** | 362 (70.2) | 308 (69.1) | 54 (77.1) |
Data are presented as n (%). *Excluded 25 responders who had not specified the used asthma medication **Alone or fixed combination inhaler. ICS = inhaled corticosteroid. LABA = long-acting β2-agonist. LAMA = long-acting muscarinic antagonist. LTRA = leukotriene receptor antagonist. SABA = short-acting β2-agonist. SAMA = short-acting muscarinic antagonist. Note: triple combination inhalers (ICS+LABA+LAMA) were not available at the time of the study.
Only 70 (12.9%) responders with asthma reported that they did not use regular asthma medication. They reported use of ICS in courses or as needed as often as SABA and/or short-acting muscarinic antagonist (SAMA) (80.0% vs 77.1%, respectively) (Table 2). None reported sole use of LABA/LAMA as needed.
Management of asthma
Guidance on inhaler technique
With 33 missing answers excluded, 493 (97.0%) of the responders with asthma reported having been taught the correct inhaler technique (138 [28.0%] by a doctor, 225 [45.6%] by a nurse, 32 [6.5%] by a pharmacist, and 98 [19.9%] by more than one of the previous) and 15 (3.0%) reported not having had any instructions on how to use their inhaler.
Self-management plan
Of the responders with asthma, 424 (78.4%) reported having an asthma self-management plan (Figure 2).
Figure 2.
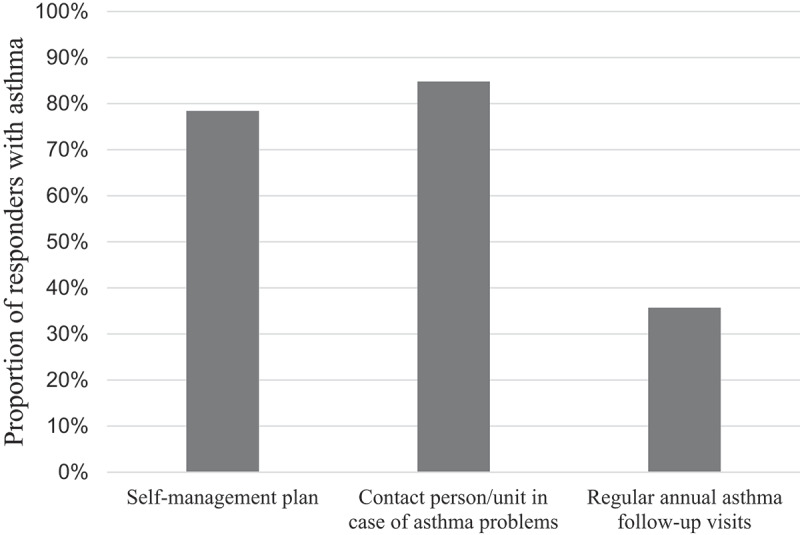
Proportions of subjects reporting a self-management plan and asthma-related control visits among responders with physician-diagnosed asthma.
Follow-up
Of the responders with asthma, 193 (35.7%) reported scheduled annual follow-up visits (Figure 2). In addition, 310 (57.3%) visited at least once (scheduled or unscheduled) a health care professional due to asthma during the previous year: 91 (16.8%) a specialist of respiratory medicine, 252 (46.6%) a primary care physician and/or 145 (26.8%) a nurse. Also, 458 (84.8%) responders were aware whom or which unit to contact in case of problems with asthma treatment, and the contact was in 348 (64.3%) responders in primary or occupational health care. Other reported contacts were a specialist of respiratory medicine, other unspecified healthcare professional (e.g. a doctor or a nurse) and ED in 30 (5.5%), 53 (9.8%) and 13 (2.4%) subjects, respectively.
Medication reimbursement
Of the responders with asthma, 410 (75.8%) had a special reimbursement for asthma medication.
