Abstract
Patients with post-acute sequelae after coronavirus disease (COVID-19) report a variety of non-specific neurological complications (e.g., myoclonus, limb weakness). In particular, they manifest scenarios as medically unexplained symptoms and are known as functional movement disorders (FMDs). We present three cases of FMDs in patients of the Institute of Clinical Medicine named after N. V. Sklifosovsky (Sechenov University). All patients had a history of COVID-19 infection and reported fatigue, weakness, and jerks of upper and lower limbs. In conclusion, there might be a major possibility of the virus negatively affecting the central nervous system, including such rare neuropsychiatric complications.
Keywords: COVID-19, fatigue, FMDs, functional movement disorders, jerks, limb weakness, myoclonus, post-COVID
INTRODUCTION
Patients with long coronavirus disease (COVID-19) report a variety of non-specific neurological complications.[1] The movement disorders are similarly reported after COVID-19.[2] Myoclonus, opsoclonus, and ataxia are the most common variety of movement impairments[3] and commonly have para-infectious and post-infectious etiology.[4,5] They also appear as functional movement disorders (FMDs).[3,6] FMDs are an impairment with voluntary movement control, despite normal ability to move and an intact neural capacity for movement.[7] Clinical evidence is generally used to establish the FMDs.
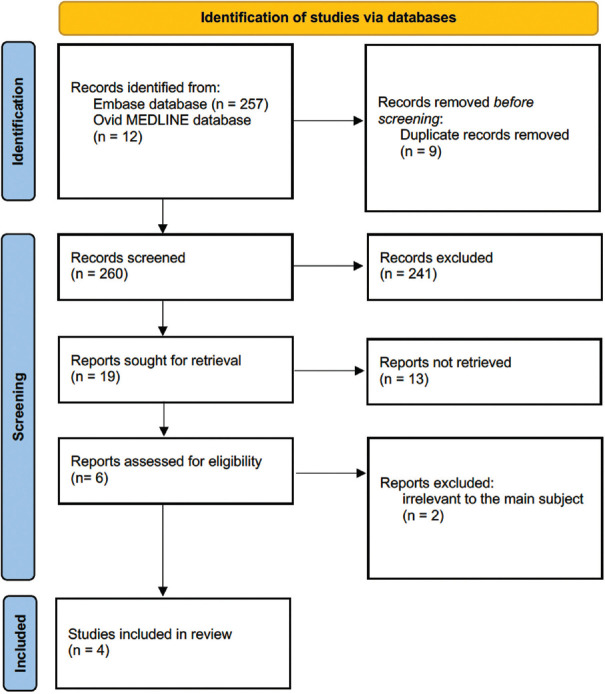
We performed an extensive electronic search using Embase/MEDLINE databases for relevant literature between December 31, 2019 and February 20, 2022. We constructed a search strategy using the terms “COVID-19” OR “SARS-CoV-2” OR “Coronavirus Disease 2019” OR “2019 n-CoV” OR “2019 Novel Coronavirus” AND (“Functional Movement Disorder” OR “Conversion Disorder” OR “Functional Gait Disorder” OR “Nonepileptic Seizure” OR “Functional (Psychogenic) Tremor” OR “Functional Weakness.” The combination of Medical Subject Headings (MeSH) terms was similarly used in the search strategy as (“SARS-CoV-2”[Mesh]) OR “COVID-19”[Mesh]) AND “Conversion Disorder”[Mesh]. The abstract screening was done after searching. Three clinical cases[8,9,10] and one cohort study[6] reported functional movement impairments in patients after COVID-19 infection. A flowchart diagram is presented in Figure 1.
Figure 1.
Flowchart
It implies that FMDs are rarely described compared to other neurological sequelae after COVID-19. We present three cases of FMDs in patients of our university.
CASE HISTORY
Case 1
The first case was a 51-year-old female patient without any previous psychiatric history. At age of 50, she got a moderate COVID-19 infection and was treated at home. Two weeks after recovering, she acutely felt significant fatigue, increasing weakness, and jerks of upper and lower limbs. She was urgently delivered to the emergency department, where she underwent an electroneuromyography (ENMG) study that revealed no pathological findings. She was discharged home and during eighteen months was experiencing body weakness, episodic jerks of limbs and screwing, and wringing pain in the affected limbs. In September 2021, her symptoms deteriorated. She collapsed and was admitted to the emergency ward. Doctors presumed her to have a myasthenic crisis, but after doing a decrement test, this presumption was precluded. Despite it, she was prescribed pyridostigmine, neostigmine, and prednisolone. However, her condition continued to deteriorate, and she was admitted to our clinic. Previous medication was canceled.
