Abstract
Infection with severe fever with thrombocytopenia syndrome (SFTS) virus, which can cause hemorrhagic febrile illness, is often transmitted by ticks. We identified 3 patients with SFTS in or near Bangkok, Thailand. Our results underscore a need for heightened awareness by clinicians of possible SFTS virus, even in urban centers.
Keywords: severe fever with thrombocytopenia syndrome virus, SFTS, SFTSV, vector-borne infections, viruses, phleboviruses, febrile illnesses, infections, Thailand, Asia
Severe fever with thrombocytopenia syndrome (SFTS) is a tickborne viral disease associated with acute fever, possibly accompanied by vomiting, diarrhea, fatigue, myalgia, and leukocytopenia (1). Most reports of infection have come from studies in South Korea, Japan, and China, although Taiwan, Vietnam, and Myanmar have had confirmed cases in recent years (2). Severe infections can cause hemorrhagic fever and multiple organ failure leading to death. SFTS results from infection by the SFTS virus (SFTSV, newly renamed Dabie bandavirus), an RNA virus in the family Phenuiviridae, genus Bandavirus (3). More frequent arbovirus infections in Thailand, primarily dengue and chikungunya, often confound diagnosis of febrile illness caused by other viruses such as SFTSV because most clinicians lack awareness.
Testing during an upsurge in chikungunya virus infection in Thailand at the end of 2018 found that >70% of acute febrile illnesses were laboratory-confirmed chikungunya (4). As the proportion of chikungunya virus–positive samples eventually decreased, we began to screen for other common viral etiologies of acute fever, including dengue and Zika viruses (Appendix Figure). Because SFTSV had been reported in 2 patients in Vietnam (5) at the time, when the samples from Thailand tested negative for all 3 more common viruses, we began examining for possible SFTSV infection. The Institutional Review Board of Chulalongkorn University Faculty of Medicine approved this study (IRB number 0453/65).
We subjected de-identified archived RNA samples from 712 patients from Bangkok and surrounding areas, hospitalized during October 2018–March 2021, to reverse transcription PCR to detect the nucleoprotein gene region of the small (S) segment of SFTSV (6). Three samples tested positive, so we used 3 primer sets described elsewhere (7) to determine full-length S-segment nucleotide sequences. We deposited sequences in the GenBank database (accession numbers ON840548–50) and constructed the SFTSV S-segment phylogenetic tree using MEGA11 (https://www.megasoftware.net).
Phylogenetic analysis suggested that the 3 SFTSV strains from Thailand shared ≈99.7% nucleotide sequence identities and were genetically closest to the SFTSV strains from China identified in 2012–2017 (99.3%–99.6% nucleotide identity) (Figure; Appendix Table). On the basis of available clinical records, all 3 patients reported myalgia with lower than normal leukocyte (<3,000 cells/μL) and platelet (<110,000 cells/μL) counts (Table). Two patients experienced elevated alanine and aspartate aminotransferase levels (>60 U/L). Although patient 1 did not demonstrate substantially altered leukocyte count or blood chemistry, he experienced gastrointestinal symptoms (abdominal pain, nausea, vomiting, and diarrhea).
Figure.
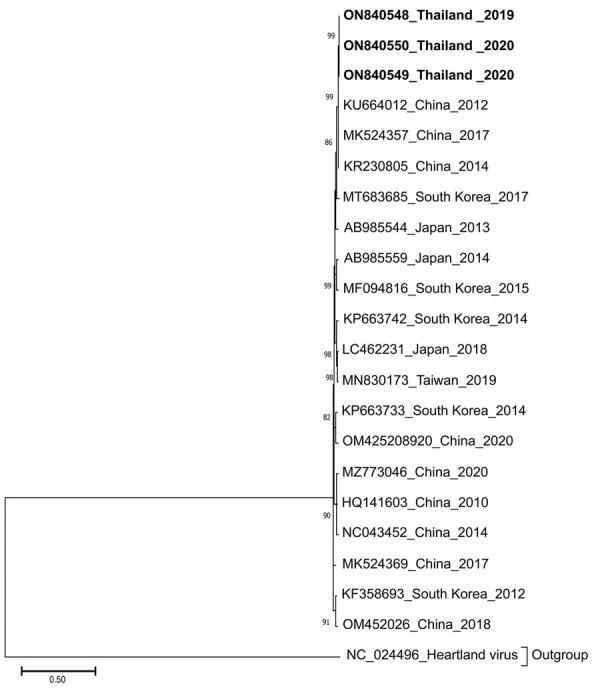
Phylogenetic analysis of the S segment sequence (1,674 bp) of 3 SFTSV strains from Thailand (bold) compared with reference sequences. The tree was generated using the maximum-likelihood method based on the Kimura 2-parameter model with 1,000 bootstrap replicates. Strains are noted with GenBank accession numbers, country, and year of isolation. Bootstrap values >70% are indicated at the branch nodes. Scale bar indicates the number of substitutions per site.