Asthma symptom control
The ACT was completed by 527 (97.4%) responders with physician-diagnosed asthma and the median score was 21 (range 5–25, IQR 17–23). Asthma was well controlled in 316 (60.0%), partly controlled in 113 (21.4%) and poorly controlled in 98 (18.6%) responders (Figure 3a). The corresponding percentages were 62.6%, 21.5% and 15.9% in the 484 responders with asthma only, and 30.2%, 20.9% and 48.8% in the 43 responders with both asthma and COPD (p < 0.001). The responses to each of the five questions of the ACT are given in Figure 3b.
Figure 3.

(a) Asthma symptom control according to the Asthma Control Test (ACT). (b) Proportions of responses to each choice of the questions in the Asthma Control Test.
Asthma exacerbations
There were 365 (67.5%) responders with asthma who reported an asthma exacerbation during the previous year as shown in Figure 4 (12 missing answers). More in detail, 329 (60.8%) responders had to increase temporarily their controller medication during the previous year and 305 reported the number of times they had to do it: 54 (10.0% of all asthmatics) once, 91 (16.8%) twice and 162 (29.9%) three or more times. Of the responders, 158 (29.2%) had taken at least one course of OCS for respiratory symptoms during the previous year: 83 (15.3% of all asthmatics) one course, 42 (7.8%) two and 29 (5.4%) three or more courses (4 missing answers on the number of courses). In addition, 118 (21.8%) subjects had had an asthma-related unscheduled health care or ED visit during the previous year: 58 (10.7% of all asthmatics) one visit, 34 (6.3%) two visits and 25 (4.6%) three or more visits (1 missing answer on the number of visits). Only 14 (2.6%) responders reported a hospitalization due to asthma. Altogether 201 (37.2%) had at least one asthma exacerbation in the last year that was considered moderate or severe.
Figure 4.
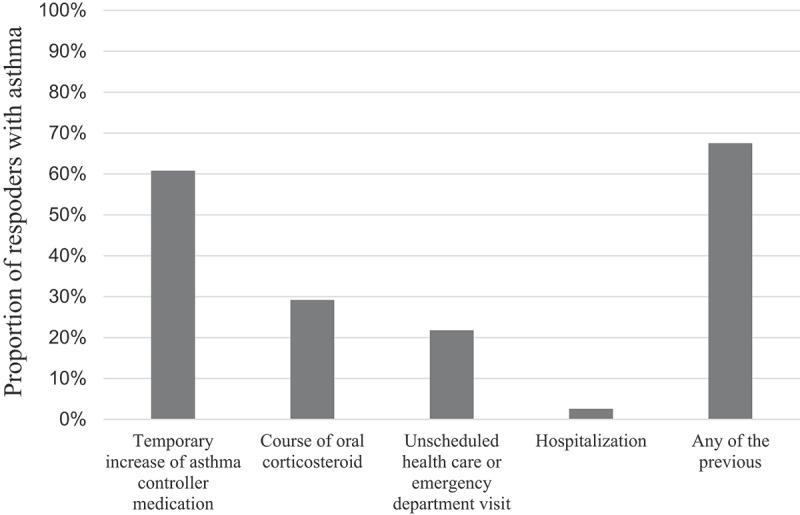
Proportions of subjects reporting different indicators of asthma exacerbations during the previous 12 months.
Of the responders with asthma only, 61.8% had to temporarily increase their controller medication, 28.7% had course(s) of OCS, 21.2% unscheduled health care visit and 1.6% hospitalization during the previous year. The corresponding percentages were 50.0%, 34.8%, 28.3% and 13.0% in responders with both asthma and COPD. These differences were statistically significant only for the percentage of subjects being hospitalized (p < 0.001).
Asthma symptom control and exacerbations according to the use of regular asthma medication and annual follow-up
Asthmatic subjects without regular asthma medication had higher median ACT-score compared to those with regular asthma medication (22 [IQR 20–24] vs 21 [IQR 16-23], p = 0.001) and their asthma was more often well controlled (76.1% vs 57.3%, p = 0.003) and less often poorly controlled (4.5% vs 20.5%, p = 0.002). Subjects without regular asthma medication reported less often temporal increase of controller medication (50.0% vs 65.9%, p = 0.01) and course(s) of OCS (17.2% vs 32.9%, p = 0.01) due to asthma during the previous year, but no significant difference was found in unscheduled health care visits between the groups (16.4% vs 23.0%, p = 0.23). None of the responders without regular asthma medication reported hospitalization in the previous year.