On therapeutic examination, she complained of pain in her limbs, severe fatigue, palpitation, dizziness, and tiredness. However, there were no pathological findings revealed after the examination. Laboratory tests of magnetic resonance imaging (MRI) and needle-ENMG showed no pathological findings. Neurological examination showed subjective limitation of upper and lower limb movement, decreased strength in proximal parts of limbs up to score of 2–4, while out of examination she was functioning without any limitations. Her gait was wide, staggering, and ataxic-like, but she had never fallen down. Pseudohyperreflective response with a fan-shaped extension of toes and repetitive intensive flexion of fingers after single touching were detected, but objectively pathological carpal and plantar reflexes were negative. During some tests, she developed clonic seizures in affected body parts. She did some coordination tests with severe intention tremor and past-pointing: S > D, but in other tests, she did correctly. She did not stand in Romberg’s pose.
After psychiatric examination, dissociative motor disorders were diagnosed according to ICD-10 (Simplified Functional Movement Disorder Rating Scale (S-FMDRS) score 34, DES-II: Total score 12, average score 4,3) without depression/anxiety.
She was treated with quetiapine 25 mg and clonazepam 2 mg with a slight improvement in night sleep and frequency of psychogenic seizures.
On discharge, she was recommended to refer to a psychiatric clinic to undergo specialized treatment.
Case 2
A 60-year-old female patient with a previous history of COVID-19 infection and admissions to the neurologic ward due to upper and lower limbs weakness was readmitted to the neurological ward. She had never been referred to a psychiatrist. She is married, has three children, and does not work. In stressful situations, she experienced apathy, muscle weakness, and fatigue for 3–5 days that were relieved without any treatment. When she was 59 years old (August 2020), she got COVID-19 and underwent inpatient treatment. She was admitted to the hospital with her spouse, but he died due to complications of coronavirus infection. After discharge, she felt upset, fatigued, inactive, and occupied with thoughts about the loss of her spouse. Also, since then she was experiencing episodes of faintness without seizures. She was treated with escitalopram for 6 months without any effect.
In January 2021, motor disturbances arose. She felt extremely fatigued and complained of weakness and dull pain in her upper and lower limbs, and insomnia. Her gait was weak, she used a baby walker to move. Her hands shook while operating. However, she still could walk and write something on the list with calm hands. In April 2021, she was admitted to our neurologic ward. Neurological workup and MRI scanning did not reveal any pathological findings. Her motor disturbances were evaluated as functional ones, and she got treatment with amitriptyline and diazepam. After 2 weeks of treatment, she reported improvement in sleep and mood and a decrease in anxiety. Her arms shook less. Fatigue and weakness of the limbs less affected her; she started to walk independently.
However, her condition was well only for a short term. She was readmitted to the neurological ward in November 2021 with a relapse of dizziness, and weakness in left upper and lower limbs. She complained of clumsy movements, so she could not serve herself. Therapeutic and neurologic examinations were the same. After psychiatric examination, she was diagnosed with moderate depressive disorder and comorbid dissociative motor disorder. On psychometric evaluation, there were high scores on Generalized Anxiety Disorder (GAD)-7 (20 points) and SOMS-2 (26 points), and moderate scores on Patient Health Questionnaire (PHQ)-9. According to S-FMDRS, the dissociative motor disorder was of moderate severity (23 points).
She was treated with quetiapine 100 mg and fluoxetine 40 mg. On discharge, she reported that her mood improved; she became more active and able to serve herself. While fatigue and weakness persisted, she was able to move without baby walkers and operate her hand precisely. She was recommended to undergo cognitive-behavioral psychotherapy.
Case 3
A female patient of 53-year-old was admitted to the neurological ward. The patient has traumatic experiences in her childhood such as violence towards her from her father, her father’s and brother’s suicide attempts and alcoholism, and abusive relationships. She considered herself ill since she was 23-year-old when the first episode of muscle jerks or muscle weakness had occurred after her first labors. From that time, such symptoms had seldom occurred again in stressful situations and were resolved in short term. In January 2021, she got a moderate COVID-19 infection and was inpatiently treated. In March 2021, she felt fatigued and had weakness in her lower limbs and left arm, so she could not move properly. Also, there were akinetic seizures when she felt that she was unconscious, could not move and control her body, and could not speak, but she could hear everything and could show signs with her eyes to her family members. These seizures happened once or twice a month and lasted some hours. Every time after seizures resolved, she felt fatigued.
She was referred to our clinic with the described symptoms and was admitted to the neurological ward. Neurological examination found some functional neurological signs. Straight leg rising caused a postural tremor in the limb during elevation up to 30°, tremor stopped after lifting the leg higher. Myoclonic movement of the whole body was observed during rest and was provoked by eyesight to the left and touching the forehead area. In the Romberg test, she fell to the left.
After psychiatric examination, dissociative motor disorder without comorbid depression/anxiety was diagnosed (S-FMDRS 26).
She was prescribed duloxetine in 60 mg daily and benzodiazepines. On discharge, her condition improved with lower rates of myoclonus.