Table. Characteristics and detection of severe fever with thrombocytopenia syndrome virus in 3 patients in Thailand, 2019–2020.
| Category | Patient 1 | Patient 2 | Patient 3 |
|---|---|---|---|
| Age, y/sex |
60/M |
16/M |
52/F |
| Location |
Bangkok |
Chachoengsao |
Bangkok |
| Collection date |
2019 Nov 14 |
2020 May 10 |
2020 Oct 19 |
| Clinical manifestations | |||
| Temperature | 37.2°C | 40.6°C | 38.1°C |
| Clinical signs and symptoms |
Myalgia, arthralgia, cough, nausea, vomiting, abdominal pain, diarrhea |
Myalgia |
Myalgia, arthralgia |
| Laboratory findings (reference range) | |||
| Leukocytes, cells/µL (4,100–10,900) | 1,790 | 900 | 2,770 |
| Neutrophils, % (40–72) | 45 | 31 | 62 |
| Lymphocytes, % (18–49) | 42 | 59 | 34 |
| Platelets, cells/µL (140,000–400,000) | 107,000 | 45,000 | 121,000 |
| Aspartate aminotransferase, U/L (<40) | Not done | 102 | 1,758 |
| Alanine aminotransferase, U/L (<41) |
24 |
63 |
973 |
| Pathogens tested for but not detected | Rickettsia/Orientia spp., influenza A/B | Rickettsia/Orientia spp., influenza A/B, Epstein-Barr, hepatitis B/C, SARS-CoV-2, malaria, Leptospira, Burkholderia pseudomallei | Rickettsia/Orientia spp., hepatitis A/B |
Patients reported no history of travel within 3 weeks before symptom onset. Patients 1 and 3 lived in Bangkok, whereas patient 2 lived in Chachoengsao Province, ≈40 km east of Bangkok. Because international travel was severely limited during the global coronavirus pandemic beginning in 2020, transboundary transmission of SFTSV was unlikely.
A study in South Korea found that roughly one quarter of SFTSV infections accompanied scrub typhus caused by Orientia tsutsugamushi infection (8) and suggested the possibility of the chigger mite as a potential vector of the virus. To further investigate potential co-infection with tickborne and chiggerborne bacteria, we performed multiplexed quantitative PCR to detect Orientia and Rickettsiae spp. None of our 3 patients tested positive for these bacteria.
Our study identified SFTSV by analyzing febrile illnesses among patients who previously tested negative for arboviruses typically suspected of causing acute fever in Thailand. We found that <0.5% of these samples tested positive for SFTSV, which represented only 0.1% prevalence when all febrile illnesses were considered. However, this percentage might be higher in patients residing in rural areas or who engage in agriculture. A strength of this study was confirmation of SFTSV from full-length S-segment nucleotide sequences from 3 symptomatic patients residing in urban areas during November 2019–October 2020.
We do not know how the patients in our study contracted SFTSV, particularly the identities of any likely reservoir hosts and arthropod vectors, because of limited available clinical information regarding viral exposure. To date, 4 tick species are known vectors for SFTSV: Haemaphysalis longicornis, Amblyomma testudinarium, Rhipicephalus microplus, and Ixodes nipponensis, the last of which is not present in Thailand (9,10). R. microplus is often found in livestock animals in countries in Southeast Asia, but all 3 patients in our study were urban dwellers. Our study was limited by using data from retrospective evaluation of clinical records, which could have been more comprehensive had physicians initially suspected SFTS. Also, the fact that patients did not travel internationally could not rule out domestic rural exposure to SFTSV. Another limitation was that insufficient S-segment sequences from SFTSV strains previously identified in countries in Southeast Asia, such as Myanmar and Vietnam, were available in the public database, preventing direct genetic comparison with the strains from Thailand identified in this study. Nevertheless, our finding of detailed molecular evidence of SFTSV infection in Thailand, although in very few patients to date, should increase awareness of SFTS and warrants further exploration into possible transmission cycles in tropical urban settings.