When comparing responders with annual asthma follow-up visits to those without, the annual visitors had more often regular asthma medication (92.7% vs 80.5%, p < 0.001), regular ICS (90.9% vs 76.5%, p < 0.001) and self-management plan (86.4% vs 76.0%, p = 0.004), but had less often well-controlled asthma (51.6% vs 64.3%, p = 0.004) and more often asthma exacerbations during the previous year (temporal increase of asthma medication 70.5% vs 57.8% [p = 0.004], OCS course 39.9% vs 23.6% [p < 0.001], unscheduled health care visit 33.9% vs 16.0% [p < 0.001] and hospitalization 5.8% vs 0.9% [p = 0.001]) than the annual non-visitors (no significant difference in age, sex, BMI, smoking status or guidance on inhaler technique).
We also compared responders with well-controlled asthma (ACT score 20–24, n = 256) to those with totally controlled (ACT 25, n = 60) asthma, and there were no statistically significant differences in need for temporal increase of asthma medication, OCS course, unscheduled health care visits or hospitalization during the preceding year. Furthermore, there were no significant differences in the use of regular ICS or proportions of subjects who used single ICS or ICS+LABA combinations between the groups.
Discussion
Most of the Finnish adult asthmatics reported using asthma medication regularly, and a vast majority of them used ICS. Only 3% had not been taught how to use their inhaler. Most subjects reported having a self-management plan and a unit to contact in case of possible problems, but only about a third had regular annual asthma control visits. Accordingly, 60% had a good asthma symptom control (ACT score ≥20). Less than 3% of the asthmatics had been hospitalized due to asthma, but milder asthma exacerbations were common with about 60% reporting a temporary increase of asthma medication and 30% a course of OCS during the previous year. Importantly, asthma symptom control was better and there were no asthma-related hospitalizations among subjects without regular asthma medication.
Over 80% of asthmatics in the present study reported using regular medication for their asthma and almost all of them used ICS. Only 13% did not use asthma medication regularly and still 80% of them used ICS as needed or in courses. Also, there were no subjects using LABA only, which is in line with current recommendations [18]. Even though regular ICS is the mainstay treatment to control asthma [2], there have been concerns over inadequate use among asthmatics [19]. Prevalence of asthmatics using regular controller medication has varied from 30% to 60% in surveys from different countries [12,13,20]. During the Finnish Asthma Program, use of ICS increased by 75% [21] and 6 years after the program in 2010, 96% of Finnish asthmatics reported using ICS maintenance therapy [22]. According to our study results, regular ICS treatment continues to be well adopted to Finnish adult asthma care. One should also acknowledge that treatment step-down and possible overtreatment, though important aspects, were not the subject of this analysis.
Under 40% of the responders with asthma in our study had regular annual follow-up visits and little over half reported having visited a health care professional due to asthma during the previous year. Regular follow-up of asthmatics have been also reported from other studies to fall short of recommendations [2,4]. Accordingly, in a Finnish longitudinal study adult-onset asthmatics had a follow-up visit on average every third year [23] and in Sweden, only 36% of asthmatics reported annual control visits [24]. Almost 80% of asthmatics from US had a control visit in the previous year, but the visit was mainly due to acute symptoms [25]. A better result was with self-management as nearly 80% of asthmatics in our study reported having a self-management plan and almost all were taught how to use their asthma inhaler. In previous reports from Canada, Britain and Europe, 11% [12], 23% [26] and 30% [27] of the patients with asthma, respectively, had personalized/written asthma action plan. One of the goals of the Finnish Asthma Program was to implement the use of guided self-management in asthma management including patient education, use of peak flow meter (PEF) and guidance on how to adjust the asthma medication according to PEF measurements [6]. However, in southern Finland in 1999 a guided self-management was used only in 46% of asthmatics [6]. The results from previous studies are notably better for inhaler technique training as 67–85% of patients have reported having one [22,26,28]. According to our study, self-management of asthma appears to have improved over the years and is presently well adopted to the treatment of Finnish adult asthmatics. The limitation of the study was that we did not request the responder to specify the individual self-management plan.