DISCUSSION
The main advantage of our study is the demonstration of the series of previously practically undescribed neurological consequences of COVID-19. The main limitation is the lack of uniform data on the clinical efficacy of drugs in relation to FMDs.
The new onset of neurologic events in people after COVID-19 infection was described in several studies. Xiong et al.[6] conducted a retrospective cohort study with a representation of two patients with functional tic/tremor. Garg et al.[8] reported a case of a 54-year-old man who presented with flexion movement of the head which started 2 months after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. At a one-year follow-up, the patient still had jerky movements, as well as cognitive impairment, frequent headaches, occasional shortness of breath, sleeping difficulties, fatigue, and dizziness. Piscitelli et al.[9] presented a case of a 39-year-old woman with functional tremors developed after 7 days of COVID-19 infection. Gilio et al.[10] reported a case of a 23-year-old man who developed a complex of symptoms characterized by fatigue, episodic shortness of breath, and chest pain. He similarly had a loss of attention and memory, fluctuating limb dysesthesia, and weakness of his left arm. The patient was all-time asymptomatic regardless of the positive polymerase chain reaction test. In all three cases, the patients had undergone extensive workup and the results were normal.
The results of our study as a whole confirm the data of previous works on a slightly larger material. A detailed study of the patient’s history allows us to confidently judge the significant role of coronavirus infection in the manifestation/exacerbation of functional motor disorders.
In the first case, COVID-19 caused the appearance of FMDs in a previously completely healthy patient. In cases 2 and 3, COVID-19 led to a significant worsening of already existing symptoms. In addition, in case 2, FMDs developed in the presence of depression, provoked by COVID-19 and the death of a spouse. Taking into account the dynamics of the state, we cannot assert that depression was the cause of the functional neurologic disorder (FDN). FMDs are uncharacteristic for depression, in addition, depression responded quite well to therapy. FDN, in turn, only slightly weakened. Therefore, we can rather talk about the coexistence of two neuropsychiatric disorders.
The most important conclusion to be drawn from this series of clinical observations is the fundamental possibility of the virus to negatively affect the central nervous system, including such rare neuropsychiatric complications.
Clinicians should be aware of the possible onset of FMDs after COVID-19, and this problem deserves closer examination in studies with a different design.
All patients included in this study signed voluntary informed consent to participate.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Al-Ramadan A, Rabab’h O, Shah J, Gharaibeh A. Acute and post-acute neurological complications of COVID-19. Neurol Int. 2021;13:102–19. doi: 10.3390/neurolint13010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cuhna P, Herlin B, Vassilev K, Kas A, Lehericy S, Worbe Y, et al. Movement disorders as a new neurological clinical picture in severe SARS-CoV-2 infection. Eur J Neurol. 2020;27:e88–90. doi: 10.1111/ene.14474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brandão PRP, Grippe TC, Pereira DA, Munhoz RP, Cardoso F. New-onset movement disorders associated with covid-19. Tremor Other Hyperkinet Mov (N Y) 2021;11:26. doi: 10.5334/tohm.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan JL, Murphy KA, Sarna JR. Myoclonus and cerebellar ataxia associated with COVID-19:A case report and systematic review. J Neurol. 2021;268:3517–48. doi: 10.1007/s00415-021-10458-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emamikhah M, Babadi M, Mehrabani M, Jalili M, Pouranian M, Daraie P, et al. Opsoclonus-myoclonus syndrome, a post-infectious neurologic complication of COVID-19:Case series and review of literature. J Neurovirol. 2021;27:26–34. doi: 10.1007/s13365-020-00941-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiong W, Mu J, Guo J, Lu L, Liu D, Luo J, et al. New onset neurologic events in people with COVID-19 in 3 regions in China. Neurology. 2020;95:e1479–87. doi: 10.1212/WNL.0000000000010034. [DOI] [PubMed] [Google Scholar]
- 7.Thomsen BLC, Teodoro T, Edwards MJ. Biomarkers in functional movement disorders:A systematic review. J Neurol Neurosurg Psychiatry. 2020;91:1261–9. doi: 10.1136/jnnp-2020-323141. [DOI] [PubMed] [Google Scholar]
- 8.Garg A, Goyal S, Comellas AP. Post-acute COVID-19 functional movement disorder. SAGE Open Med Case Rep. 2021;9:2050313X211039377. doi: 10.1177/2050313X211039377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piscitelli D, Perin C, Tremolizzo L, Peroni F, Cerri CG, Cornaggia CM. Functional movement disorders in a patient with COVID-19. Neurol Sci. 2020;41:2343–4. doi: 10.1007/s10072-020-04593-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gilio L, Galifi G, Centonze D, Bassi MS. Case report: Overlap between long COVID and functional neurological disorders. Front Neurol. 2022;12:811276. doi: 10.3389/fneur.2021.811276. [DOI] [PMC free article] [PubMed] [Google Scholar]