Addition information about study of severe fever with thrombocytopenia syndrome in Thailand.
Acknowledgments
This work was funded by the Center of Excellence in Clinical Virology of the Faculty of Medicine of Chulalongkorn University and Hospital. S.K. and P.R. were supported by the Second Century Fund of Chulalongkorn University.
Biography
Dr. Rattanakomol is a postdoctoral fellow in the Center of Excellence in Clinical Virology of Chulalongkorn University. Her research interests include emerging and reemerging respiratory and arthropod-borne viral infections.
Footnotes
Suggested citation for this article: Rattanakomol P, Khongwichit S, Linsuwanon P, Lee KH, Vongpunsawad S, Poovorawan Y. Severe fever with thrombocytopenia syndrome virus infection, Thailand, 2019–2020. Emerg Infect Dis. 2022 Dec [date cited]. https://doi.org/10.3201/eid2812.221183
References
- 1.Seo JW, Kim D, Yun N, Kim DM. Clinical update of severe fever with thrombocytopenia syndrome. Viruses. 2021;13:1213. 10.3390/v13071213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Casel MA, Park SJ, Choi YK. Severe fever with thrombocytopenia syndrome virus: emerging novel phlebovirus and their control strategy. Exp Mol Med. 2021;53:713–22. 10.1038/s12276-021-00610-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Committee on Taxonomy of Viruses. Taxon details: severe fever with thrombocytopenia syndrome virus [cited 2022 Jun 19]. https://ictv.global/taxonomy/taxondetails?taxnode_id=202100166
- 4.Khongwichit S, Chansaenroj J, Thongmee T, Benjamanukul S, Wanlapakorn N, Chirathaworn C, et al. Large-scale outbreak of Chikungunya virus infection in Thailand, 2018-2019. PLoS One. 2021;16:e0247314. 10.1371/journal.pone.0247314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tran XC, Yun Y, Van An L, Kim SH, Thao NTP, Man PKC, et al. Endemic severe fever with thrombocytopenia syndrome, Vietnam. Emerg Infect Dis. 2019;25:1029–31. 10.3201/eid2505.181463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang YZ, He YW, Dai YA, Xiong Y, Zheng H, Zhou DJ, et al. Hemorrhagic fever caused by a novel Bunyavirus in China: pathogenesis and correlates of fatal outcome. Clin Infect Dis. 2012;54:527–33. 10.1093/cid/cir804 [DOI] [PubMed] [Google Scholar]
- 7.Han XH, Ma Y, Liu HY, Li D, Wang Y, Jiang FH, et al. Identification of severe fever with thrombocytopenia syndrome virus genotypes in patients and ticks in Liaoning Province, China. Parasit Vectors. 2022;15:120. 10.1186/s13071-022-05237-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wi YM, Woo HI, Park D, Lee KH, Kang CI, Chung DR, et al. Severe fever with thrombocytopenia syndrome in patients suspected of having scrub typhus. Emerg Infect Dis. 2016;22:1992–5. 10.3201/eid2211.160597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takhampunya R, Sakolvaree J, Chanarat N, Youngdech N, Phonjatturas K, Promsathaporn S, et al. The bacterial community in questing ticks from Khao Yai national park in Thailand. Front Vet Sci. 2021;8:764763. 10.3389/fvets.2021.764763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang X, Zhao C, Cheng C, Zhang G, Yu T, Lawrence K, et al. Rapid spread of severe fever with thrombocytopenia syndrome virus by parthenogenetic Asian longhorned ticks. Emerg Infect Dis. 2022;28:363–72. 10.3201/eid2802.211532 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Addition information about study of severe fever with thrombocytopenia syndrome in Thailand.