In the present study, 60% of asthmatics had a well-controlled disease (ACT score ≥20). In clinical trials well-controlled asthma is achievable in about 70% of asthmatics [11], but in real-life, well-controlled asthma is mostly reported in under 50% of patients. In previous surveys, the proportion of well-controlled asthma has been 52% and 20% in Europe [13,29], 47% in Canada [12], 30% in USA [14], and only about 8% in Asia-Pacific region [15]. The current result is slightly better than reported from these other studies worldwide, but similar to those from Italy and Australia, where 64% [30] and 54% [20] of asthmatics, respectively, were well controlled.
During the last year, almost 2/3 of the responders had to increase at least once their asthma medication, nearly a third had a course of OCS, little over 20% had an asthma-related unscheduled health care visit, but the hospitalization rate was under 3%. This would indicate that milder asthma exacerbations are quite frequent among Finnish adult asthmatics but more severe exacerbations are rare. Similar results have been reported from UK and Korea with 19% [31] and 44% [32], respectively, of asthmatics needing a course of OCS per year and with low rate of hospitalization [32]. However, in database studies from US and UK moderate or severe exacerbation per year were found in 13% and 8% of asthmatics, respectively [33]. In a cohort of Northern European asthmatics, only 9% had a moderate exacerbation in 12 months and 8% had to increase the dosage of ICS [34]. Moreover, self-reported hospitalizations have been published to continuously decrease among studied asthma cohorts in Finland (in 2001 18% and in 2010 6%) but the proportion of subjects needing OCS courses have remained the same (36%) [22]. It appears that severe asthma exacerbations have continuously decreased in Finland but there has not been a change regarding moderate exacerbations.
Since our study was a questionnaire, we did not have lung function measurements available. A Finnish single-center study has previously reported 72% of adult-onset asthmatics to have controlled asthma according to symptoms but with stricter criteria of no exacerbations and normal lung function for controlled disease, only 34% had controlled asthma [35]. When comparing studies, the definition of asthma control is pivotal.
Inadequate use of ICS is one of the factors associated with asthma exacerbations [36]. In the present study, only 13% of asthmatics did not use regular asthma medication and they actually reported less often asthma exacerbation in the previous year and better symptom control of asthma than the asthmatics with regular medication. Similar result was recently published in a Finnish study on adult-onset asthmatics, except they did not find difference in symptom scores [37]. At least among Finnish adult asthmatics, it would appear that inadequate use of medication is not the reason for suboptimal asthma control, in contrary to previous reports [30]. Co-diagnosis of COPD in asthma patients has also in previous studies been associated with higher exacerbation rates as well as lower quality of life than in asthma only [38,39]. This is in line with our finding on the poorer symptom control in subjects with asthma and COPD. However, in our study the difference in the numbers of exacerbations between these groups was only significant in regard of hospitalizations, and this could be related to the quite small number of subjects with asthma and COPD (n = 46).
The subjects with annual asthma follow-up reported more often use of regular asthma medication and regular use of ICS, as well as having a self-management plan than the ones without annual visits. On the other hand, the annual visitors had less often well-controlled asthma and more often mild to severe asthma exacerbations. In another Finnish study by Takala et al., no difference was found in asthma control or lung function between adult-onset asthmatics with frequent or less frequent asthma contacts, but the asthmatics with more frequent contacts had more often regular ICS and higher adherence to ICS, which is in line with our study [23]. This might suggest that more symptomatic, less-controlled asthmatics with more difficult disease are keener to adhere to regular medication and follow-up [23].
Our sample was obtained from adult asthmatics who had bought any R03 medication at least once during the previous year. We thus missed those asthmatics who did not use any medication. These are most likely subjects with very mild and less symptomatic asthma and their proportion is probably quite low. Exclusion of very mild asthmatics may underestimate asthma control while exclusion of subjects totally ignoring asthma treatment would overestimate the results. However, it is likely that symptomatic subjects with poor compliance of controller medication still use short-acting reliever medication and therefore, would have been included in the sample. A recall bias is always possible in a questionnaire study. On the other hand, a strength of the study was that it comprised a large unselected sample of Finnish adult asthmatics using any kind of asthma medication. The responders were quite similar to non-responders of the study and our sample therefore probably allows reliable estimation on the adult asthmatic population in Finland.
Conclusions
Asthma treatment guidelines and clinical practice are well aligned in Finland and the achieved asthma control among adults is good. Most of the responders with asthma report regular use of ICS and having a self-management plan, but only about a third report regular annual follow-up visits. Sixty percent of the responders report good asthma symptom control and hospitalizations are rare, but milder exacerbations are more frequent and these are mostly self-treated by increasing inhaled medication and about a third of the asthmatics report having used at least one course of OCS during the previous year. Among asthmatics not using regular medication, as-needed ICS was used by as many subjects as as-needed SABA. Asthma control was better in subjects not on regular medication, suggesting that there is no significant undertreatment of asthma. Further action should focus on promoting regular follow-up visits and to find out if the number of milder exacerbations can be reduced with the currently available treatment options.
Supplementary Material
Biographies
Johanna Pakkasela is a specialist in Respiratory Medicine at Tampere University Hospital, Finland. Her research focuses on asthma, allergy and outcomes of patients with asthma.
Petri Salmela is a specialist in Respiratory Medicine at Tampere University Hospital, Finland. His research focuses on outcomes and management of patients with chronic obstructive respiratory diseases.
Pekka Juntunen is specialising in Respiratory Medicine at Tampere University, Finland. His research focuses on outcomes and management of patients with chronic obstructive respiratory diseases.
Jussi Karjalainen is Head of the Allergy Centre at Tampere University, Finland. His research focuses on phenotypes and clinical and occupational outcomes among patients with asthma.
Lauri Lehtimäki is a Professor of Respiratory Medicine at Tampere University, Finland. His recent research focuses on airway inflammation in asthma, COPD and occupational lung diseases.
Funding Statement
This study was supported by grants from Tampere Tuberculosis Foundation, Competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital, the Research Foundation of the Pulmonary Diseases, Allergy Research Foundation, and the Foundation of the Finnish Anti-Tuberculosis Association.
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/20018525.2022.2149918.
Contribution
JP, JK and LL designed the study, created the questionnaire and collected the data. JP, PS and PJ conducted the statistical analyses with help from LL and JK. JP, PS, PJ, JK and LL interpreted the data, critically reviewed the manuscript, read and approved the manuscript before submission.
Data availability statement
Data available on request from the authors.
Disclosure statement
The authors report no conflicts of interest related to this study.
Disclaimer
None of the funders were involved in the planning, execution, drafting or write-up of this study.
References
- [1].Masoli M, Fabian D, Holt S, et al. Global Initiative for Asthma (GINA) Program. The global burden of asthma: executive summary of the GINA dissemination committee report. Allergy. 2004;59(5):469–10. [DOI] [PubMed] [Google Scholar]
- [2].GINA. Global Initiative for Asthma (GINA) . Global strategy for asthma management and prevention. https://ginasthma.org/wp-content/uploads/2020/06/GINA-2020-report_20_06_04-1-wms.pdf. Date last accessed: September 13, 2020. <misc>Date last updated: 2020.
- [3].BTS/SIGN British guideline on the management of asthma , 2019. Date last accessed: May 4, 2020. Date last updated: 2020. Date last updated: 2019 May 4. Available from: https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/
- [4].Asthma. Current Care Guidelines . Working group set up by the Finnish Medical Society Duodecim, the Finnish Respiratory Society, the Finnish Paediatric Society, the Finnish Society of Clinical Physiology. Helsinki: The Finnish Medical Society Duodecim, 2022. Date last accessed: November 20, 2022. Date last updated: 2022. Date last accessed: https://www.kaypahoito.fi/hoi06030 [Google Scholar]
- [5].Boulet L-B, Dorval E, Labrecque M, et al. Towards excellence in asthma management: final report of an eight-year program aimed at reducing care gaps in asthma management in Quebec. Can Respir J. 2008;15(6):302–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Haahtela T, Tuomisto, LE, Pietinalho, A , et al. A 10 year asthma programme in Finland: major change for the better. Thorax. 2006;61(8):663–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Woolcock A, Rubinfeld A, Seale P, et al. Asthma management plan, 1989. Med J Aust. 1989;151(11–12):650–653. [PubMed] [Google Scholar]
- [8].Haahtela T, Herse F, Karjalainen J, et al. The Finnish experience to save asthma costs by improving care in 1987-2013. J Allergy Clin Immunol. 2017;139(2):408–414.e2. [DOI] [PubMed] [Google Scholar]
- [9].McCaul KA, Wakefield MA, Roder DM, et al. Trends in hospital readmission for asthma: has the Australian National Asthma campaign had an effect? Med J Aust. 2000;172(2):62–66. [DOI] [PubMed] [Google Scholar]
- [10].Soto-Martínez M, Avila L, Soto N, et al. Trends in hospitalizations and mortality from asthma in CostaRica over a 12- to 15-year period. J Allergy Clin Immunol Pract. 2014;2(1):85–90. [DOI] [PubMed] [Google Scholar]
- [11].Bateman ED, Boushey HA, Bousquet J, et al. Can guideline-defined asthma control be achieved? The gaining optimal asthma control study. Am J Respir Crit Care Med. 2004;170(8):836–844. [DOI] [PubMed] [Google Scholar]
- [12].FitzGerald JM, Boulet L-P, McIvor RA, et al. Asthma control in Canada remains suboptimal: the Reality of Asthma Control (TRAC) study. Can Respir J. 2006;13(5):253–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Price D, Fletcher M, van der Molen T.. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to symptoms and experience (REALISE) survey. npj Prim Care Respir Med. 2014;24(1):14009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Murphy KR, Meltzer EO, Blaiss MS, et al. Asthma management and control in the USA: results of the 2009 Asthma Insight and Management survey. Allergy Asthma Proc. 2012;33(1):54–64. [DOI] [PubMed] [Google Scholar]
- [15].Gold LS, Thompson P, Salvi S, et al. Level of asthma control and health care utilization in Asia-Pacific countries. Respir Med. 2014;108(2):271–277. [DOI] [PubMed] [Google Scholar]
- [16].WHO Collaborating Centre for Drug Statistics Methodology , guidelines for ATC classification and DDD assignment 2020. Oslo: Norway, 2019. Date last accessed: Mar 15, 2020. Date last updated: 2020. Date last updated: 2020 Mar 15. Available from: https://www.whocc.no/filearchive/publications/2020_guidelines_web.pdf [Google Scholar]
- [17].Schatz M, Sorkness CA, Li JT, et al. Asthma control test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117(3):549–556. [DOI] [PubMed] [Google Scholar]
- [18].Weatherall M, Wijesinghe M, Perrin K, et al. Meta-analysis of the risk of mortality with salmeterol and the effect of concomitant inhaled corticosteroid therapy. Thorax. 2010;65(1):39–43. [DOI] [PubMed] [Google Scholar]
- [19].Janson C, de Marco, R, Accordini, S, et al. Changes in the use of anti-asthmatic medication in an international cohort. Eur Respir J. 2005;26(6):1047–1055. [DOI] [PubMed] [Google Scholar]
- [20].Reddel HK, Sawyer SM, Everett PW, et al. Asthma control in Australia: a cross-sectional web-based survey in a nationally representative population. Med J Aust. 2015;202(9):492–496. [DOI] [PubMed] [Google Scholar]
- [21].Haahtela T, Klaukka, T, Koskela, K, et al. Asthma programme in Finland: a community problem needs community solutions. Thorax. 2001;56(10):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kauppi P, Peura S, Salimäki J, et al. Reduced severity and improved control of self-reported asthma in Finland during 2001-2010. Asia Pac Allergy. 2015;5(1):32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Takala J, Ilmarinen P, Tuomisto LE, et al. Planned primary health care asthma contacts during 12-year follow-up after Finnish national Asthma programme: focus on spirometry. npj Prim Care Respir Med. 2020;30(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Axelsson M, Ekerljung L, Lundbäck B. The significance of asthma follow-up consultations for adherence to asthma medication, asthma medication beliefs, and asthma control. Nurs Res Pract. 2015;2015:139070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Yawn BP, Rank MA, Cabana MD, et al. Adherence to asthma guidelines in children, tweens, and adults in primary care settings: a practice-based network assessment. Mayo Clin Proc. 2016;91(4):411–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Royal College of Physicians . Why asthma still kills: the National Review of Asthma Deaths (NRAD) confidential enquiry report. London: RCP, 2014. Date last accessed: Apr 20, 2020. Date last updated: 2020. Date last updated: 2014 Apr 20. Available from: https://www.rcplondon.ac.uk/projects/outputs/why-asthma-still-kills. [Google Scholar]
- [27].Cazzoletti L, Marcon A, Janson C, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol. 2007;120(6):1360–1367. [DOI] [PubMed] [Google Scholar]
- [28].Giraud V, Allaert F-A, Roche N. Inhaler technique and asthma: feasibility and acceptability of training by pharmacists. Respir Med. 2011;105(12):1815–1822. [DOI] [PubMed] [Google Scholar]
- [29].Vervloet D, Williams AE, Lloyd A, et al. Costs of managing asthma as defined by a derived Asthma Control TestTM score in seven European countries. Eur Respir Rev. 2006;15(98):17–23. [Google Scholar]
- [30].Allegra L, Cremonesi G, Girbino G, et al. Real-life prospective study on asthma control in Italy: cross-sectional phase results. Respir Med. 2012;106(2):205–214. [DOI] [PubMed] [Google Scholar]
- [31].Price DB, Rigazio A, Campbell JD, et al. Blood eosinophil count and prospective annual asthma disease burden: a UK cohort study. Lancet Respir Med. 2015;3(11):849–858. [DOI] [PubMed] [Google Scholar]
- [32].Kang H, Song HJ, Nam JH, et al. Risk factors of asthma exacerbation based on asthma severity: a nationwide population-based observational study in South Korea. BMJ Open. 2018;8(3):e020825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Suruki RY, Daugherty JB, Boudiaf N, et al. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm Med. 2017;17(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Kim J-L, Henneberger PK, Lohman S, et al. Impact of occupational exposures on exacerbation of asthma: a population-based asthma cohort study. BMC Pulm Med. 2016;16(1):148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Ilmarinen P, Tuomisto LE, Niemelä O, et al. Prevalence of patients eligible for anti-IL-5 treatment in a cohort of adult-onset asthma. J Allergy Clin Immunol Pract. 2019;7(1):165–174.e4. [DOI] [PubMed] [Google Scholar]
- [36].Watase H, Hagiwara Y, Chiba T, et al. Multicentre observational study of adults with asthma exacerbations: who are the frequent users of the emergency department in Japan? BMJ Open. 2015;5(4):e007435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Vähätalo I, Ilmarinen P, Tuomisto LE, et al. 12-year adherence to inhaled corticosteroids in adult-onset asthma. ERJ Open Res. 2020;6(1):00324–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Bloom CI, Palmer T, Feary J, et al. Exacerbation patterns in adults with asthma in England. A population-based study. Am J Respir Crit Care Med. 2019;199(4):446–453. [DOI] [PubMed] [Google Scholar]
- [39].Alshabanat A, Zafari Z, Albanyan O, et al. Asthma and COPD overlap syndrome (ACOS): a systematic review and meta analysis. PLoS One. 2015;10:e0136065. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request from the authors.


